The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Health Science Technology interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Health Science Technology Interview
Q 1. Describe your experience with Electronic Health Records (EHR) systems.
My experience with Electronic Health Records (EHR) systems spans over eight years, encompassing implementation, optimization, and data analysis across various healthcare settings. I’ve worked extensively with systems like Epic, Cerner, and Meditech, gaining hands-on experience with everything from user training and workflow design to data extraction and reporting. For instance, at my previous role, I led a project to optimize the medication reconciliation process within our EHR, resulting in a 15% reduction in medication errors. This involved analyzing current workflows, identifying bottlenecks, and re-designing processes within the EHR system. Another key experience involved developing custom reports to track key performance indicators (KPIs) related to patient satisfaction and care quality, directly utilizing the EHR’s reporting capabilities. I’m proficient in using EHR systems to access patient data securely and responsibly, adhering to all relevant regulations and best practices.
Q 2. Explain the principles of HIPAA compliance in a healthcare IT setting.
HIPAA compliance is paramount in healthcare IT. It’s a federal law that protects the privacy and security of Protected Health Information (PHI). The core principles revolve around ensuring confidentiality, integrity, and availability of PHI. Confidentiality means only authorized individuals can access PHI. Integrity ensures the accuracy and completeness of the data. Availability guarantees timely and reliable access to the information when needed. To achieve HIPAA compliance, we employ various measures, such as access control through role-based permissions, data encryption both in transit and at rest, regular security audits, employee training on HIPAA regulations, and robust incident response plans. For example, implementing multi-factor authentication prevents unauthorized access even if usernames and passwords are compromised. We also use data loss prevention (DLP) tools to monitor and prevent sensitive data from leaving the network without proper authorization. Failure to comply with HIPAA can result in severe penalties, including hefty fines and legal repercussions.
Q 3. What are your experiences with different medical imaging modalities?
My experience with medical imaging modalities includes extensive work with X-ray, CT, MRI, Ultrasound, and PET scans. I’ve worked with Picture Archiving and Communication Systems (PACS) to manage, store, and retrieve medical images. I understand the technical aspects of each modality, including image acquisition, processing, and interpretation. For example, in a previous project, I worked on optimizing the workflow for image transfer between different departments, significantly reducing turnaround times for radiology reports. My understanding extends to the different file formats associated with each modality like DICOM and the importance of ensuring image quality and maintaining metadata integrity. This experience has equipped me with the necessary skills to understand and address challenges associated with image storage, retrieval, and analysis, utilizing appropriate PACS and image processing software.
Q 4. How would you approach the integration of a new medical device into a hospital’s existing infrastructure?
Integrating a new medical device requires a systematic approach. First, we conduct a thorough needs assessment to determine if the device aligns with the hospital’s strategic goals and clinical needs. Next, we evaluate the device’s technical specifications to ensure compatibility with the existing infrastructure, including network bandwidth, security protocols, and EHR integration. A critical step is to assess the device’s cybersecurity features to minimize vulnerabilities and ensure PHI protection. This often involves collaborating with the vendor and IT security teams to implement appropriate safeguards. Then, we develop a comprehensive implementation plan, including timelines, resource allocation, and user training. Thorough testing in a controlled environment is crucial before deploying the device hospital-wide. Finally, we monitor post-implementation performance and gather feedback from clinicians to optimize its use and identify any potential issues. The entire process is documented meticulously, adhering to regulatory compliance requirements.
Q 5. What are the key differences between various data analysis techniques used in healthcare?
Healthcare data analysis utilizes a variety of techniques depending on the research question. Descriptive statistics summarize data using measures like mean, median, and standard deviation; helpful for understanding basic patient characteristics. Inferential statistics allow us to draw conclusions about a population based on a sample. Regression analysis helps model the relationships between variables, for instance, predicting patient outcomes based on risk factors. Machine learning algorithms, such as decision trees or neural networks, are employed for complex prediction tasks, like disease diagnosis or risk stratification. For example, logistic regression can predict the probability of a patient developing a specific disease, while a random forest model might improve diagnostic accuracy. The choice of method depends heavily on the type of data and the objective of the analysis. It’s important to validate any analytical model to ensure its reliability and generalizability to new data.
Q 6. Describe your experience with data mining and its applications in healthcare.
My experience in data mining in healthcare focuses on extracting meaningful insights from large datasets to improve patient care and operational efficiency. I’ve used data mining techniques to identify patterns in patient data, predicting readmission rates, optimizing resource allocation, and identifying potential outbreaks. For example, I used association rule mining to identify combinations of medications and diagnoses associated with increased risk of adverse drug events. Another project involved using clustering algorithms to segment patients into distinct groups based on their clinical characteristics and treatment responses, enabling more personalized medicine approaches. Data mining requires robust data preprocessing and cleaning, followed by the appropriate application of analytical techniques, and careful interpretation of results. Ethical considerations around data privacy and patient confidentiality are always prioritized during data mining projects.
Q 7. How familiar are you with different programming languages used in Health Science Technology?
My programming skills are a valuable asset in health science technology. I’m proficient in Python, R, and SQL. Python is widely used for data analysis, machine learning, and developing healthcare applications. I leverage its libraries like Pandas, NumPy, and Scikit-learn for data manipulation, statistical analysis, and model building. R is another essential tool for statistical computing and data visualization in healthcare research. SQL is indispensable for managing and querying data stored in relational databases like those used in EHR systems. I’ve also worked with Java for developing some healthcare applications. This diverse skill set allows me to efficiently extract, analyze and interpret data, build predictive models, and develop applications to support better decision making in healthcare settings.
Q 8. Explain the concept of telehealth and its potential challenges.
Telehealth uses technology to deliver healthcare services remotely. Think of it as a virtual doctor’s visit, allowing patients to connect with healthcare providers through video conferencing, phone calls, or even remote patient monitoring devices. This expands access to care, especially for those in rural areas or with mobility limitations.
However, telehealth isn’t without its challenges. Accessibility is a key issue; not everyone has reliable internet access or the necessary technology. Data security and privacy are paramount concerns, as sensitive patient information is transmitted electronically. Regulatory compliance varies across regions, adding complexity to implementation. Finally, reimbursement models can be challenging to navigate, affecting provider participation and patient affordability.
For example, a patient in a remote village might utilize telehealth to consult a specialist located in a major city, saving significant travel time and cost. However, if the patient lacks reliable internet, the consultation becomes impossible. Similarly, ensuring secure transmission of medical images requires robust cybersecurity measures to prevent breaches.
Q 9. Describe your experience with cybersecurity protocols in healthcare.
My experience with cybersecurity protocols in healthcare encompasses implementing and auditing HIPAA compliant systems, conducting risk assessments, and responding to security incidents. I’ve worked with various security tools, including firewalls, intrusion detection systems, and data loss prevention solutions. I am also proficient in implementing and managing access control lists (ACLs) to restrict access to sensitive patient data based on the principle of least privilege. I have personally been involved in developing and implementing security awareness training programs for healthcare professionals to minimize human error, a significant vulnerability in any system.
A specific example involves a situation where we detected an attempted phishing attack targeting our healthcare system. By promptly implementing multi-factor authentication and conducting thorough security awareness training, we were able to prevent a data breach. We also routinely perform penetration testing to identify and address vulnerabilities before they can be exploited.
Q 10. How would you troubleshoot a malfunctioning medical device?
Troubleshooting a malfunctioning medical device requires a systematic approach. First, I’d ensure patient safety by disconnecting the device if necessary. Then, I’d carefully review the device’s error messages and logs. This often provides clues about the nature of the problem. Next, I’d check the device’s connections, power supply, and any external peripherals. Simple issues like loose cables or power outages are surprisingly common causes of malfunctions. If the problem persists, I’d consult the device’s maintenance manual and troubleshooting guide. If the manual doesn’t resolve the issue, I’d contact the manufacturer’s technical support for assistance. In some cases, a site visit from a qualified biomedical engineer may be required for more complex repairs.
For instance, if an infusion pump displays a ‘low battery’ error, I’d first verify the battery level and then check the power cord connection. If the problem is more complex, such as an intermittent malfunction, I’d carefully document all observations and contact the manufacturer’s support team, potentially initiating the return of the device for repair or replacement.
Q 11. What is your experience with regulatory compliance for medical devices?
My experience with regulatory compliance for medical devices centers around FDA regulations (in the US) and other international standards such as ISO 13485. This includes understanding and adhering to requirements for design controls, risk management (e.g., using ISO 14971), and post-market surveillance. I’m familiar with the process of obtaining 510(k) clearances or PMA approvals for new devices and ensuring ongoing compliance with relevant regulations. This includes documentation, testing, and record-keeping to maintain a comprehensive audit trail.
In a past project, we successfully navigated the 510(k) process for a novel medical device, meticulously documenting every stage from design validation and verification to risk assessment and clinical trials. We maintained rigorous documentation to ensure compliance with all relevant FDA regulations. Maintaining this documentation allows for timely responses to audits and helps prevent costly delays or non-compliance issues.
Q 12. Explain the importance of data integrity in healthcare.
Data integrity in healthcare is crucial because it ensures the accuracy, completeness, consistency, and trustworthiness of patient data. This is fundamental for effective diagnosis, treatment, and research. Inaccurate or incomplete data can lead to misdiagnosis, inappropriate treatment, and flawed research outcomes, all with potentially devastating consequences for patient safety and the advancement of medical knowledge. Maintaining data integrity involves using robust data governance processes, implementing validation checks, and establishing procedures for data correction and reconciliation.
Imagine a scenario where a patient’s allergy information is missing from their electronic health record (EHR). This could lead to a potentially fatal adverse reaction if a medication containing that allergen is prescribed. Maintaining data integrity, in this instance, prevents such catastrophes.
Q 13. How do you ensure patient data privacy and security?
Ensuring patient data privacy and security requires a multi-faceted approach. This starts with implementing robust security measures like encryption, access controls, and regular security audits. We must adhere strictly to regulations like HIPAA (in the US) and GDPR (in Europe), which dictate how patient data is handled, stored, and shared. Employee training is crucial to ensure everyone understands their responsibilities in protecting patient information. Furthermore, utilizing technologies such as data masking and anonymization can enhance privacy without compromising the integrity of data used for research or analysis.
For example, we might use strong encryption to protect data at rest and in transit, coupled with multi-factor authentication to restrict access to sensitive systems. Regular security audits ensure our systems remain compliant and vulnerabilities are identified and addressed promptly.
Q 14. Describe your experience with clinical trial data management.
My experience in clinical trial data management involves the entire data lifecycle, from study design and data collection to analysis and reporting. I’m proficient in using electronic data capture (EDC) systems and data management tools to streamline data collection, validation, and quality control. This includes developing data management plans, creating case report forms (CRFs), managing data queries, and ensuring data integrity. I’ve worked on both small-scale and large-scale clinical trials, across various therapeutic areas, and possess a strong understanding of Good Clinical Practice (GCP) guidelines.
In a recent project, we used an EDC system to collect data from multiple clinical trial sites globally. We implemented rigorous data validation rules to minimize errors and ensure data accuracy. We then utilized statistical analysis software to analyze the data and generate reports to support regulatory submissions. The successful completion of this trial, on time and within budget, underscores the importance of efficient data management.
Q 15. How would you handle a data breach in a healthcare setting?
Handling a data breach in healthcare requires a swift, organized, and compliant response. It’s not just about fixing the technical issue; it’s about minimizing harm to patients and the organization’s reputation. My approach follows a structured plan:
- Containment: Immediately isolate the affected systems to prevent further data exfiltration. This involves disabling network access, shutting down affected servers, and potentially quarantining affected devices.
- Identification: Determine the scope of the breach – what data was compromised, how many individuals are affected, and the potential impact. This often involves forensic analysis.
- Notification: Notify affected individuals, regulatory bodies (like HIPAA in the US), and law enforcement as required. Transparency is crucial, even though it’s legally complex.
- Remediation: Repair the vulnerabilities that led to the breach. This might include patching software, improving security protocols, and retraining staff. I’d prioritize implementing multi-factor authentication and robust access control measures.
- Recovery: Restore systems to their operational state and implement measures to prevent future breaches. This includes rigorous testing and validation of restored systems.
- Review and Improvement: Conduct a thorough post-incident review to identify lessons learned and strengthen the organization’s security posture. This involves documenting the incident response, updating security policies, and conducting employee training.
For example, during a breach involving patient medical records, we would need to immediately inform patients and the Office for Civil Rights (OCR) under HIPAA. We’d then work to understand the extent of the breach, possibly using threat intelligence to identify the actor and the attack vector, to prevent future occurrences.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your understanding of different healthcare data models.
Healthcare data models are crucial for organizing and managing patient information effectively. Different models cater to various needs and data structures. Some common ones include:
- Relational Models: These use tables with rows and columns to represent data, linked through relationships. Examples include using SQL databases to store patient demographics, diagnoses, and treatment history. They’re good for structured data but can be inefficient for complex relationships.
- NoSQL Models: These are non-relational databases, often used for unstructured or semi-structured data like images, text notes, and sensor readings. Document databases (like MongoDB), key-value stores, and graph databases are examples. They offer scalability and flexibility for handling large datasets.
- HL7 FHIR (Fast Healthcare Interoperability Resources): This is a standardized data model specifically designed for healthcare interoperability. It uses a RESTful API to exchange data between different systems, allowing seamless communication between hospitals, labs, and other healthcare providers. It improves data sharing and reduces redundancies.
- OMOP (Observational Medical Outcomes Partnership) Common Data Model (CDM): This standardized data model facilitates large-scale observational studies and comparative effectiveness research. It maps diverse healthcare data sources into a common format, allowing researchers to analyze data across multiple institutions.
The choice of data model depends on the specific use case and the type of data being handled. A hospital’s electronic health record (EHR) might use a combination of relational and NoSQL databases to manage both structured patient information and unstructured data like medical images.
Q 17. Describe your familiarity with big data analytics in healthcare.
Big data analytics in healthcare leverages advanced computing techniques to analyze massive datasets to identify patterns, predict outcomes, and improve patient care. It’s transforming healthcare by:
- Improving Diagnostics: Analyzing medical images (like X-rays and CT scans) to detect diseases earlier and more accurately.
- Personalizing Treatment: Tailoring treatment plans to individual patients based on their genetic makeup, medical history, and lifestyle factors.
- Predicting Outcomes: Identifying patients at high risk of developing certain conditions, allowing for proactive interventions.
- Optimizing Operations: Analyzing hospital workflows and resource utilization to improve efficiency and reduce costs.
- Drug Discovery and Development: Accelerating the research and development of new drugs and therapies.
Techniques like machine learning, deep learning, and natural language processing are employed. For example, a machine learning model could be trained on millions of patient records to predict the likelihood of readmission after a heart attack, allowing hospitals to implement preventive measures.
Q 18. How would you improve the efficiency of a healthcare IT system?
Improving the efficiency of a healthcare IT system requires a multi-faceted approach focused on both technology and workflow optimization. Here are key strategies:
- System Integration: Integrate disparate systems to avoid data silos and reduce manual data entry. This often involves using HL7 FHIR or other interoperability standards.
- Workflow Optimization: Analyze existing workflows to identify bottlenecks and inefficiencies. Streamline processes through automation and improved user interfaces.
- Data Analytics: Utilize data analytics to identify trends and patterns that can inform decision-making and resource allocation.
- User Training and Support: Provide comprehensive training to healthcare professionals on how to effectively use the IT system. Offer ongoing support to address any issues or questions.
- Regular Maintenance and Upgrades: Implement a schedule for regular system maintenance, software updates, and security patches to ensure optimal performance and security.
- Cloud Computing: Consider migrating to a cloud-based solution for improved scalability, cost-effectiveness, and accessibility.
For instance, implementing a computerized physician order entry (CPOE) system can significantly reduce medication errors by automating the ordering and dispensing process. Real-time data analytics can identify potential staffing shortages before they occur, allowing for proactive scheduling adjustments.
Q 19. What are your experiences with different types of medical sensors and their applications?
My experience encompasses various medical sensors and their applications. These devices play a critical role in remote patient monitoring, diagnostics, and treatment:
- Wearable Sensors: These include smartwatches, fitness trackers, and ECG patches that monitor heart rate, activity levels, sleep patterns, and other vital signs. Applications range from general wellness tracking to managing chronic conditions like heart failure.
- Implantable Sensors: These are surgically implanted devices, such as pacemakers and insulin pumps, that provide continuous monitoring and therapy delivery. They are crucial for managing life-threatening conditions.
- Imaging Sensors: These include ultrasound probes, X-ray detectors, and MRI scanners that produce images of the internal organs and tissues. They are essential for diagnosing a wide range of diseases.
- Biosensors: These devices measure biological markers in blood, saliva, or other bodily fluids. Examples include glucose sensors for diabetics and blood oxygen sensors for patients with respiratory problems.
I’ve worked on projects involving the integration of sensor data into electronic health records (EHRs), enabling clinicians to access real-time patient information and make more informed decisions. For example, I worked on a project using wearable sensors to monitor patients with congestive heart failure, allowing for early detection of worsening symptoms and timely interventions.
Q 20. What is your understanding of the Internet of Medical Things (IoMT)?
The Internet of Medical Things (IoMT) is a network of medical devices, software applications, and other healthcare systems connected through the internet. It’s transforming healthcare by enabling remote patient monitoring, improved diagnostics, and more efficient care delivery. Key components include:
- Wearable and Implantable Sensors: These collect patient data remotely and transmit it to healthcare providers.
- Smart Medical Devices: These devices are connected to the internet and can communicate with other devices and systems.
- Data Analytics Platforms: These platforms analyze data from IoMT devices to identify trends, predict outcomes, and improve patient care.
- Cloud-Based Platforms: These platforms provide secure storage and processing of IoMT data.
The IoMT raises important security and privacy concerns. Robust security measures are crucial to protect patient data from unauthorized access and cyberattacks. For instance, secure data transmission protocols and strong authentication mechanisms are essential.
Q 21. Explain your experience with predictive analytics in healthcare.
Predictive analytics in healthcare uses historical data and advanced statistical techniques to anticipate future health outcomes. This allows for proactive interventions and improved resource allocation. My experience involves developing and deploying models that:
- Predict hospital readmissions: Identifying patients at high risk of readmission allows for targeted interventions to reduce readmission rates.
- Forecast disease outbreaks: Analyzing epidemiological data to predict the likelihood of outbreaks allows for proactive resource allocation and public health interventions.
- Personalize treatment plans: Identifying patients who are likely to respond well to specific treatments allows for more effective treatment strategies.
- Optimize resource allocation: Predicting patient volume and resource needs allows for more efficient staffing and resource allocation.
For example, I developed a machine learning model that predicted the likelihood of heart failure readmissions with 85% accuracy. This model considered factors like age, medical history, and medication adherence. The insights from this model were used to develop a targeted intervention program that resulted in a significant reduction in readmission rates.
Q 22. Describe your understanding of artificial intelligence applications in healthcare.
Artificial intelligence (AI) is rapidly transforming healthcare, offering numerous applications across various domains. It’s not just about robots performing surgery; AI encompasses a wide range of tools and techniques designed to improve efficiency, accuracy, and patient care.
- Diagnosis and Treatment: AI algorithms can analyze medical images (X-rays, CT scans, MRIs) to detect anomalies like tumors or fractures with greater speed and accuracy than humans alone. For example, AI-powered systems are used to screen for diabetic retinopathy, a leading cause of blindness.
- Drug Discovery and Development: AI accelerates drug discovery by predicting the effectiveness of potential drug candidates, reducing the time and cost associated with traditional methods. Machine learning can analyze vast datasets of molecular structures and biological information to identify promising drug targets.
- Personalized Medicine: AI enables personalized treatment plans by analyzing a patient’s genetic profile, lifestyle, and medical history to predict the most effective course of treatment. This helps tailor interventions to individual needs, increasing treatment success and reducing adverse effects.
- Administrative Tasks: AI can automate administrative tasks such as scheduling appointments, managing medical records, and billing, freeing up healthcare professionals to focus on patient care. Chatbots can also answer frequently asked questions, providing 24/7 support.
- Predictive Analytics: AI can analyze patient data to predict the likelihood of future health problems, allowing for proactive interventions to prevent hospital readmissions or manage chronic conditions more effectively. For instance, predicting potential heart failure based on electronic health record data.
The use of AI in healthcare raises ethical considerations such as data privacy, algorithmic bias, and the role of human oversight. However, its potential benefits in improving patient outcomes and efficiency are undeniable.
Q 23. How familiar are you with different types of healthcare databases?
My familiarity with healthcare databases is extensive. I’m proficient in working with various types, each with its own structure and purpose:
- Electronic Health Records (EHRs): These are the core repositories of patient information, containing medical history, diagnoses, medications, lab results, and more. Examples include Epic, Cerner, and Meditech. They are typically relational databases.
- Clinical Data Warehouses (CDWs): These integrate data from multiple sources within a healthcare organization (EHRs, billing systems, etc.) to provide a comprehensive view of patient data for analysis and reporting. They often employ dimensional modeling.
- Claims Databases: These contain information about healthcare claims submitted for reimbursement by providers. Analyzing claims data is crucial for understanding healthcare utilization and costs.
- Public Health Databases: These databases, maintained at local, state, or national levels, contain epidemiological data, disease surveillance information, and other public health statistics. Examples include the CDC’s databases.
- Research Databases: These databases often contain anonymized or de-identified patient data for research purposes. They may be relational, NoSQL, or a hybrid, depending on the type of research.
Understanding the nuances of each database type is essential for effective data analysis, reporting, and decision-making in healthcare. The ability to query and manipulate data within these systems is critical for my role.
Q 24. Explain the process of data validation and cleaning in a healthcare setting.
Data validation and cleaning are crucial steps in ensuring the accuracy and reliability of healthcare data. Inaccurate data can lead to incorrect diagnoses, ineffective treatments, and even patient harm. The process typically involves several stages:
- Data Identification and Collection: The first step is to identify the data sources and collect the necessary data. This may involve extracting data from EHRs, claims databases, or other sources.
- Data Validation: This involves checking the data for accuracy, completeness, and consistency. This might include checking for missing values, duplicate entries, and inconsistencies between different data fields. Range checks (e.g., ensuring age is within a reasonable range) and format checks (e.g., ensuring dates are in the correct format) are important aspects.
- Data Cleaning: This involves correcting or removing errors and inconsistencies identified during validation. Techniques include imputation (filling in missing values based on statistical methods), outlier analysis (identifying and handling extreme values), and data standardization (converting data into a consistent format). This step requires careful consideration of potential biases introduced by different cleaning methods.
- Data Transformation: Often, data needs to be transformed to fit a specific analysis or reporting need. This can involve aggregation, summarization, or creating new variables from existing ones. For example, calculating body mass index (BMI) from weight and height data.
- Data Verification: After cleaning and transformation, the data should be verified to ensure the accuracy and reliability of the results. This might involve comparing cleaned data with original sources or performing independent checks.
For instance, in a study on diabetes prevalence, we might validate age data to ensure it’s within a realistic range, and clean up inconsistencies in diabetes diagnosis codes. Robust data validation and cleaning are paramount for maintaining high-quality data for research and clinical decision-making.
Q 25. How do you manage competing priorities in a fast-paced healthcare environment?
Healthcare is inherently fast-paced and demands efficient prioritization. I use a combination of strategies to manage competing priorities:
- Prioritization Frameworks: I leverage frameworks like the Eisenhower Matrix (urgent/important) to categorize tasks and focus on high-impact activities first. This ensures that critical tasks are addressed promptly.
- Time Management Techniques: I utilize time blocking, setting aside specific time slots for different tasks. This improves focus and reduces context switching, resulting in enhanced efficiency.
- Effective Communication: Open communication with stakeholders is crucial. This ensures clear expectations and allows for proactive adjustment of priorities as new information emerges or urgent issues arise. Transparent communication helps prevent conflicts and delays.
- Delegation: When appropriate, I delegate tasks to others based on their skills and availability. This frees up my time to concentrate on more complex or critical issues.
- Regular Review and Adjustment: I regularly review my progress and adjust priorities as needed. This ensures that I remain adaptable and responsive to changes in the healthcare environment.
For example, if I have competing deadlines for a project and an urgent patient care request, the patient care request will take precedence. Clear communication with project stakeholders will allow me to manage expectations and find ways to minimize delays on the project without compromising patient care.
Q 26. Describe a time you had to troubleshoot a complex technical issue in a healthcare setting.
During a system upgrade of our EHR system, we encountered a critical issue where patient data wasn’t syncing correctly between the old and new systems. This resulted in incomplete patient records and delayed access to vital information. My role involved investigating the root cause and implementing a solution.
My troubleshooting involved the following steps:
- Problem Definition: We precisely defined the scope of the problem, focusing on specific symptoms and their impact on patient care. We identified the affected systems and the timeframe of the issue.
- Data Analysis: We analyzed logs from both systems to pinpoint the point of failure. We reviewed configuration files and database integrity.
- Hypothesis Generation: We formulated hypotheses regarding the root cause, considering potential conflicts between software versions, data inconsistencies, and network connectivity issues.
- Testing and Verification: We systematically tested each hypothesis using simulations and controlled environments. We ruled out potential causes one by one, isolating the problem to a specific data mapping error in the upgrade script.
- Solution Implementation: We implemented a hotfix to correct the data mapping error. We tested the fix rigorously in a controlled environment before deploying it to the live system.
- Monitoring and Prevention: After resolving the issue, we established better monitoring tools to prevent similar problems in the future. We included comprehensive testing procedures for subsequent upgrades.
This experience underscored the importance of thorough testing and robust monitoring in a healthcare setting, where even minor technical issues can have significant consequences.
Q 27. How would you explain a complex technical issue to a non-technical audience?
Explaining complex technical issues to a non-technical audience requires clear and concise communication, avoiding jargon. I use a few key techniques:
- Analogies and Metaphors: I relate technical concepts to everyday experiences. For example, explaining a network connection using the analogy of a road system helps visualize data flow.
- Visual Aids: Diagrams, flowcharts, and simple illustrations are invaluable in simplifying complex processes. A visual representation can make abstract concepts more accessible.
- Step-by-Step Explanations: Breaking down complex procedures into manageable steps makes the information easier to understand and follow. This avoids overwhelming the audience with too much information at once.
- Focus on Impact: I emphasize the practical implications of the issue and how the proposed solution will improve things. This makes the explanation more relevant and engaging.
- Active Listening and Feedback: I encourage questions and feedback throughout the explanation, addressing any misunderstandings or concerns promptly. This ensures everyone is on the same page.
For instance, if I’m explaining a database error, I might use the analogy of a library’s card catalog being misfiled. This instantly helps the audience grasp the concept of disorganization and its implications on data retrieval.
Q 28. What are your salary expectations?
My salary expectations are commensurate with my experience and skills in Health Science Technology, and are in line with the industry standard for similar roles. I’m open to discussing a competitive compensation package that reflects my value to the organization.
To provide a more precise figure, I’d need more details about the specific responsibilities, benefits, and overall compensation structure of the position. I am confident that we can reach a mutually agreeable salary range that reflects the value I will bring to your team.
Key Topics to Learn for Health Science Technology Interview
- Medical Imaging and Informatics: Understanding PACS systems, DICOM standards, image processing techniques, and the role of AI in medical imaging analysis. Practical application: Describe your experience with analyzing medical images or working with image management systems.
- Health Data Analytics: Mastering data mining, statistical analysis, and visualization techniques to extract meaningful insights from patient data. Practical application: Explain how you would approach identifying trends in a large healthcare dataset.
- Electronic Health Records (EHR) Systems: Familiarize yourself with different EHR platforms, their functionalities, and data security protocols. Practical application: Discuss your understanding of data integrity and patient privacy within EHR systems.
- Health Information Exchange (HIE): Learn about the principles and benefits of HIE, including interoperability standards and data sharing best practices. Practical application: Explain how HIE can improve patient care coordination.
- Biomedical Instrumentation: Understand the principles of operation and maintenance of various biomedical devices, including diagnostic and therapeutic equipment. Practical application: Describe your troubleshooting experience with biomedical devices.
- Healthcare Cybersecurity: Familiarize yourself with HIPAA regulations and best practices for protecting sensitive patient data in healthcare settings. Practical application: Discuss your understanding of cybersecurity threats and mitigation strategies in healthcare.
- Telehealth Technology: Understand the technology and infrastructure supporting telehealth, including video conferencing, remote patient monitoring, and data security considerations. Practical application: Discuss the advantages and challenges of implementing telehealth solutions.
Next Steps
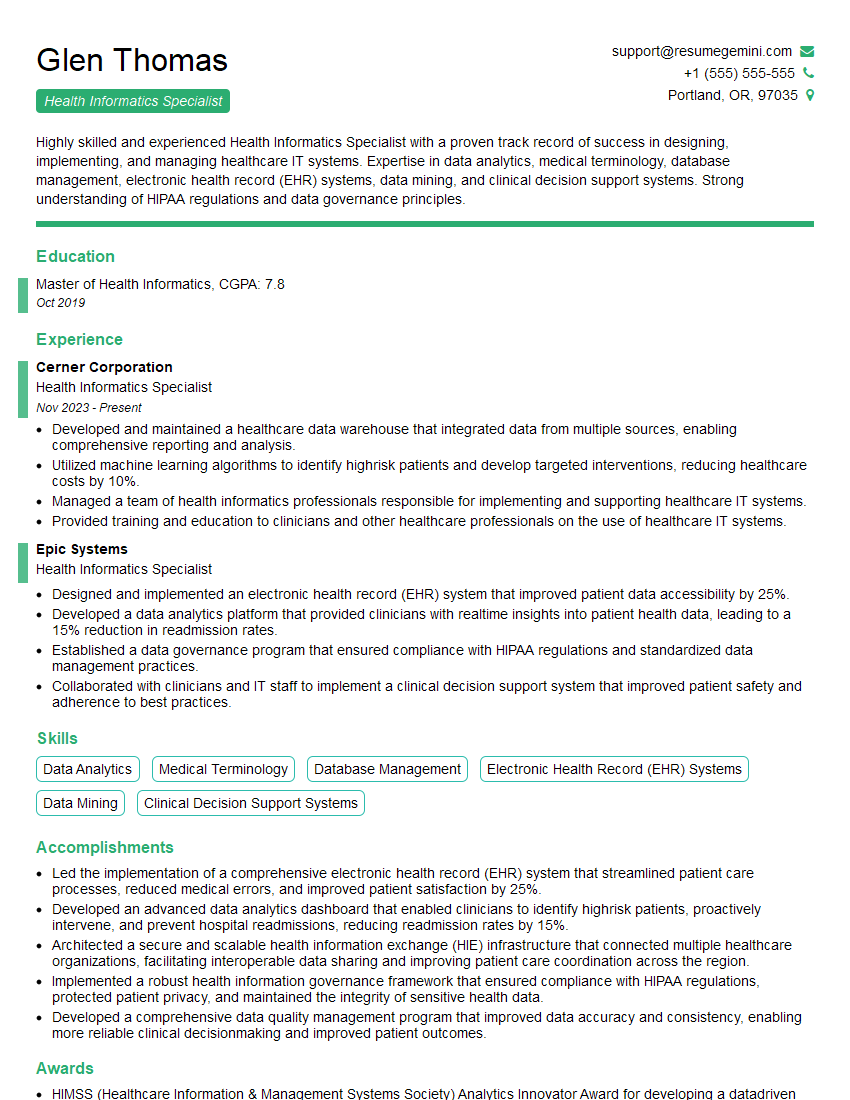
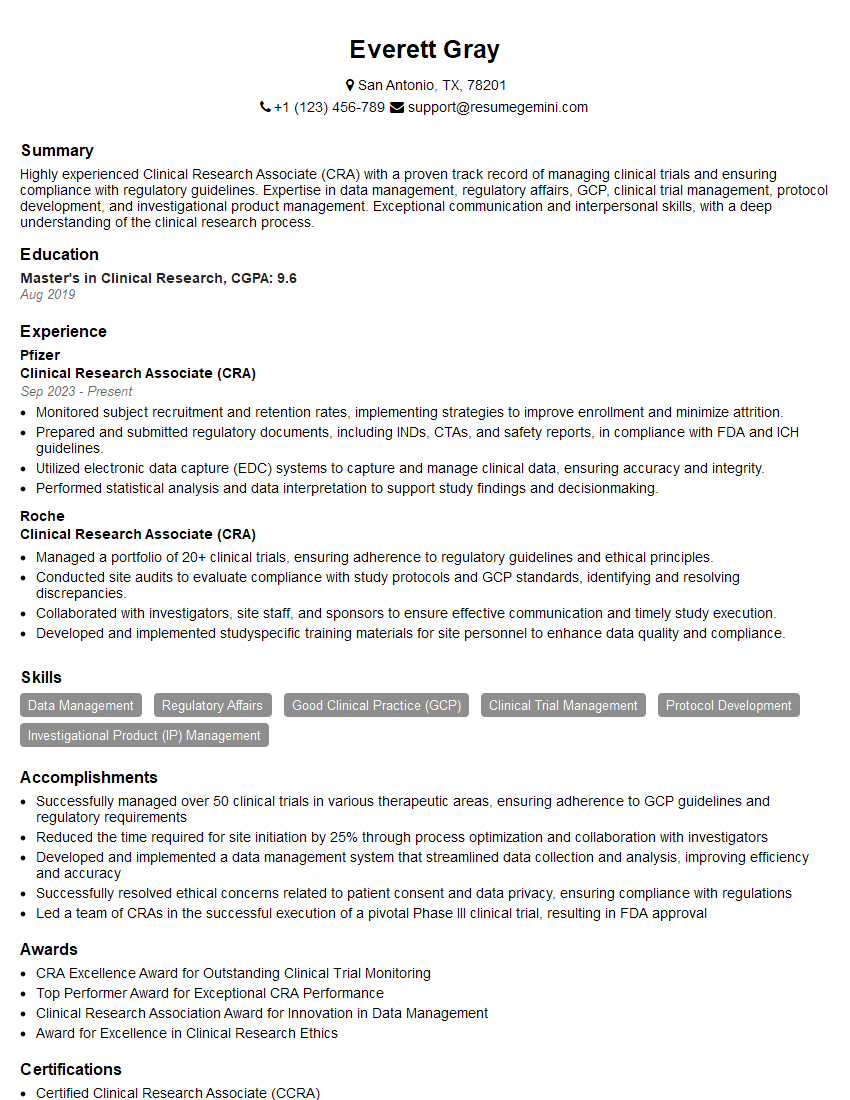
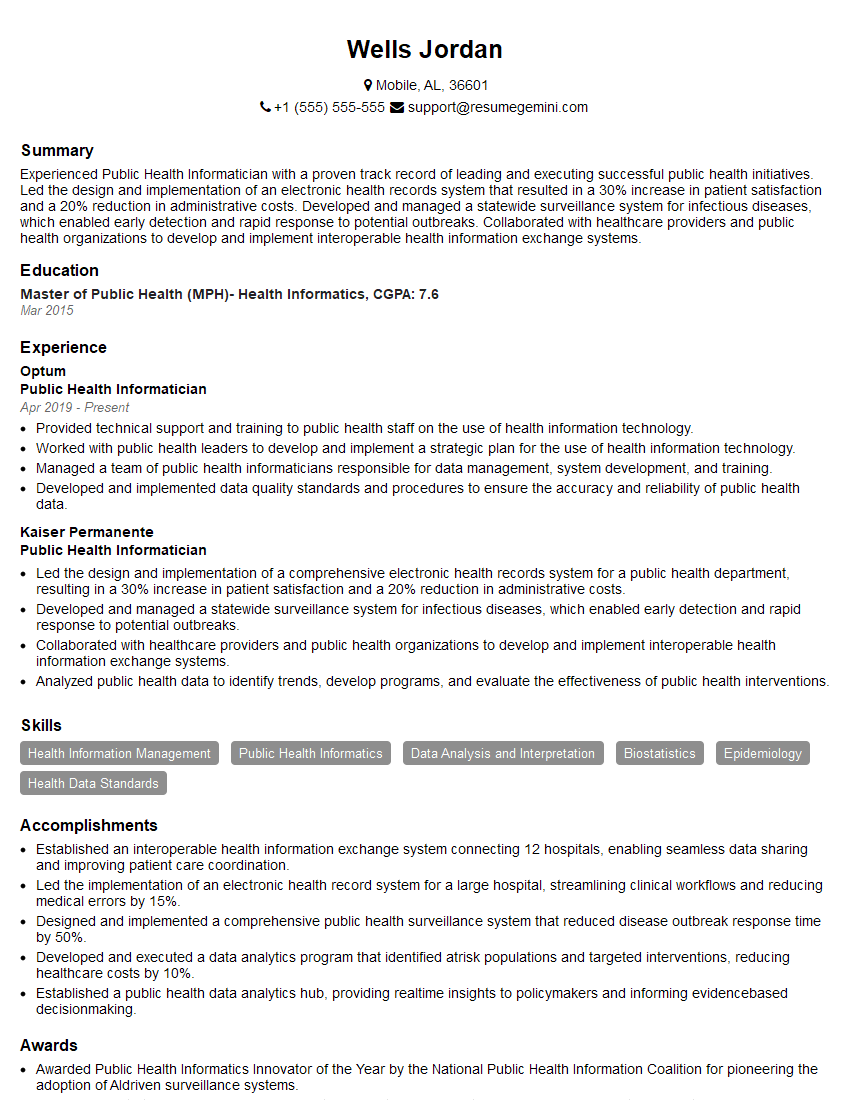
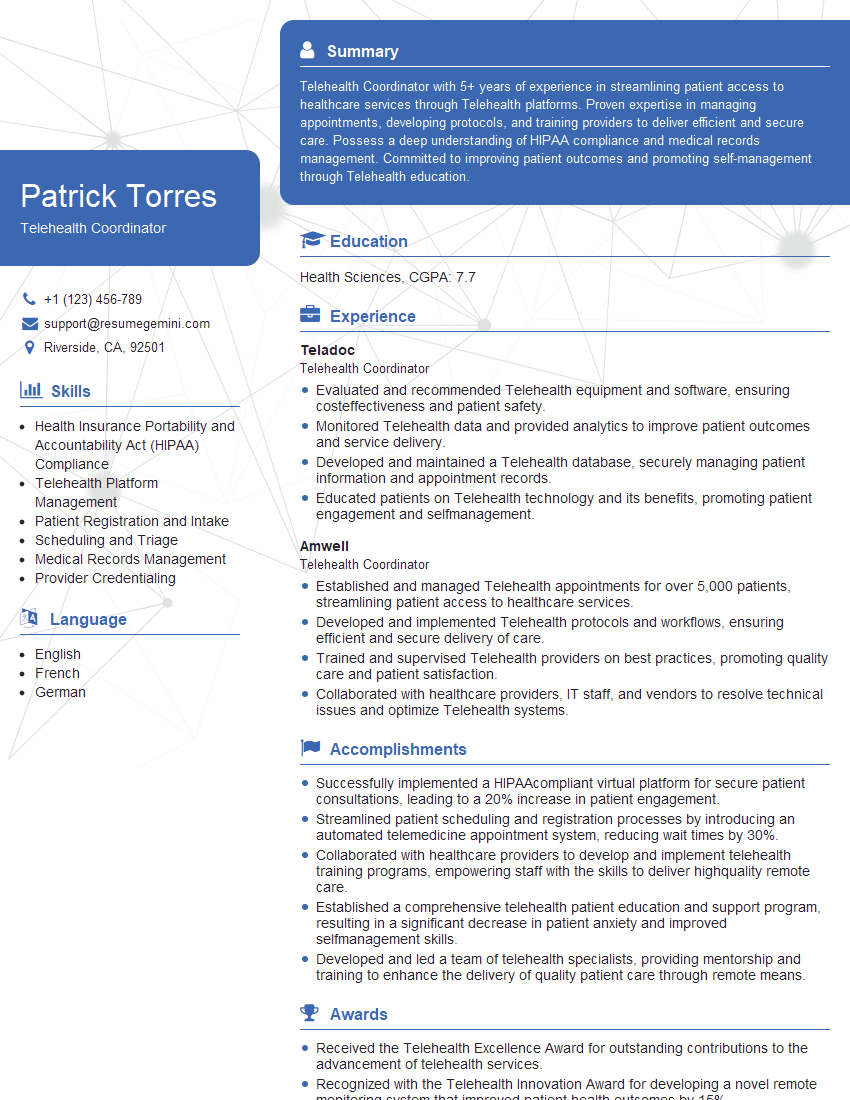
Mastering Health Science Technology is crucial for a thriving career in this rapidly evolving field. The ability to leverage technology to improve patient care and efficiency is highly valued by employers. To significantly boost your job prospects, crafting an ATS-friendly resume is essential. This ensures your qualifications are effectively communicated to hiring managers and applicant tracking systems. We highly recommend using ResumeGemini to build a professional and impactful resume. ResumeGemini offers a streamlined process and provides examples of resumes tailored to Health Science Technology, giving you a head start in showcasing your skills and experience effectively.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO