Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Health Insurance Portability and Accountability Act (HIPPA) interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Health Insurance Portability and Accountability Act (HIPPA) Interview
Q 1. What are the three main rules under HIPAA?
HIPAA, the Health Insurance Portability and Accountability Act of 1996, comprises three main rules that work together to protect individuals’ health information: the Privacy Rule, the Security Rule, and the Breach Notification Rule. Think of them as three pillars supporting the overall structure of patient data protection.
- Privacy Rule: Governs the use and disclosure of protected health information (PHI). It dictates who can access PHI and under what circumstances.
- Security Rule: Establishes national standards for securing electronic protected health information (ePHI). This rule focuses on the technical and administrative safeguards needed to protect ePHI from unauthorized access, use, disclosure, disruption, modification, or destruction.
- Breach Notification Rule: Specifies the process for notifying individuals and the government when a breach of unsecured PHI occurs. This ensures transparency and allows for swift remedial action.
Q 2. Explain the Privacy Rule’s requirements for protected health information (PHI).
The Privacy Rule defines protected health information (PHI) as individually identifiable health information held or transmitted by a covered entity or its business associate, in any form or media, whether electronic, paper, or oral. This includes things like names, addresses, medical records, and even payment information related to healthcare. The rule sets strict limits on the use and disclosure of PHI, requiring covered entities to obtain authorization from individuals before using or disclosing their PHI for purposes other than treatment, payment, or healthcare operations (TPO).
For example, a doctor can’t share a patient’s diagnosis with their employer without the patient’s explicit consent, unless it falls under a permitted use or disclosure (like reporting a communicable disease).
Key requirements include:
- Minimum Necessary Standard: Only the minimum amount of PHI necessary to accomplish the intended purpose should be used or disclosed.
- Individual Rights: Individuals have the right to access their PHI, request amendments, request restrictions on certain uses or disclosures, and obtain an accounting of disclosures.
- Administrative Safeguards: Covered entities must implement policies and procedures to comply with the rule, including training staff on privacy practices.
Q 3. Describe the Security Rule’s safeguards for electronic protected health information (ePHI).
The Security Rule safeguards ePHI by mandating the implementation of administrative, physical, and technical safeguards. Imagine it as a three-layered security system protecting digital patient data.
- Administrative Safeguards: These are the policies, procedures, and processes designed to manage the security of ePHI. Examples include security risk analysis, risk management, workforce security (like background checks), and information system activity review.
- Physical Safeguards: These protect the physical location and hardware where ePHI is stored and accessed. Think measures like facility access controls, device and media controls, and environmental controls.
- Technical Safeguards: These involve technology used to protect ePHI. Examples include access control (usernames and passwords), audit controls (tracking who accesses what data), integrity controls (ensuring data hasn’t been tampered with), and encryption (scrambling data to make it unreadable without a key).
For example, a hospital using an electronic health record (EHR) system must implement strong passwords, encrypt sensitive data at rest and in transit, and regularly update its security software to meet the Security Rule’s requirements.
Q 4. What is the role of a designated record set under HIPAA?
A designated record set (DRS) is a group of records maintained by or for a covered entity, which may include medical records, billing records, claims, and other documents related to the provision of healthcare. It’s essentially the collection of documents that constitute an individual’s health information under HIPAA’s purview. Think of it as the complete file on a patient’s care, encompassing various sources of information.
The importance of identifying a DRS lies in defining the scope of information covered under HIPAA regulations. It clarifies what records are subject to access, use, and disclosure limitations under the Privacy Rule.
Q 5. Explain the concept of minimum necessary under HIPAA.
The minimum necessary standard requires covered entities to use, disclose, request, receive, maintain, or otherwise access only the minimum amount of PHI necessary to accomplish the intended purpose of the use, disclosure, request, or receipt. This principle limits the amount of PHI exposed to minimize the risk of unauthorized access or disclosure.
For instance, if a doctor needs to share a patient’s lab results with a specialist, they shouldn’t share the entire medical record; only the relevant lab results should be transmitted. This helps prevent unnecessary exposure of sensitive information.
Q 6. What are the permitted uses and disclosures of PHI without authorization?
HIPAA permits certain uses and disclosures of PHI without individual authorization. These are generally categorized under treatment, payment, and healthcare operations (TPO), as well as other specific exceptions outlined in the Privacy Rule. These exceptions are designed to balance the need for patient privacy with the operational requirements of healthcare and public health.
- Treatment: Sharing information among healthcare providers involved in a patient’s care.
- Payment: Disclosing information to insurance companies to process claims.
- Healthcare Operations: Using information for quality assurance, training, and other administrative functions.
- Public Health: Reporting certain communicable diseases or suspected abuse or neglect.
- Legal Proceedings: Responding to court orders or subpoenas.
- Law Enforcement: Reporting certain crimes or providing information in response to law enforcement requests.
It is critical to remember that even these permitted disclosures must adhere to the minimum necessary standard.
Q 7. Describe the process for obtaining an individual’s authorization for the use or disclosure of PHI.
Obtaining an individual’s authorization for the use or disclosure of PHI involves a formal process ensuring informed consent. The authorization must be in writing and must contain specific information, including:
- A description of the information to be used or disclosed. Be specific. Don’t just say ‘medical records’; specify what types of records are needed.
- The purpose of the use or disclosure. Clearly state why the information is needed.
- The recipient(s) of the information. Identify who will receive the information.
- An expiration date. Set a reasonable time limit.
- A statement that the individual may revoke the authorization at any time. Empower individuals to control their information.
- A statement that the individual’s signature signifies their consent. Make the authorization process clear and transparent.
The authorization must be understandable, and the individual must be given an opportunity to ask questions before signing. Failing to follow these steps can result in a HIPAA violation.
Q 8. What are the penalties for HIPAA violations?
Penalties for HIPAA violations can be severe and vary depending on the nature and extent of the violation, as well as the violator’s knowledge and culpability. They range from relatively minor civil monetary penalties to significant criminal charges.
- Civil Penalties: These are the most common and can reach up to $50,000 per violation, with a maximum of $1.5 million per calendar year for identical violations. The amount depends on factors like whether the violation was intentional or negligent, and whether it resulted in the breach of protected health information (PHI). For example, a clinic accidentally emailing a patient’s medical records to the wrong recipient might face a lower penalty than a deliberate attempt to sell patient data.
- Criminal Penalties: More serious violations, particularly those involving intentional breaches or the knowing misuse of PHI for personal gain, can lead to criminal charges. These can include hefty fines, imprisonment, and even both. Think of a healthcare worker who steals patient data to sell on the black market – this is a criminal offense with serious consequences.
- Corrective Actions: Beyond fines, the Office for Civil Rights (OCR) can require covered entities to implement corrective actions such as improved training, enhanced security measures, and comprehensive audits to prevent future violations. This could involve mandatory staff retraining on HIPAA compliance after an accidental data breach.
It’s crucial to remember that HIPAA compliance is not just about avoiding penalties; it’s about protecting patient privacy and maintaining trust.
Q 9. How does HIPAA address breaches of unsecured PHI?
HIPAA’s response to breaches of unsecured PHI is multifaceted and focuses on timely notification, investigation, and remediation. The process starts with immediate identification of the breach, followed by a thorough investigation to determine its scope and impact.
- Notification: Covered entities and business associates are required to notify affected individuals, the OCR, and in some cases, the media, within specific timeframes. The notification must provide details about the breach, the types of information compromised, and steps individuals can take to mitigate potential harm. This notification is crucial for allowing patients to take proactive measures to protect themselves from potential identity theft or other risks.
- Investigation and Mitigation: A comprehensive investigation is necessary to determine the cause of the breach, the extent of the compromise, and to prevent similar incidents. This involves analyzing systems, reviewing procedures, and interviewing relevant personnel. Corrective actions may include updating security protocols, implementing stricter access controls, or adding more robust data encryption methods.
- Risk Assessment: A key part of HIPAA compliance is conducting regular risk assessments to identify vulnerabilities and develop mitigation strategies. A breach highlights the importance of thorough risk assessments to prevent future incidents and protect sensitive patient data.
The OCR plays a vital role in overseeing breach notification and enforcement, ensuring accountability and driving improvements in data security practices.
Q 10. What is a business associate agreement (BAA) and why is it important?
A Business Associate Agreement (BAA) is a contract between a covered entity (like a hospital or doctor’s office) and a business associate (a third-party vendor) that outlines the responsibilities for protecting PHI. It’s vital because it ensures that the business associate adheres to HIPAA’s privacy and security rules when handling protected health information on behalf of the covered entity. Imagine a hospital using a cloud-based service to store patient records – a BAA ensures that the cloud provider follows HIPAA rules and maintains the privacy and security of the patient data.
- Key Provisions: A BAA typically specifies permitted uses of PHI, security requirements, breach notification procedures, and data disposal methods. It essentially establishes a legally binding agreement on how PHI will be protected throughout the business relationship.
- Importance: Without a BAA, a covered entity might be held liable for a business associate’s HIPAA violations even if they had no direct involvement. The BAA provides a crucial layer of protection for both parties by clearly defining responsibilities and liabilities.
- Example: A medical billing company that receives PHI from a hospital would need a BAA to legally handle that information. Failure to have a BAA could result in significant penalties for both the hospital and the billing company.
Choosing and carefully reviewing BAAs is a critical component of a robust HIPAA compliance program.
Q 11. Explain the difference between a covered entity and a business associate.
The difference between a covered entity and a business associate lies in their relationship to the handling of protected health information (PHI).
- Covered Entity: This is a health plan, healthcare provider, or healthcare clearinghouse that electronically transmits health information. These are the organizations directly responsible for patient care and handling of PHI. Examples include hospitals, doctors’ offices, insurance companies, and pharmacies.
- Business Associate: This is a person or entity that performs certain functions or activities that involve the use or disclosure of PHI on behalf of a covered entity. They don’t directly provide healthcare but support the covered entity in its operations. Examples include medical billing companies, cloud storage providers, legal consultants, and data-processing firms.
The key distinction is that covered entities are directly involved in the provision of healthcare and have direct responsibility for patient information. Business associates are hired to assist but don’t have a direct patient care role. However, both are accountable for complying with HIPAA regulations, the former directly and the latter via the BAA.
Q 12. Describe the requirements for HIPAA compliant data encryption.
HIPAA doesn’t mandate specific encryption methods but requires the implementation of appropriate safeguards to protect electronic PHI (ePHI). The choice of encryption method depends on various factors like the sensitivity of the data, the risk environment, and the technical capabilities of the organization.
- Data at Rest: Encryption is crucial for data stored on servers, hard drives, or other storage devices. This means that the data is unreadable without the decryption key, even if the storage medium is stolen or accessed without authorization. Common methods include AES (Advanced Encryption Standard) with a key length of at least 256 bits.
- Data in Transit: Encryption is also necessary for data transmitted over networks, such as when sending emails or accessing data remotely. HTTPS (with TLS/SSL) is commonly used to encrypt data during transmission.
- Key Management: The security and management of encryption keys are paramount. Robust key management practices are essential to prevent unauthorized access or compromise of the encrypted data. This includes secure key generation, storage, and rotation.
- Other Safeguards: Encryption is only one part of a comprehensive security strategy. Other measures like access controls, audit trails, and intrusion detection systems are also critical to maintaining HIPAA compliance.
The strength of the encryption, the implementation methods and the key management practices are all assessed during a HIPAA risk assessment to determine their suitability.
Q 13. What are the key elements of a HIPAA risk assessment?
A HIPAA risk assessment is a systematic process of identifying vulnerabilities and threats to the confidentiality, integrity, and availability of ePHI. It’s a crucial step in developing a comprehensive security plan. Think of it like a home security audit – you check windows, doors, and alarm systems to identify potential weaknesses before a burglar tries to break in.
- Identify Assets: The first step involves identifying all ePHI and related systems. This includes databases, servers, laptops, mobile devices, and any other locations where ePHI is stored or processed.
- Identify Threats and Vulnerabilities: Next, you identify potential threats (e.g., hacking, malware, insider threats, natural disasters) and vulnerabilities (e.g., weak passwords, outdated software, lack of encryption) that could expose ePHI.
- Assess Risks: This step involves evaluating the likelihood and potential impact of each identified threat. A risk is the combination of a threat, a vulnerability, and the potential impact.
- Implement Safeguards: Based on the risk assessment, appropriate safeguards are implemented to mitigate the identified risks. This could include implementing encryption, access controls, employee training, and incident response plans.
- Monitor and Review: The risk assessment is not a one-time event. It needs to be regularly monitored and reviewed to account for changes in technology, threats, and business processes.
The output of a risk assessment is a prioritized list of risks with recommendations for remediation. This helps organizations focus resources on addressing the most significant threats.
Q 14. How does HIPAA address the use of telehealth and remote patient monitoring?
HIPAA’s approach to telehealth and remote patient monitoring (RPM) acknowledges the increasing use of these technologies while maintaining the need for strong data security and patient privacy. Essentially, the same HIPAA rules that apply to in-person care also apply to telehealth and RPM.
- Security Measures: Covered entities must implement appropriate safeguards to protect ePHI transmitted and stored during telehealth and RPM. This includes strong encryption, secure communication channels, and access controls. Using only HIPAA-compliant platforms and maintaining proper audit trails is crucial.
- Patient Consent: Patients must provide informed consent for telehealth and RPM services, including the use and disclosure of their PHI. This consent should clearly explain how their information will be handled and protected.
- Business Associate Agreements: If a telehealth platform or RPM vendor handles PHI, a BAA is required to ensure the vendor’s compliance with HIPAA regulations.
- Breach Notification: If a breach involving PHI occurs during telehealth or RPM, the covered entity must follow HIPAA’s breach notification rules, promptly notifying affected patients, the OCR, and potentially law enforcement if necessary.
The key takeaway is that the shift towards telehealth does not lessen the importance of HIPAA compliance. In fact, the increased reliance on technology necessitates even more robust security measures to protect patient data.
Q 15. What are the requirements for HIPAA compliance in cloud computing?
HIPAA compliance in cloud computing requires meticulous attention to data security and privacy. Think of it like renting a highly secure apartment for your patient data; you wouldn’t leave the door unlocked, would you? The same principles apply to the cloud.
- Data Encryption: Both data in transit (while traveling over networks) and data at rest (stored on servers) must be encrypted using strong encryption algorithms. This is like using a strong lock on your apartment door and a high-tech safe for valuables.
- Access Control: Implement robust access control measures, including multi-factor authentication (MFA) and role-based access control (RBAC). This is analogous to having a key card system for your apartment building and assigning keys to specific residents based on their needs.
- Business Associate Agreements (BAAs): Cloud providers acting as Business Associates must sign BAAs with covered entities, legally obligating them to comply with HIPAA. This is like a formal contract ensuring your landlord is responsible for the building’s security.
- Data Breach Notification: Establish procedures for promptly notifying OCR and affected individuals in case of a breach. This is your emergency plan in case of a break-in – you need to know what to do and who to contact.
- Risk Assessment and Management: Regularly assess risks and implement appropriate safeguards. This is akin to regularly checking your apartment’s security system and making repairs as needed.
Failing to meet these requirements can lead to severe penalties, including hefty fines and reputational damage. Choosing a cloud provider with strong HIPAA compliance certifications and a proven track record is crucial.
Career Expert Tips:
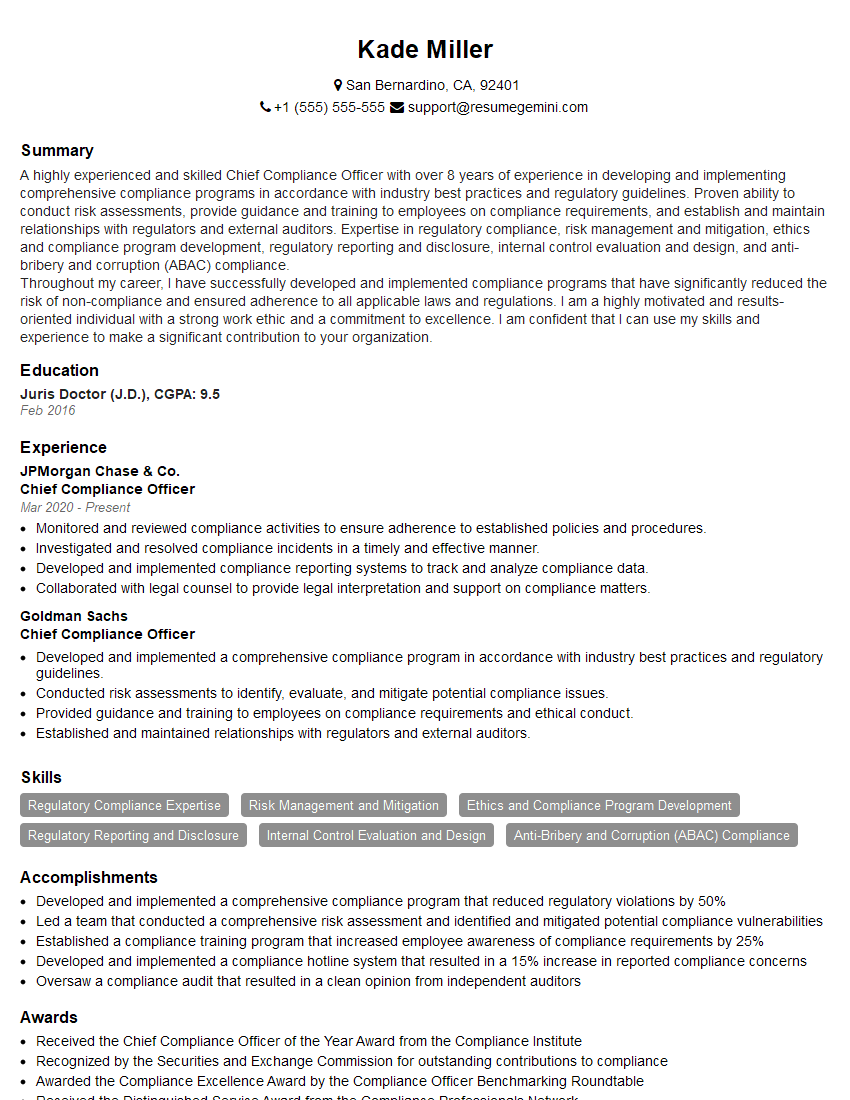
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain the concept of de-identification of PHI.
De-identification of Protected Health Information (PHI) is the process of removing or altering identifying information to render it unidentifiable. Imagine taking a photo and blurring out all the faces – the image is still there, but the individuals are unrecognizable. The goal is to allow the use of health data for research or other purposes without compromising individual privacy.
The HIPAA Privacy Rule specifies methods for de-identification, including the ‘Safe Harbor’ method and the expert determination method. The Safe Harbor method involves removing 18 specific identifiers, such as name, address, and medical record number. The expert determination method allows for other methods if an expert determines there’s minimal risk of re-identification. However, even after de-identification, data should be handled carefully to avoid potential re-identification.
For example, a dataset of patient demographics might be de-identified by removing names and addresses but retaining age and gender. While seemingly safe, this could still potentially be linked to individuals if combined with other datasets containing similar information.
Q 17. What is the role of the Office for Civil Rights (OCR) in enforcing HIPAA?
The Office for Civil Rights (OCR) within the U.S. Department of Health and Human Services (HHS) is the primary enforcement agency for HIPAA. Think of them as the police of the HIPAA world.
The OCR investigates complaints, conducts audits, and enforces compliance through civil monetary penalties, corrective action plans, and other remedies. They ensure covered entities and business associates are adhering to HIPAA regulations and protecting patient privacy. They have the power to impose significant fines for violations, driving accountability within the healthcare industry.
The OCR’s role is essential in maintaining public trust in the healthcare system by ensuring that patient health information is handled responsibly and securely.
Q 18. How do you ensure compliance with the HIPAA Omnibus Rule?
The HIPAA Omnibus Rule significantly broadened the scope of HIPAA, particularly concerning Business Associates. To ensure compliance, organizations must:
- Update BAAs: Ensure all BAAs are updated to reflect the Omnibus Rule’s requirements, particularly regarding breach notification and subcontractors.
- Strengthen Privacy and Security Policies: Implement strong policies and procedures that address all aspects of the Omnibus Rule, including the new provisions on genetic information and breach notification.
- Provide Appropriate Training: Ensure all staff receive comprehensive training on the updated HIPAA regulations.
- Implement Robust Breach Notification Procedures: Establish clear protocols for notifying OCR and affected individuals in the event of a data breach.
- Maintain Detailed Audit Trails: Implement robust logging and auditing to track all access to and changes in PHI.
The Omnibus Rule places greater responsibility on covered entities for the actions of their business associates, highlighting the importance of diligent oversight and contract management.
Q 19. Describe the process for handling a HIPAA complaint.
Handling a HIPAA complaint involves a multi-step process that prioritizes investigation and resolution. Think of it like a formal grievance procedure.
- Complaint Filing: The complaint is filed with the OCR, either online or via mail.
- Investigation: The OCR investigates the complaint, gathering information from the covered entity and the complainant.
- Resolution: Based on the investigation, the OCR may mediate a resolution between the parties, issue a finding of non-compliance, or take enforcement action.
- Enforcement: Enforcement actions can include corrective action plans, financial penalties, and even legal action.
The entire process can be lengthy, and timely documentation and cooperation are key to a favorable outcome for the covered entity.
Q 20. What are the requirements for HIPAA training for healthcare workers?
HIPAA training for healthcare workers must be comprehensive, covering all relevant aspects of the Privacy Rule, Security Rule, and Breach Notification Rule. This training isn’t a one-time event; it’s an ongoing process.
- Regular Training: Training should be provided initially and then updated regularly, particularly after significant regulatory changes or internal policy updates. Think of it like a driver’s license – you need initial training and ongoing refresher courses.
- Content Specificity: Training must be tailored to the employee’s role and responsibilities. A receptionist will have different training needs than a physician.
- Documentation: The training should be documented, including the date, attendees, and the content covered. This serves as proof of compliance.
- Practical Application: Training should incorporate practical scenarios and case studies to reinforce learning. It shouldn’t be just rote memorization; it should be about understanding application.
Failing to provide adequate HIPAA training can leave your organization vulnerable to violations, leading to fines and reputational damage.
Q 21. What is the difference between PHI and PII?
While both PHI and PII relate to personal information, there’s a key distinction. PII (Personally Identifiable Information) is any information that can be used to identify an individual, while PHI is a subset of PII specifically relating to health information. Think of it like this: PII is a broad category, and PHI is a specific type within that category.
PII examples include name, address, social security number, driver’s license number, email address, etc. PHI includes the same information, *plus* medical records, diagnoses, treatment information, insurance details, etc.
All PHI is PII, but not all PII is PHI. For instance, your social security number is PII but not necessarily PHI unless it’s linked to your medical records.
Understanding this difference is crucial for accurate data handling and compliance with relevant regulations, including HIPAA and other privacy laws.
Q 22. Explain the concept of a breach notification under HIPAA.
A HIPAA breach notification is a crucial step in responding to a data breach involving protected health information (PHI). It’s essentially a formal announcement to affected individuals, and in some cases, regulatory agencies, that their PHI has been, or is reasonably believed to have been, compromised. The notification process isn’t triggered by every security incident; it only applies when there’s an unauthorized acquisition, access, use, or disclosure of PHI that compromises the privacy or security of the information.
The notification must include specific details, like the type of PHI involved (e.g., name, address, medical records), the date of the breach, steps individuals can take to mitigate potential harm, and contact information for assistance. The timeline for notification is critical; it’s usually required within 60 days of discovery of the breach, though exceptions exist for cases involving a law enforcement investigation.
For example, imagine a laptop containing patient records is stolen from a healthcare provider’s office. This would trigger a breach notification as PHI has been compromised. The provider would then be obligated to inform affected patients and potentially the Department of Health and Human Services (HHS) depending on the number of individuals affected.
Q 23. How do you address the disposal of PHI and ePHI?
Securely disposing of PHI and electronic PHI (ePHI) is paramount to maintaining HIPAA compliance. It’s not enough to simply delete files; a robust disposal process is needed to prevent unauthorized access to sensitive information. For paper-based PHI, methods such as shredding or incineration are recommended, ensuring the information is rendered irretrievable. For ePHI, secure deletion methods are crucial, often involving multiple passes of data overwriting to prevent data recovery.
Furthermore, hardware containing ePHI should also be handled carefully. Hard drives and other storage devices should be physically destroyed or securely wiped before disposal. This might involve using specialized data destruction services that provide certification of complete data eradication. It’s also vital to have a documented disposal policy that outlines the approved procedures and ensures staff are properly trained on these processes. For example, our clinic uses a certified vendor for hard drive destruction and maintains a log of all disposal activities.
Q 24. What are your strategies for maintaining HIPAA compliance in your workplace?
Maintaining HIPAA compliance is an ongoing process, not a one-time event. My strategies center around several key pillars:
- Comprehensive Training: Regular, mandatory training for all staff on HIPAA regulations, security best practices, and privacy policies. This includes understanding the consequences of non-compliance.
- Strong Security Measures: Implementing robust physical, technical, and administrative safeguards. This encompasses access controls, encryption, firewall protection, regular security audits, and incident response planning. We utilise multi-factor authentication and regular security updates across all devices.
- Strict Access Control: Implementing the principle of least privilege – ensuring employees only have access to the PHI absolutely necessary for their job functions. We utilize role-based access controls (RBAC) to manage this effectively.
- Data Breach Response Plan: Developing and regularly testing a comprehensive data breach response plan to quickly and effectively address potential breaches. This plan includes notification procedures and coordination with regulatory agencies.
- Risk Assessment & Mitigation: Regularly assessing potential risks to PHI and implementing measures to mitigate those risks. We use a risk assessment framework to identify and address vulnerabilities.
- Regular Audits and Monitoring: Conducting regular internal audits and external reviews to ensure ongoing compliance and identify areas for improvement.
Q 25. Describe a time you had to deal with a HIPAA violation or potential violation.
In a previous role, we discovered a potential HIPAA violation involving a misplaced USB drive containing patient data. The drive contained PHI and was not encrypted. Following our incident response plan, we immediately initiated an investigation. We determined who last had possession of the drive and searched the premises. Fortunately, we recovered the drive before it could be accessed by unauthorized individuals.
We immediately implemented corrective actions, including mandatory encryption of all portable storage devices and refresher training on data security protocols for all staff. We also conducted a thorough review of our existing security policies and procedures to identify any weaknesses and enhance our safeguards further. This incident reinforced the importance of proactive security measures and rigorous adherence to established protocols.
Q 26. How do you balance patient privacy with the need to share information for care coordination?
Balancing patient privacy with the need for information sharing for care coordination requires a delicate approach. The key is to adhere to the minimum necessary standard. This means only sharing the minimum amount of PHI necessary to achieve the specific purpose of care coordination. For instance, when consulting with another provider, only the relevant medical information needed to facilitate appropriate treatment should be shared.
Methods like secure messaging platforms, encrypted email, and designated health information exchanges (HIEs) can facilitate secure information sharing while maintaining patient confidentiality. Before sharing any PHI, explicit patient consent should be obtained whenever possible, or when legally required. Detailed documentation is also crucial, outlining the reason for sharing information and the parties involved. This ensures a clear audit trail and demonstrates compliance with HIPAA guidelines.
Q 27. What resources do you use to stay up-to-date on HIPAA regulations?
Staying updated on HIPAA regulations is crucial for maintaining compliance. I utilize several resources, including:
- The HHS website: The official source for HIPAA regulations, guidance documents, and updates.
- Professional organizations: Organizations such as the American Health Information Management Association (AHIMA) and the Healthcare Information and Management Systems Society (HIMSS) provide resources, publications, and continuing education opportunities related to HIPAA compliance.
- HIPAA compliance software and services: Many vendors offer software and services designed to assist with compliance, including training modules and audit tools.
- Legal counsel specializing in healthcare law: Consulting with legal experts helps to navigate complex issues and ensure adherence to all relevant laws and regulations.
- Industry publications and journals: Staying abreast of current events and emerging challenges through relevant publications.
Q 28. Explain the importance of incident response planning for HIPAA compliance.
An incident response plan is crucial for HIPAA compliance because it outlines the procedures to follow in the event of a data breach or other security incident. A well-defined plan minimizes the impact of a breach, facilitates a timely response, and aids in demonstrating compliance with regulatory requirements. This plan should include steps for containment, eradication, recovery, and notification, as well as a communication strategy for stakeholders.
For example, the plan should detail how to identify and contain a breach, isolate affected systems, assess the extent of the damage, recover data, notify affected individuals and authorities, and conduct a post-incident review to identify vulnerabilities and prevent future breaches. Regular testing and training of the incident response plan are vital to ensure effectiveness. This preparedness is essential not only for protecting patient data but also for demonstrating a commitment to compliance and minimizing potential penalties and legal liabilities.
Key Topics to Learn for a Health Insurance Portability and Accountability Act (HIPAA) Interview
- HIPAA Privacy Rule: Understand the core principles of protecting patient health information (PHI), including permitted uses and disclosures, patient rights (access, amendment, accounting of disclosures), and the concept of minimum necessary.
- HIPAA Security Rule: Learn about administrative, physical, and technical safeguards organizations must implement to ensure the confidentiality, integrity, and availability of e-PHI. Consider practical applications like risk analysis and incident response planning.
- HIPAA Breach Notification Rule: Familiarize yourself with the procedures for identifying, responding to, and reporting breaches of unsecured PHI. Think about how to analyze a potential breach scenario and determine appropriate actions.
- HIPAA Enforcement and Penalties: Understand the potential consequences of HIPAA violations, including civil and criminal penalties. Consider how to navigate compliance challenges and avoid potential risks.
- Business Associate Agreements (BAAs): Learn the importance of BAAs in managing the flow of PHI between covered entities and their business associates. Understand the responsibilities of both parties.
- Covered Entities and Business Associates: Clearly define who constitutes a covered entity and a business associate under HIPAA regulations and the implications for each.
- Patient Rights and Responsibilities: Understand the rights afforded to patients under HIPAA, including the right to access, amend, and request restrictions on their PHI. This includes understanding how to properly handle patient requests.
Next Steps
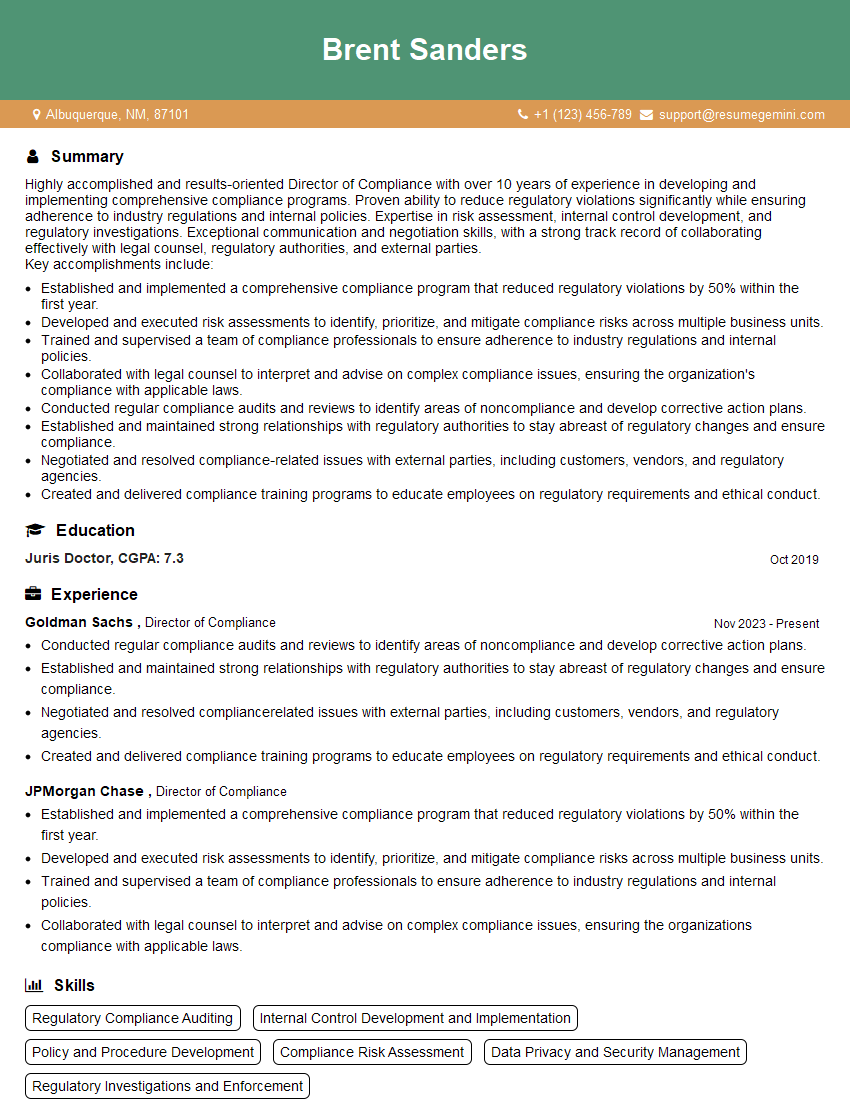
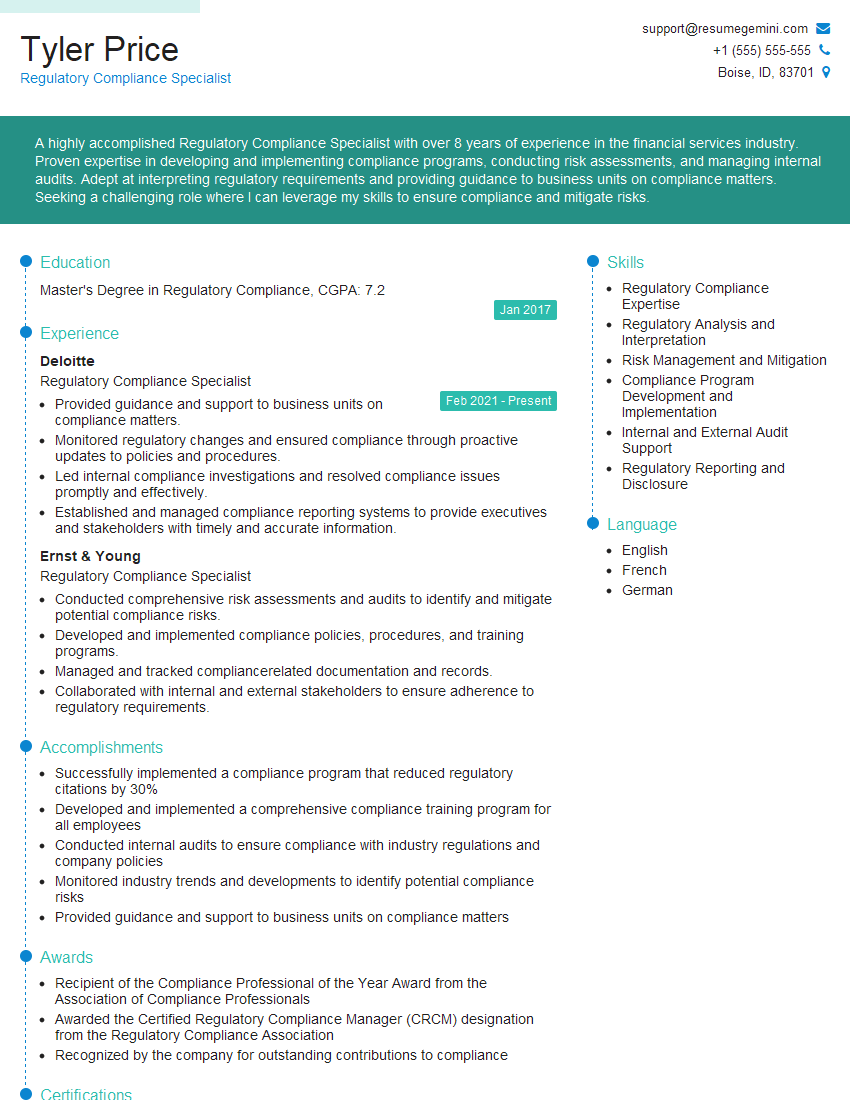
Mastering HIPAA is crucial for career advancement in healthcare and related fields. A strong understanding of these regulations demonstrates your commitment to patient privacy and data security, making you a highly valuable asset to any organization. To significantly boost your job prospects, create an ATS-friendly resume that highlights your HIPAA knowledge and relevant experience. We recommend using ResumeGemini to build a professional and effective resume. ResumeGemini offers valuable resources and even provides examples of resumes tailored to HIPAA-related roles, helping you present your skills and experience in the best possible light.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO