Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Trauma-Informed and Culturally Responsive Practices interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Trauma-Informed and Culturally Responsive Practices Interview
Q 1. Define trauma-informed care and its core principles.
Trauma-informed care is a strength-based framework that recognizes the pervasive impact of trauma and emphasizes physical, psychological, and emotional safety for both providers and survivors. It shifts from a “what’s wrong with you?” approach to a “what happened to you?” approach. Core principles include:
- Safety: Creating a physically and emotionally safe environment where clients feel secure and protected.
- Trustworthiness and Transparency: Building rapport through open communication, clear expectations, and honesty.
- Peer Support and Mutual Self-Help: Utilizing the power of shared experience and support among trauma survivors.
- Collaboration and Mutuality: Working in partnership with clients, respecting their choices and autonomy.
- Empowerment, Voice, and Choice: Centering clients’ experiences and preferences in the therapeutic process.
- Cultural, Historical, and Gender Issues: Recognizing the intersectionality of trauma and its impact on diverse populations.
Imagine a clinic designed with trauma-informed care in mind. It might have soft lighting, comfortable seating, and clear, visible exits, all contributing to a sense of safety. Staff would be trained to be mindful of their own reactions and to create a calm and reassuring atmosphere.
Q 2. Explain the difference between trauma-informed and trauma-specific approaches.
While both trauma-informed and trauma-specific approaches acknowledge the impact of trauma, they differ in their focus and intensity. Trauma-informed care is a broad framework that integrates trauma awareness into all aspects of service delivery. It’s about creating a safe and supportive environment. Trauma-specific treatments, on the other hand, directly address the symptoms and effects of trauma through evidence-based therapies like Eye Movement Desensitization and Reprocessing (EMDR) or Cognitive Processing Therapy (CPT). Think of it this way: trauma-informed care is the foundation, while trauma-specific treatments are targeted interventions built on that foundation.
For example, a trauma-informed school might have a flexible attendance policy, understanding that trauma can affect a child’s ability to attend regularly. A trauma-specific intervention might involve working with a child individually using EMDR to process a specific traumatic event.
Q 3. Describe how cultural responsiveness influences trauma-informed practice.
Cultural responsiveness is crucial in trauma-informed practice because trauma is experienced and expressed differently across cultures. Ignoring cultural context can lead to misinterpretations of behavior, ineffective interventions, and even further harm. Cultural responsiveness involves understanding the client’s worldview, values, beliefs, and practices, and adapting the therapeutic approach accordingly. It means considering factors like family structures, communication styles, and spiritual beliefs.
For instance, some cultures may emphasize collectivism over individualism, which could influence how a survivor discloses their trauma. A culturally responsive therapist would adapt their approach to honor the client’s cultural norms and build trust within that context.
Q 4. How do you assess for trauma in diverse populations?
Assessing for trauma in diverse populations requires a holistic and culturally sensitive approach. It’s not about ticking boxes on a checklist but about building a trusting relationship and observing subtle cues. This involves understanding that trauma manifests differently, and symptoms may be masked by other cultural factors or interpreted as something else entirely. It’s crucial to use culturally appropriate assessment tools and avoid making assumptions based on stereotypes.
For example, instead of directly asking about specific traumatic events, which might be culturally inappropriate or triggering, a practitioner might ask open-ended questions about past experiences, challenges faced, or significant life events. Active listening, observation of body language, and collaboration with community resources are all key.
Q 5. What are the ethical considerations of working with trauma survivors?
Ethical considerations in working with trauma survivors are paramount. These include maintaining confidentiality, ensuring informed consent, avoiding retraumatization, recognizing power dynamics, and setting appropriate boundaries. It’s crucial to prioritize the client’s safety and well-being and to be mindful of the potential for transference and countertransference. Continuing education and supervision are vital to maintaining ethical and competent practice.
For instance, a therapist must carefully consider the potential impact of their questions and interventions and be prepared to adjust their approach if the client appears distressed. They must also be aware of their own biases and limitations and seek consultation when necessary.
Q 6. Explain how you would adapt your approach based on a client’s cultural background.
Adapting my approach based on a client’s cultural background requires pre-session research and ongoing dialogue. This involves learning about the client’s culture, values, and beliefs. This might involve seeking information from trusted sources within that community. I would then incorporate this knowledge into the therapeutic process by adjusting my communication style, treatment modalities, and even the physical setting if necessary. For instance, I might adjust the pace of sessions or incorporate culturally relevant metaphors or stories to build rapport and facilitate understanding.
For example, if working with a client from a collectivist culture, I might invite family members to participate in sessions, if the client desires. This respects their cultural values and strengthens the support system.
Q 7. Describe a situation where you had to navigate cultural differences in a therapeutic setting.
In a previous session with a client from a Southeast Asian background, I noticed she was hesitant to make eye contact, which I initially interpreted as a lack of engagement. However, after further research into her cultural background, I learned that avoiding direct eye contact is a sign of respect in her culture. Recognizing this, I adapted my approach, focusing on building rapport through other means, such as careful listening and attentive nonverbal cues. This change led to a significant increase in her comfort level and willingness to open up about her trauma.
Q 8. How do you build rapport and trust with trauma survivors from diverse backgrounds?
Building rapport and trust with trauma survivors from diverse backgrounds requires a nuanced approach that prioritizes cultural humility and sensitivity. It’s not a one-size-fits-all process; rather, it’s about meeting individuals where they are, acknowledging their unique experiences, and fostering a sense of safety and validation.
Active Listening and Empathy: Truly hearing their story, without judgment or interruption, is paramount. This means paying attention not only to their words but also to their body language and emotional tone. For example, if someone hesitates to share, I might say, “I understand this might be difficult, and you can take your time.”
Cultural Sensitivity: Recognizing that cultural values, communication styles, and expressions of trauma vary significantly is crucial. I ensure my communication is respectful of their cultural norms and avoid making assumptions based on stereotypes. For example, direct eye contact may be considered disrespectful in some cultures, while silence can signify respect in others.
Building a Collaborative Relationship: I emphasize that they are the expert on their own experiences and work collaboratively to define goals and treatment strategies. This shared decision-making process is empowering and builds trust. I might say, “What are your hopes for our work together?”
Establishing Boundaries and Safety: Clearly outlining the therapeutic boundaries and ensuring their physical and emotional safety is essential. This can involve creating a safe space, verbally assuring them of their right to set limits, and having clear protocols for handling potential crisis situations.
For instance, I once worked with a refugee who had experienced significant trauma during wartime. It took several sessions before she felt comfortable enough to share her experiences, partly due to the language barrier and cultural differences. By using a translator and employing a slow, patient approach focused on building trust, we eventually established a strong therapeutic relationship.
Q 9. What strategies do you use to promote client empowerment and self-determination?
Promoting client empowerment and self-determination is fundamental to trauma-informed care. It shifts the focus from a deficit-based model to one that recognizes the survivor’s inherent strengths and resilience.
Strengths-Based Approach: I begin by identifying their strengths, skills, and resources – past and present. This helps them recognize their capacity for growth and healing. I might ask, “What are some things you’re proud of accomplishing?”
Shared Decision-Making: I involve clients in every aspect of the treatment process, ensuring they have a voice in defining their goals, selecting interventions, and evaluating progress. I avoid imposing my own perspectives or solutions.
Narrative Therapy: This approach empowers clients to re-author their stories, shifting from victimhood to agency. By helping them reinterpret their experiences and reclaim their narrative, they gain a sense of control and self-efficacy.
Skill-Building: I provide clients with tools and skills to manage their symptoms, cope with stressors, and navigate challenging situations. This can include coping mechanisms, communication skills, or problem-solving techniques.
For example, I worked with a young woman who experienced domestic violence. Instead of focusing solely on the trauma, we explored her strengths – her artistic talent, her supportive network of friends, and her determination to create a better life. By highlighting these strengths, she was able to build upon them and actively participate in shaping her recovery journey.
Q 10. How do you address vicarious trauma and maintain your own well-being?
Vicarious trauma, the emotional residue of exposure to another’s trauma, is a significant concern for those working with trauma survivors. Addressing it is vital for maintaining my own well-being and ensuring I can continue providing effective care.
Self-Care Practices: This is not a luxury but a necessity. I prioritize regular exercise, healthy eating, sufficient sleep, and mindfulness practices such as meditation or yoga. These help me regulate my emotions and manage stress.
Supervision and Peer Support: Regularly discussing my cases with a supervisor or trusted colleague allows me to process difficult emotions and receive guidance. Peer support groups provide a safe space to share experiences and gain perspective.
Setting Boundaries: It’s crucial to establish and maintain healthy boundaries to prevent emotional burnout. This means limiting my caseload, prioritizing self-care, and avoiding bringing work home.
Mindfulness and Self-Compassion: Practicing mindfulness helps me stay grounded and present, while self-compassion helps me avoid self-criticism when feeling overwhelmed. I acknowledge that it’s okay to feel affected by the trauma of others and that seeking support is a strength, not a weakness.
I use a simple self-reflection technique after each session to process my emotional state, noting any feelings that need attention. This helps prevent the accumulation of vicarious trauma and allows for timely self-care intervention.
Q 11. Describe your experience with implementing trauma-informed practices in a specific setting.
I implemented trauma-informed practices in a community-based mental health clinic serving a diverse population, including refugees, survivors of domestic violence, and individuals experiencing homelessness. We adopted a multi-pronged approach.
Staff Training: We conducted extensive training for all staff on trauma-informed principles, including understanding the impact of trauma, recognizing signs of trauma, and employing trauma-sensitive communication techniques.
Environmental Modifications: We redesigned the clinic space to be more calming and welcoming, minimizing triggers such as bright lights or loud noises. We also created a comfortable waiting area with soothing colors and soft lighting.
Policy Changes: We revised our policies to be more client-centered and trauma-sensitive. For example, we ensured clients had control over their appointment scheduling and treatment plans. We also implemented a flexible approach to missed appointments, recognizing that various factors can prevent attendance.
Collaboration: We worked closely with community partners to provide comprehensive support services, including housing assistance, legal advocacy, and vocational training.
The results were remarkable. Client satisfaction increased significantly, and we observed improved engagement in therapy and better overall outcomes. The trauma-informed approach fostered trust and created a more supportive environment for healing.
Q 12. How do you incorporate cultural humility into your practice?
Cultural humility is not about possessing expert knowledge about every culture; it’s about acknowledging the limitations of my own understanding and actively seeking to understand the client’s cultural context within their lived experience.
Self-Reflection: I regularly reflect on my own cultural biases and assumptions. This includes considering how my background and beliefs might influence my interactions with clients from different cultures.
Client-Centered Approach: I prioritize understanding the client’s perspective and beliefs, allowing them to define their cultural identity and its impact on their experience of trauma. This might involve asking open-ended questions like, “How does your cultural background influence your understanding of health and well-being?”
Collaboration and Consultation: When needed, I consult with cultural experts or community leaders to gain a deeper understanding of a client’s cultural context and adapt my approach accordingly.
Respect for Differences: I recognize that cultural values and norms are diverse and avoid imposing my own values or beliefs. I embrace differences and consider various communication styles and expressions of emotions.
For example, I worked with a client who had a different worldview on mental health compared to mine. Instead of imposing my framework, I took the time to learn about her beliefs and collaborated with her to develop a treatment plan that honored her cultural perspective.
Q 13. What are some common barriers to providing culturally responsive trauma-informed care?
Providing culturally responsive trauma-informed care presents several significant barriers:
Language Barriers: Communication difficulties can hinder the ability to build rapport, understand the client’s experience, and effectively deliver treatment. Access to qualified interpreters is crucial but often limited.
Cultural Misunderstandings: Differences in cultural values, beliefs, and communication styles can lead to misinterpretations and mistrust. This underscores the importance of continuous learning and cultural humility.
Lack of Culturally Specific Resources: Many communities lack culturally appropriate resources, such as mental health professionals from the same cultural background or trauma-informed services tailored to specific cultural needs.
Systemic Barriers: Systemic racism, discrimination, and inequities in access to healthcare can create significant barriers for marginalized communities, making it difficult for them to access and benefit from culturally responsive care. This includes challenges like insurance coverage, transportation, and scheduling conflicts.
Lack of Training and Awareness: Many mental health professionals lack adequate training in culturally responsive and trauma-informed practices, limiting their ability to effectively serve diverse populations.
Addressing these barriers requires a multi-pronged approach involving increased funding for culturally specific services, enhanced training for mental health professionals, and policy changes to address systemic inequities. It also requires active community engagement and collaboration to build trust and ensure culturally relevant care is accessible to all.
Q 14. How do you ensure safety and create a supportive environment for trauma survivors?
Ensuring safety and creating a supportive environment for trauma survivors is the foundation of effective trauma-informed care. It involves both physical and emotional safety.
Physical Safety: This includes a safe and accessible physical space free from potential triggers, as well as clear protocols for handling emergencies or crisis situations. It also involves ensuring clients feel safe during transportation to and from sessions.
Emotional Safety: This is about creating a therapeutic relationship that is built on trust, respect, and validation. It means listening without judgment, validating their experiences, and empowering them to set their own pace and boundaries. I utilize validating statements such as, “That sounds incredibly difficult,” or “I understand why you feel that way.”
Collaboration and Choice: It is crucial to involve clients in all decisions related to their care, allowing them the autonomy to choose their treatment goals and methods. This ensures they feel in control and empowered throughout the therapeutic process.
Trauma-Sensitive Language: I avoid using language that could be triggering, such as blaming or shaming language. Instead, I use person-first language and focus on the client’s strengths and resilience.
Safety Planning: Collaborating with clients to develop safety plans for managing potential triggers or crisis situations is an essential aspect of ensuring their continued safety and well-being.
For example, in a session with a survivor of domestic violence, we might discuss strategies for managing potential contact with the abuser, creating a support network, and developing a plan for leaving the abusive situation if necessary.
Q 15. How do you collaborate effectively with colleagues and community resources to support trauma survivors?
Effective collaboration is the cornerstone of trauma-informed and culturally responsive care. It involves building strong relationships based on trust, mutual respect, and shared understanding. With colleagues, this means regular case conferencing, utilizing a collaborative treatment planning process, and actively seeking feedback to ensure a consistent and supportive therapeutic environment.
With community resources, it involves establishing strong referral networks and actively engaging with other professionals like medical providers, social workers, legal aid, and faith-based organizations to create a comprehensive support system. This might involve attending community meetings, participating in joint training, or co-developing programs to meet the specific needs of the community. For instance, if a client needs housing assistance, I would directly connect them with appropriate local agencies and even help them navigate the application process if needed. This coordinated effort ensures that clients receive holistic support, addressing their needs across multiple domains.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your understanding of the impact of historical and systemic trauma.
Historical and systemic trauma refers to the cumulative emotional and psychological wounds inflicted on individuals and groups due to pervasive historical injustices and ongoing oppressive systems. These can include colonization, slavery, racism, poverty, and gender-based violence. The impact is far-reaching, manifesting in present-day disparities in health, education, and economic opportunity. For example, the intergenerational trauma resulting from historical oppression can show up in communities with higher rates of mental health challenges, substance abuse, and family conflict. It’s crucial to acknowledge these systemic factors when working with survivors because individual trauma often exists within a larger context of societal injustice. Understanding this context informs culturally responsive practices and guides us in addressing the root causes of suffering rather than solely focusing on individual symptoms.
Q 17. What are some common trauma responses you might encounter, and how would you address them?
Trauma responses are diverse and depend on the individual’s experiences, coping mechanisms, and cultural background. Some common responses include hypervigilance (being constantly on alert), anxiety, depression, flashbacks, nightmares, emotional numbness, difficulty with relationships, and substance abuse. Addressing these responses requires a trauma-informed approach, prioritizing safety, trustworthiness, choice, collaboration, and empowerment.
For instance, if a client exhibits hypervigilance, I would create a safe and predictable environment, explaining procedures in advance, and respecting their need for personal space and control. If they’re experiencing flashbacks, I would employ grounding techniques and help them identify triggers to manage their emotional distress. Throughout, I would emphasize collaborative goal setting, ensuring that the client feels empowered to participate in their own healing journey.
Q 18. How do you handle situations where your personal beliefs conflict with a client’s cultural values?
Addressing conflicts between personal beliefs and a client’s cultural values requires a commitment to humility, self-reflection, and cultural humility. It starts with acknowledging that my own worldview is just one perspective among many. The most crucial step is to prioritize the client’s autonomy and self-determination. This means understanding and respecting their beliefs, even if they differ from my own, and actively working to provide culturally sensitive and appropriate care.
For example, if a client’s cultural practices conflict with a recommended treatment plan, I would engage in open and respectful dialogue to explore alternative options that align with their values while still effectively addressing their needs. Seeking consultation with colleagues or cultural experts might be beneficial in these scenarios. It’s about adapting, not compromising ethical standards, but creatively finding solutions that respect the client’s cultural context and beliefs.
Q 19. What resources are available to you for support and continuing education in trauma-informed care?
Numerous resources support continuing education and professional development in trauma-informed care. These include professional organizations offering workshops and conferences, online courses and certifications through reputable institutions, and supervision or consultation with experienced clinicians. Many organizations provide specialized training in areas like cultural competency, specific trauma types (e.g., complex trauma), and effective intervention strategies. Additionally, peer support groups and mentoring programs offer valuable opportunities for sharing experiences and learning from others in the field. Keeping up-to-date with evidence-based practices is crucial, ensuring I provide the most effective and ethical care.
Q 20. How do you adapt your communication style to meet the needs of individuals with varying levels of literacy and communication skills?
Adapting communication is vital for ensuring accessibility and inclusivity. This involves using clear and simple language, avoiding jargon, and employing various communication modalities as needed. For clients with low literacy, I might use visual aids, pictures, or written materials with large font sizes. I might also break down complex information into smaller, manageable chunks. For clients with communication difficulties, I might use alternative methods like nonverbal cues, assistive technology, or interpreters, always adapting to meet individual needs and preferences. Active listening and observation are crucial in these scenarios to ensure understanding and build rapport.
Q 21. Describe a time you had to modify your approach due to a client’s cultural beliefs or practices.
I once worked with a client from a collectivist culture who preferred family involvement in their therapy sessions. Initially, my approach was more aligned with traditional individual therapy. However, understanding the importance of family support in their cultural context, I adapted my approach to incorporate family meetings. This required modifying my therapeutic framework, focusing more on family dynamics and working collaboratively with family members to support the client’s healing process. This was a significant adjustment, but ultimately resulted in much better engagement and positive outcomes for the client.
Q 22. How do you utilize strengths-based approaches in your work with trauma survivors?
Strengths-based approaches are crucial in working with trauma survivors because they shift the focus from deficits to capabilities. Instead of dwelling on the trauma’s negative impact, we identify and build upon the survivor’s inherent resilience, coping mechanisms, and existing strengths. This empowers them to actively participate in their healing journey.
For example, a client might have demonstrated remarkable perseverance in overcoming past challenges. We would acknowledge and validate this strength, emphasizing how this same resilience can be utilized to navigate current difficulties. We might collaboratively explore past successes and identify the skills and resources that contributed to those positive outcomes. This approach fosters hope and self-efficacy, vital components of the healing process. Another example could involve a client who is highly creative; we might integrate art therapy or journaling into their treatment plan to leverage their artistic expression as a tool for processing emotions and building self-esteem.
Q 23. How do you ensure confidentiality and maintain ethical boundaries in your practice?
Confidentiality and ethical boundaries are paramount in my practice. I adhere strictly to professional codes of ethics, which include obtaining informed consent before initiating any intervention, maintaining client records securely, and only sharing information with others involved in their care with their explicit permission. This includes adhering to HIPAA regulations in the US, or equivalent regulations in other jurisdictions.
To maintain ethical boundaries, I establish clear professional relationships. I avoid dual relationships, such as becoming friends or engaging in social activities with clients outside of therapeutic sessions. I always prioritize the client’s well-being and avoid situations that could create a conflict of interest. If personal feelings or biases arise, I utilize supervision or consultation to ensure objectivity and ethical practice. For example, I may seek consultation when working with a client whose trauma experience resonates with my own past experiences. This helps me maintain professional distance and objectivity, ensuring the client’s needs remain the priority.
Q 24. Describe your experience with crisis intervention and de-escalation techniques.
Crisis intervention and de-escalation are essential skills in trauma work. My training encompasses various techniques, including active listening, validation of emotions, and identifying triggers. I aim to create a safe and predictable environment where the client feels understood and respected.
De-escalation strategies include using calming language, reducing environmental stimuli (e.g., dimming lights, lowering volume), and offering choices to regain a sense of control. For instance, if a client is experiencing an intense emotional outburst, I might offer them a quiet space to breathe or a comforting object to hold. I’m trained in recognizing signs of escalating distress, such as increased agitation, rapid breathing, or changes in vocal tone, allowing me to intervene proactively. If a situation surpasses my capabilities, I ensure the client receives appropriate emergency services.
Q 25. How do you recognize and respond to signs of potential relapse or crises in trauma survivors?
Recognizing potential relapse or crisis requires attentive observation and a strong therapeutic relationship. Changes in sleep patterns, appetite, mood swings, increased anxiety, substance use, or a recurrence of trauma symptoms (such as nightmares or flashbacks) can all be indicators. I actively collaborate with clients to identify their individual triggers and warning signs, enabling early intervention.
For example, if a client reports increased nightmares and difficulty sleeping, we explore potential triggers and develop coping strategies, such as relaxation techniques or revisiting previously established safety plans. Regular check-ins and open communication are crucial to maintain a sense of connection and support during potentially challenging periods. We create a safety plan together as a proactive measure, outlining specific steps they can take when feeling overwhelmed, such as contacting a support person or engaging in self-soothing activities. This collaborative approach empowers clients to actively manage their symptoms and reduce the risk of crisis.
Q 26. What are your skills in working with families affected by trauma?
Working with families affected by trauma requires a family systems perspective. I assess the impact of trauma on family dynamics, communication patterns, and individual roles within the system. My approach focuses on strengthening family relationships, improving communication, and fostering mutual support.
For instance, I might facilitate family therapy sessions to address trauma’s ripple effects on family members, providing a safe space to express emotions and rebuild trust. I also work individually with family members to address their unique needs and experiences. I might teach the family evidence-based coping strategies to deal with stress and conflict, creating a more stable environment for healing. I strive to empower families to develop resilience and support one another in the healing process. I would be mindful of the possibility of intergenerational trauma and its impact across family systems.
Q 27. How do you measure the effectiveness of trauma-informed interventions?
Measuring the effectiveness of trauma-informed interventions involves a multifaceted approach that includes both qualitative and quantitative methods. Quantitative measures might involve using standardized assessment tools to track changes in symptoms of PTSD, anxiety, or depression over time.
Qualitative data, however, often provides a richer understanding of the client’s experience. This might involve regular feedback sessions with the client to gauge their progress, assess their satisfaction with the intervention, and monitor their self-reported improvement in symptoms and overall well-being. We can also use narrative techniques to gain insight into their experiences. Combining these approaches gives a comprehensive picture of the intervention’s impact, leading to better informed treatment planning and improved outcomes. The success isn’t solely based on symptom reduction, but also on the client’s improved sense of safety, self-efficacy, and improved quality of life.
Key Topics to Learn for Trauma-Informed and Culturally Responsive Practices Interview
- Understanding Trauma: Defining trauma, its impact on individuals and communities, and the neurobiological effects.
- Trauma-Informed Principles: Safety, trustworthiness, choice, collaboration, and empowerment in practice. How these principles translate into specific actions and interventions.
- Cultural Humility: Defining cultural humility, its distinction from cultural competence, and the ongoing process of self-reflection and learning.
- Cultural Responsiveness in Practice: Adapting interventions and approaches to meet the unique needs of diverse populations, considering factors like race, ethnicity, gender, sexual orientation, and socioeconomic status.
- Ethical Considerations: Navigating ethical dilemmas related to confidentiality, power dynamics, and cultural sensitivity in trauma-informed care.
- Practical Application: Developing strategies for creating safe and supportive environments, engaging clients effectively, and responding to trauma-related behaviors.
- Assessment and Intervention: Discuss various assessment tools and therapeutic approaches suited for trauma-informed and culturally responsive care.
- Collaboration and Advocacy: Importance of working collaboratively with diverse teams and advocating for policy changes that promote equity and justice.
- Self-Care and Resilience: Recognizing the importance of self-care practices for professionals working in trauma-informed settings.
Next Steps
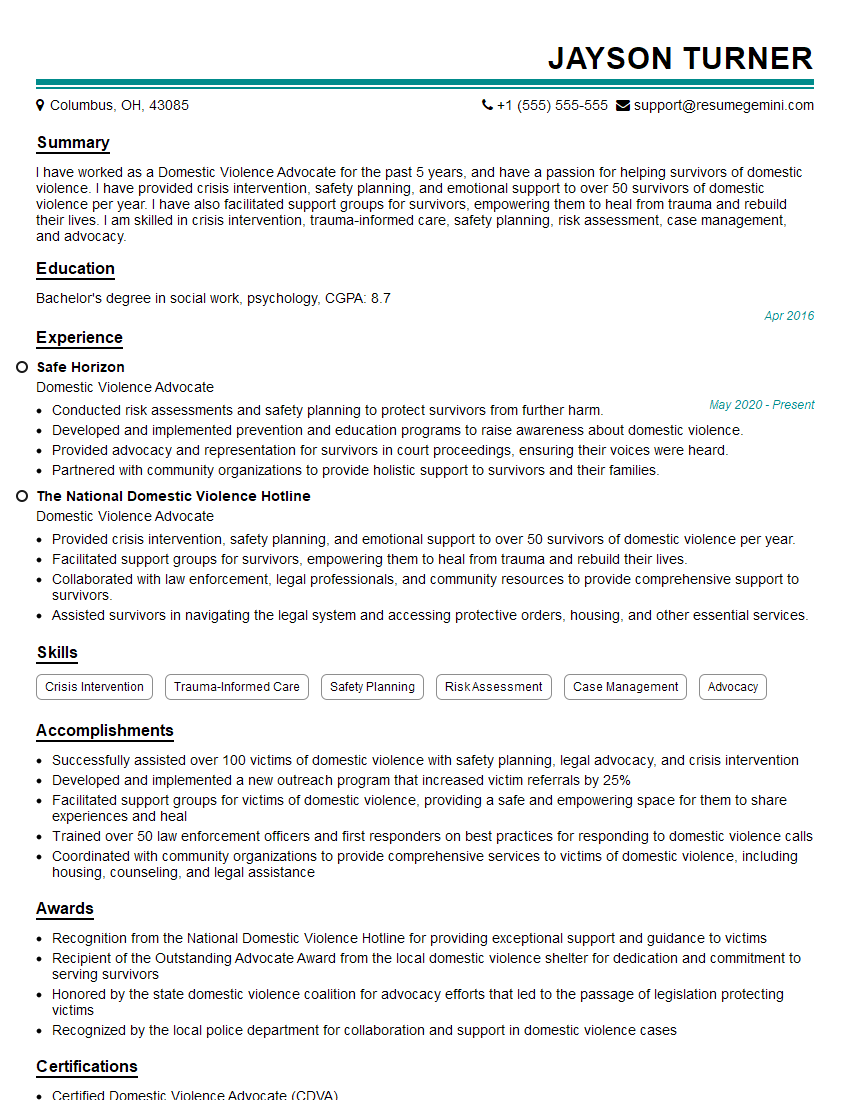
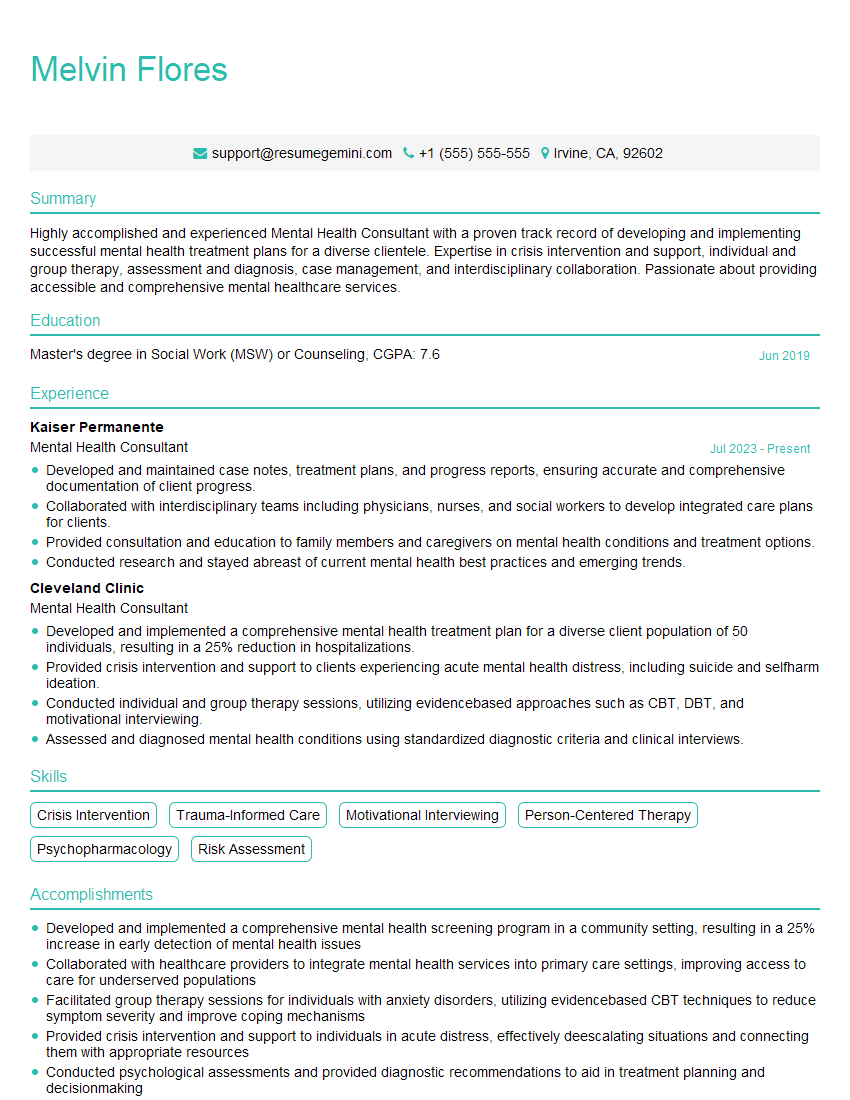
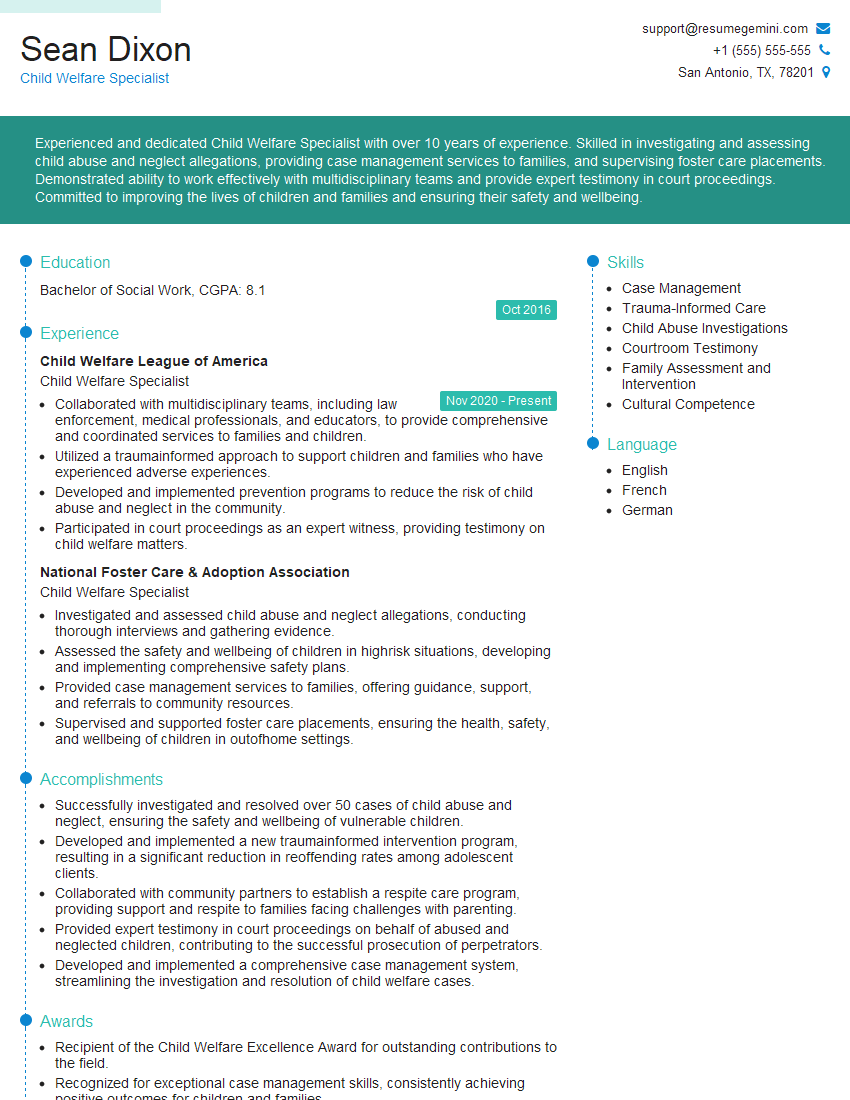
Mastering Trauma-Informed and Culturally Responsive Practices is crucial for career advancement in today’s diverse and increasingly trauma-aware world. Demonstrating a strong understanding of these principles will significantly enhance your job prospects and allow you to make a truly meaningful impact on the lives of others. To maximize your chances of landing your dream role, creating a strong, ATS-friendly resume is essential. ResumeGemini is a trusted resource to help you build a compelling resume that showcases your skills and experience effectively. We provide examples of resumes tailored to Trauma-Informed and Culturally Responsive Practices to guide you through the process. Take the next step towards your career success today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO