Cracking a skill-specific interview, like one for Speech and Language Impairments, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Speech and Language Impairments Interview
Q 1. Explain the difference between articulation disorders and phonological disorders.
Articulation and phonological disorders both affect speech sound production, but they differ significantly in their underlying causes. Think of it like this: articulation is the mechanics of speech, while phonology is the rule system.
Articulation disorders involve difficulties producing individual speech sounds due to problems with the motor movements of the articulators (tongue, lips, jaw). These problems can be due to structural issues (e.g., a cleft palate), neurological impairments, or apraxia of speech. A child with an articulation disorder might substitute sounds (e.g., saying ‘wabbit’ for ‘rabbit’), omit sounds (e.g., saying ‘boo’ for ‘blue’), or distort sounds (e.g., a lateralized ‘s’). The child typically understands the sounds but can’t physically produce them correctly.
Phonological disorders involve difficulty with the sound system of a language itself. This isn’t about the physical production, but rather the rules governing how sounds are combined and used. A child with a phonological disorder might show patterns of sound errors, such as consistently deleting final consonants in words (‘ca’ for ‘cat’), or simplifying consonant clusters (‘poon’ for ‘spoon’). They might have difficulty with the phonological processes that typically disappear during early language development. These errors aren’t just isolated mispronunciations, but reflect a broader difficulty understanding and applying the sound patterns of their language.
In essence, articulation disorders are problems with the physical act of making sounds, while phonological disorders are problems with the mental organization of sounds. Often, children present with both.
Q 2. Describe the assessment process for a child suspected of having a language delay.
Assessing a child suspected of a language delay is a multi-faceted process requiring a comprehensive approach. It’s not a simple test, but rather a detailed investigation.
- Parent/Caregiver Interview: This is crucial to gather developmental history, family history, and concerns. I’ll ask about milestones like first words, sentence structure development, and any communication challenges noticed at home or in other settings.
- Hearing Screening: Untreated hearing loss is a common cause of language delays, so this is an essential first step.
- Formal Language Assessment: Standardized tests are used to objectively measure different aspects of language, including receptive (understanding) and expressive (producing) language skills, vocabulary, grammar, and narrative skills. Examples include the CELF-5 (Clinical Evaluation of Language Fundamentals) or the PLS-5 (Preschool Language Scale). These tests provide quantifiable data to compare the child’s performance to age-matched peers.
- Informal Language Assessment: This is an observation of the child’s language in natural settings (e.g., during play). It allows for a more holistic understanding of how the child communicates and includes observation of their social interactions and play.
- Speech-Language Sample: A language sample is collected, either during play or through storytelling, and analyzed for grammar, vocabulary, and sentence length. This provides qualitative data to supplement the quantitative data from standardized tests.
- Oral-Motor Examination: This examines the structure and function of the oral-motor mechanism to rule out any physical issues that might be contributing to the delay.
The findings from these assessments, along with observations from teachers and other professionals, are integrated to formulate a comprehensive diagnosis and develop an individualized intervention plan.
Q 3. What are the common causes of dysphagia?
Dysphagia, or difficulty swallowing, can stem from a variety of causes. It’s a complex issue affecting the entire swallowing process, not just the act of eating.
- Neurological Conditions: Stroke, cerebral palsy, Parkinson’s disease, and multiple sclerosis can impair the neurological control of swallowing muscles.
- Structural Abnormalities: Conditions like cleft palate, tumors, or scar tissue can physically obstruct the passage of food.
- Musculoskeletal Disorders: Conditions affecting the muscles and bones of the head and neck (e.g., arthritis, muscular dystrophy) can weaken swallowing muscles.
- Medication Side Effects: Certain medications can have dysphagia as a side effect, causing dry mouth or muscle weakness.
- Aging: Normal aging can lead to changes in muscle strength and coordination, increasing the risk of dysphagia.
- Cancer Treatments: Radiation therapy and chemotherapy can damage the tissues involved in swallowing, leading to dysphagia.
It is important to note that dysphagia can be caused by a combination of factors, and a thorough evaluation is crucial to identify the underlying cause and design an effective treatment plan.
Q 4. How would you differentiate between apraxia of speech and dysarthria?
Apraxia of speech and dysarthria are both motor speech disorders, meaning they affect the ability to produce speech sounds, but they are distinct disorders. The key difference lies in the underlying cause and the nature of the speech errors.
Apraxia of speech is a neurological disorder characterized by difficulty planning and programming the motor movements for speech. Individuals with apraxia understand what they want to say, but they have trouble coordinating the muscles needed to say it. This results in inconsistent errors, often with groping attempts at articulation and difficulty with longer or more complex words. Think of it like having a great recipe (the words they want to say) but not being able to put together the right ingredients (motor movements) in the right order.
Dysarthria is a group of speech disorders resulting from weakness, incoordination, or paralysis of the muscles used for speech. This is typically caused by damage to the nervous system. Dysarthria often leads to consistent errors, such as slurred speech, reduced speech clarity (intelligibility), and difficulty controlling the breath. The problem is less about planning and programming and more about the actual execution of the motor movements.
In short: apraxia is a problem with planning the movements, while dysarthria is a problem with executing them. A thorough neurological examination is essential to differentiate between these two conditions.
Q 5. Describe your experience with AAC devices and strategies.
I have extensive experience using Augmentative and Alternative Communication (AAC) devices and strategies with individuals of all ages and communication abilities. My experience ranges from low-tech methods like picture exchange systems (PECS) to high-tech devices like speech-generating devices (SGDs).
I find that a successful AAC implementation begins with a thorough assessment of the individual’s communication needs and abilities. Factors such as cognitive skills, motor skills, and literacy levels significantly impact device selection and strategy implementation. For example, a child with limited motor skills might benefit from an eye-gaze system, while a child with good fine motor skills might use a touch screen device.
My approach prioritizes empowering individuals to communicate their thoughts and needs effectively. This includes collaboration with families, caregivers, educators, and other professionals. Training and ongoing support are crucial, ensuring the individual, their family, and their support network become proficient in using the chosen AAC system. I’ve successfully helped individuals use AAC to increase social participation, improve academic performance, and increase their overall quality of life.
One memorable case involved a young child with severe autism who was nonverbal. Using PECS, we gradually increased his communication skills. It was incredibly rewarding to see him gain independence and express his desires and needs, creating a positive impact on his social relationships and daily life.
Q 6. What is your approach to treating stuttering in children?
My approach to treating stuttering in children is multifaceted and child-centered. It emphasizes a holistic approach and is tailored to each child’s unique needs, developmental stage, and family dynamics.
Assessment: A thorough evaluation assesses the severity, frequency, and types of stutters, along with associated behaviors (e.g., eye blinking, tension). I assess the child’s overall communication skills and emotional well-being as stuttering can significantly impact self-esteem.
Treatment: I typically use a combination of techniques, adapting them to the child’s age and response. These include:
- Parent Training: Educating parents on how to respond positively and supportively to their child’s stuttering.
- Child-Centered Techniques: These focus on reducing speech rate, modifying speech patterns (e.g., easy onset, prolonged syllables), and improving fluency through playful activities.
- Indirect Therapy: This approach focuses on optimizing the child’s environment to promote fluent speech, including reducing pressure and creating opportunities for relaxed communication.
- Direct Therapy: This involves actively working on specific stuttering behaviors. Techniques include stuttering modification (reducing tension and changing the shape of stutters) and fluency shaping (developing smoother speech patterns).
Regular monitoring and adjustment are crucial. The focus isn’t just on immediate reduction of stuttering, but on building the child’s confidence and self-esteem, fostering positive communication experiences.
Q 7. How do you assess and treat voice disorders?
Assessing and treating voice disorders requires a comprehensive approach combining objective and subjective measures. The assessment involves a detailed history of the voice problem, including onset, duration, and any related symptoms. A physical examination focuses on the larynx and other relevant areas.
Assessment Techniques:
- Voice Sample Analysis: This includes recording the voice to assess parameters such as pitch, loudness, quality, and breath support.
- Acoustic Analysis: Using specialized software to objectively quantify voice characteristics.
- Videostroboscopy: A technique using a fiber-optic scope and a strobe light to visualize the vocal folds during phonation, identifying any structural or functional abnormalities.
- Laryngeal Electromyography (EMG): This procedure measures the electrical activity of the laryngeal muscles to detect muscle dysfunction.
Treatment: Treatment strategies are tailored to the underlying cause and nature of the disorder. This could include:
- Vocal Hygiene Education: Advice on habits that could contribute to vocal strain, such as excessive talking, yelling, and throat clearing.
- Voice Therapy Techniques: Improving breath support, pitch control, vocal fold coordination, and reducing vocal strain through exercises and strategies.
- Medical Management: Depending on the cause, medical interventions, such as medication or surgery, may be necessary.
Regular monitoring and follow-up are essential to assess treatment progress and make necessary adjustments. The goal is to improve the voice’s quality, function, and overall health while considering the individual’s personal needs and context.
Q 8. Explain your understanding of the International Classification of Functioning, Disability and Health (ICF) model.
The International Classification of Functioning, Disability and Health (ICF) model is a framework developed by the World Health Organization (WHO) that provides a standardized language and structure for describing and understanding health and health-related states. It moves beyond simply classifying diseases and instead focuses on the whole person, considering their body functions and structures, activities, and participation in society. Think of it as a holistic approach, looking at not just the impairment (like difficulty with speech), but also its impact on a person’s ability to perform daily tasks (like ordering food at a restaurant) and their overall engagement in life (like participating in social events).
The ICF model uses two main components:
- Functioning and Disability: This encompasses body functions (physiological functions of body systems), body structures (anatomical parts of the body), activities (tasks or actions a person undertakes), and participation (involvement in life situations).
- Contextual Factors: These include environmental factors (physical, social, and attitudinal environments) and personal factors (age, gender, lifestyle, etc.) that influence functioning and disability.
For example, a child with a speech sound disorder (body function impairment) might struggle to communicate effectively in the classroom (activity limitation) and feel socially isolated (participation restriction). However, with supportive teachers (environmental factor) and targeted speech therapy (intervention), their communication skills can improve, leading to better classroom participation and increased social interaction.
Q 9. Describe your experience working with individuals with autism spectrum disorder.
My experience working with individuals with Autism Spectrum Disorder (ASD) has spanned several years and diverse settings. I’ve worked with children, adolescents, and adults, each presenting with unique communication challenges. Many individuals with ASD exhibit difficulties with social communication, pragmatic language (understanding and using language in social contexts), and repetitive or restricted behaviors. Some may also have accompanying speech sound disorders or other language impairments.
My approach involves a thorough assessment of their strengths and challenges, including their communication skills, sensory processing, and social interactions. I then tailor interventions to their specific needs, focusing on improving communication skills using strategies such as visual supports (pictures, schedules), social stories, and play-based therapy. Collaboration with parents and other professionals is crucial for a holistic approach. For instance, I once worked with a nonverbal adolescent who, through intensive therapy combining visual aids and augmentative and alternative communication (AAC), gradually started communicating his needs and desires, leading to a significant improvement in his quality of life. Each case requires individualized strategies and patience.
Q 10. How do you collaborate with other professionals (e.g., teachers, doctors, therapists)?
Collaboration is absolutely essential in my work. I regularly communicate and work alongside various professionals, including teachers, doctors, occupational therapists, physical therapists, and psychologists. This multidisciplinary approach ensures a holistic and comprehensive understanding of the client’s needs.
With teachers, I discuss the client’s communication skills in the classroom, identifying challenges and developing strategies to support their learning and participation. With doctors, I share information about the client’s communication abilities to contribute to a complete medical picture and rule out any underlying medical conditions affecting communication. Collaboration with other therapists allows me to coordinate services, avoiding conflicting approaches and ensuring a cohesive treatment plan. Effective communication, such as regular meetings, shared documentation (electronic health records are vital here!), and a willingness to adapt to others’ perspectives, builds a strong collaborative environment.
For example, I might collaborate with an occupational therapist to address fine motor skills impacting handwriting or typing skills if these are impacting communication. This integrated approach improves outcomes and fosters better support for the individual.
Q 11. What are some common assessment tools you utilize in your practice?
The assessment tools I use depend on the client’s age, suspected diagnosis, and specific communication needs. However, some common tools include:
- Standardized tests: These provide a quantifiable measure of communication skills, such as the Goldman-Fristoe Test of Articulation (GFTA), the Clinical Evaluation of Language Fundamentals (CELF), and the Preschool Language Scale (PLS). These offer normative data for comparison.
- Informal assessments: These are observation-based, focusing on a client’s natural communication in various contexts. This can involve language samples, conversational analysis, or play-based assessments.
- Parent/Teacher/Caregiver questionnaires: These provide valuable information on the client’s communication skills and behaviors in different settings.
- Dynamic Assessment: This type of assessment focuses on a client’s ability to learn and respond to intervention, providing insights into their learning potential. It might involve structured teaching tasks followed by immediate assessment.
It is critical to remember that assessment is an ongoing process, and results inform intervention planning and ongoing progress monitoring.
Q 12. What is your approach to therapy for clients with traumatic brain injuries?
Therapy for clients with traumatic brain injuries (TBIs) requires a highly individualized approach. The specific deficits and the severity of the injury greatly influence the treatment plan. Common communication impairments resulting from TBI include aphasia (difficulty with language processing), dysarthria (speech motor difficulties), cognitive-communication deficits (difficulty with attention, memory, problem-solving affecting communication), and swallowing difficulties (dysphagia).
My approach focuses on a comprehensive assessment to identify specific communication weaknesses. Then, I utilize a variety of evidence-based techniques, including:
- Aphasia therapy: This includes techniques to improve language comprehension, verbal expression, reading, and writing.
- Speech therapy for dysarthria: This focuses on improving articulatory precision, strength, and control using exercises and strategies.
- Cognitive-communication therapy: This addresses difficulties with attention, memory, and executive functions impacting communication.
- Augmentative and Alternative Communication (AAC): This might involve the use of communication boards, devices, or other methods to support communication if verbal communication is severely impaired.
Collaboration with other therapists and the client’s family is crucial for successful rehabilitation. Regular monitoring and adjustment of therapy techniques are essential due to the fluctuating nature of recovery from a TBI.
Q 13. Explain your experience with evidence-based practice in speech therapy.
Evidence-based practice (EBP) is the cornerstone of my speech therapy approach. EBP involves integrating the best available research evidence with clinical expertise and client values to make informed decisions about assessment and intervention. I regularly consult peer-reviewed journals, research databases (like PubMed), and professional organizations’ guidelines to stay updated on the latest research findings and treatment approaches.
For example, when working with a child with a phonological disorder, I would refer to research on effective phonological therapy approaches like minimal pairs or cycles approach. This ensures I’m using interventions supported by scientific evidence and proven to be effective. I also utilize outcome measures to track progress and modify my therapy based on the evidence of its efficacy for that specific client.
Continuing education, attending conferences, and actively participating in professional development activities are vital for maintaining my knowledge of current research and translating findings into practical clinical practice. I believe that incorporating evidence-based practices is essential for providing high-quality, ethical, and effective speech therapy services.
Q 14. How do you adapt your therapy techniques for clients with different learning styles?
Adapting therapy techniques to suit diverse learning styles is vital for optimal client outcomes. I employ a variety of strategies to cater to visual, auditory, kinesthetic, and other learning preferences.
For visual learners, I utilize visual aids like charts, pictures, and videos. For auditory learners, I use auditory cues and repetition, emphasizing verbal instructions and feedback. Kinesthetic learners benefit from hands-on activities, role-playing, and tactile materials. I might use manipulatives like blocks, puppets, or even just simple actions to illustrate concepts. I also consider individual learning preferences for pace, environment, and overall communication style. Some clients prefer quiet, structured environments while others thrive in more interactive and dynamic settings. Building a strong rapport and understanding the client’s communication needs, preferences, and learning styles are paramount.
For example, when teaching a child with articulation difficulties, I might use a mirror for visual feedback, auditory cues to help them discriminate sounds, and then have them practice saying the sounds while manipulating play dough or other tactile objects.
Q 15. Describe your experience with data collection and documentation in speech therapy.
Data collection and documentation are crucial in speech therapy for tracking progress, informing treatment decisions, and ensuring accountability. My approach involves a multi-faceted strategy combining standardized assessments, informal observations, and ongoing data collection throughout the therapeutic process.
Standardized Assessments: I utilize standardized tests like the Goldman-Fristoe Test of Articulation or the Clinical Evaluation of Language Fundamentals to establish a baseline and objectively measure progress. Results are meticulously documented, including raw scores, percentiles, and standard scores. This provides a benchmark against which future performance can be compared.
Informal Assessments and Observations: I regularly observe the client’s communication skills in naturalistic settings, noting areas of strength and weakness. This qualitative data complements the quantitative data from standardized tests, giving a more holistic picture. Examples include observing conversational skills, narrative abilities, and pragmatic language use. This is carefully documented using detailed notes and anecdotal records.
Ongoing Data Collection: Throughout the therapy sessions, I collect data on specific target behaviors. This could involve frequency counts of correct responses, error patterns, or duration of speech samples. I utilize data sheets, graphs, and progress reports to visually represent this data, making it easy to monitor improvement and adjust treatment plans as needed. For example, I might track the client’s accuracy in producing /s/ blends over several sessions.
Technology Integration: I’m comfortable using technology to aid in data collection. This includes apps for tracking progress, recording speech samples for analysis, and utilizing teletherapy platforms for virtual sessions. The data collected via such methods is secured and stored according to HIPAA guidelines.
All documentation is maintained in a secure, organized manner, following ethical guidelines and adhering to relevant privacy regulations (e.g., HIPAA). This comprehensive approach ensures that I can provide the most effective and evidence-based therapy for my clients.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How would you address a parent’s concerns about their child’s speech development?
Addressing parental concerns requires empathy, active listening, and a collaborative approach. I begin by creating a safe and supportive environment where parents feel comfortable expressing their anxieties. I then focus on understanding their specific concerns and validating their feelings.
Active Listening and Empathy: I listen carefully to the parents’ concerns, asking clarifying questions to ensure I fully understand their perspective. I acknowledge their feelings and validate their concerns, even if I don’t necessarily agree with their interpretation of the situation. For instance, if a parent expresses worry about their child’s slow language development, I might say, “I understand your concern about your child’s language, and it’s natural to feel anxious when your child is not meeting typical milestones.”
Clear and Accessible Explanation: I explain the child’s speech and language development in simple, non-technical terms. I use relatable analogies and avoid overwhelming them with jargon. I might explain the developmental stages involved and highlight the child’s current skills. This empowers parents with understanding and reduces their anxiety.
Collaborative Goal Setting: I work collaboratively with parents to set realistic and achievable goals for the child. This involves discussing the child’s strengths and weaknesses, considering the family’s values and preferences, and outlining a plan for addressing the concerns. Parents are active partners in the process, not passive recipients of instructions.
Providing Resources and Support: I provide parents with resources and support networks, such as links to relevant websites, support groups, or other professionals. I emphasize that I am a partner in their child’s journey and that open communication is key to success.
This multifaceted approach ensures that parents feel heard, informed, and empowered to participate fully in their child’s speech therapy journey. The goal is to foster a strong therapeutic alliance based on mutual trust and collaboration.
Q 17. What are some ethical considerations in speech-language pathology?
Ethical considerations are paramount in speech-language pathology. Maintaining confidentiality, ensuring client autonomy, and providing culturally competent care are central to my practice.
Confidentiality: I strictly adhere to the principles of confidentiality, ensuring that client information is protected and only shared with authorized individuals. This includes following HIPAA guidelines and maintaining secure electronic records. I never disclose information without obtaining informed consent from the client or guardian.
Client Autonomy: I respect the client’s right to make informed decisions about their treatment. This includes explaining treatment options clearly, answering questions thoroughly, and allowing the client (or guardian) to participate actively in goal setting and decision-making. I never impose my own values or preferences on a client.
Cultural Competence: I am committed to providing culturally competent care, taking into account the client’s cultural background, beliefs, and values. This includes being sensitive to diverse communication styles and adapting my therapeutic approach to meet the client’s individual needs. I actively seek knowledge about different cultures and strive to build rapport based on mutual respect and understanding.
Professional Boundaries: Maintaining appropriate professional boundaries is vital. This involves avoiding dual relationships, maintaining appropriate communication channels, and ensuring that my interactions with clients remain strictly professional. This is to avoid potential conflicts of interest or harm.
Competence and Continuing Education: I am responsible for maintaining my professional competence and staying current with best practices. This involves ongoing professional development, seeking supervision when necessary, and referring clients to other professionals when appropriate.
Adherence to these ethical principles is essential for building trust, ensuring client well-being, and maintaining the integrity of the profession.
Q 18. Describe a challenging case and how you overcame the difficulties.
One challenging case involved a young child with severe apraxia of speech, coupled with significant social anxiety. Apraxia of speech is a neurological disorder that affects the planning and programming of speech movements, making it difficult to coordinate the muscles needed to produce clear speech. The child’s anxiety further exacerbated the communication difficulties, making therapy sessions extremely challenging.
To overcome these difficulties, I employed a multi-pronged approach:
Building Rapport and Trust: I began by focusing on building a strong therapeutic relationship with the child, using play-based activities and creating a safe and non-judgmental environment. This gradually helped reduce the child’s anxiety.
Individualized Treatment Plan: I developed a highly individualized treatment plan that incorporated techniques specifically designed for apraxia, such as motor learning principles and intensive practice. The plan also included strategies to address the child’s anxiety, such as incorporating relaxation techniques and positive reinforcement.
Collaboration with Parents and Educators: I closely collaborated with the child’s parents and teachers to ensure consistent support and carryover of techniques across different settings. This involved regular communication, sharing of progress reports, and joint goal setting.
Utilizing Technology: I incorporated technology into therapy to make the sessions more engaging, utilizing apps and games that encouraged speech practice in a fun and motivating way. This helped maintain the child’s engagement and motivation, even during challenging moments.
Celebrating Successes and Adapting Treatment: I consistently celebrated even small successes, reinforcing the child’s progress and boosting their confidence. I also remained flexible and adaptable, regularly modifying the treatment plan based on the child’s progress and response.
Through consistent effort and a tailored approach, the child made significant progress in both speech production and social communication. This experience reinforced the importance of a holistic and client-centered approach to therapy.
Q 19. What are your professional development goals?
My professional development goals center on expanding my expertise in specific areas and enhancing my skills in working with diverse populations. I aim to:
Deepen my knowledge of neurogenic communication disorders: I plan to pursue advanced training or certifications in the assessment and treatment of aphasia and other neurogenic speech disorders.
Expand my proficiency in AAC (Augmentative and Alternative Communication): I intend to enhance my skills in assessing and implementing AAC strategies for individuals with complex communication needs.
Improve my fluency in Spanish: I want to improve my Spanish proficiency to better serve the growing Hispanic population in my community.
Enhance my telehealth skills: I aim to stay updated on the latest telehealth technology and evidence-based practices to deliver high-quality virtual therapy services.
By pursuing these goals, I hope to enhance my effectiveness as a clinician and provide even more comprehensive and equitable care to my clients.
Q 20. How do you stay updated with the latest research and best practices in speech-language pathology?
Staying updated with the latest research and best practices in speech-language pathology is a continuous process. I actively engage in several strategies:
Professional Organizations: I am an active member of the American Speech-Language-Hearing Association (ASHA), attending conferences, workshops, and webinars. This offers opportunities for professional networking and exposure to cutting-edge research and clinical advancements.
Peer-Reviewed Journals: I regularly read peer-reviewed journals such as the Journal of Speech, Language, and Hearing Research and the American Journal of Speech-Language Pathology to stay informed about new research findings and treatment techniques.
Continuing Education Courses: I participate in various continuing education courses and workshops to enhance my knowledge and skills in specific areas. This ensures that my practice remains aligned with current best practices.
Mentorship and Collaboration: I actively seek mentorship opportunities and collaborate with other professionals to share knowledge, discuss challenging cases, and learn from each other’s experiences.
Online Resources: I utilize reputable online resources, such as ASHA’s website and other evidence-based websites, to access current information, guidelines, and treatment protocols.
This multifaceted approach guarantees that my clinical practice remains evidence-based, ethical, and aligned with the latest advancements in the field.
Q 21. Describe your experience with conducting therapy sessions virtually.
My experience with conducting therapy sessions virtually has been largely positive and highly effective. I’ve adapted my approach to utilize the unique opportunities provided by telehealth, while also mitigating potential challenges.
Platform Familiarity: I am proficient in using various telehealth platforms, ensuring secure and reliable communication with my clients. This includes understanding the features and functions of these platforms, ensuring both client and therapist comfort.
Adapting Therapeutic Techniques: I’ve modified my therapeutic techniques to be suitable for the virtual setting. This includes using interactive online activities, incorporating visual aids effectively, and ensuring clear audio and visual communication.
Addressing Technical Challenges: I have strategies in place to address potential technical challenges, such as internet connectivity issues or software malfunctions. This includes having backup plans and ensuring that clients have the necessary technological support.
Maintaining Client Engagement: I proactively engage my clients to ensure their active participation and maintain a positive therapeutic alliance. This involves utilizing interactive elements and creating engaging sessions to mimic the face-to-face interaction as much as possible.
Privacy and Security: I adhere strictly to HIPAA regulations and maintain the confidentiality of all client information during virtual sessions, using only secure and compliant platforms.
While telehealth presents some unique challenges, it has also expanded my accessibility and reach, allowing me to provide services to clients who may otherwise have difficulty accessing in-person therapy. I believe it is a valuable and effective tool in providing comprehensive speech therapy services.
Q 22. Explain your understanding of various types of aphasia.
Aphasia is a language disorder affecting the ability to communicate, caused by damage to the brain, typically from stroke. There are several types, each impacting different aspects of language processing.
- Broca’s Aphasia: Characterized by difficulty producing fluent speech, though comprehension is relatively preserved. Individuals might understand what is said but struggle to form complete sentences. Think of it as having the words stuck in their head. For example, a person might say, “Walk…dog…park,” instead of “I will take the dog to the park.”
- Wernicke’s Aphasia: This is characterized by fluent but nonsensical speech. Comprehension is severely impaired. They might speak in sentences that sound grammatically correct but lack meaning. Imagine a word salad—words strung together without forming a coherent thought.
- Global Aphasia: This is the most severe form, impacting both expressive and receptive language abilities significantly. Communication is extremely limited.
- Conduction Aphasia: Individuals have difficulty repeating words or phrases, despite relatively intact comprehension and speech fluency. They might understand what is said and be able to speak normally but struggle to repeat something.
- Anomic Aphasia: This type is characterized by difficulty retrieving words, often using circumlocutions (talking around the word) or substituting words. A person might say, “The thing you write with,” instead of “pen.”
The type of aphasia depends on the location and extent of the brain damage. Accurate diagnosis requires a comprehensive speech-language evaluation.
Q 23. How do you differentiate between receptive and expressive language disorders?
Receptive and expressive language disorders both affect communication, but in different ways. Think of it like this: receptive is about understanding, while expressive is about communicating.
- Receptive Language Disorder: This involves difficulty understanding spoken or written language. Someone with a receptive language disorder may struggle to follow directions, understand stories, or engage in conversations due to difficulty processing the information. For example, they may not grasp the meaning of a complex sentence or a subtle nuance in a conversation.
- Expressive Language Disorder: This involves difficulty expressing oneself verbally or in writing. Individuals might have limited vocabulary, struggle to form sentences, or have difficulty articulating their thoughts. A child with an expressive language disorder might struggle to tell a story or explain their ideas clearly. They might use very simple sentences or make frequent grammatical errors.
It’s important to note that these disorders can co-occur; someone can have difficulties both understanding and expressing language. A thorough assessment is necessary to differentiate and determine the severity of each aspect.
Q 24. How do you incorporate family involvement in therapy?
Family involvement is crucial for successful speech therapy. They are the client’s primary support system and play a vital role in carrying over therapy techniques into daily life.
- Education and Training: I educate family members about the specific language impairment, its impact, and the therapy goals. This ensures everyone is on the same page and understands the strategies used.
- Active Participation: I involve family members in therapy sessions, demonstrating techniques and encouraging their active participation in practicing language skills at home.
- Collaborative Goal Setting: We work together to establish realistic and achievable goals, integrating therapy strategies into the client’s daily routines.
- Regular Communication: Open communication through regular meetings or phone calls ensures we address any concerns or questions and monitor progress effectively. This also helps to maintain consistency between therapy sessions and home practice.
For instance, if a child has a speech sound disorder, I would teach parents how to model correct pronunciation during daily interactions, creating a supportive and consistent language environment. This collaborative approach significantly improves outcomes and ensures the child’s long-term success.
Q 25. What are your strengths and weaknesses as a speech-language pathologist?
My strengths lie in my ability to build rapport with clients of all ages and backgrounds. I am highly skilled in diagnostic assessment and creating individualized treatment plans tailored to each client’s needs and learning style. I am also adept at using a variety of intervention techniques and staying current with the latest research and evidence-based practices.
My area for improvement is time management when dealing with a high caseload and the administrative tasks associated with it. I am actively working on developing more efficient organizational skills to address this.
Q 26. How do you manage your time effectively when working with multiple clients?
Managing my time effectively with multiple clients involves careful planning and organization. I utilize a scheduling system that allows me to allocate appropriate time for each client, considering the complexity of their needs and the type of therapy involved.
- Prioritization: I prioritize tasks based on urgency and importance. This ensures that essential activities, such as client sessions and report writing, are given adequate time.
- Time Blocking: I block specific times for client sessions, administrative tasks, and professional development activities. This prevents tasks from overlapping and creates a structured work schedule.
- Delegation: Where possible, I delegate administrative tasks to reduce my workload and focus on direct client care.
- Regular Review: I regularly review my schedule to assess its effectiveness and make adjustments as needed to ensure optimal time management.
This structured approach helps to avoid feeling overwhelmed and ensures I provide quality care to all my clients.
Q 27. Describe your experience with different intervention strategies (e.g., play therapy, modeling, etc.)
My experience encompasses a wide range of intervention strategies, each tailored to the individual’s needs and the specific communication disorder.
- Play Therapy: I frequently use play therapy for younger children, as it provides a fun and engaging way to work on language skills. This can involve using toys, games, and storytelling to target specific language goals.
- Modeling: This involves demonstrating the correct language form or behavior. For example, I might model correct pronunciation or sentence structure for a child with articulation or grammatical difficulties.
- Augmentative and Alternative Communication (AAC): For clients with severe communication impairments, I utilize AAC techniques, such as picture exchange systems or speech-generating devices, to help them communicate their needs and desires.
- Computer-Assisted Therapy: I incorporate technology such as language learning apps and software to enhance therapy and provide engaging practice opportunities.
- Social Communication Groups: These groups provide a structured environment for clients to practice social communication skills in a peer-interaction setting.
The selection of the most appropriate strategies is based on a thorough assessment and ongoing monitoring of the client’s progress. Regular modifications and adjustments to the therapy plan are essential to ensure effectiveness.
Key Topics to Learn for Speech and Language Impairments Interview
- Articulation Disorders: Understanding different types (e.g., phonological processes, apraxia), assessment methods (e.g., phonetic inventory, speech sound analysis), and intervention strategies (e.g., phonological awareness activities, articulation drills).
- Fluency Disorders (Stuttering): Knowing the characteristics of stuttering, various assessment techniques, and evidence-based intervention approaches (e.g., fluency shaping, stuttering modification).
- Language Disorders (Receptive & Expressive): Differentiating between receptive and expressive language impairments, exploring diagnostic tools (e.g., language sample analysis, standardized tests), and outlining intervention strategies targeting vocabulary, grammar, and pragmatics across various developmental stages.
- Voice Disorders: Familiarity with vocal anatomy and physiology, common voice disorders (e.g., nodules, polyps, dysphonia), diagnostic procedures (e.g., laryngeal examination, acoustic analysis), and relevant therapeutic approaches.
- Assessment and Intervention Techniques: Demonstrate understanding of the entire assessment process, including case history, standardized testing, and informal assessment methods. Show your knowledge of various intervention strategies – their theoretical underpinnings and practical application – including direct and indirect service delivery models.
- Neurogenic Communication Disorders: Understanding the impact of neurological conditions (e.g., stroke, traumatic brain injury) on communication and swallowing. Knowledge of assessment and treatment approaches specific to aphasia, apraxia of speech, and dysphagia.
- Social Communication Disorders (e.g., Autism Spectrum Disorder): Understanding the unique communication challenges presented by ASD and other social communication disorders and evidence-based intervention strategies (e.g., social skills training, augmentative and alternative communication (AAC)).
- Ethical Considerations and Professional Practice: Demonstrating awareness of ethical principles relevant to the profession, including confidentiality, informed consent, and cultural sensitivity.
Next Steps
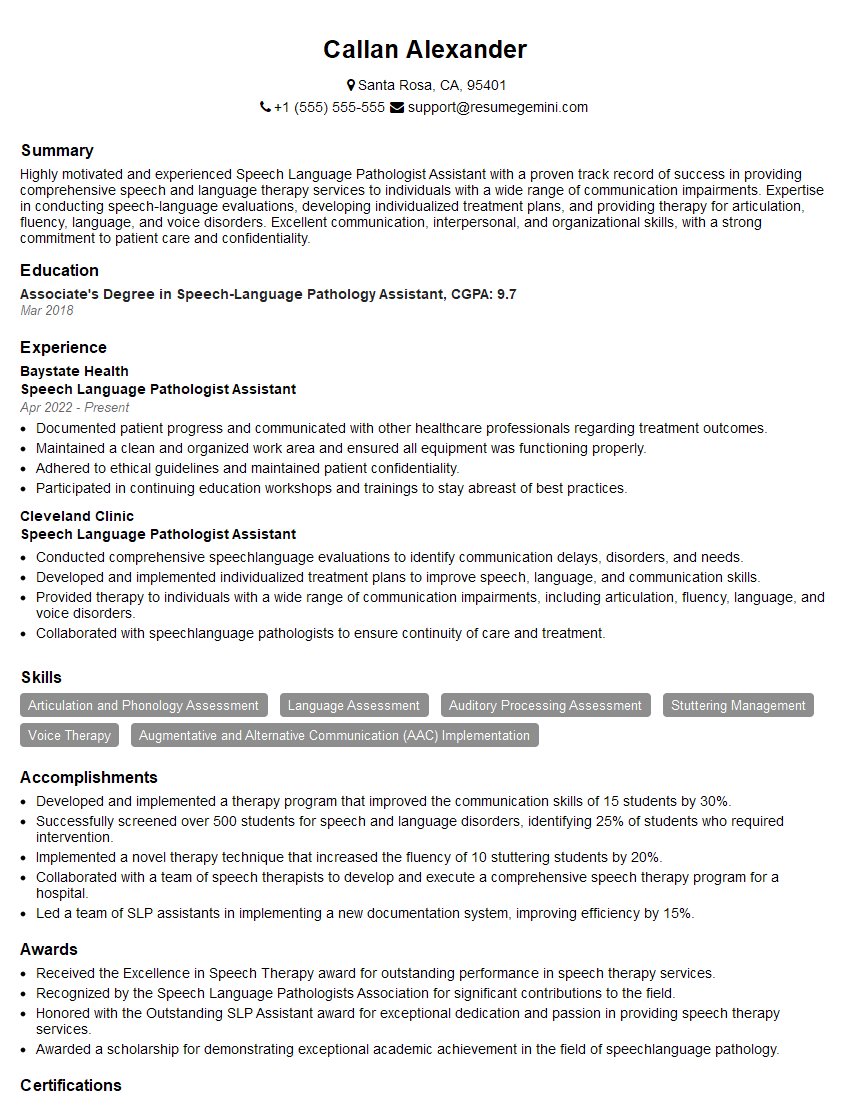
Mastering Speech and Language Impairments opens doors to a rewarding career with diverse opportunities in schools, hospitals, private practices, and research settings. To stand out, a strong, ATS-friendly resume is crucial. ResumeGemini is a trusted resource to help you create a compelling resume that highlights your skills and experience effectively. ResumeGemini provides examples of resumes tailored to Speech and Language Impairments to guide you in building your professional profile. Take the next step towards your dream career today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO