Unlock your full potential by mastering the most common Loss and Bereavement Support interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Loss and Bereavement Support Interview
Q 1. Describe your experience providing grief counseling to individuals experiencing complicated grief.
Complicated grief is a prolonged and debilitating response to loss, often characterized by intense longing, disbelief, and persistent intrusive thoughts. My experience working with individuals experiencing complicated grief involves utilizing a variety of therapeutic approaches tailored to their specific needs. This includes Cognitive Behavioral Therapy (CBT) to challenge maladaptive thought patterns and behaviors, Acceptance and Commitment Therapy (ACT) to help clients accept their grief and commit to valued actions, and Eye Movement Desensitization and Reprocessing (EMDR) to process traumatic memories associated with the loss. For example, I worked with a client who lost her spouse unexpectedly. She was experiencing intense guilt and self-blame, alongside debilitating anxiety. Using CBT, we identified and challenged her negative thought patterns, and through ACT, we developed coping strategies to manage her anxiety and participate in activities that brought her a sense of purpose. I also incorporate mindfulness and somatic techniques to help clients connect with their bodies and regulate their emotional responses.
Q 2. Explain your understanding of Kubler-Ross’s five stages of grief and its limitations.
The Kübler-Ross model proposes five stages of grief: denial, anger, bargaining, depression, and acceptance. While this model has increased awareness of the emotional complexities of grief, it’s crucial to understand its limitations. It presents grief as a linear progression, suggesting individuals move through these stages sequentially. In reality, grief is highly individualized and non-linear. People may experience these emotions in a different order, experience some stages more intensely than others, or not experience all stages at all. Some individuals may experience prolonged grief disorder, where their grief significantly impacts their daily functioning, long after the expected period of mourning. The model also fails to address the diverse ways individuals cope with loss and the influence of factors like social support, personality, and the nature of the loss. For instance, a person may primarily experience anger throughout their grieving process, while another might focus on bargaining, and neither is inherently ‘wrong’. It’s essential to approach grief with a nuanced understanding, recognizing its unique and often unpredictable path for each individual.
Q 3. How do you assess the needs of bereaved individuals and tailor your support accordingly?
Assessing the needs of bereaved individuals is a crucial first step. I begin with a thorough intake interview, exploring the circumstances of the loss, the individual’s history, their coping mechanisms, and their current support system. This includes assessing their emotional, physical, and social well-being. I utilize validated assessment tools, such as the Inventory of Complicated Grief (ICG) or the Prolonged Grief Disorder-13 (PG-13) to help quantify the intensity and duration of their grief. Then, through active listening and empathetic inquiry, I work collaboratively with the individual to develop personalized goals. For example, if someone is struggling with sleep disturbances, we might incorporate relaxation techniques. If they are experiencing social isolation, we may explore strategies to reconnect with their support network. The support tailored is always individualized and respects their unique circumstances and preferences.
Q 4. What methods do you employ to build rapport and trust with grieving clients?
Building rapport and trust with grieving clients requires creating a safe and non-judgmental space. I emphasize empathy, active listening, and genuineness in my interactions. This includes validating their feelings, acknowledging the uniqueness of their experience, and refraining from offering unsolicited advice. I focus on building a collaborative therapeutic relationship, where clients feel empowered to share their experiences without fear of criticism or judgment. Nonverbal cues are also important; maintaining appropriate eye contact, offering a comforting touch (when appropriate and culturally sensitive), and using an open and approachable body language. Sharing my own experiences (appropriately and in a professional capacity), helps create a connection with clients, showcasing my understanding of their struggles. Small acts of kindness and acknowledging their resilience also go a long way.
Q 5. How do you address the unique needs of children and adolescents coping with loss?
Children and adolescents grieve differently than adults. Their understanding of death is developmentally dependent, influenced by age and cognitive abilities. For younger children, grief may manifest as behavioral changes, such as clinginess or regression. Teenagers might display anger, isolation, or risky behaviors. My approach involves age-appropriate communication, using simple language and avoiding euphemisms. Play therapy can be invaluable for younger children, allowing them to express their emotions through creative activities. For adolescents, providing a safe space for them to openly discuss their feelings and validating their experience is crucial. Collaborating with parents or guardians is important, ensuring consistent support at home. Educational resources and activities are also valuable in helping children and teenagers understand the concepts of death and loss in ways they can grasp and process.
Q 6. Describe your experience facilitating grief support groups.
Facilitating grief support groups offers a unique opportunity for shared healing. I create a structured yet flexible environment that prioritizes safety, confidentiality, and mutual respect. Sessions typically involve structured activities like sharing circles, creative expression exercises, and education on coping strategies. My role is to guide discussions, facilitate connection between members, and offer support without imposing my own views or interpretations. Creating clear ground rules ensures the group remains focused and respectful. I actively monitor group dynamics and offer individual support as needed, addressing any conflicts or challenges that might arise. For example, I facilitated a group for parents who had lost a child. The shared experience created a strong sense of community and provided a platform for mutual support and empathy. This mutual support often proves as effective as, or more so than, individual therapy.
Q 7. How do you handle situations where a client is exhibiting self-harming behaviors or suicidal ideation?
Safety is paramount. If a client expresses self-harming behaviors or suicidal ideation, my immediate priority is to assess the level of risk. I use standardized risk assessment tools and engage in a detailed conversation to understand their current state, triggers, and plans. If there is an immediate risk, I will take the necessary steps to ensure their safety, which may include hospitalizing them or contacting emergency services. This may involve arranging a safety plan with the client, which outlines strategies for coping with difficult emotions and accessing support when needed. Ongoing therapy focuses on addressing the underlying issues contributing to their suicidal thoughts or self-harming behaviors, which often includes grief and trauma processing, stress management techniques, and development of coping strategies. Collaboration with other mental health professionals might be necessary, considering the complexity of these situations.
Q 8. Explain your approach to working with families experiencing the loss of a loved one.
My approach to working with bereaved families is grounded in a person-centered, holistic framework. I believe in meeting each family where they are in their grief journey, understanding that there’s no ‘right’ way to grieve. This means initially focusing on active listening and validating their emotions. I avoid offering unsolicited advice, instead, offering empathy and creating a safe space for them to express their feelings, memories, and concerns. I work collaboratively with them to identify their specific needs and tailor support accordingly. This might involve practical assistance, emotional support, or connecting them with other resources. A key component is normalizing grief—letting them know that their experience is valid and expected, and that intense emotions are part of the healing process. I typically begin by building rapport, establishing trust, and collaboratively setting goals for the support process.
For example, with a family who has recently lost a child, I might begin by acknowledging the immeasurable pain of their loss and offering my sincere condolences. Then, I would focus on listening to their stories about their child, validating their unique bond, and allowing them to express their range of emotions – from sadness and anger to guilt and confusion. From there, we’d collaboratively explore how I can best support them, perhaps through grief counseling, connecting them with support groups, or helping them navigate practical tasks.
Q 9. What resources do you typically utilize to support bereaved individuals?
The resources I utilize are multifaceted and tailored to the individual’s needs. This often includes:
- Individual and group therapy: Providing a safe space for processing emotions and developing coping mechanisms.
- Support groups: Connecting individuals with others who share similar experiences, fostering a sense of community and shared understanding.
- Referral to specialists: Connecting individuals with other professionals, such as psychiatrists, if needed for medication or treatment for complicated grief.
- Community resources: Linking families with local organizations offering practical assistance (e.g., meal delivery, childcare support).
- Educational materials: Providing access to books, articles, and websites that offer information on grief and bereavement.
- Creative arts therapies: Utilizing art, music, or writing as outlets for emotional expression.
- Spiritual/religious resources: Connecting clients with faith-based communities or leaders, if desired.
The choice of resources depends heavily on the individual’s preferences, needs, and cultural background.
Q 10. How do you maintain your own emotional well-being while working with grieving clients?
Maintaining my own emotional well-being is paramount in this field. It’s crucial to prevent compassion fatigue and burnout. My strategies include:
- Regular supervision: Meeting with a supervisor to debrief about challenging cases and discuss strategies for self-care.
- Self-reflection and journaling: Processing my own emotional responses to client experiences through writing or mindfulness practices.
- Maintaining healthy boundaries: Setting clear limits on my availability and avoiding taking on too much work.
- Engaging in self-care activities: Prioritizing activities that promote physical and mental health, such as exercise, spending time in nature, and pursuing hobbies.
- Seeking support from colleagues: Connecting with other professionals to share experiences and receive support.
- Utilizing mindfulness techniques: Employing meditation or deep breathing exercises to manage stress and promote emotional regulation.
Essentially, it’s about recognizing that I cannot effectively support others if I am not taking care of myself.
Q 11. Describe a challenging case involving a bereaved individual, and how you addressed it.
One challenging case involved a young widow who experienced the sudden death of her husband. She was overwhelmed by grief, struggling with intense feelings of guilt, anger, and isolation. Initially, she was resistant to engaging in therapy, preferring to isolate herself. My approach involved building rapport slowly, showing empathy for her pain, and validating her feelings. I didn’t pressure her to talk about her grief until she was ready. We started with small steps, focusing on practical issues such as managing finances and navigating bureaucratic processes. Gradually, we started exploring her grief, using techniques such as cognitive behavioral therapy (CBT) to challenge her negative thought patterns and helping her develop healthy coping strategies. We also explored the use of mindfulness techniques to help manage overwhelming emotions. Slowly, with consistent support and patience, she began to find her footing, developing a support network and eventually returning to work. The key was patience, empathy, and adapting my approach based on her response to the situation, not forcing a particular method on her.
Q 12. How do you incorporate cultural sensitivity into your bereavement support practices?
Cultural sensitivity is vital in bereavement support. Grief manifests differently across cultures. What might be considered a normal expression of grief in one culture may be seen as inappropriate in another. My approach involves:
- Seeking to understand cultural norms: Asking clients about their cultural background and beliefs surrounding death and dying. This includes how grief is expressed, rituals surrounding loss, and preferred methods of support.
- Respecting cultural practices: Recognizing and respecting the client’s cultural practices and traditions related to mourning. This might involve adapting my approach to align with their preferred methods of expression and support.
- Avoiding imposing my own beliefs: Recognizing that my understanding of grief is influenced by my cultural background and refraining from imposing my own views on the client.
- Utilizing culturally sensitive resources: Connecting individuals with community resources and support groups that are culturally relevant.
- Seeking consultation when needed: If I encounter cultural practices that I am unfamiliar with, I seek consultation from colleagues with relevant expertise.
For example, I might adjust my approach significantly when working with a family from a culture where public displays of emotion are less common. Instead of encouraging immediate emotional expression, I might offer a more quiet, contemplative approach.
Q 13. How do you differentiate between normal grief and complicated grief?
While grief is a highly personal experience, there are key differences between normal grief and complicated grief. Normal grief involves a wide range of emotions – sadness, anger, guilt, and acceptance – that typically lessen in intensity over time. While the grieving process can be challenging, individuals are generally able to function daily, maintain relationships, and gradually adapt to their life without their loved one.
Complicated grief, on the other hand, is characterized by persistent and overwhelming distress that significantly impairs an individual’s ability to function. This may include intrusive thoughts, intense longing for the deceased, avoidance of reminders of the loss, difficulty accepting the loss, and a sense of identity disruption. Symptoms of complicated grief can persist for an extended period, often exceeding six months to a year, and may interfere with various aspects of their life. Symptoms may also include significant impairment in social, occupational, and other important areas of functioning. A professional assessment is needed to determine whether grief is complicated.
Q 14. What are the ethical considerations involved in providing bereavement support?
Ethical considerations in bereavement support are crucial. These include:
- Confidentiality: Maintaining strict confidentiality of client information, adhering to professional codes of ethics and relevant legal requirements.
- Informed consent: Obtaining informed consent from clients before initiating any interventions, ensuring they understand the nature of the services being offered.
- Competence: Practicing within my scope of competence, recognizing my limitations and referring clients to other professionals when necessary.
- Avoiding dual relationships: Avoiding conflicts of interest by refraining from engaging in any dual relationships with clients.
- Cultural sensitivity: Respecting the cultural beliefs and practices of clients, avoiding cultural biases or assumptions.
- Boundary setting: Maintaining appropriate professional boundaries with clients, avoiding emotional entanglement or personal relationships.
- Avoiding coercion: Not pressuring clients into accepting services or interventions they are not comfortable with.
- Self-care: Prioritizing my own mental and emotional health to avoid burnout and ensure effective client care.
Ethical practice is foundational to providing compassionate and effective bereavement support.
Q 15. How would you handle a situation where a client’s beliefs conflict with your own?
Maintaining a client’s autonomy and dignity is paramount in bereavement support. When a client’s beliefs differ from mine, I prioritize understanding their perspective rather than imposing my own. This involves active listening, empathetic questioning, and a genuine effort to grasp their worldview. I focus on the client’s emotional experience and needs, tailoring my approach to align with their values and beliefs. For example, if a client holds deeply religious beliefs about death and the afterlife that contrast with my own secular views, I would carefully avoid imposing my perspectives. Instead, I would explore how their beliefs provide comfort and meaning during their grief, and integrate these into our sessions. The core of my practice remains centering on the client’s needs and supporting their grieving process regardless of our differences.
To achieve this, I utilize a person-centered approach, valuing their subjective experience. I acknowledge any potential discomfort caused by differing viewpoints and make it clear that I respect their beliefs. I’m committed to creating a safe and non-judgmental space where they feel comfortable expressing themselves fully. If I feel genuinely unable to provide support due to irreconcilable differences, I would refer them to another professional who better aligns with their belief system, ensuring ethical and sensitive care.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your understanding of trauma-informed approaches to grief counseling.
Trauma-informed grief counseling recognizes that past trauma can significantly impact a person’s experience of grief and bereavement. It acknowledges that grief can be exacerbated by past trauma, and vice versa, creating a complex interplay of emotional and psychological challenges. This approach emphasizes safety, trustworthiness, choice, collaboration, and empowerment.
- Safety: Creating a secure and predictable environment where clients feel safe to explore their emotions without fear of judgment or retraumatization is paramount.
- Trustworthiness: Building rapport and trust is crucial, as clients who have experienced trauma may struggle to trust others.
- Choice: Empowering clients by offering them choices regarding the pace and direction of therapy respects their autonomy and control.
- Collaboration: A collaborative approach emphasizes working together to address the client’s needs and goals.
- Empowerment: Focusing on the client’s strengths and resilience helps them regain a sense of control and agency.
For example, a client who experienced childhood abuse may react to the loss of a loved one with heightened anxiety and emotional dysregulation. A trauma-informed approach would prioritize understanding and validating these responses, rather than dismissing them as simply ‘excessive’ grief. Strategies might include pacing the therapeutic process, using somatic techniques to manage emotional overwhelm, and helping the client connect with their inherent resilience.
Q 17. How do you assess the effectiveness of your bereavement support interventions?
Assessing the effectiveness of bereavement interventions is a multifaceted process involving both quantitative and qualitative measures. I use a combination of methods to gauge progress, ensuring a holistic evaluation.
- Client Self-Report Measures: Standardized questionnaires, such as the Grief Experience Inventory or the Texas Revised Inventory of Grief, provide quantitative data on the client’s symptoms and coping mechanisms.
- Clinical Observation: I carefully observe client behavior during sessions, noting changes in mood, emotional regulation, and verbal/non-verbal communication. Changes in their ability to discuss their loss, engage in meaningful activities, and manage daily life are all valuable indicators.
- Goal Attainment Scaling: Collaboratively setting achievable goals at the beginning of therapy provides a framework for measuring progress. We regularly revisit these goals, modifying them as needed, and evaluating their attainment over time.
- Qualitative Feedback: I regularly solicit feedback from clients through open-ended discussions, allowing them to share their perceptions of the intervention’s effectiveness. This provides valuable insights into their subjective experience.
Combining these methods offers a richer, more nuanced picture of intervention effectiveness than any single approach could provide. Regular reassessment ensures ongoing adaptation and improvement of the support provided. For example, if a client’s self-reported grief intensity remains high despite several sessions, I might need to adjust the therapeutic approach, perhaps incorporating additional coping strategies or exploring underlying issues.
Q 18. Describe your experience working with diverse populations experiencing loss.
My experience working with diverse populations experiencing loss has underscored the importance of cultural sensitivity and tailoring interventions to meet unique needs. Cultural beliefs about death and mourning vary widely, influencing how individuals process and express their grief.
For example, working with families from Asian cultures, I would be mindful of the importance of filial piety and the specific rituals surrounding death and mourning. With clients from Indigenous communities, I would be sensitive to their spiritual beliefs and traditions, understanding that these practices are integral to their healing process. Similarly, I would understand and accommodate the varying grief expression and support networks found among different ethnic groups and religious communities.
Understanding these differences requires ongoing learning, collaboration with community leaders, and a commitment to continuous cultural competence training. It involves actively seeking out resources and educating myself on the specific cultural contexts of my clients’ experiences. My primary goal is to meet clients where they are, respecting their individual and cultural identities, and providing support that aligns with their values and beliefs. This sensitivity often determines the effectiveness of the therapeutic process and builds trust.
Q 19. How do you ensure client confidentiality and privacy?
Client confidentiality and privacy are fundamental to my practice, underpinned by ethical guidelines and legal requirements. I adhere strictly to professional codes of conduct and relevant data protection laws.
- Informed Consent: Clients are fully informed about how their information will be used and stored before any treatment begins. This includes explanation of record-keeping practices, limits to confidentiality (e.g., mandatory reporting of abuse), and their right to access their own records.
- Secure Data Management: All client records, both electronic and paper-based, are stored securely and accessed only by authorized personnel. Strict password protection, encryption, and secure file storage are implemented. I also follow all HIPAA regulations (in the US) or equivalent data protection laws of other countries.
- Confidentiality Boundaries: I discuss the limits of confidentiality openly and honestly with clients, explaining situations where I may be legally obligated to disclose information (such as suspected child abuse or harm to self or others).
- Supervision and Consultation: I regularly engage in clinical supervision, discussing cases in a confidential and anonymized manner to ensure ethical practice and obtain peer support. This also provides another layer of accountability.
Breaching confidentiality is rare and would only occur under legally mandated circumstances, always following proper procedures and ensuring the client’s safety is the priority.
Q 20. What are the signs of secondary traumatic stress, and how do you mitigate it?
Secondary Traumatic Stress (STS) is a consequence of repeatedly being exposed to others’ traumatic experiences, affecting those who work in helping professions. It’s essentially compassion fatigue – emotional exhaustion and burnout resulting from empathetic engagement with clients’ suffering.
- Signs of STS: Symptoms can include emotional numbness, anxiety, intrusive thoughts, difficulty sleeping, irritability, cynicism, feelings of helplessness, and a decreased sense of accomplishment.
- Mitigation Strategies: Preventing and managing STS requires a proactive approach.
- Self-Care: Prioritizing self-care is crucial. This includes adequate sleep, healthy diet, regular exercise, and engaging in activities that promote relaxation and enjoyment.
- Supervision: Regular supervision provides a safe space to process emotional reactions to clients’ experiences and receive guidance and support from experienced colleagues.
- Boundaries: Setting clear boundaries between professional and personal life is essential to prevent emotional overflow. This includes limiting work hours and avoiding taking work home.
- Mindfulness and Relaxation Techniques: Practices like mindfulness meditation, deep breathing, and yoga can help manage stress and promote emotional regulation.
- Professional Support: If symptoms persist or worsen, seeking professional help from a therapist or counselor specializing in trauma or burnout is recommended.
Recognizing the signs of STS and taking proactive steps to mitigate its effects is critical for maintaining professional wellbeing and ensuring sustainable and effective client care. It’s a sign of professional responsibility to safeguard one’s mental health to better support those in need.
Q 21. How do you navigate working with clients who are resistant to receiving support?
Resistance to support is common in bereavement, often stemming from fear, shame, or a perceived inability to cope. It’s not a rejection of the helper, but rather a reflection of the individual’s internal struggles.
My approach emphasizes understanding and validating the client’s resistance, rather than directly confronting it. I begin by building rapport and fostering a safe and non-judgmental environment. I listen attentively to their concerns and attempt to understand the reasons behind their resistance. It’s a collaborative process, not a battle of wills.
- Empathetic Validation: Acknowledging their feelings and experiences without judgment, such as: “I understand that you may not be ready for this right now, and that’s okay.”
- Collaborative Goal Setting: Instead of imposing a specific therapeutic approach, I work with them to define goals that align with their readiness and pace. This could involve setting small, achievable steps rather than tackling everything at once.
- Flexibility and Patience: The process is often gradual. Patience, understanding and recognizing that change takes time is vital.
- Referral When Necessary: If the resistance is persistent and hindering the therapeutic process, I might suggest a referral to another professional whose approach may be a better fit.
Ultimately, the goal is not to ‘force’ support but to create an atmosphere where the client feels empowered to engage in the healing process at their own pace. Sometimes, just providing a listening ear and acknowledging their pain is enough to build trust and open the door to future support.
Q 22. Explain your understanding of different theoretical frameworks used in grief counseling.
Grief counseling draws upon several theoretical frameworks to understand and address the complexities of bereavement. These frameworks aren’t mutually exclusive; often, a therapist integrates elements from several to best suit the client’s needs.
Attachment Theory: This framework emphasizes the importance of early relationships and their impact on how we cope with loss. A secure attachment style often leads to healthier grieving, while insecure attachments can complicate the process. For example, someone with an avoidant attachment might suppress their emotions, hindering healthy grieving.
Kubler-Ross’s Stages of Grief: While not a universally accepted linear model, this framework (denial, anger, bargaining, depression, acceptance) provides a helpful structure for understanding the emotional journey. It’s crucial to remember that grief is not always linear, and individuals may experience these stages in different orders, intensities, or not at all.
Dual Process Model (DPM): This model acknowledges the oscillation between loss-oriented coping (e.g., confronting grief, acknowledging loss) and restoration-oriented coping (e.g., adapting to life changes, developing new routines). A client might spend a day immersed in memories (loss-oriented) and the next focusing on rebuilding their life (restoration-oriented).
Grief as a relational process: This more contemporary approach emphasizes the relational aspect of grief, focusing on the meaning of the relationship with the deceased and how that loss impacts the bereaved person’s identity and relationships with others. For instance, a client might explore how the deceased’s values and influence still shape their choices.
Understanding these frameworks allows me to tailor my approach to each client, acknowledging the uniqueness of their grief experience and providing appropriate support.
Q 23. How do you document client progress and outcomes?
Thorough documentation is essential for ethical practice and effective client care. I maintain detailed case notes, adhering to all relevant privacy regulations. These notes include:
Client demographics and presenting problem: Basic information about the client and their reason for seeking support.
Session summaries: Key discussion points, emotional state of the client, and any significant events.
Treatment plan: Goals for therapy, strategies used, and progress towards those goals. This is a collaborative process, with the client’s input being vital.
Outcome measures: Regular assessments using validated scales to track the client’s progress in managing grief and improving their overall well-being. Examples include standardized grief measures.
Relevant observations: Anything relevant to the client’s progress that doesn’t neatly fit into other categories.
These notes are stored securely, both electronically and physically, in accordance with all relevant professional and legal requirements. Regular review of these notes allows for ongoing evaluation of treatment efficacy and adjustments as needed.
Q 24. What strategies do you use to help clients develop healthy coping mechanisms?
Helping clients develop healthy coping mechanisms is central to grief counseling. My strategies are individualized but often involve:
Mindfulness and meditation: These practices can help clients manage overwhelming emotions and cultivate self-awareness.
Emotional regulation techniques: Teaching clients skills like deep breathing, progressive muscle relaxation, and journaling to help them manage intense feelings.
Cognitive restructuring: Challenging negative thought patterns and replacing them with more realistic and helpful ones. For example, addressing beliefs like ‘I should have done more’ or ‘I’ll never be happy again’.
Social support: Encouraging connection with supportive friends, family, or support groups. Facilitating this connection is a vital part of the healing process.
Creative expression: Using art, music, writing, or other creative outlets to process emotions and experiences.
Physical activity: Encouraging exercise, which has been shown to improve mood and reduce stress.
I always emphasize the importance of self-compassion and validating the client’s feelings throughout this process.
Q 25. Describe your experience with crisis intervention related to bereavement.
Crisis intervention in bereavement often involves responding to immediate, intense emotional distress. This might include suicidal ideation, severe anxiety, or acute psychological trauma related to the death. My approach prioritizes safety and stabilization.
I use a collaborative approach, actively listening to the client’s experience and validating their emotions. Immediate interventions might include:
Safety planning: Developing a plan to ensure the client’s safety, addressing potential risks, and providing access to emergency resources if needed. This might involve phone numbers of crisis lines or agreements regarding checking in with a loved one.
Grounding techniques: Helping the client to feel present in the moment and reduce overwhelming feelings through sensory exercises.
Emotional first aid: Offering empathy, validation, and reassurance to help the client feel less alone and overwhelmed.
Referral to specialist services: If needed, I will promptly refer the client to psychiatric services, trauma specialists, or other appropriate professionals.
In crisis situations, rapid assessment and intervention are crucial to stabilizing the client’s emotional state and reducing immediate risk. Follow-up support is then vital for long-term healing.
Q 26. How would you handle a situation involving a family conflict related to grief and loss?
Family conflicts arising from grief and loss are common. These can stem from disagreements about funeral arrangements, inheritance, blame, or differing grieving styles. My approach emphasizes a neutral, facilitative role.
I facilitate family meetings in a safe and respectful environment, encouraging open communication and active listening. Techniques I use include:
Mediation: Helping family members understand each other’s perspectives and find common ground.
Conflict resolution skills: Teaching family members effective communication skills, such as assertive communication and active listening.
Emotional regulation strategies: Supporting family members to manage their emotions in a constructive manner during discussions.
Setting boundaries: Assisting the family in establishing healthy boundaries to protect their emotional well-being. This might involve creating clear communication protocols.
Individual sessions: If needed, I offer individual sessions to family members to address specific concerns and process their emotions before tackling the family dynamics.
The goal is to help the family navigate their conflict in a way that respects their differences and promotes healing for everyone. Sometimes, referral to family therapy is appropriate.
Q 27. What are some common misconceptions about grief and dying that you encounter?
Several misconceptions surrounding grief and dying frequently arise:
The myth of linear stages: Believing that grief follows a predictable series of stages and that there’s a ‘right’ way to grieve. Grief is highly individual and non-linear.
The ‘get over it’ mentality: Expecting individuals to quickly overcome their grief. Grief is a process that takes time and varies across individuals.
Comparing grief experiences: Believing that one type of loss is ‘worse’ than another. All grief is valid, regardless of the relationship or cause of death.
The belief that grief ends: Grief is often a lifelong journey of adaptation. While intensity might decrease, the loss is always a part of the person’s life story.
Ignoring the needs of the bereaved: A common societal response which leads to increased suffering and isolation.
Addressing these misconceptions is vital in providing sensitive and effective support. I help clients understand that their grief is normal and valid, regardless of societal expectations.
Q 28. What continuing education or professional development have you pursued in the area of loss and bereavement?
My commitment to professional growth is ongoing. I regularly participate in continuing education activities focusing on advancements in grief and bereavement care. Recent examples include:
Advanced training in trauma-informed grief therapy: This enhanced my ability to support clients who have experienced trauma related to the death.
Workshops on working with complicated grief: This deepened my understanding of prolonged or debilitating grief and how to effectively intervene.
Seminars on cultural considerations in bereavement: This broadened my awareness of cultural variations in grieving practices and their impact on the therapeutic process.
Supervision and consultation with experienced grief counselors: This provides ongoing support and opportunities for professional reflection.
Staying abreast of the latest research and best practices ensures I provide the most effective and compassionate support to my clients.
Key Topics to Learn for Loss and Bereavement Support Interview
- Understanding Grief and Loss: Explore the various stages of grief, acknowledging the diverse and individualized nature of the grieving process. Consider the impact of different types of loss (e.g., death of a loved one, job loss, relationship breakdown).
- Communication and Active Listening Skills: Develop your ability to empathetically listen and communicate effectively with grieving individuals. Practice using verbal and nonverbal cues to create a safe and supportive space.
- Ethical Considerations: Familiarize yourself with ethical guidelines and professional boundaries within Loss and Bereavement Support. Understand the importance of maintaining confidentiality and respecting client autonomy.
- Practical Application: Consider case studies and scenarios involving diverse client needs and challenging situations. Think about how you would approach providing support in different settings (hospitals, hospices, community centers).
- Trauma-Informed Care: Learn about the impact of trauma on grief and bereavement and how to tailor your approach to support individuals with complex needs.
- Support Resources and Referral Networks: Understand the importance of knowing available resources and community support systems. Develop your ability to identify when a referral to a specialist is necessary.
- Self-Care and Compassion Fatigue: Learn strategies for managing your own emotional wellbeing while providing support to others. Understand the signs of compassion fatigue and develop coping mechanisms.
Next Steps
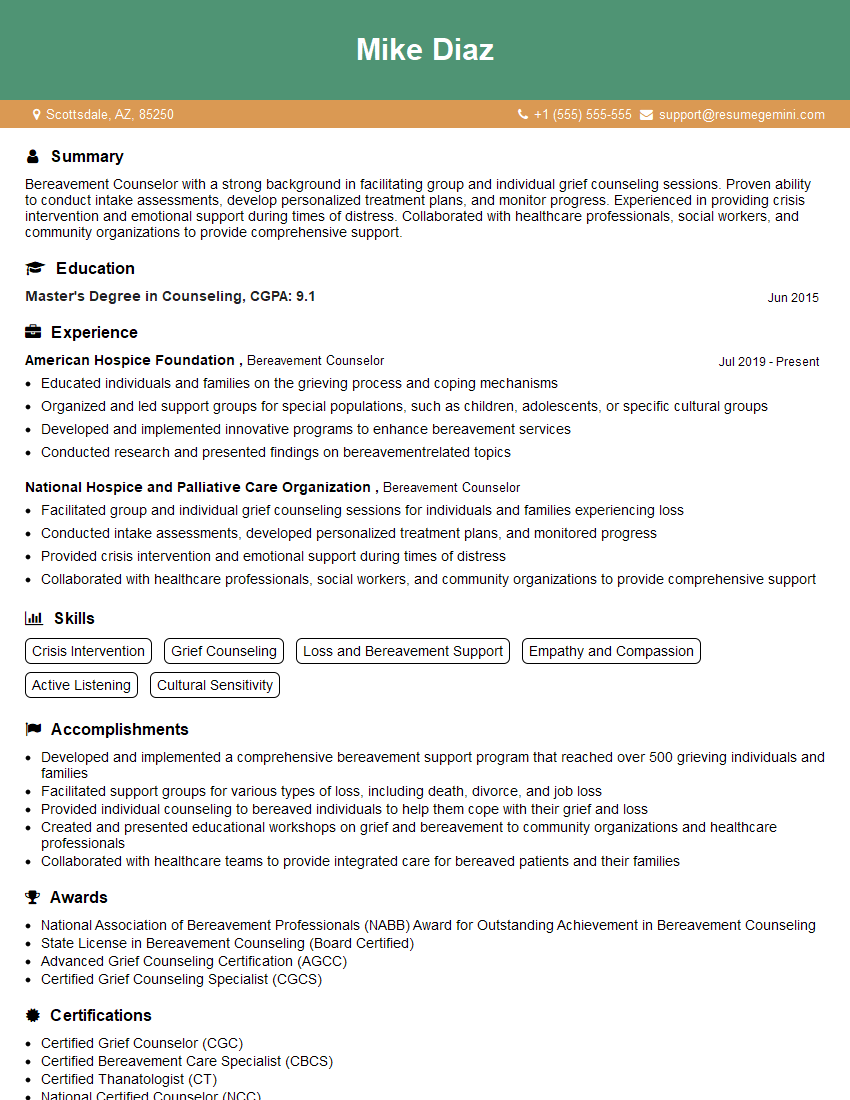
Mastering Loss and Bereavement Support opens doors to fulfilling and impactful careers, allowing you to make a profound difference in the lives of others. A well-crafted resume is crucial for showcasing your skills and experience to potential employers. To maximize your job prospects, create an ATS-friendly resume that highlights your relevant qualifications and experience. ResumeGemini is a trusted resource that can help you build a professional and impactful resume. Examples of resumes tailored to Loss and Bereavement Support are available to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO