Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Grief Counseling Experience interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Grief Counseling Experience Interview
Q 1. Describe your experience working with individuals experiencing different types of grief.
My experience spans a wide range of grief types, from bereavement following the death of a loved one – encompassing sudden deaths like accidents, anticipated deaths like long-term illnesses, and ambiguous losses like a missing person – to the grief associated with other significant losses such as divorce, job loss, or the end of a long-term relationship. I’ve worked with individuals grappling with disenfranchised grief, where their loss is not socially acknowledged or validated, such as the loss of a pet or a miscarriage. Each presents unique challenges and requires a tailored approach. For example, the intense shock and disbelief often seen in sudden death requires a different therapeutic strategy compared to the gradual acceptance often seen with a long-term illness. I adapt my approach to meet the individual’s specific needs and cultural context.
I remember one client who experienced the sudden loss of her husband in a car accident. Her grief was characterized by intense anger and disbelief, coupled with significant sleep disturbances. This contrasted sharply with another client who had cared for her aging mother for several years before her passing. While sadness was present, her grief was more centered around acceptance and reflection on their shared memories.
Q 2. Explain your approach to assessing the needs of grieving clients.
My assessment approach is holistic and client-centered. It begins with building rapport and creating a safe space for open communication. I use a combination of methods, including open-ended questioning, active listening, and observing nonverbal cues to understand the client’s individual experience. I assess the intensity, duration, and impact of their grief on their daily life. This involves exploring their emotional, physical, social, and spiritual well-being. I delve into their coping mechanisms and support systems, identifying both strengths and areas where additional support is needed. Standardized assessments, such as grief scales, might be employed to provide an objective measure of grief intensity, but they are always supplemented by a rich qualitative understanding of the individual’s narrative.
For instance, I might ask questions like, “Can you describe your relationship with the person you lost?” or “How has this loss affected your sleep, appetite, or daily activities?” The goal is not just to diagnose but to truly understand the individual’s unique journey through grief and identify the most appropriate interventions.
Q 3. How do you differentiate between normal grief and complicated grief?
Normal grief, while intensely painful, is characterized by a gradual process of healing. Emotions fluctuate, but generally decrease in intensity over time. Individuals eventually regain their ability to function in daily life and find meaning in their experiences. Complicated grief, on the other hand, is persistent and debilitating. It’s characterized by an intense and prolonged yearning for the deceased, an inability to accept the loss, and significant impairment in daily functioning for an extended period (typically over 6 months). Symptoms may include intrusive thoughts, avoidance of reminders of the loss, or significant identity disruption. The key differentiator lies in the duration and intensity of the symptoms and their impact on the individual’s ability to cope and move forward.
For example, feeling sadness for months after a loss is normal, but if that sadness is accompanied by debilitating anxiety, an inability to work, or persistent thoughts of self-harm, it may indicate complicated grief requiring professional intervention.
Q 4. What therapeutic modalities are you proficient in using with grieving clients?
My therapeutic toolbox includes several evidence-based modalities. I’m proficient in Cognitive Behavioral Therapy (CBT), which helps clients identify and challenge unhelpful thought patterns and behaviors related to their grief. Acceptance and Commitment Therapy (ACT) assists clients in accepting difficult emotions and focusing on values-based actions. Narrative Therapy helps clients reframe their grief story and find new meaning in their experiences. I also incorporate mindfulness techniques to help clients manage intense emotions and improve self-awareness. The specific modality or combination of modalities employed depends on the individual’s needs and preferences.
For instance, CBT might be particularly useful for a client struggling with excessive rumination, while ACT might be more beneficial for a client who is avoiding social interactions due to their grief.
Q 5. How do you address the unique needs of grieving children or adolescents?
Working with grieving children and adolescents requires a developmentally sensitive approach. Understanding their cognitive and emotional capacity is crucial. Play therapy is often effective with younger children, allowing them to express their feelings through creative means. For adolescents, I might use expressive arts therapies, or engage in conversations that validate their feelings and experiences. It’s essential to create a safe and non-judgmental space where they feel comfortable expressing their emotions without feeling pressured. Working collaboratively with parents or guardians is also crucial to ensure a consistent and supportive environment.
For example, a young child might express their grief through drawing or playing with dolls, while an adolescent might prefer talking about their feelings or writing poetry.
Q 6. Describe your experience facilitating group grief support sessions.
Facilitating group grief support sessions offers a unique opportunity for shared healing and mutual support. I create a structured yet flexible environment where participants feel safe to share their experiences without judgment. I emphasize active listening, empathy, and respect for individual differences. The sessions often incorporate activities that promote emotional expression, such as journaling, sharing stories, or creative arts. I provide guidance and structure, but also empower participants to support one another. Confidentiality is paramount, and I ensure all group members understand and adhere to the group’s rules and boundaries.
A typical session might begin with a check-in, followed by a guided activity, and conclude with a summary and planning for the next meeting. The focus is on creating a community of support and fostering hope amidst grief.
Q 7. How do you handle ethical dilemmas that might arise in grief counseling?
Ethical dilemmas in grief counseling can arise in several ways. Maintaining client confidentiality is paramount, except in situations where there is a risk of harm to the client or others. Boundary issues, such as dual relationships or managing personal feelings about the client’s loss, need careful attention. Cultural sensitivity and ensuring equitable access to services are also crucial ethical considerations. I address these dilemmas by referring to relevant ethical codes, seeking consultation from supervisors or colleagues, and carefully documenting my decision-making process. Transparency and open communication with clients are key to maintaining trust and navigating ethical complexities.
For example, if a client expresses suicidal ideation, I have an ethical obligation to take appropriate steps to ensure their safety, which might involve contacting emergency services or hospitalizing them if necessary. This action, though potentially disruptive to the therapeutic relationship, prioritizes the client’s well-being.
Q 8. What is your approach to supporting clients dealing with traumatic loss?
My approach to supporting clients dealing with traumatic loss is grounded in a trauma-informed lens, recognizing that grief following trauma is often more complex and intense. I prioritize building a safe and trusting therapeutic relationship, emphasizing validation and empathy. We begin by acknowledging the reality of their experience, validating the intensity of their emotions, and avoiding pressure to ‘move on’. My therapeutic techniques include:
- Trauma-focused Cognitive Behavioral Therapy (CBT): Helping clients identify and challenge unhelpful thoughts and beliefs related to the trauma and loss.
- Eye Movement Desensitization and Reprocessing (EMDR): A valuable tool for processing traumatic memories and reducing their emotional impact.
- Somatic Experiencing (SE): Focusing on body awareness and releasing trauma stored in the body, as trauma often manifests physically.
- Narrative Therapy: Helping clients rewrite their stories around the trauma, empowering them to reclaim their narratives.
For example, a client who lost a loved one in a car accident might experience intense flashbacks and nightmares. We would work together to process these experiences, develop coping skills for managing triggers, and rebuild a sense of safety and security.
Q 9. How do you help clients develop healthy coping mechanisms for grief?
Helping clients develop healthy coping mechanisms is a crucial aspect of grief counseling. It’s about equipping them with tools to navigate the emotional rollercoaster of grief, rather than suppressing or avoiding their feelings. My strategies involve:
- Mindfulness and Meditation: Teaching techniques to ground themselves in the present moment, reducing anxiety and rumination.
- Journaling: Providing a safe space for expressing emotions and processing thoughts related to the loss.
- Physical Activity: Encouraging exercise as a healthy outlet for stress and emotional release.
- Social Support: Connecting clients with support groups or encouraging them to lean on their existing support networks.
- Creative Expression: Utilizing art, music, or other creative outlets to process grief.
For instance, a client might find journaling helpful to articulate their feelings of anger or sadness. We would then explore ways to manage those emotions constructively, perhaps through mindful breathing exercises or engaging in a physical activity like walking.
Q 10. Describe your experience working with diverse populations experiencing grief.
My experience encompasses working with diverse populations, understanding that grief manifests differently across cultures, ethnicities, and socioeconomic backgrounds. I’m acutely aware of the cultural nuances surrounding death and bereavement. For example, some cultures emphasize public displays of mourning, while others prefer more private expressions. My approach involves:
- Cultural Sensitivity: Adapting my therapeutic approach to respect and accommodate clients’ unique cultural backgrounds and beliefs.
- Acknowledging Systemic Factors: Recognizing how social inequalities, such as racism or poverty, can exacerbate the impact of grief.
- Collaboration with Community Resources: Connecting clients with culturally specific support services when appropriate.
I’ve worked with clients from various backgrounds, including immigrant communities facing unique challenges related to loss and separation from their home countries, and individuals from marginalized groups navigating systemic barriers to accessing grief support. Understanding these diverse perspectives enriches my practice and allows me to tailor my support to the individual’s needs.
Q 11. How do you address the spiritual or religious beliefs of grieving clients?
Spiritual and religious beliefs often play a significant role in how individuals cope with grief. My approach is one of respect and understanding, not imposing my own beliefs. I strive to create a space where clients feel comfortable exploring the intersection of their faith and their grief. This might involve:
- Active Listening: Carefully listening to how their faith shapes their understanding of death and the afterlife.
- Collaboration with Clergy: Working collaboratively with religious leaders, if the client desires, to integrate their faith into the healing process.
- Respectful Inquiry: Gently exploring how their beliefs provide comfort or challenge during this difficult time.
For instance, a client might find solace in prayer or religious rituals. We would explore how these practices can offer comfort and support while navigating their grief. I would never attempt to dissuade or impose my own views on their beliefs.
Q 12. How do you manage your own emotional well-being when working with grieving individuals?
Managing my own emotional well-being is paramount in this demanding profession. Compassion fatigue and vicarious trauma are real risks. My self-care strategies include:
- Supervision: Regular consultation with a supervisor to process challenging cases and maintain professional boundaries.
- Self-Reflection: Journaling or engaging in mindful practices to process my own emotions and experiences.
- Personal Therapy: Utilizing personal therapy to maintain my own mental health and well-being.
- Healthy Boundaries: Setting clear professional boundaries to prevent emotional burnout.
- Support Network: Maintaining strong relationships with colleagues, friends, and family.
It’s vital to recognize that caring for others’ emotional well-being requires taking care of my own. Neglecting this crucial aspect can lead to burnout and ultimately compromise the quality of care I can provide to my clients.
Q 13. What are the warning signs of complicated grief, and how do you intervene?
Complicated grief is characterized by prolonged and intense grief that significantly impairs daily functioning. Warning signs include:
- Intense yearning or longing for the deceased that interferes with daily life.
- Difficulty accepting the death.
- Numbness or detachment.
- Intrusive thoughts or memories of the deceased.
- Avoidance of reminders of the deceased.
- Significant impairment in social, occupational, or other areas of functioning.
Intervention involves a multifaceted approach, often requiring specialized therapeutic techniques such as:
- Cognitive Processing Therapy (CPT): Addressing maladaptive thoughts and beliefs.
- Exposure Therapy: Gradually confronting reminders of the loss.
- Grief Therapy Groups: Connecting with others experiencing similar challenges.
- Medication: In some cases, medication may be helpful in managing symptoms of anxiety or depression.
Early intervention is crucial to prevent complicated grief from becoming chronic. If I observe these warning signs, I would engage in a thorough assessment, discuss treatment options with the client, and potentially collaborate with other professionals.
Q 14. How do you collaborate with other professionals (doctors, clergy, family) in providing grief support?
Collaboration is vital in providing holistic grief support. I regularly collaborate with various professionals, including:
- Physicians: To address any underlying medical or physical health issues that might be contributing to the client’s grief.
- Clergy: To integrate the client’s spiritual beliefs into the healing process, with the client’s consent.
- Family Members: To offer support and guidance to the family unit as a whole, ensuring everyone has the necessary resources.
- Other Therapists: Referring clients to specialists, such as trauma therapists or psychiatrists, as needed.
Effective communication and shared goals are essential for successful collaboration. I maintain open lines of communication with all involved parties, ensuring everyone is informed and working towards the client’s best interests. This collaborative approach provides comprehensive support, addressing the various dimensions of grief.
Q 15. Describe a challenging case involving grief counseling and how you approached it.
One of the most challenging cases I encountered involved a young widow, Sarah, who lost her husband unexpectedly in a car accident. She was struggling intensely with survivor’s guilt, compounded by feelings of intense anger and betrayal towards fate. Her grief manifested as both profound sadness and unpredictable outbursts of rage. Initially, she was resistant to therapy, expressing disbelief that anyone could understand her pain.
My approach involved building a strong therapeutic alliance based on empathy and unconditional positive regard. I actively listened to her pain, validating her feelings without judgment. We started with exploring her relationship with her husband, focusing on the positive memories and celebrating their life together. This helped create a safe space where she could express her anger without feeling judged. Gradually, we incorporated coping mechanisms like mindfulness exercises and journaling to manage her intense emotions. We also explored the concept of survivor’s guilt and reframed her experience in a way that emphasized her resilience and strength. Over time, Sarah began to accept her grief, move towards healing, and even find some small moments of joy and hope.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your understanding of the grief process and its various stages.
The grief process is a deeply personal and complex journey, not a linear progression through stages as sometimes portrayed. While models like Kübler-Ross’s five stages (denial, anger, bargaining, depression, acceptance) provide a framework, they don’t capture the nuanced individual experiences. Grief can manifest in various ways, including physical symptoms, emotional turmoil, behavioral changes, and cognitive difficulties.
Instead of rigid stages, I prefer to view grief as a process with fluctuating intensity and diverse expressions. It’s characterized by waves of emotion – intense sadness, anger, guilt, anxiety – punctuated by periods of relative calm. The individual’s journey is shaped by their personality, the nature of the loss, their support system, and cultural factors. For example, some individuals may experience prolonged grief disorder, a persistent and debilitating form of grief. Understanding the complexity of this process is crucial for effective intervention.
Q 17. How do you tailor your therapeutic approach to the specific needs of each client?
Tailoring my approach hinges on a thorough assessment of the client’s unique needs and circumstances. This begins with active listening and creating a safe, non-judgmental space. I use a variety of therapeutic modalities, selecting those most appropriate for each individual. For instance, cognitive behavioral therapy (CBT) can be effective in addressing maladaptive thought patterns contributing to prolonged grief. Mindfulness-based interventions can help manage overwhelming emotions. Narrative therapy can empower clients to reframe their stories and find meaning in their loss. Sometimes, a psychodynamic approach is necessary to explore unconscious conflicts related to grief. Throughout the process, I regularly reassess the client’s progress and adapt my strategies accordingly, prioritizing their comfort and agency.
For example, a client struggling with intense guilt might benefit from exploring the roots of this feeling through narrative therapy, while a client experiencing debilitating anxiety might find relief through mindfulness and relaxation techniques. Regular check-ins and collaboration ensure that the therapeutic plan remains relevant and effective.
Q 18. What is your familiarity with different grief models (e.g., Kubler-Ross, Worden)?
I’m familiar with several grief models, including Kübler-Ross’s five stages and Worden’s four tasks of mourning. While Kübler-Ross’s model offers a general framework, its linear nature is a significant limitation. Worden’s model, focusing on accepting the reality of the loss, processing the pain of grief, adjusting to the environment without the deceased, and emotionally relocating the deceased and moving on with life, offers a more nuanced perspective and is often more helpful in guiding therapy. However, I find that integrating elements from multiple models offers the most comprehensive approach. I don’t adhere rigidly to any single model, preferring instead to utilize aspects that align with the client’s unique experience and needs. Other valuable models I consider include the dual process model, emphasizing the oscillation between loss-oriented and restoration-oriented coping, and the attachment-based model, highlighting the role of attachment in shaping grief responses.
Q 19. How do you assess a client’s risk for suicide or self-harm when dealing with grief?
Assessing suicide risk is a crucial part of grief counseling. I utilize a comprehensive approach that includes direct questioning about suicidal thoughts and plans, assessing hopelessness and helplessness, evaluating access to lethal means, and exploring the client’s overall mental state. The Columbia-Suicide Severity Rating Scale (C-SSRS) is a helpful tool in this assessment. I also pay close attention to subtle indicators, such as changes in sleep patterns, appetite, and social withdrawal. Any expression of self-harm or suicidal ideation necessitates immediate intervention, which may include hospitalization, involving family members, and collaborating with other professionals like psychiatrists. Building a strong therapeutic alliance fosters open communication, enabling early identification and management of these serious risks.
Q 20. What resources and referrals do you typically utilize to support grieving clients?
Supporting grieving clients often requires collaboration with other professionals and resources. This may include referrals to psychiatrists for medication management, support groups tailored to specific losses (e.g., grief groups for parents who have lost children), clergy members for spiritual guidance, and social workers for practical assistance with navigating bureaucratic hurdles. I frequently utilize online resources providing information and support, such as grief helplines and websites offering self-help materials. Community resources like hospice organizations and palliative care services can also provide vital assistance. The specific referrals depend on the client’s individual needs and preferences. My goal is to create a holistic support network to aid the healing process.
Q 21. Describe your experience documenting client progress and maintaining confidentiality.
Accurate and ethical documentation is essential. I maintain detailed session notes that adhere to HIPAA regulations and professional guidelines. These notes include the client’s presentation, key discussion points, treatment plans, interventions utilized, and progress observed. Progress is documented regularly using both qualitative and quantitative measures, such as standardized assessment tools to monitor changes in mood, symptoms, and functioning. Confidentiality is paramount. All client information is protected, ensuring that it is only accessed by authorized individuals, and all electronic records are stored securely with appropriate password protection. I regularly review my documentation practices to ensure compliance with all relevant laws and ethical codes.
Q 22. How do you address cultural differences in the experience of grief and loss?
Grief is a deeply personal experience, and its expression varies significantly across cultures. Addressing cultural differences is paramount to providing effective grief counseling. My approach begins with acknowledging that there’s no single ‘right’ way to grieve. I start by actively listening to my clients, understanding their cultural background, and learning about their traditions surrounding death and mourning. This includes exploring their beliefs about the afterlife, acceptable expressions of grief (e.g., outward displays of emotion vs. stoicism), and the roles of family and community in the grieving process.
For example, in some cultures, public displays of intense grief are expected and even encouraged, while in others, quieter, more private mourning is the norm. Understanding these nuances helps me tailor my approach to avoid inadvertently causing distress. I might ask open-ended questions like, “Can you tell me about how your family and community typically handle loss?” or “What are some of the traditions or rituals you are planning or participating in?” This information guides my interventions and ensures I’m respectful of their cultural values and beliefs.
Beyond direct questioning, I rely on cultural sensitivity training and continuing education to deepen my understanding of various cultural perspectives on grief. I strive to be a lifelong learner in this area, recognizing that cultural competence is an ongoing process.
Q 23. What are your strategies for helping clients process unresolved trauma related to loss?
Unresolved trauma related to loss can significantly complicate the grieving process. My strategies focus on creating a safe and trusting therapeutic relationship where clients feel empowered to explore their pain without judgment. This often involves techniques from Trauma-Informed Care, including a careful assessment of the client’s history of trauma and the nature of the loss. I avoid pressuring clients to disclose trauma if they are not ready. Instead, I focus on building rapport and creating a collaborative environment.
Once a level of trust is established, I might incorporate techniques like EMDR (Eye Movement Desensitization and Reprocessing) or somatic experiencing, which address the body’s memory of traumatic events. Cognitive Behavioral Therapy (CBT) can help clients challenge negative thought patterns and develop healthier coping mechanisms. Narrative therapy can be helpful in reconstructing the client’s story around the loss and trauma, allowing them to find agency in their narrative.
For example, a client struggling with the death of a loved one due to a violent crime might need help processing the trauma surrounding the crime itself, in addition to grieving the loss. A phased approach, starting with building safety and stability, then carefully exploring the trauma, and finally working on grief, is essential. Throughout this process, collaboration and client autonomy are crucial. The client is the expert on their own experience.
Q 24. How do you maintain professional boundaries while providing compassionate care?
Maintaining professional boundaries while providing compassionate care is a delicate balance. It requires constant self-reflection and a commitment to ethical practice. Key aspects include setting clear boundaries around time, communication (e.g., responding to emails or calls within a specific timeframe), and the nature of the therapeutic relationship. I ensure clients understand the parameters of our sessions and the limitations of my role.
Avoiding dual relationships is critical. This means refraining from social interactions outside of therapy sessions, and disclosing any potential conflicts of interest upfront. I also prioritize self-care to prevent burnout, as emotional exhaustion can blur boundaries. This includes maintaining a healthy work-life balance, seeking supervision, and engaging in regular self-reflection to monitor my emotional well-being.
For example, I would avoid accepting gifts from clients, except perhaps a small token of appreciation at the conclusion of therapy, and always address any potential boundary crossings immediately and professionally. Regular supervision and continuing education help me stay informed about best practices in ethical conduct.
Q 25. Explain your understanding of the impact of grief on physical and mental health.
Grief significantly impacts both physical and mental health. The emotional toll of loss can manifest physically through symptoms such as fatigue, sleep disturbances, changes in appetite, weakened immune system, and even cardiovascular problems. Mentally, individuals may experience intense sadness, anger, anxiety, guilt, and difficulty concentrating. They might also develop depression, anxiety disorders, or PTSD (Post-Traumatic Stress Disorder), particularly if the loss was sudden or traumatic.
The intensity and duration of these effects vary greatly depending on individual factors, such as the nature of the relationship with the deceased, the circumstances of the death, access to support systems, and pre-existing mental health conditions. It is important to note that prolonged or debilitating symptoms might indicate a need for professional intervention, beyond grief counseling alone. Referrals to medical doctors or psychiatrists might be necessary for physical or mental health concerns.
Imagine a client who lost their spouse unexpectedly. They might experience insomnia, chest pains, and significant weight loss in addition to intense sadness and feelings of isolation. Understanding this connection between physical and mental health allows me to offer holistic support and recommend appropriate referrals when needed.
Q 26. What are your methods for assisting clients in finding meaning and hope after loss?
Helping clients find meaning and hope after loss is a central goal in grief counseling. This process is unique to each individual and often involves exploring their values, beliefs, and personal narratives. I encourage clients to reflect on the positive aspects of their relationship with the deceased and to identify ways to honor their memory. This can involve creating memorials, sharing stories, or engaging in activities the deceased loved.
Techniques such as reminiscence therapy and narrative therapy can facilitate this exploration. I also help clients identify their strengths, resilience, and resources within their support network. This might involve encouraging them to reconnect with friends and family or to seek out support groups. It’s crucial to acknowledge the pain and validate their feelings without rushing the healing process. Finding meaning isn’t about magically erasing the pain, but about integrating the loss into a revised life narrative.
For instance, a client grieving the loss of a parent might find meaning by carrying on the parent’s legacy by volunteering at a similar organization or by sharing stories and photos to keep the memory alive. The focus is on finding ways to move forward while honoring their past.
Q 27. How do you measure the effectiveness of your grief counseling interventions?
Measuring the effectiveness of grief counseling interventions requires a multifaceted approach. I use a combination of methods, including standardized outcome measures, qualitative feedback, and ongoing assessment of the client’s progress. Standardized questionnaires, such as the Texas Revised Inventory of Grief (TRIG), can track changes in grief symptoms over time. These provide objective data on the client’s emotional and psychological state.
In addition to quantitative data, I regularly assess the client’s subjective experiences through open-ended questions and reflective listening during sessions. This provides valuable insight into their progress, challenges, and overall well-being. Tracking significant milestones, such as the ability to engage in daily activities, improvements in sleep patterns, and shifts in emotional regulation, are also key indicators. Regular supervision provides another lens for reviewing progress and refining strategies.
For instance, I might use a standardized grief inventory at the start and end of therapy to quantify changes in symptom severity. I would also rely on qualitative feedback from the client about their experience and their perception of progress. This combined approach offers a more comprehensive understanding of the effectiveness of the interventions.
Q 28. Describe your experience with crisis intervention related to grief and loss.
Crisis intervention related to grief and loss often involves working with individuals experiencing acute distress following a sudden or traumatic loss. My approach prioritizes immediate stabilization and support. This might involve helping the client regulate their emotions, access immediate resources such as family or friends, and develop short-term coping strategies. The focus is on ensuring their safety and preventing immediate harm to themselves or others.
Depending on the circumstances, this might involve collaboration with emergency services, hospital staff, or other professionals. In these acute situations, practical support is often essential, such as assisting with funeral arrangements or connecting the client with financial or housing assistance if needed. The initial phase involves assessing the immediate risks and providing emotional first aid. Longer-term therapeutic work can begin once the individual is stabilized.
For example, if a client calls expressing suicidal ideation following the unexpected death of a loved one, my immediate priority is to assess the level of risk and ensure their safety. This might involve contacting emergency services, activating a crisis response team, or hospitalizing the client if necessary. Subsequent sessions would then focus on providing emotional support, exploring coping strategies, and developing a safety plan.
Key Topics to Learn for Grief Counseling Experience Interview
- Understanding Grief Theories: Familiarize yourself with various models of grief (Kubler-Ross, Bowlby, etc.) and their implications for therapeutic approaches.
- Practical Application: Develop examples demonstrating your ability to apply these theories in real-world scenarios. Consider how you’ve helped clients navigate different stages of grief and identified their unique needs.
- Ethical Considerations: Explore ethical dilemmas specific to grief counseling, such as maintaining client confidentiality and setting appropriate boundaries.
- Trauma-Informed Care: Understand how past trauma can impact grief and how to integrate trauma-informed practices into your counseling approach.
- Cultural Sensitivity: Recognize the diverse ways grief is experienced across different cultures and how to adapt your approach accordingly.
- Group and Family Counseling: Explore your experience (if any) in facilitating grief support groups or working with families experiencing loss.
- Crisis Intervention: Discuss your skills in providing immediate support to individuals experiencing acute grief or crisis.
- Assessment and Treatment Planning: Demonstrate your ability to conduct thorough assessments and develop individualized treatment plans tailored to the specific needs of grieving clients.
- Case Management: Describe your experience in coordinating care with other professionals, such as medical doctors, social workers, or clergy.
- Self-Care and Burnout Prevention: Showcase your understanding of the importance of self-care and strategies for preventing burnout in the demanding field of grief counseling.
Next Steps
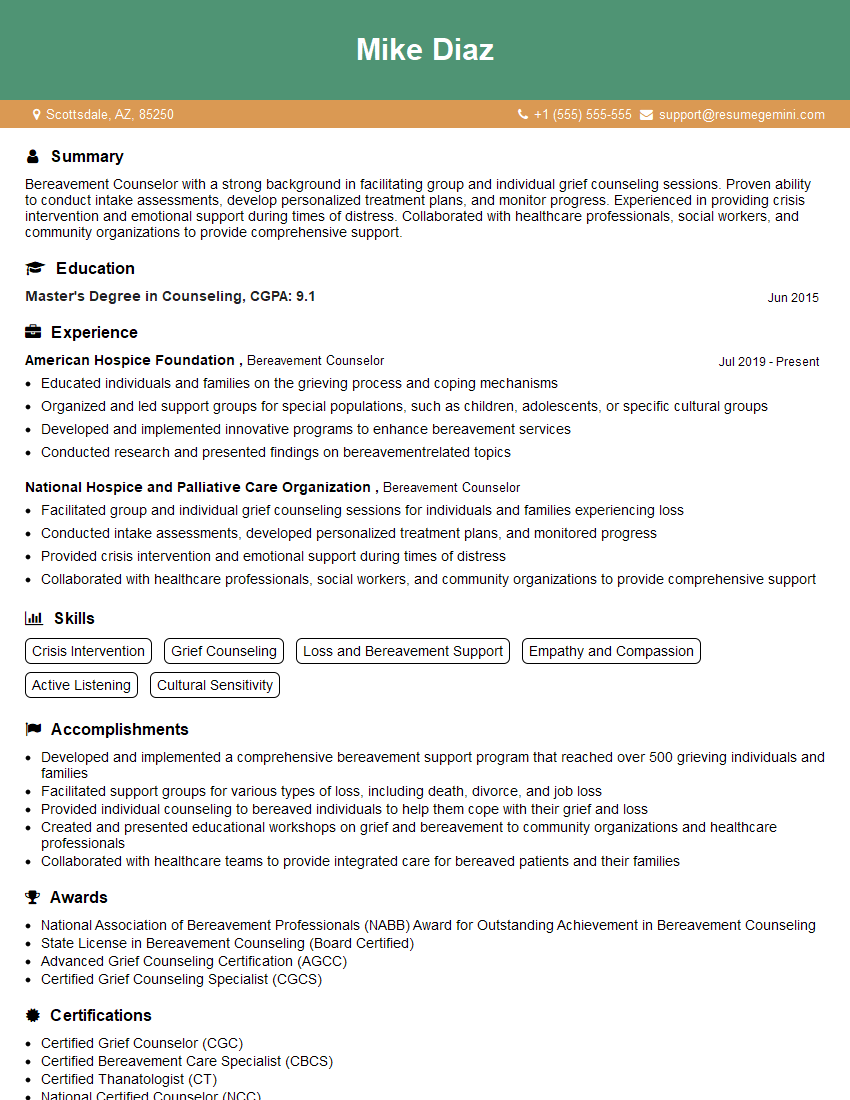
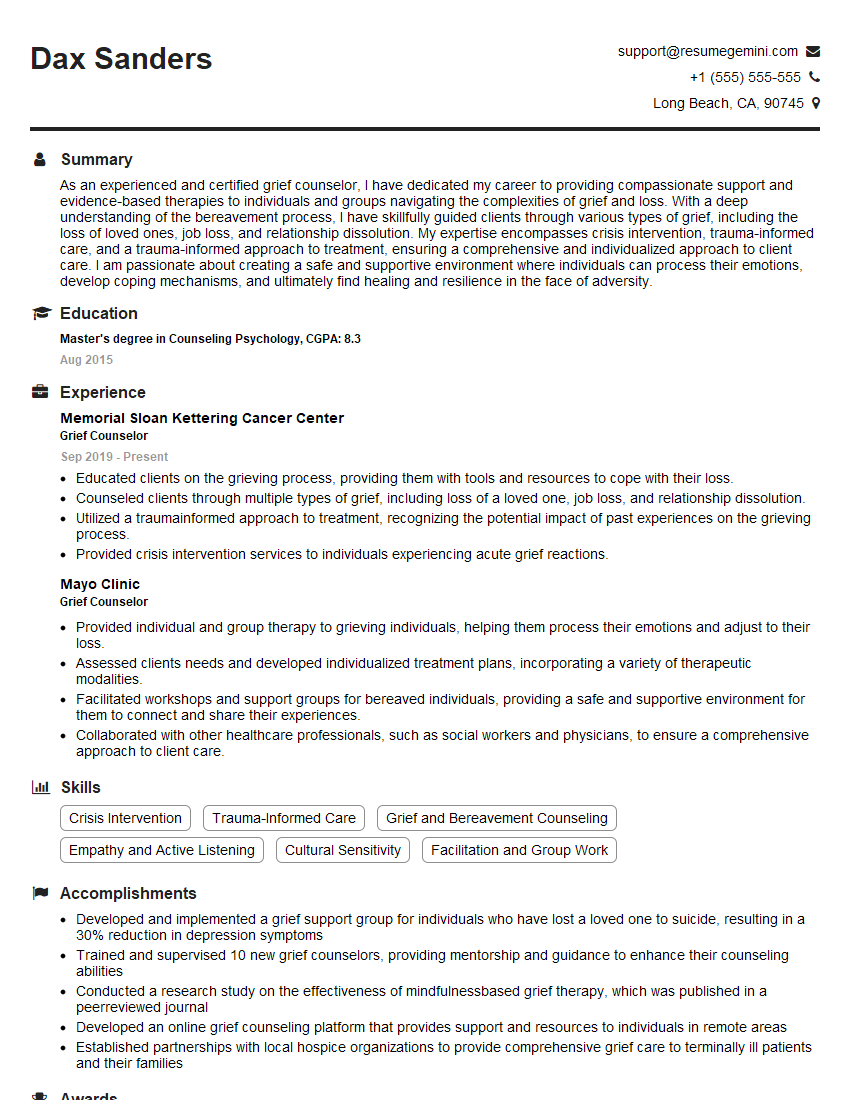
Mastering grief counseling concepts is crucial for career advancement in this compassionate and impactful field. A well-crafted resume is your key to unlocking opportunities. To ensure your qualifications shine, create an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional and impactful resume. Examples of resumes tailored to Grief Counseling Experience are available to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO