Interviews are more than just a Q&A session—they’re a chance to prove your worth. This blog dives into essential Health Science Research interview questions and expert tips to help you align your answers with what hiring managers are looking for. Start preparing to shine!
Questions Asked in Health Science Research Interview
Q 1. Explain the difference between observational and interventional studies.
The core difference between observational and interventional studies lies in the researcher’s role. In observational studies, researchers simply observe and measure characteristics or outcomes in a group of participants without intervening. They don’t manipulate any variables. Think of it like watching a natural phenomenon unfold. In contrast, interventional studies (like clinical trials) involve the researcher actively manipulating one or more variables (e.g., administering a treatment) to observe its effect on an outcome. This is akin to conducting an experiment to test a hypothesis.
- Observational Example: A cohort study tracking the incidence of heart disease in smokers versus non-smokers over 10 years. The researchers don’t influence who smokes or not; they simply observe and analyze the data.
- Interventional Example: A randomized controlled trial comparing the effectiveness of a new drug versus a placebo in treating hypertension. Researchers actively assign participants to different treatment groups.
Choosing between these study designs depends heavily on the research question. If you’re investigating the association between variables, an observational design might suffice. If you want to establish cause-and-effect, an interventional study is usually necessary, although even then, careful consideration of confounding variables is crucial.
Q 2. Describe your experience with statistical software packages (e.g., R, SAS, SPSS).
I have extensive experience with several statistical software packages, including R, SAS, and SPSS. My proficiency spans data cleaning, manipulation, statistical analysis, and visualization. In R, I’m comfortable using packages like ggplot2 for creating publication-quality graphics and dplyr for efficient data wrangling. I’ve utilized SAS for large-scale data management and complex statistical modeling, especially in clinical trial data analysis. With SPSS, I’m proficient in conducting various statistical tests, including t-tests, ANOVA, regression analysis, and survival analysis. I’ve used all three in numerous research projects, selecting the most appropriate package based on the project’s specific needs and data size. For example, for a recent meta-analysis involving several thousand studies, SAS was the most efficient option due to its ability to handle large datasets and perform complex calculations. For smaller projects with more exploratory analyses, R’s flexibility and open-source nature was a better fit.
Q 3. What are the key ethical considerations in conducting health science research?
Ethical considerations are paramount in health science research. They encompass several key areas:
- Informed Consent: Participants must be fully informed about the study’s purpose, procedures, risks, and benefits before providing voluntary consent. This includes ensuring they understand their right to withdraw at any time without penalty.
- Confidentiality and Privacy: Protecting participants’ identities and data is crucial. Data should be anonymized or de-identified wherever possible, and appropriate security measures should be in place.
- Beneficence and Non-maleficence: The research should maximize benefits and minimize harms to participants. This involves careful risk assessment and mitigation strategies.
- Justice and Equity: The benefits and burdens of research should be fairly distributed across different populations. Avoiding exploitation of vulnerable groups is essential.
- Data Integrity and Transparency: Maintaining accurate and complete data is critical, as is being transparent about the research process and findings.
Ethical review boards (IRBs) play a crucial role in overseeing research ethics by reviewing research protocols before they commence and ensuring that ethical standards are upheld throughout the research process.
Q 4. How do you ensure the accuracy and reliability of research data?
Ensuring data accuracy and reliability is a multifaceted process that begins with meticulous study design and extends throughout data collection, analysis, and reporting. Key strategies include:
- Standardized Data Collection Methods: Using well-defined protocols, validated instruments, and trained data collectors helps to minimize errors and biases.
- Data Validation and Cleaning: Regular checks for data entry errors, outliers, and inconsistencies are essential. This often involves using statistical software to identify and address these issues.
- Data Audit Trails: Maintaining detailed records of all data manipulations and changes allows for transparency and traceability.
- Blinding or Masking: In studies where blinding is feasible (e.g., clinical trials), it can help to prevent bias from influencing data interpretation.
- Appropriate Statistical Methods: Choosing appropriate statistical techniques for analyzing the data minimizes the risk of drawing inaccurate conclusions.
- Peer Review: Seeking feedback from peers and experts helps to identify potential flaws and improve the quality of the research.
For example, in a clinical trial, regularly checking for missing data and investigating potential reasons for missingness is crucial. Similarly, using a double-data entry method, where data are entered twice independently and discrepancies are resolved, improves data quality and reduces data entry error.
Q 5. Explain the process of designing a clinical trial.
Designing a clinical trial involves a systematic approach encompassing several key stages:
- Defining the Research Question and Objectives: Clearly stating the research question and specifying the primary and secondary outcomes is the first critical step.
- Literature Review: Conducting a thorough review of existing literature helps to inform the study design and identify potential challenges.
- Study Design Selection: Choosing the appropriate study design (e.g., randomized controlled trial, crossover trial) based on the research question and feasibility.
- Sample Size Calculation: Determining the appropriate sample size to ensure sufficient statistical power to detect meaningful differences.
- Participant Selection and Recruitment: Establishing clear inclusion and exclusion criteria and developing a robust recruitment strategy.
- Intervention Development and Standardization: Clearly defining the intervention and developing standardized protocols to ensure consistency in its delivery.
- Data Collection and Management: Developing data collection tools and establishing a system for managing and storing data securely.
- Statistical Analysis Plan: Specifying the statistical methods to be used for analyzing the data.
- Ethical Considerations: Ensuring that the study adheres to ethical guidelines and obtaining necessary ethical approvals.
Each stage requires careful planning and consideration to ensure the clinical trial is rigorous, efficient, and yields reliable results. A well-designed clinical trial protocol minimizes biases, ensures the safety of participants, and maximizes the chance of obtaining meaningful results.
Q 6. Describe your experience with literature reviews and meta-analyses.
I have significant experience conducting literature reviews and meta-analyses. Literature reviews involve systematically identifying, appraising, and synthesizing research evidence on a specific topic. This involves using various databases like PubMed and Embase to search for relevant studies, applying inclusion and exclusion criteria, critically appraising the quality of the included studies, and summarizing the findings. Meta-analyses take this a step further by statistically combining the results of multiple studies to provide a more precise estimate of the effect of an intervention or association between variables.
My experience includes using software like Review Manager (RevMan) for meta-analyses. I’m familiar with assessing heterogeneity between studies, employing different statistical models (e.g., fixed-effects, random-effects), and interpreting the results in a meaningful way. For example, in a recent meta-analysis on the effectiveness of a particular therapy, I utilized RevMan to pool effect sizes across various studies and assess the overall effectiveness while accounting for publication bias. The meta-analysis provided a more comprehensive and precise estimate of the treatment’s effectiveness than any single study could offer.
Q 7. How do you handle conflicting research findings?
Conflicting research findings are common in health science. Handling these requires a critical and systematic approach.
- Assess the Quality of Studies: Critically evaluating the methodology, sample size, and potential biases of conflicting studies is crucial. Studies with methodological flaws should be given less weight.
- Consider Publication Bias: Recognizing that studies with positive results are more likely to be published than those with negative results is important. This bias can skew the overall picture.
- Examine Potential Moderator Variables: Exploring whether differences in study populations, interventions, or outcome measures might explain the conflicting findings is essential.
- Synthesize Findings: Instead of dismissing conflicting findings, integrating them into a broader narrative that acknowledges the complexities and nuances of the research area is often the most appropriate approach. This might involve a narrative synthesis, a meta-analysis with appropriate statistical models, or a qualitative synthesis if appropriate.
- Identify Areas for Future Research: Conflicting findings often highlight gaps in the knowledge base and suggest areas where further research is needed to resolve the discrepancies.
For instance, if two studies show conflicting results on the efficacy of a new drug, examining the characteristics of the participants (age, comorbidities, etc.), the dosage of the drug, and the methods used to measure the outcome can provide insights into the reasons for the conflict. It might suggest that the drug is effective in a specific subgroup of patients but not in others.
Q 8. What are the limitations of your chosen research methods?
Research methods, while powerful, always have inherent limitations. The choice of method dictates the type and scope of the findings. For instance, a randomized controlled trial (RCT), considered the gold standard in many health science areas, can be expensive, time-consuming, and may not always be ethically feasible. The participants in an RCT might not represent the broader population, limiting the generalizability of the results. Similarly, observational studies, while less costly and less intrusive, are susceptible to confounding variables that can obscure the true relationships between variables. Qualitative methods, like interviews and focus groups, provide rich data but are subject to researcher bias and may not be easily replicable.
In my research on the effectiveness of a new diabetes management program, we employed a quasi-experimental design. While this allowed us to study the program in a real-world setting, it lacked the randomization of a true RCT, increasing the risk that observed improvements could be due to other factors, not solely the program itself. To mitigate this limitation, we employed rigorous statistical techniques to control for known confounders, such as age, pre-existing conditions, and socio-economic status.
Q 9. What is your experience with data visualization and presentation?
Data visualization is crucial for effectively communicating research findings. My expertise spans various tools and techniques, from basic bar charts and scatter plots to more advanced methods like heatmaps, network graphs, and interactive dashboards. I’m proficient in software like R, Python (with libraries like Matplotlib and Seaborn), and Tableau. Beyond technical skills, I emphasize the importance of selecting the most appropriate visualization for the specific data and audience. A poorly chosen visualization can obscure, rather than illuminate, the results.
For example, in a recent project on antibiotic resistance, we used a network graph to visually represent the complex relationships between different bacterial strains and their resistance patterns. This allowed stakeholders to quickly grasp the overall picture of resistance spread, which would have been much harder to understand from a simple table of data. In my presentations, I prioritize clarity and conciseness, avoiding excessive clutter and focusing on the key takeaways.
Q 10. How do you ensure the validity and generalizability of research results?
Ensuring validity and generalizability is paramount in health science research. Validity refers to the accuracy of the study’s findings, while generalizability refers to the extent to which the findings can be applied to other populations and settings. We address validity through rigorous study design, appropriate statistical analysis, and careful attention to potential biases. Generalizability is enhanced by using representative samples, clearly defining the study population, and conducting rigorous analyses to test the robustness of the findings.
For instance, if a study on a new drug is only conducted on a homogenous group of young, healthy adults, the results may not be generalizable to older patients or those with co-morbidities. To enhance generalizability, we might employ stratified sampling to ensure representation of different demographic and clinical subgroups. We also conduct sensitivity analyses to examine whether the primary findings change when alternative analytical methods are used.
Q 11. Explain the different types of bias in research and how to mitigate them.
Bias in research can significantly distort results, leading to inaccurate conclusions. Common types of bias include selection bias (systematic differences between study groups), measurement bias (errors in measuring variables), recall bias (inaccuracies in participants’ memories), and publication bias (a tendency to publish only positive results). Mitigating bias requires careful planning at all stages of the research process.
- Selection bias: Randomization, blinding, and careful sampling strategies can minimize selection bias.
- Measurement bias: Using standardized protocols, validated instruments, and blinding assessors helps to reduce measurement bias.
- Recall bias: Employing objective measures and utilizing validated questionnaires can mitigate recall bias.
- Publication bias: Promoting transparent reporting practices, pre-registration of studies, and encouraging the publication of negative or null results can address publication bias.
For example, in a study evaluating a new diagnostic test, blinding the assessors to the participants’ clinical status ensures that their assessment is not influenced by prior knowledge.
Q 12. Describe your experience with grant writing and funding applications.
I have extensive experience in grant writing and securing funding for research projects. My success stems from a strong understanding of funding agency priorities, meticulous proposal writing, and a clear articulation of the research question, methodology, and potential impact. I’ve been involved in securing grants from various sources, including NIH, NSF, and private foundations. The process involves carefully aligning the research objectives with the funder’s mission, developing a compelling narrative, and demonstrating a clear path to achieving the research goals.
One successful grant application I worked on focused on developing a novel intervention for reducing childhood obesity. The key to its success was a strong emphasis on community engagement and the translation of research findings into practical, policy-relevant recommendations. This resonated strongly with the funding agency, emphasizing the broader impact of the research beyond the scientific contribution.
Q 13. How do you manage and prioritize multiple research projects?
Managing multiple research projects requires effective organization, prioritization, and time management skills. I utilize project management tools like Trello or Asana to track tasks, deadlines, and milestones for each project. Prioritization is based on factors such as the urgency of deadlines, potential impact, and available resources. I also delegate tasks effectively to research assistants and collaborators, fostering a collaborative environment. Regular meetings and progress reports ensure that all projects remain on track and address any challenges proactively.
For example, I recently managed three projects concurrently: a clinical trial, a cohort study, and a systematic review. By using a project management tool and assigning clear responsibilities, I ensured the successful completion of all three, delivering high-quality results on time.
Q 14. What is your experience with regulatory guidelines (e.g., ICH-GCP)?
I have a thorough understanding of regulatory guidelines, particularly ICH-GCP (International Council for Harmonisation – Good Clinical Practice) guidelines, essential for conducting ethical and high-quality clinical research. My experience encompasses all aspects of GCP, from informed consent procedures to data management and safety monitoring. I’m adept at designing protocols that meet regulatory requirements and ensuring compliance throughout the research process. This includes meticulous documentation, appropriate training of research personnel, and adherence to strict ethical principles.
In a recent clinical trial, our meticulous adherence to GCP guidelines, including proper documentation of adverse events and timely reporting to regulatory bodies, facilitated a smooth and successful trial completion without any compliance-related issues.
Q 15. Explain your understanding of statistical significance and p-values.
Statistical significance, often represented by the p-value, helps us determine if observed results in a study are likely due to a real effect or simply random chance. A p-value is the probability of obtaining results as extreme as, or more extreme than, the observed results, assuming there is no real effect (the null hypothesis is true). It’s crucial to understand that a p-value doesn’t measure the size or importance of an effect, only the likelihood of observing it by chance.
For example, a p-value of 0.05 (or 5%) means there’s a 5% chance of observing the results if there’s no actual difference between groups being compared. Conventionally, a p-value less than 0.05 is considered statistically significant, implying the null hypothesis can be rejected. However, it’s essential to consider the context, effect size, and other factors before drawing conclusions. A small p-value with a tiny effect size might not be clinically significant, while a larger p-value might be relevant depending on the context. It’s better to consider effect sizes and confidence intervals alongside p-values for a more comprehensive interpretation.
In a clinical trial testing a new drug, a statistically significant p-value might indicate the drug is effective. However, we need to consider the magnitude of the effect. If the drug only improves the outcome by a tiny amount, even with statistical significance, it might not be worth the cost or side effects. Therefore, we consider clinical significance alongside statistical significance in making informed decisions.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you interpret and communicate complex research findings to a non-technical audience?
Communicating complex research findings to a non-technical audience requires simplifying the information without sacrificing accuracy. I utilize several strategies: First, I start by identifying the core message – the key finding that’s most important for the audience to understand. Then, I translate technical terms into plain language, using analogies and real-world examples to illustrate complex concepts. Visual aids, such as charts, graphs, and infographics, are incredibly helpful in conveying data in a digestible format.
For instance, instead of saying ‘the hazard ratio for mortality was 0.75 (95% CI 0.60-0.90, p=0.002)’, I might say, ‘Our study showed that the treatment reduced the risk of death by 25%, and this result is highly statistically significant’. I focus on answering the ‘so what?’ question: what are the implications of the research for the audience? Finally, I use storytelling techniques to engage the audience and make the information relatable, highlighting the human aspects of the research and its potential benefits.
Q 17. What are your strengths and weaknesses in conducting health science research?
My strengths lie in my strong analytical skills and ability to design rigorous research studies. I’m adept at formulating research questions, selecting appropriate methodologies, and performing detailed data analysis using statistical software like R and SPSS. I’m also proficient in writing clear and concise research reports and publications. I have extensive experience in meta-analysis and systematic reviews, allowing for comprehensive synthesis of existing research.
One area I’m continually working to improve is my grant writing skills. While I have successfully obtained funding, I aim to enhance my ability to articulate the significance and feasibility of my research proposals more effectively to secure larger and more competitive grants. I am actively seeking professional development opportunities in this area, including attending workshops and studying successful grant applications.
Q 18. Describe your experience with qualitative research methods.
I have significant experience with qualitative research methods, primarily employing semi-structured interviews and thematic analysis. In one project, I conducted in-depth interviews with patients to understand their experiences with a new cancer treatment. This qualitative approach allowed me to gather rich data that complemented quantitative findings from the clinical trial. I used NVivo software to assist with data management and coding.
The thematic analysis involved identifying recurring themes and patterns within the interview transcripts, providing valuable insights into the patients’ perspectives on the treatment’s effectiveness, side effects, and impact on their quality of life. Understanding the emotional and social aspects of illness and treatment is vital for comprehensive health research, and qualitative methods are invaluable in gaining this understanding. I’m also experienced in grounded theory, which is a valuable approach for generating theory from data collected from participant interviews.
Q 19. How do you stay current with advances in health science research?
Staying current in health science research requires a multi-pronged approach. I regularly read peer-reviewed journals, particularly those focusing on my specific area of expertise (e.g., epidemiology, clinical trials). I also actively participate in professional organizations, attending conferences and workshops to learn about the latest advancements and network with colleagues. I use online resources like PubMed and Google Scholar to search for relevant articles and keep abreast of new publications. Furthermore, I subscribe to relevant newsletters and podcasts related to health research methodologies and advancements in treatment and prevention.
Finally, I actively seek out mentorship and collaborations with leading researchers in my field. These interactions provide invaluable insights into emerging trends and ongoing research initiatives. This blend of formal and informal learning strategies ensures I maintain a deep understanding of the ever-evolving landscape of health science research.
Q 20. Describe your experience with data management and analysis.
My experience with data management and analysis is extensive. I’m proficient in using statistical software packages like R and SPSS for data cleaning, manipulation, and analysis. I have a strong understanding of different statistical techniques, including regression analysis, ANOVA, and survival analysis, and I select the most appropriate method based on the research question and data characteristics. I’m experienced in managing large datasets, ensuring data integrity and accuracy through proper cleaning and validation procedures.
For example, in a recent project involving a large-scale epidemiological study, I was responsible for cleaning and processing a dataset with millions of records. This involved handling missing data, identifying outliers, and transforming variables to meet the requirements of the chosen analytical methods. I meticulously documented all data management steps to ensure reproducibility and transparency. I’m familiar with various data visualization techniques to effectively communicate findings in a visually compelling manner.
Q 21. What is your experience with peer review and publication?
I have extensive experience with peer review and publication. I’ve served as a peer reviewer for several reputable journals in the field of health sciences, providing constructive feedback on manuscripts submitted for publication. This experience has honed my critical appraisal skills and enhanced my understanding of the publication process. I’ve also successfully published numerous articles in peer-reviewed journals, presenting original research findings and contributing to the body of knowledge in my area of expertise.
The peer review process is crucial for maintaining the quality and integrity of scientific literature. It involves carefully evaluating the methodology, results, and conclusions of submitted manuscripts to ensure they meet rigorous standards before publication. My contributions as a reviewer have helped improve the quality of published research, and my own publications have broadened the understanding of health science issues and informed clinical practice.
Q 22. Explain your understanding of different study designs (e.g., randomized controlled trials, cohort studies).
Study designs are the blueprints for how we conduct health science research. Different designs are chosen depending on the research question and what type of evidence we need. Let’s look at two common examples:
- Randomized Controlled Trials (RCTs): These are considered the gold standard for evaluating the effectiveness of interventions like new drugs or therapies. Participants are randomly assigned to either an intervention group (receiving the treatment) or a control group (receiving a placebo or standard treatment). Randomization minimizes bias and allows us to draw causal conclusions about the intervention’s impact. For instance, an RCT might compare a new cholesterol-lowering medication against a placebo to determine its efficacy in reducing LDL cholesterol levels. The results are analyzed to see if the intervention group experienced a statistically significant difference compared to the control group.
- Cohort Studies: In cohort studies, we follow a group of individuals (the cohort) over time to observe the occurrence of a particular outcome, such as a disease. We compare the outcome rates between individuals exposed to a risk factor (e.g., smokers) and those not exposed (non-smokers). Cohort studies are excellent for investigating the incidence and risk factors of diseases but they cannot prove causation definitively; they can only show associations. For example, a cohort study might follow a group of nurses, some of whom smoke and some who don’t, over several years to see if there’s a higher incidence of lung cancer among smokers.
Other important designs include case-control studies (comparing individuals with a disease to those without to identify potential risk factors), cross-sectional studies (measuring the prevalence of a condition or exposure at a single point in time), and case series (describing the characteristics of a group of patients with a specific condition).
Q 23. How do you identify and address potential conflicts of interest in research?
Conflicts of interest (COIs) are situations where personal interests might compromise professional judgment or objectivity in research. Identifying and addressing them is crucial for maintaining research integrity. My approach involves:
- Proactive Disclosure: I always disclose any potential COIs upfront, including financial interests (e.g., grants, stock options from companies related to the research), personal relationships with researchers or participants, or intellectual property rights related to the study.
- Independent Review: Research proposals and results are subject to rigorous review by an Institutional Review Board (IRB) or ethics committee. These committees are designed to identify and mitigate potential COIs.
- Transparency and Documentation: All potential and actual COIs are meticulously documented. This allows for open scrutiny and helps prevent any appearance of impropriety.
- Mitigation Strategies: If a COI is identified, strategies like recusal from certain aspects of the research or blinded review of data are implemented to minimize bias.
For example, if I were researching a new drug, and I owned stock in the company developing that drug, I would disclose that interest before the research begins. This ensures that my personal financial interest does not influence the conduct or reporting of the research. My commitment is to always prioritize rigorous scientific methods and ethical conduct.
Q 24. Describe your experience working in a team setting.
I thrive in collaborative team settings. In my previous research projects, I’ve consistently demonstrated strong teamwork skills by contributing effectively to diverse teams comprised of clinicians, statisticians, and other researchers.
- Communication and Collaboration: I prioritize clear and open communication, actively participating in team meetings and providing constructive feedback. I excel at listening to different perspectives and incorporating them into our shared goals.
- Task Management: I am adept at managing my individual tasks efficiently and contributing to the overall project timeline. I understand the importance of meeting deadlines and ensuring the smooth progress of the project.
- Conflict Resolution: When disagreements arise, I actively participate in finding consensus through respectful dialogue and compromise. I believe that constructive conflict can lead to innovative solutions.
For instance, in one project investigating the effectiveness of a new rehabilitation program for stroke patients, I worked closely with a physiotherapist, a statistician, and a neurologist. My role was to analyze the collected data and prepare reports. Through effective team communication, we were able to overcome challenges, ensuring the project was completed successfully and the findings were published in a peer-reviewed journal.
Q 25. Explain your understanding of power analysis and sample size calculation.
Power analysis and sample size calculation are critical for ensuring the reliability and validity of research findings. A power analysis determines the minimum sample size needed to detect a statistically significant effect, if one truly exists. This prevents us from investing resources in a study that is too small to provide meaningful results.
The process usually involves these steps:
- Defining the research question and hypothesis: This sets the stage for choosing the appropriate statistical test.
- Determining the significance level (alpha): Typically set at 0.05, indicating the probability of rejecting the null hypothesis when it’s actually true (Type I error).
- Estimating the effect size: This is the magnitude of the difference or association we expect to observe between groups or variables. This estimate can come from previous research or pilot studies. A larger effect size requires a smaller sample size.
- Specifying the desired power (1-beta): This is the probability of correctly rejecting the null hypothesis when it’s false (1-Type II error). A higher power reduces the risk of missing a true effect. Typically, a power of 0.8 or 80% is considered acceptable.
- Calculating the sample size: Using statistical software or formulas, we calculate the minimum sample size required based on the above parameters.
If the calculated sample size is not feasible due to resource limitations, we may need to adjust the significance level, power, or effect size to achieve a more attainable sample size, which might compromise the study’s sensitivity or conclusiveness.
Q 26. How do you handle unexpected challenges or setbacks in a research project?
Research is rarely without unexpected challenges. I approach setbacks systematically:
- Problem Identification and Assessment: First, I clearly identify the challenge or setback, determining its nature and scope. This could range from equipment malfunctions to unexpected participant attrition.
- Solution Brainstorming: I then engage in brainstorming sessions with my team, exploring various potential solutions. This collaborative approach often yields creative and effective strategies.
- Risk Assessment and Mitigation: For each potential solution, we assess its risks and benefits. We select the option that offers the best balance between addressing the problem and minimizing negative consequences for the project.
- Documentation and Reporting: All challenges, the chosen solutions, and their impact are thoroughly documented. This ensures transparency and facilitates learning from experiences.
For example, in a study using wearable sensors, we encountered difficulties with data synchronization from the devices. We brainstormed solutions, ultimately deciding to implement a more robust data management system and develop a more efficient data cleaning protocol. This required additional time and resources, but it enabled us to overcome the setback and complete the project successfully.
Q 27. Describe your experience with scientific writing and communication.
Scientific writing and communication are essential aspects of research. My experience encompasses various aspects of this process:
- Manuscript Preparation: I am proficient in writing research manuscripts for publication in peer-reviewed journals. I follow established guidelines for structure, style, and clarity, using clear and concise language.
- Grant Writing: I have experience writing grant proposals to secure funding for research projects. This involves clearly articulating the research question, methodology, and expected impact to convince reviewers of the project’s merit.
- Presentations and Dissemination: I effectively present research findings at conferences and meetings, tailoring my presentations to the audience’s expertise and interests. I can communicate complex scientific concepts clearly and engagingly.
- Data Visualization: I am proficient in using various software tools (e.g., R, GraphPad Prism) to create high-quality figures and tables to visually represent research data effectively.
I believe strong scientific communication is crucial for translating research findings into practical applications and contributing to the advancement of health science.
Key Topics to Learn for Health Science Research Interview
- Research Design & Methodology: Understand various research designs (e.g., experimental, observational, qualitative), data collection methods, and statistical analysis techniques. Consider the ethical implications of each approach.
- Biostatistics & Data Analysis: Gain proficiency in interpreting statistical outputs, understanding p-values, confidence intervals, and hypothesis testing. Practice applying these concepts to real-world health data.
- Literature Review & Critical Appraisal: Develop skills in effectively searching and evaluating scientific literature. Learn to identify biases, limitations, and strengths in research studies.
- Specific Research Areas: Depending on the role, familiarize yourself with key concepts within relevant areas such as epidemiology, clinical trials, public health, or a specific disease area.
- Grant Writing & Funding: Understand the process of securing research funding, including writing compelling proposals and budgeting.
- Data Visualization & Communication: Master the art of presenting complex research findings clearly and concisely through various mediums, including charts, graphs, and presentations.
- Problem-Solving & Critical Thinking: Practice applying your knowledge to solve hypothetical research problems and critically evaluate different approaches.
Next Steps
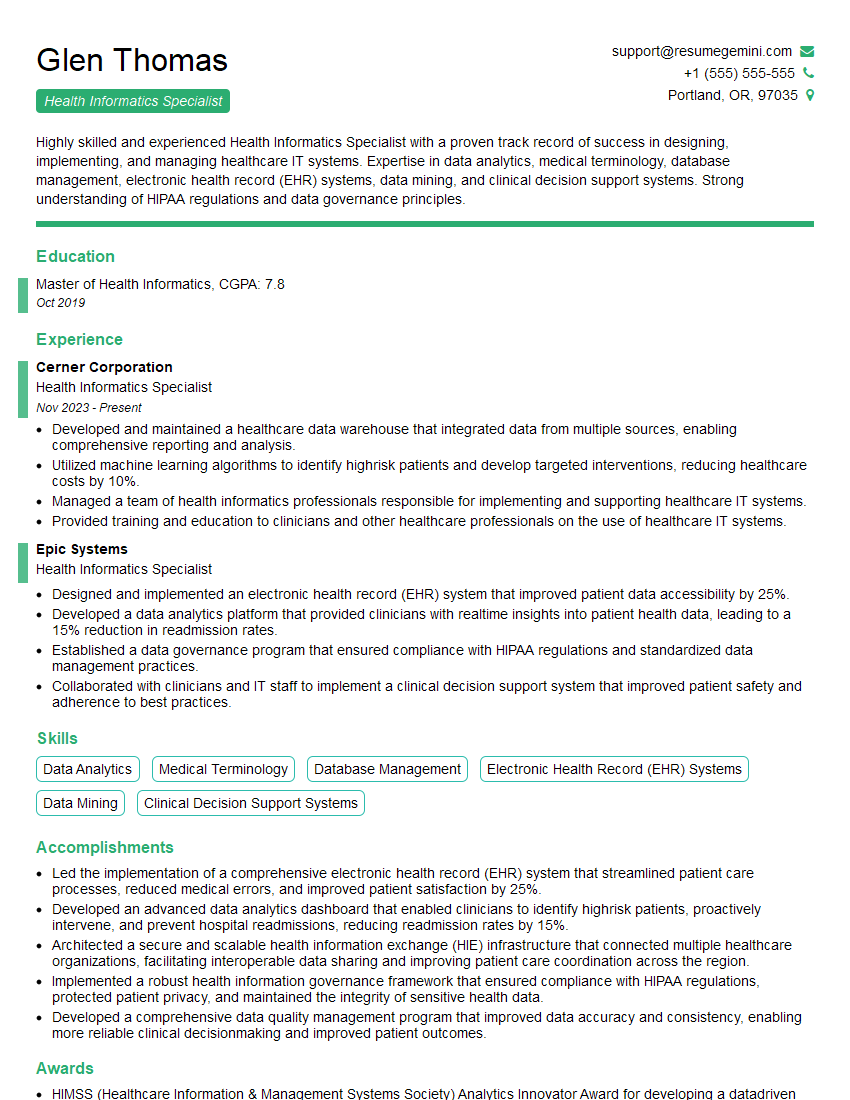
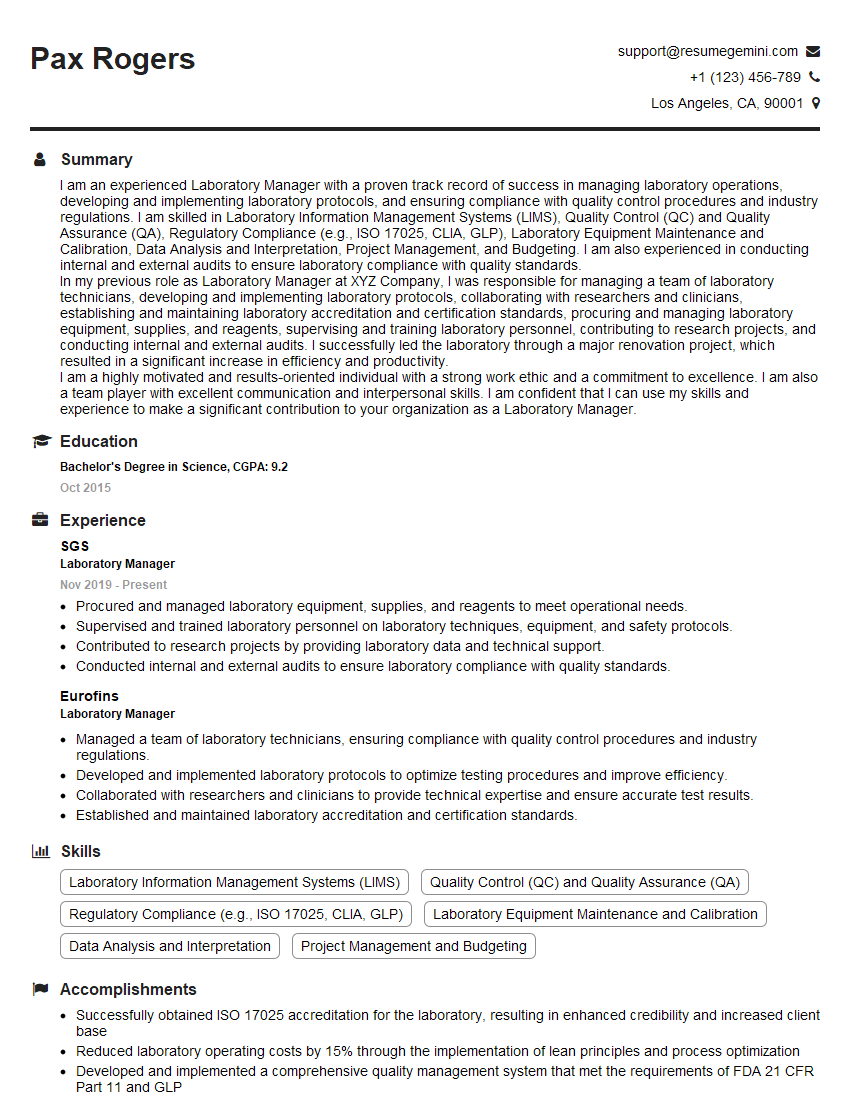
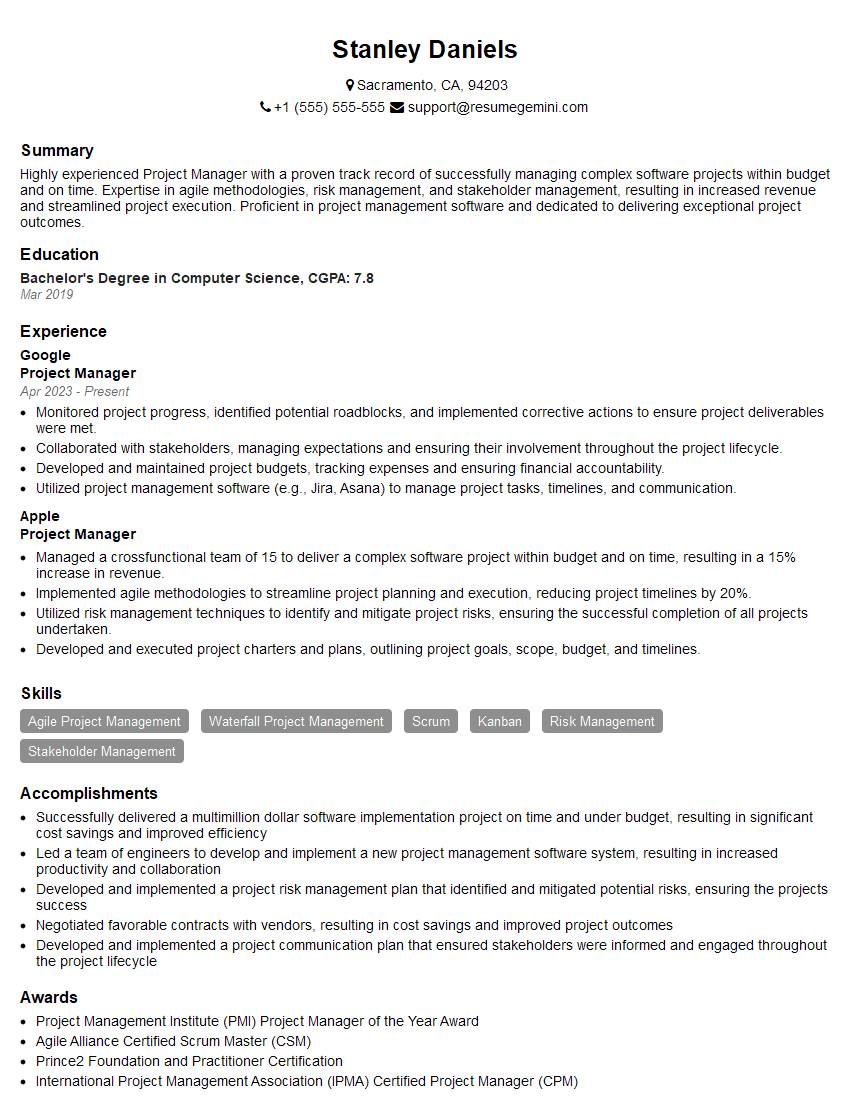
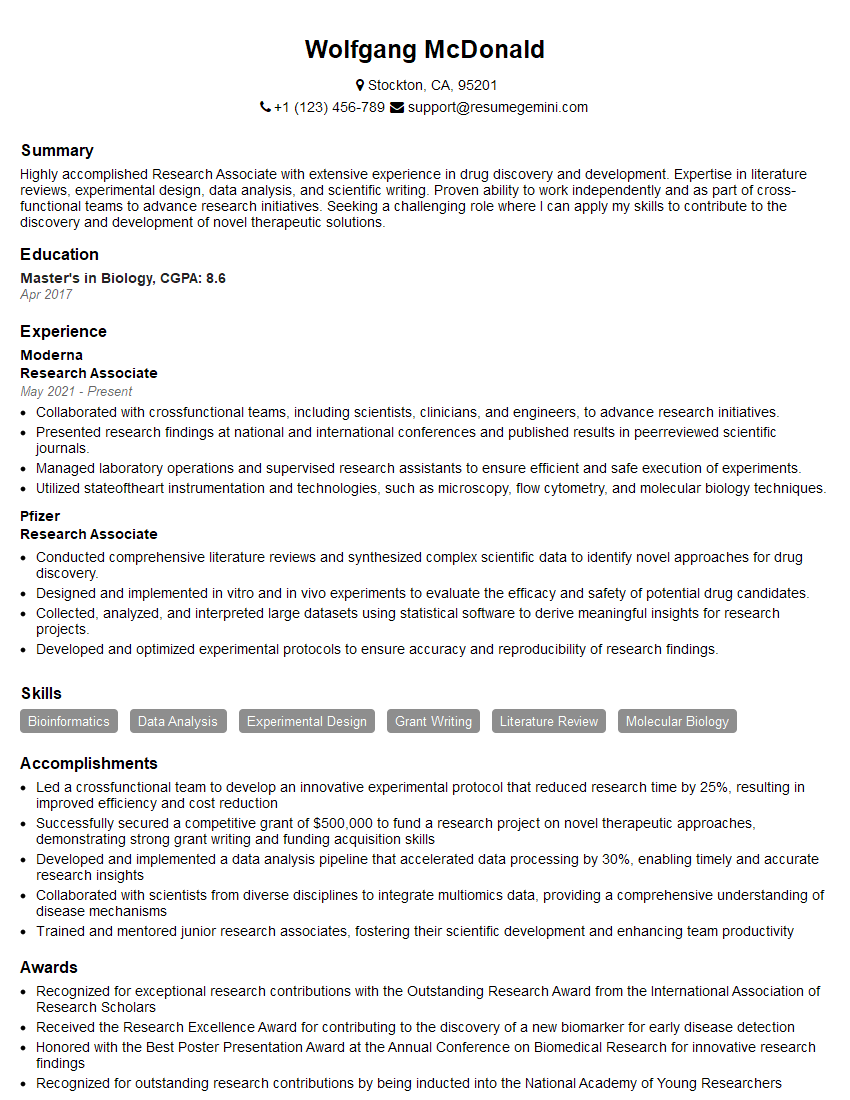
Mastering Health Science Research opens doors to exciting and impactful careers, offering opportunities for innovation and contributing to advancements in healthcare. A strong resume is crucial for showcasing your skills and experience to potential employers. To maximize your job prospects, create an ATS-friendly resume that highlights your qualifications effectively. ResumeGemini is a trusted resource to help you build a professional and impactful resume. We provide examples of resumes tailored to Health Science Research to guide you in crafting a compelling application that stands out.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO