The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Injections and vaccinations interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Injections and vaccinations Interview
Q 1. Describe the proper technique for intramuscular (IM) injections.
Intramuscular (IM) injections deliver medication directly into a muscle, allowing for rapid absorption. Proper technique is crucial to ensure effective delivery and minimize discomfort and complications. Here’s a step-by-step guide:
- Preparation: Gather all necessary supplies: medication, appropriate syringe and needle (gauge and length determined by the medication and patient factors), alcohol swabs, gauze pads, sharps container, gloves. Verify the medication’s name, dosage, expiration date, and integrity (check for discoloration or particulate matter).
- Patient Identification: Confirm the patient’s identity using two identifiers (e.g., name and date of birth) to prevent medication errors.
- Site Selection and Preparation: Choose an appropriate IM injection site (deltoid, vastus lateralis, ventrogluteal) based on medication, patient age, and muscle mass. Cleanse the selected site with an alcohol swab using a circular motion, moving outwards from the center. Allow the site to air dry.
- Injection Technique: With the dominant hand, pinch the skin at the injection site, creating a taut surface. Use the other hand to hold the syringe, inserting the needle at a 90-degree angle for most adults. Aspirate (pull back on the plunger) to check for blood return (although this practice is debated amongst healthcare professionals). If blood is present, withdraw the needle and choose a different location. If no blood returns, slowly inject the medication.
- Withdrawal and Disposal: Once the injection is complete, withdraw the needle at the same angle it was inserted. Apply gentle pressure to the injection site with a gauze pad. Do not massage the area. Dispose of the needle and syringe immediately in an approved sharps container.
Remember, proper hand hygiene before and after the procedure is essential. Patient education and reassurance are critical to alleviate anxiety.
Q 2. Explain the different injection sites for IM, subcutaneous (SC), and intradermal (ID) injections.
Different injection routes target various tissue layers for optimal medication absorption and action:
- Intramuscular (IM): Injects medication into muscle tissue. Common sites include the deltoid (upper arm), vastus lateralis (thigh), and ventrogluteal (buttock). The ventrogluteal is often preferred for larger volumes and to minimize nerve damage.
- Subcutaneous (SC): Delivers medication into the subcutaneous fat layer, just beneath the skin. Common sites are the outer aspect of the upper arm, the anterior thigh, and the abdomen. This route is suitable for smaller volumes and slower absorption rates.
- Intradermal (ID): Injects medication into the dermis, the layer of skin just beneath the epidermis. The inner forearm and upper back are typically used for ID injections. This route is used for allergy testing and TB skin tests, producing a small wheal or bleb.
Site selection depends on the medication, injection volume, patient factors (e.g., age, body habitus), and the desired absorption rate. For example, a viscous medication might require a larger muscle for injection, while a small volume of insulin might be readily absorbed subcutaneously.
Q 3. What are the potential complications associated with injections and how are they managed?
Injection-related complications can range from minor to serious:
- Pain, swelling, redness, or bruising: These are common, usually mild, and often resolve spontaneously. Cold compresses and over-the-counter pain relievers can help.
- Abscess formation: A localized collection of pus, potentially requiring drainage.
- Nerve damage: Accidental needle insertion into a nerve can cause pain, numbness, or tingling. This is minimized by proper site selection and technique.
- Infection: Improper aseptic technique can introduce bacteria, leading to infection. This requires prompt medical attention and antibiotic treatment.
- Hematoma: Bleeding into the surrounding tissues due to vessel puncture. Applying pressure to the site can help.
- Allergic reaction: Rare but potentially life-threatening reactions can occur, requiring immediate medical intervention (e.g., epinephrine administration).
Management involves careful assessment of symptoms, supportive care (e.g., pain relief, cold compresses), and potentially antibiotic treatment or other interventions depending on the severity of the complication.
Q 4. How do you ensure patient safety during injections?
Ensuring patient safety during injections is paramount. Key strategies include:
- Strict adherence to aseptic technique: Hand hygiene, proper site preparation, and sterile equipment prevent infection.
- Accurate medication identification and dosage verification: Preventing medication errors is critical. This involves double-checking labels and confirming the order with the patient’s chart.
- Proper injection technique: Minimizes pain, discomfort, and the risk of complications.
- Patient education and communication: Explaining the procedure, answering questions, and reassuring the patient reduces anxiety.
- Monitoring for adverse reactions: Observing the patient for any immediate reactions post-injection is crucial. This includes allergic reactions or pain at the injection site.
- Documentation: Meticulously documenting the injection site, medication administered, dosage, route, time, date, and any observed reactions is essential.
A systematic approach focusing on each of these points minimizes the risk of complications and ensures a safe injection experience for every patient.
Q 5. Describe your experience with various types of syringes and needles.
My experience encompasses a wide range of syringes and needles, from standard disposable syringes used for routine immunizations to specialized syringes used for precise fluid delivery. This includes:
- Various sizes and capacities: From 1ml tuberculin syringes for small volumes to larger 10ml syringes for higher volumes of medication.
- Different needle gauges: Smaller gauge numbers (e.g., 25G) indicate thicker needles, suitable for subcutaneous injections, whereas larger gauges (e.g., 22G or 21G) are often used for intramuscular injections depending on the viscosity and volume of the medication.
- Needle lengths: Varying lengths accommodate different injection sites and tissue depths. Longer needles (e.g., 1 inch) are often used for intramuscular injections, while shorter needles are used for subcutaneous and intradermal injections.
- Safety-engineered needles: These needles have built-in safety features, such as retractable needles or needle shields, reducing needle stick injuries.
My experience includes familiarity with different brands and types of syringes, ensuring selection based on the specific requirements of each injection.
Q 6. How do you select the appropriate needle size and length for different injections?
Needle size and length selection is crucial for effective and safe injection. This is determined by several factors:
- Injection route: IM injections generally require longer needles (1-1.5 inches for adults) to reach the muscle tissue, while SC injections use shorter needles (1/2 – 5/8 inch), and ID injections use very short needles (1/4 – 1/2 inch).
- Patient characteristics: Needle length might need adjustment for obese patients (longer needles) or smaller children (shorter needles).
- Medication viscosity and volume: Highly viscous medications often require larger bore needles (smaller gauge) to facilitate smooth injection, but for smaller volumes, a smaller bore needle is appropriate to reduce discomfort and bruising.
For instance, administering a viscous medication intramuscularly in an adult might require a 22G needle, while a subcutaneous insulin injection might use a 25G or 27G needle. Always consult guidelines and package inserts to determine the appropriate needle size for each medication.
Q 7. What are the contraindications for receiving certain vaccinations?
Contraindications for certain vaccinations are factors that increase the risk of adverse events and should be carefully considered before vaccination. These include:
- Severe allergic reaction to a previous dose or vaccine component: A history of anaphylaxis or other severe allergic reactions to a specific vaccine or its components is a contraindication for further administration.
- Moderate or severe illness: Vaccinations are often deferred until recovery from a significant illness to avoid potential interference with immune response and increased risk of adverse events.
- Pregnancy or breastfeeding: Certain vaccines are not recommended during pregnancy or breastfeeding because their effects on fetal or infant development are not fully understood. Specific guidelines vary based on vaccine and maternal health.
- Immunodeficiency: Individuals with compromised immune systems might have a diminished response to vaccinations or an increased risk of complications. Immunosuppressive medications and certain conditions can fall into this category.
- Specific medical conditions: Certain health conditions might be contraindications, dependent on vaccine type. For example, individuals with thrombocytopenia might have increased bleeding risk with injections. Careful evaluation by a healthcare professional is needed.
It’s crucial to carefully review the patient’s medical history, including medications, allergies, and current health status to ensure appropriate vaccination planning. Consulting relevant vaccination guidelines is paramount.
Q 8. How do you handle a patient experiencing an adverse reaction to a vaccination?
Handling an adverse reaction to a vaccination begins with immediate assessment of the patient’s symptoms. Mild reactions like redness, swelling, or soreness at the injection site are common and usually resolve within a few days. However, more serious reactions require immediate intervention. These could include anaphylaxis (a severe, life-threatening allergic reaction), high fever, difficulty breathing, or severe dizziness.
My first step is to immediately stop the procedure and assess the patient’s airway, breathing, and circulation (ABCs). I’d then initiate emergency care protocols, which may involve administering epinephrine (adrenaline) in cases of anaphylaxis, monitoring vital signs, and contacting emergency medical services. Accurate documentation of the event, including the type of vaccine, time of administration, symptoms observed, interventions performed, and patient response, is crucial for reporting and future care. Following the incident, a thorough follow-up with the patient is essential to monitor their recovery and provide any necessary support.
For instance, I once had a patient develop hives and difficulty breathing shortly after receiving a flu shot. I immediately administered epinephrine, monitored their vital signs, and contacted emergency medical services. Thankfully, they recovered fully after treatment. This highlights the importance of being prepared to handle various adverse events.
Q 9. Explain the importance of proper injection site preparation.
Proper injection site preparation is paramount in preventing infection and ensuring the vaccine’s efficacy. The skin is teeming with microorganisms, and failure to properly clean the area can introduce these contaminants into the bloodstream, leading to infections.
The process typically involves cleansing the injection site with an antiseptic solution, such as isopropyl alcohol or povidone-iodine, using a circular motion, moving outward from the center. This helps to remove surface dirt and bacteria. Allowing the area to air dry is crucial before administering the injection, as residual moisture can interfere with the injection process and potentially dilute the vaccine. The use of sterile gloves is also mandatory to maintain aseptic technique. Finally, choosing the correct injection site based on the patient’s age and the type of vaccine is essential. For example, the deltoid muscle is preferred for intramuscular injections in adults, while the vastus lateralis muscle in the thigh is suitable for infants and young children.
Q 10. What are the steps involved in administering a vaccination?
Administering a vaccination involves several crucial steps to ensure safety and efficacy. These steps include:
- Verification of Patient Identity: Confirming the patient’s identity using two identifiers, such as name and date of birth, is a critical first step to prevent medication errors.
- Site Preparation: Cleaning the injection site with an antiseptic solution as described earlier.
- Vaccine Selection and Preparation: Selecting the correct vaccine and ensuring it’s correctly prepared, including checking expiry dates and verifying the integrity of the vaccine vial.
- Injection Technique: Administering the vaccine using appropriate injection technique (e.g., intramuscular, subcutaneous, intradermal), depending on the vaccine type. This involves correct needle insertion angle and depth.
- Post-Injection Care: Applying a small bandage to the injection site (if needed), and providing the patient with post-vaccination instructions including expected side effects and what to do if adverse reactions occur.
- Disposal: Properly disposing of used needles and syringes in designated sharps containers to prevent needle-stick injuries.
Each step is essential, and deviation can compromise the safety and efficacy of the vaccination process.
Q 11. How do you document injection and vaccination administration?
Accurate and thorough documentation is paramount in injection and vaccination administration. It’s essential for tracking patient health, ensuring vaccine coverage rates, and managing potential adverse events. Documentation should include the patient’s full name, date of birth, date and time of vaccination, the type and lot number of the vaccine administered, the injection site, the route of administration, any observed reactions, and the administering healthcare professional’s signature.
Electronic health records (EHRs) are increasingly utilized, providing a centralized and easily accessible record. However, even with EHRs, a paper record is often maintained as a backup to prevent data loss. Maintaining detailed records is not just about following protocol, but about patient safety and accountability. In the case of any adverse event, thorough documentation is essential for investigations and analysis.
Q 12. What is your experience with vaccine storage and handling?
My experience encompasses all aspects of vaccine storage and handling, adhering strictly to the manufacturer’s guidelines. This includes maintaining the recommended cold chain temperature throughout the vaccine’s shelf life using specialized refrigerators and freezers equipped with temperature monitoring systems. Regular temperature checks are conducted, and any deviations are documented and reported. Vaccines are stored according to their specific requirements, with some needing ultra-cold storage, while others can be stored at standard refrigeration temperatures.
Proper handling includes ensuring that vaccines are protected from light exposure, and avoiding freezing unless specifically indicated by the manufacturer. First-in, first-out (FIFO) inventory management systems are utilized to ensure that vaccines with the soonest expiration dates are used first. Regular inventory audits are carried out to identify expiring vaccines and address any storage issues promptly. Strict adherence to these protocols ensures vaccine potency and safety.
Q 13. Describe the different types of vaccines and their administration methods.
Vaccines are classified into several types, each with its own administration method:
- Live-attenuated vaccines: These contain weakened versions of the virus or bacteria. Examples include the measles, mumps, and rubella (MMR) vaccine and the varicella (chickenpox) vaccine. They are usually administered intramuscularly or subcutaneously.
- Inactivated vaccines: These contain killed viruses or bacteria. Examples include the influenza vaccine (injected) and the polio vaccine (injected). They’re generally administered intramuscularly.
- Subunit, recombinant, polysaccharide, and conjugate vaccines: These vaccines use specific components of the virus or bacteria, rather than the whole organism. Examples include the hepatitis B vaccine and the HPV vaccine. They are typically given intramuscularly.
- Toxoid vaccines: These vaccines use inactivated toxins produced by bacteria. An example is the tetanus vaccine, which is usually administered intramuscularly.
The choice of administration method depends on the vaccine type, age of the patient, and the intended immune response. For example, intradermal administration is used for certain types of tuberculosis testing. Proper training and adherence to manufacturer’s instructions are vital to ensure safe and effective vaccination.
Q 14. How do you verify patient identity before administering an injection or vaccination?
Verifying patient identity is a critical step before any injection or vaccination. It’s a cornerstone of safe healthcare practice. I always use at least two identifiers to confirm a patient’s identity before administering any medication or vaccine. This typically involves checking the patient’s name and date of birth against their identification documents, such as a driver’s license or health insurance card.
In addition to checking documentation, I also visually confirm the patient’s identity by comparing their appearance with the information on their identification. This multi-step approach minimizes the risk of administering the wrong vaccine to the wrong patient, a serious medication error that could have life-threatening consequences. This meticulous approach ensures that the right patient receives the correct vaccine, promoting safety and preventing errors.
Q 15. How do you communicate effectively with patients about injections and vaccinations?
Effective communication is paramount when discussing injections and vaccinations. I always begin by establishing a comfortable and trusting environment. I use plain language, avoiding medical jargon whenever possible. For example, instead of saying ‘intramuscular injection,’ I might say ‘a shot in the muscle.’ I actively listen to the patient’s concerns and answer their questions thoroughly and patiently. I explain the procedure step-by-step, what to expect, and address any anxieties they might have. Visual aids, like diagrams or brochures, can be very helpful, especially when explaining vaccine schedules or potential side effects. I also emphasize the benefits of vaccination in a way that resonates with their individual circumstances and health goals. Finally, I provide clear, written information to reinforce the discussion and answer any lingering questions.
For example, with a hesitant parent considering the MMR vaccine for their child, I would explain the importance of protecting their child from measles, mumps, and rubella, highlighting the potential severity of these diseases. I would then carefully detail the vaccination process, address any concerns about side effects (emphasizing their rarity and typical mildness), and answer their questions with empathy and patience.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain the importance of following infection control protocols during injections.
Strict adherence to infection control protocols is non-negotiable when administering injections. This is crucial to prevent the transmission of infectious diseases. My practice incorporates several key elements: hand hygiene (thorough handwashing or use of an alcohol-based hand rub), wearing appropriate personal protective equipment (PPE) such as gloves and gowns when necessary, using sterile needles and syringes, ensuring proper disposal of sharps and other potentially infectious waste according to established guidelines, and adhering to aseptic techniques during the injection process. This includes cleaning the injection site with an antiseptic solution before administering the injection. Any accidental needlestick injuries are immediately reported and managed according to established procedures.
For instance, if administering an injection to a patient with a known infection, I would utilize extra precautions, such as wearing a gown and mask in addition to gloves, and ensuring a thorough cleaning of the injection site and the proper disposal of all contaminated materials. The goal is to create a completely sterile environment to minimize any risk of infection.
Q 17. What are your experience with electronic health records (EHRs) related to injections and vaccinations?
I have extensive experience using electronic health records (EHRs) for managing injection and vaccination data. I am proficient in using EHR systems to document patient vaccination history, record injection administration details (date, time, injection site, vaccine lot number, vaccine type, and any adverse events), generate vaccination reports and reminders, and access relevant patient information quickly and efficiently. I am comfortable utilizing EHRs to ensure accurate tracking of vaccine inventory, manage recalls and expiration dates, and comply with reporting requirements for various public health agencies. My ability to navigate EHRs effectively allows for seamless patient care and enhances the overall efficiency of the vaccination process.
For example, using the EHR, I can easily generate a report showing the number of influenza vaccines administered in a specific time period, identify patients due for booster shots, and quickly access a patient’s complete vaccination history to make informed decisions about their care.
Q 18. How do you manage sharps waste safely?
Safe sharps disposal is critical for preventing accidental needlestick injuries and protecting healthcare workers and the environment. My process involves using puncture-resistant sharps containers that are clearly labeled and readily accessible at the point of care. Used needles and syringes are immediately disposed of into these containers without recapping. Once the container is approximately two-thirds full, it’s sealed according to facility protocols and sent for proper incineration or autoclaving, following all relevant regulations. Regular training and adherence to these protocols ensure the safety of staff and prevent accidental exposure to infectious materials.
For example, imagine a scenario where a sharps container is accidentally dropped. We must ensure no one touches the broken container. We should follow our established safety protocols; we need to call our safety team to safely clean the area, dispose of the broken container correctly, and review the actions to prevent this from occurring again.
Q 19. Describe your knowledge of various injection routes and their applications.
I’m knowledgeable in various injection routes, each having specific applications.
- Intradermal (ID): Injections administered into the dermis, the layer of skin just below the epidermis. This route is mainly used for allergy testing and tuberculosis testing (Mantoux test) because it allows for a localized reaction to be observed.
- Subcutaneous (SC): Injections delivered into the subcutaneous tissue, the fatty layer just below the dermis. This route is suitable for medications that are absorbed slowly, such as insulin and some vaccines. The absorption rate is relatively slow compared to intramuscular injections.
- Intramuscular (IM): Injections given into a muscle, typically the deltoid muscle of the arm, the vastus lateralis muscle of the thigh, or the gluteus maximus muscle of the buttock. This route allows for rapid absorption of the medication and is used for many vaccines and medications requiring faster onset.
- Intravenous (IV): Injections directly into a vein, delivering the medication immediately into the bloodstream. This is the fastest route of administration and is typically used for emergencies or medications requiring immediate action.
Q 20. What is your experience with administering vaccines to different age groups?
I have extensive experience administering vaccines to diverse age groups, from infants to elderly individuals. Each age group presents unique considerations. Infants, for example, require smaller needle sizes and specific injection sites (vastus lateralis muscle is preferred). Children may need a more playful and reassuring approach to minimize anxiety. Adolescents may have specific questions or concerns related to vaccine safety and efficacy, requiring open communication and accurate information. Adults, including older adults, may have pre-existing medical conditions that need to be considered when selecting a vaccine or injection site. My approach always prioritizes patient comfort and safety, adapting my techniques and communication style to the individual’s age and developmental stage.
For example, when vaccinating infants, I would prioritize a calm and comforting demeanor, involving the parents actively in the process, and ensuring the infant is properly restrained and soothed before administering the vaccine.
Q 21. Explain the concept of vaccine efficacy and effectiveness.
Vaccine efficacy and effectiveness are often used interchangeably but have distinct meanings. Efficacy refers to a vaccine’s performance under ideal conditions during clinical trials. It’s usually expressed as a percentage representing the reduction in disease incidence among vaccinated individuals compared to a placebo group. Effectiveness, on the other hand, reflects how well a vaccine performs in the real world. It considers factors that aren’t controlled in clinical trials, such as variations in vaccine storage, administration techniques, and the population’s characteristics (age, immune status, etc.). Effectiveness is often lower than efficacy because of these real-world challenges. For example, a vaccine might have 95% efficacy in a clinical trial, but its effectiveness in a real-world setting might be closer to 85%, due to factors such as inconsistent storage or administration, differences in immune responses within the population, or the emergence of new virus variants.
Understanding both efficacy and effectiveness helps to assess the true impact of a vaccine in protecting a population. High efficacy is a promising indicator, but real-world effectiveness is the ultimate measure of a vaccine’s success.
Q 22. How do you address patient concerns or anxieties about injections or vaccinations?
Addressing patient concerns about injections or vaccinations requires empathy, clear communication, and evidence-based information. I begin by actively listening to their anxieties, validating their feelings, and acknowledging that needles can be frightening for many. Then, I explain the procedure in simple terms, using clear and concise language, avoiding medical jargon. I answer their questions honestly and thoroughly, providing evidence-based information about the benefits and risks of the injection or vaccination. For example, if a patient is worried about side effects, I’ll explain the common side effects, their likelihood, and how to manage them. I might share personal anecdotes (with patient permission) about my own vaccination experiences or those of colleagues. Visual aids like brochures or diagrams can also be helpful. Building trust and rapport is key; a calm and reassuring demeanor can significantly alleviate anxieties.
For example, if a patient expresses fear of needles, I might demonstrate the injection site and the process, allowing them to watch the preparation and even practice on a doll or simulated skin. I might also offer relaxation techniques, such as deep breathing exercises, to help them manage their anxiety during the procedure.
Q 23. How do you handle a situation where a patient refuses a vaccination?
When a patient refuses a vaccination, my approach is to respectfully understand their reasons. I begin by engaging in a non-judgmental conversation, actively listening to their concerns and addressing any misconceptions. I provide accurate information about the benefits of vaccination, addressing specific concerns they may have, such as safety, efficacy, or religious beliefs. I present information from reputable sources, such as the CDC or WHO. However, I respect their autonomy and right to refuse medical treatment. I document the conversation, the reasons for refusal, and any information provided. Depending on the context (e.g., workplace mandates, school requirements), I may need to inform the appropriate authorities or discuss alternative solutions, like offering alternative vaccination schedules or exploring potential exemptions based on medical contraindications. The goal is to empower the patient with information, allowing them to make an informed decision, while still respecting their bodily autonomy.
For instance, if a patient expresses concerns about vaccine safety, I would carefully explain the rigorous testing and monitoring processes that vaccines undergo before being approved. If the refusal is based on misinformation, I’ll politely correct the inaccuracies and provide evidence-based counterarguments, referencing reliable sources.
Q 24. Describe your understanding of vaccine schedules and recommendations.
Vaccine schedules and recommendations are established by public health organizations such as the CDC and WHO. These schedules are based on extensive research and epidemiological data, aiming to provide optimal protection against vaccine-preventable diseases at different stages of life. The recommendations are age-specific, considering the immune system’s development and the risks of different diseases at various ages. They also account for the different types of vaccines available, their efficacy, and their safety profile. These schedules are regularly reviewed and updated as new scientific evidence emerges or as disease patterns change. For example, the childhood immunization schedule typically includes vaccines against diseases such as polio, measles, mumps, rubella, and diphtheria, while adult schedules often include vaccines for influenza, tetanus, and shingles. My understanding encompasses the rationale behind each recommendation, the potential benefits and risks associated with each vaccine, and any contraindications that might preclude vaccination. I am well-versed in recognizing and addressing situations requiring individualized vaccination strategies based on patient-specific factors like medical history and travel plans.
Q 25. What is your experience with managing vaccine inventory?
Managing vaccine inventory requires meticulous attention to detail and adherence to strict guidelines. It involves ordering, receiving, storing, and dispensing vaccines according to established protocols. This includes ensuring proper cold chain maintenance, using appropriate storage equipment (refrigerators, freezers), regularly monitoring temperatures, and rotating stock to ensure that vaccines are used within their expiration dates. Accurate record-keeping is crucial, using a computerized inventory management system to track vaccine quantities, lot numbers, expiration dates, and vaccination records. Regular audits are conducted to ensure compliance with regulatory standards and best practices. Waste management also plays a crucial role; I know the processes for handling expired or unusable vaccines according to safety regulations. Proper training on vaccine handling and storage procedures is critical to minimize risks of vaccine degradation and ensure the efficacy and safety of the vaccines administered.
Q 26. How do you stay updated on current recommendations and guidelines for injections and vaccinations?
Staying updated on current recommendations and guidelines is crucial for providing safe and effective care. I regularly consult reputable sources, including the CDC, WHO, and relevant professional organizations (e.g., the Infectious Diseases Society of America). I subscribe to professional journals and newsletters, and actively participate in continuing medical education (CME) activities focused on injection techniques, vaccine updates, and relevant clinical guidelines. This includes attending conferences, webinars, and workshops to remain abreast of new research findings, updated vaccine recommendations, and emerging infectious disease threats. I also engage in peer-to-peer learning and participate in professional discussions to share best practices and address any challenges in keeping up-to-date with the evolving field of injections and vaccinations.
Q 27. Describe your experience with administering medications via injection.
I have extensive experience administering medications via various injection routes, including intramuscular (IM), subcutaneous (SC), and intradermal (ID). I am proficient in selecting the appropriate injection site, needle size, and technique based on the medication, the patient’s age and body habitus, and the injection route. I follow strict aseptic techniques to minimize the risk of infection, ensuring proper hand hygiene and using sterile equipment. I am adept at managing potential complications such as accidental needle sticks or hematomas. I am also trained to recognize and respond to adverse reactions to injections, such as allergic reactions or fainting. I am comfortable administering injections to patients of all ages, from infants to the elderly, adapting my technique as needed. My experience extends to both routine vaccinations and therapeutic injections, and I am familiar with different types of syringes and needles.
Q 28. What is your knowledge of the legal and ethical considerations surrounding injections and vaccinations?
Legal and ethical considerations surrounding injections and vaccinations are multifaceted. Legally, healthcare providers must adhere to all relevant laws and regulations concerning informed consent, patient privacy (HIPAA), and the proper handling and storage of vaccines. Ethical considerations involve respecting patient autonomy, ensuring informed consent before any procedure, maintaining patient confidentiality, and providing evidence-based care. The principle of beneficence requires us to act in the best interest of the patient, while non-maleficence demands we do no harm. Justice mandates fair and equitable access to vaccinations for all patients, regardless of socioeconomic status or other factors. Understanding and upholding these principles is paramount in my practice. Furthermore, I am aware of potential legal ramifications related to vaccine adverse events and the importance of proper documentation and reporting procedures. I am very familiar with the legal implications of mandatory vaccination policies in various settings, such as schools and workplaces, and the exceptions allowed based on medical or religious grounds.
Key Topics to Learn for Injections and Vaccinations Interviews
- Anatomy and Physiology of Injection Sites: Understanding the different injection sites (intramuscular, subcutaneous, intradermal), their anatomical landmarks, and associated risks.
- Injection Techniques: Mastering the proper techniques for each injection type, including needle selection, aspiration (where applicable), and injection angles. Practical application involves demonstrating proficiency and understanding the rationale behind each step.
- Vaccine Storage and Handling: Knowledge of proper vaccine storage temperatures, expiry dates, and handling procedures to maintain vaccine potency and safety.
- Vaccine Schedules and Recommendations: Familiarity with common vaccine schedules for different age groups and populations, and understanding the rationale behind recommended vaccination strategies.
- Adverse Events and Management: Recognizing and managing potential adverse events following injections or vaccinations, including immediate and delayed reactions. Problem-solving here involves quick thinking and appropriate response protocols.
- Infection Control and Prevention: Strict adherence to infection control protocols to prevent the transmission of infectious diseases during injection procedures. This includes understanding sterilization techniques and proper disposal of sharps.
- Pharmacology of Vaccines: Understanding the different types of vaccines (live attenuated, inactivated, etc.) and their mechanisms of action.
- Legal and Ethical Considerations: Knowledge of relevant regulations, consent procedures, and ethical considerations related to vaccinations.
- Documentation and Record Keeping: Accurate and complete documentation of all vaccination procedures, including patient information, vaccine details, and any adverse events.
Next Steps
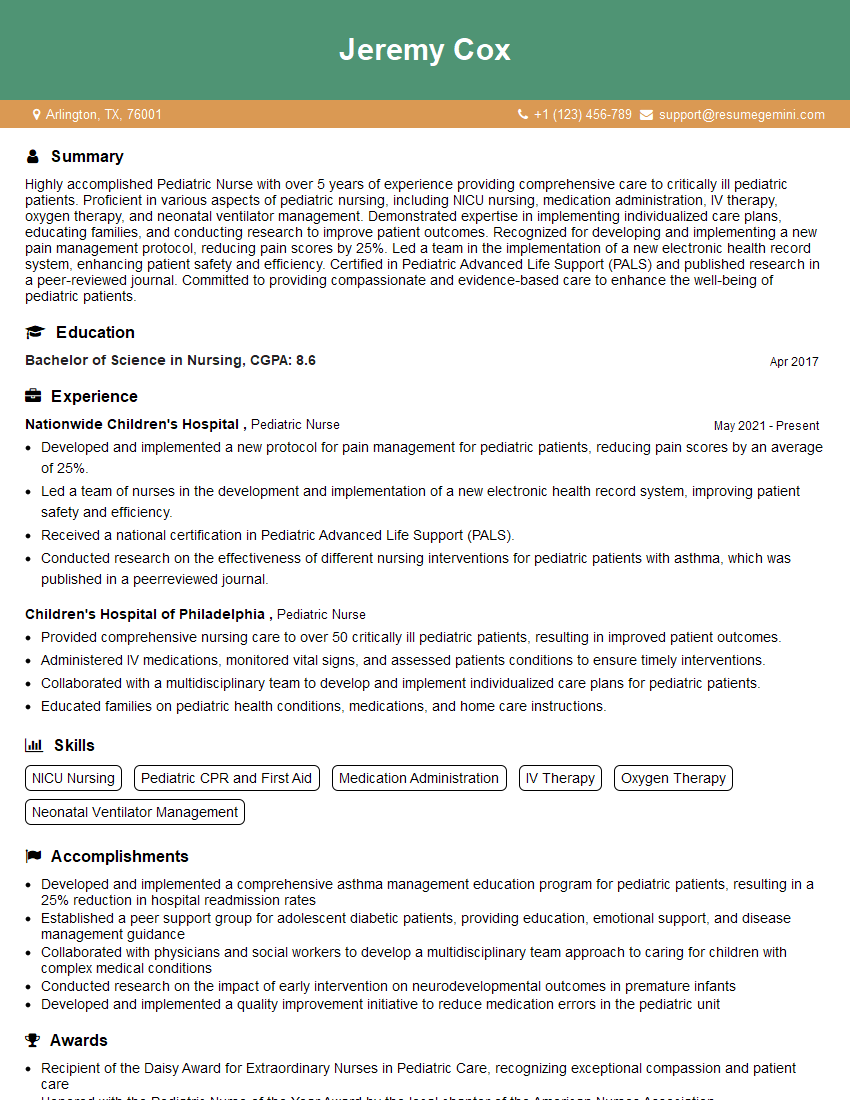
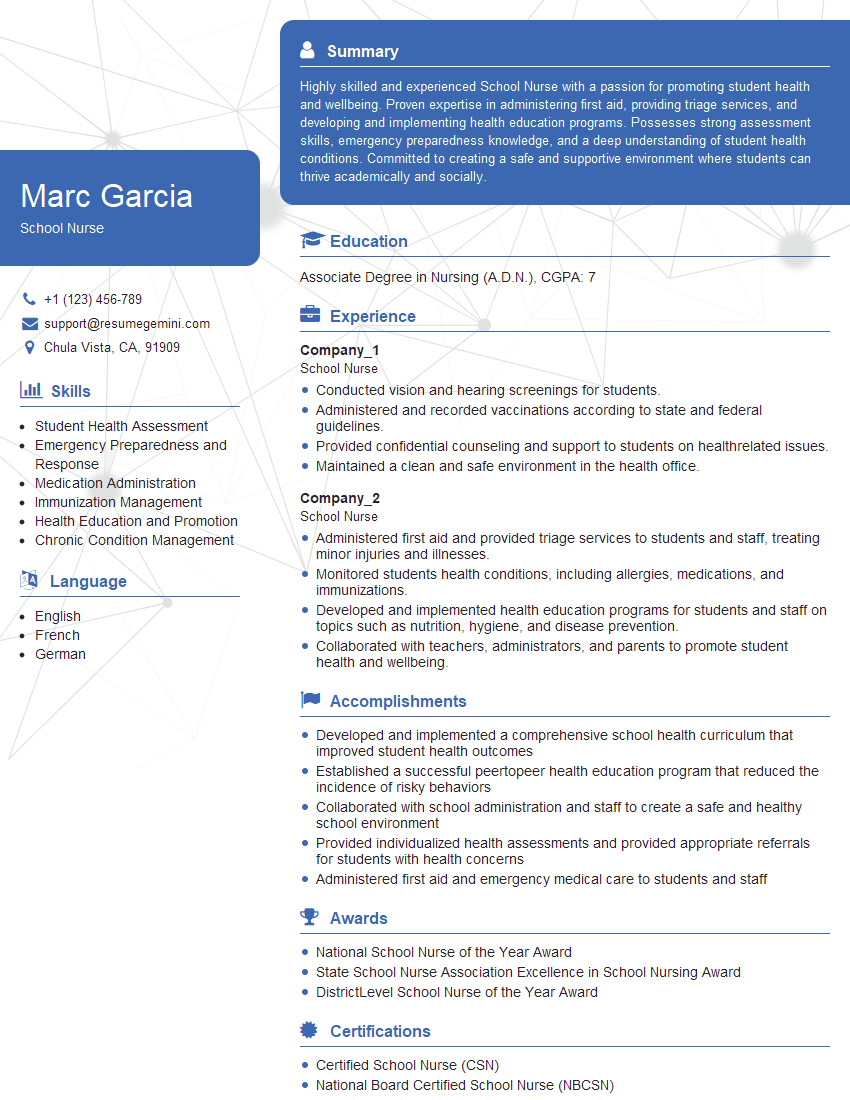
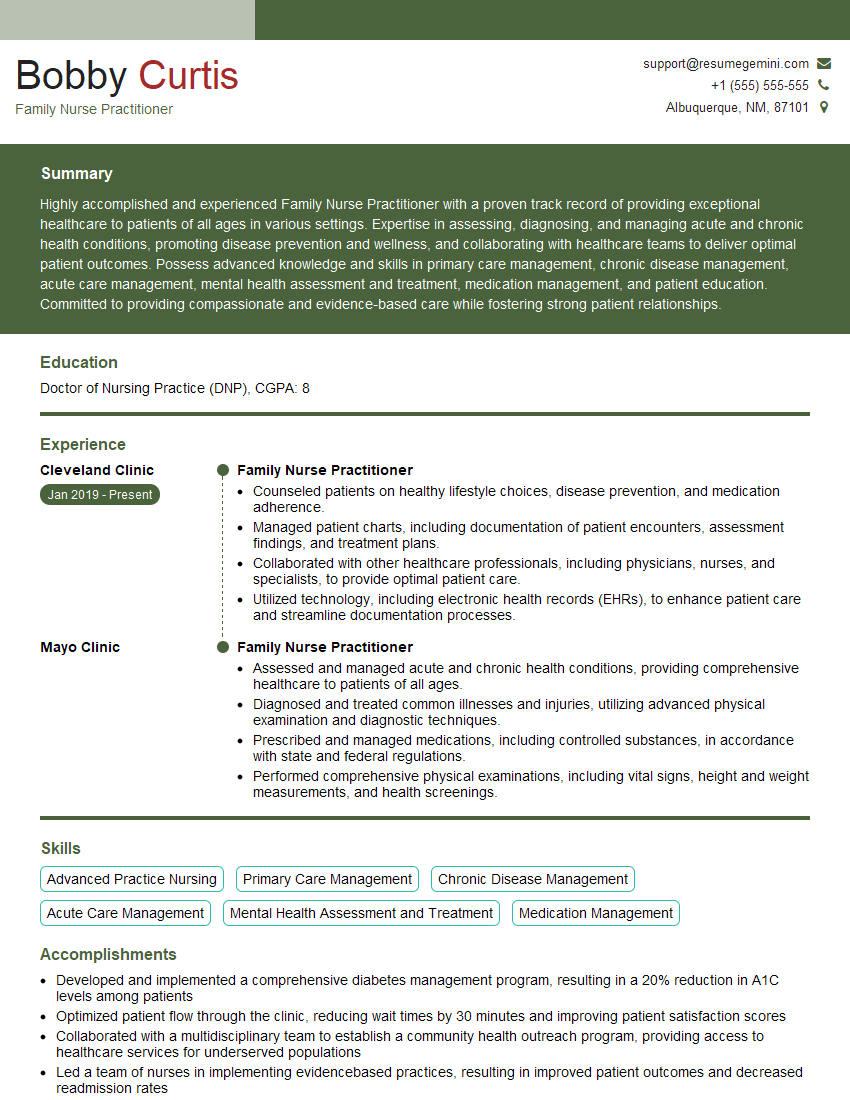
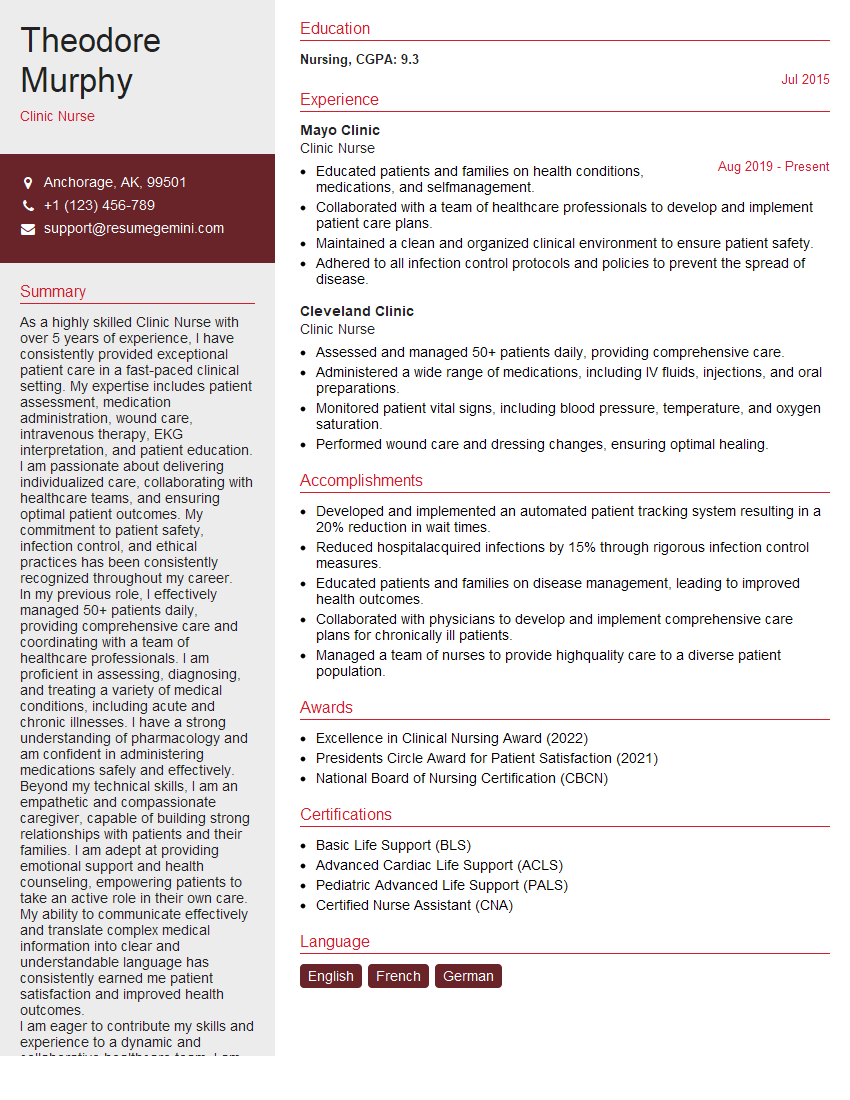
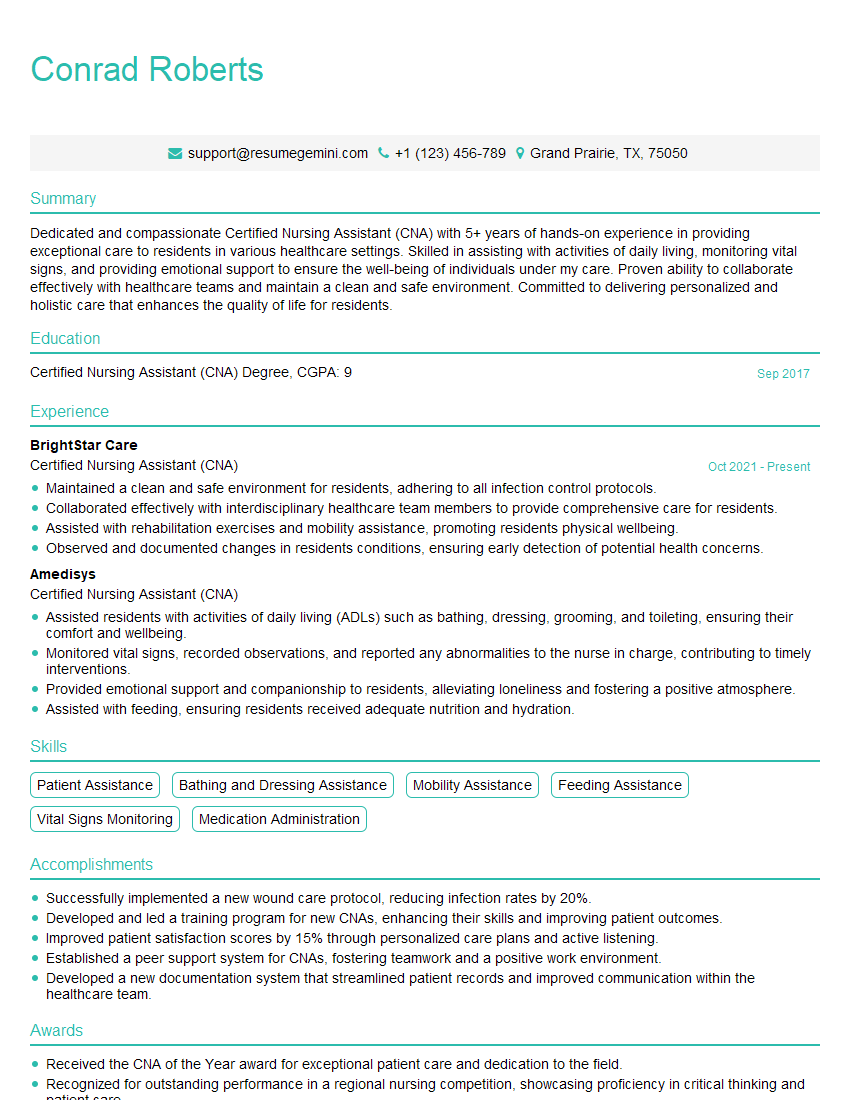
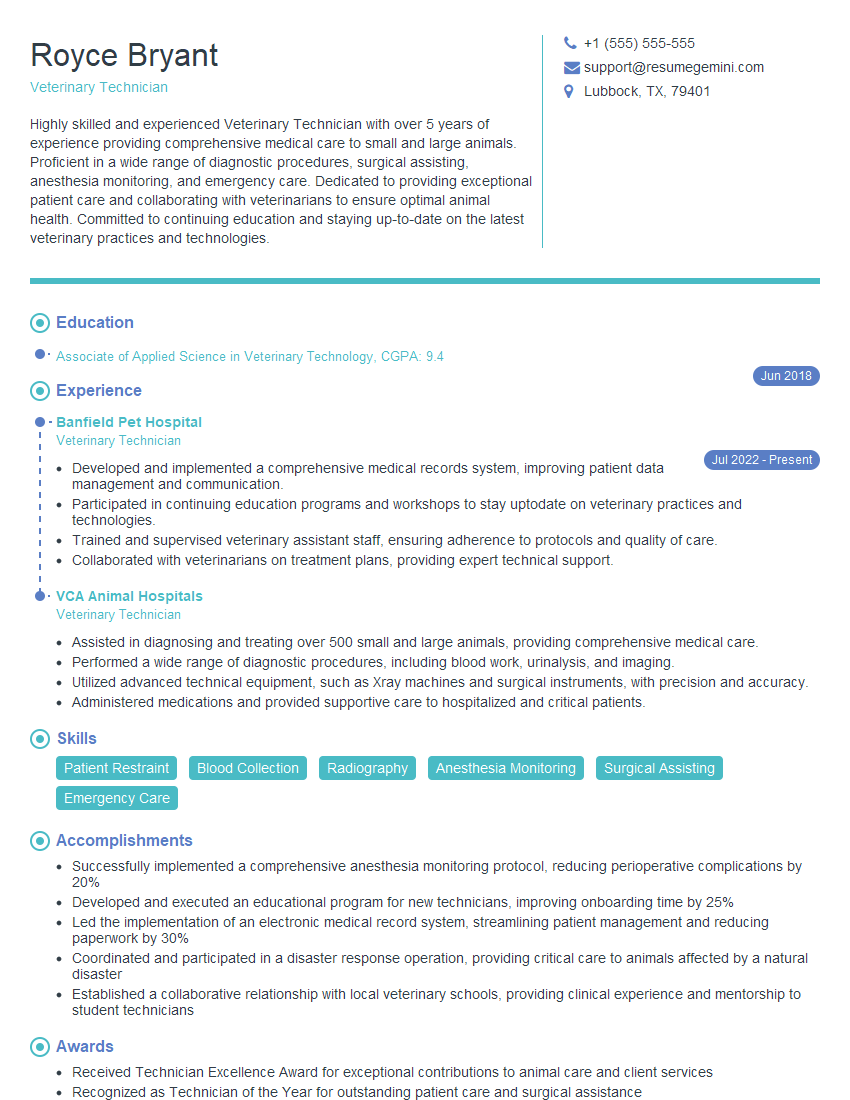
Mastering the intricacies of injections and vaccinations significantly enhances your career prospects in healthcare. A strong understanding of these procedures demonstrates competence and commitment to patient safety, opening doors to a wider range of roles and opportunities. To maximize your chances of landing your dream job, focus on crafting an ATS-friendly resume that effectively highlights your skills and experience. ResumeGemini is a trusted resource to help you build a professional and impactful resume. We provide examples of resumes tailored specifically to the Injections and Vaccinations field to help you get started.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
There are no reviews yet. Be the first one to write one.