Interviews are more than just a Q&A session—they’re a chance to prove your worth. This blog dives into essential Cerebral Palsy Expertise interview questions and expert tips to help you align your answers with what hiring managers are looking for. Start preparing to shine!
Questions Asked in Cerebral Palsy Expertise Interview
Q 1. Describe the different types of Cerebral Palsy.
Cerebral palsy (CP) is classified based on the type of movement disorder. It’s crucial to remember that CP is a spectrum disorder, meaning the severity and presentation vary greatly from child to child. The main types are:
- Spastic CP: This is the most common type, characterized by increased muscle tone and stiffness. Spasticity can affect different parts of the body, leading to classifications like spastic diplegia (legs primarily affected), spastic hemiplegia (one side of the body), or spastic quadriplegia (all four limbs). Imagine a child struggling to relax their muscles; this is a hallmark of spasticity.
- Dyskinetic CP: This type involves involuntary movements, like writhing or uncontrolled jerking. Athetosis (slow, writhing movements) and chorea (rapid, jerky movements) are common subtypes. Think of a child’s movements appearing almost dance-like, but without voluntary control.
- Ataxic CP: This is less common and involves problems with balance and coordination. Children with ataxic CP often have difficulty with walking and fine motor skills. Imagine a child struggling to walk a straight line or catch a ball, even if they want to.
- Mixed CP: Many children have a combination of these types; for example, they might have spasticity in their legs and athetosis in their arms. This highlights the complexity of the disorder.
Understanding the different types helps tailor treatment plans to address the specific challenges each child faces.
Q 2. Explain the impact of spasticity on motor function in CP.
Spasticity in CP significantly impacts motor function by causing increased muscle tone and resistance to passive movement. This means that the muscles are constantly in a state of tension, making it difficult for the child to move smoothly and voluntarily. For example, a child with spastic diplegia might have stiff legs, making walking challenging and requiring significant effort. The resistance to movement also affects range of motion, potentially leading to contractures (permanent shortening of muscles) and joint deformities. The impact extends beyond movement; it can affect activities of daily living, like dressing and eating, and significantly impact participation in social activities. The severity of spasticity varies, from mild tightness to severe rigidity, impacting the level of support and intervention required. Managing spasticity is a key focus in CP care.
Q 3. What are the common complications associated with Cerebral Palsy?
Children with CP face a range of complications, extending beyond the primary motor impairments. These can include:
- Intellectual disability: While not all children with CP have intellectual disabilities, it’s a common co-occurring condition.
- Epilepsy: Seizures are more frequent in children with CP than in the general population.
- Vision and hearing impairments: These sensory issues can add to the challenges of development and learning.
- Feeding difficulties: Muscle weakness and coordination problems can make eating and swallowing difficult.
- Dental problems: Difficulty with chewing and swallowing can lead to dental issues.
- Communication disorders: Speech and language delays are common.
- Bowel and bladder problems: These can stem from muscle weakness or neurological issues.
- Orthopedic problems: Scoliosis (curvature of the spine), hip dislocations, and contractures are common complications that require ongoing management.
Careful monitoring and proactive intervention are vital to minimize the impact of these complications.
Q 4. Discuss various therapeutic interventions for children with CP.
Therapeutic interventions for children with CP are multifaceted and tailored to the individual’s needs. They aim to improve motor function, maximize independence, and enhance quality of life. These interventions often involve a multidisciplinary team:
- Physiotherapy: Focuses on improving muscle strength, range of motion, and mobility through exercises, stretching, and the use of specialized equipment.
- Occupational therapy: Helps children develop fine motor skills, adapt to their environment, and participate in daily activities.
- Speech therapy: Addresses communication and swallowing difficulties.
- Pharmacological interventions: Medications like botulinum toxin injections (Botox) can temporarily reduce spasticity, while oral medications can manage pain and muscle spasms.
- Surgery: In some cases, surgical interventions may be necessary to correct contractures, improve joint mobility, or reduce spasticity.
- Assistive technology: This plays a crucial role in enhancing independence and participation, as discussed later.
A comprehensive and individualized treatment plan is crucial for optimal outcomes, involving regular monitoring and adjustments as the child develops.
Q 5. How do you assess the gross motor skills of a child with CP?
Assessing gross motor skills in a child with CP involves a combination of methods, tailored to the child’s age and abilities. These include:
- Observation: Watching the child’s spontaneous movements during play and functional tasks provides valuable information about their posture, balance, and coordination.
- Standardized assessments: Tests like the Gross Motor Function Measure (GMFM) provide objective measures of motor performance and track progress over time.
- Clinical examination: Assessing muscle tone, reflexes, range of motion, and postural control provides crucial information about the type and severity of CP.
- Functional assessments: Evaluating the child’s ability to perform daily tasks like sitting, standing, walking, and transferring provides a practical measure of their motor abilities.
The information gathered from these assessments is essential for developing a targeted intervention plan and monitoring progress. It’s important to remember that assessing a child with CP requires sensitivity and careful consideration of their individual needs and limitations.
Q 6. Describe your experience with assistive technology for CP.
My experience with assistive technology (AT) for children with CP is extensive. I’ve seen firsthand how AT can transform their lives. It’s not merely about devices; it’s about empowering independence and participation. This can range from simple devices like adapted utensils for feeding to more complex technology such as:
- Orthotics: Braces and splints can help improve posture, support weakened limbs, and prevent contractures.
- Wheelchairs: Provide mobility and access for children with significant mobility limitations, tailored to their individual needs.
- Adaptive seating systems: Help maintain proper posture and prevent pressure sores, improving comfort and function.
- Communication devices: Augmentative and alternative communication (AAC) systems are essential for children with communication difficulties.
- Mobility aids: Walkers, crutches, and other mobility devices can enhance independence and participation.
Choosing and implementing the right AT involves a collaborative process with the child, family, therapists, and other professionals, ensuring the technology is effective and user-friendly. The goal is to maximize functionality and promote inclusion.
Q 7. Explain your approach to working with families of children with CP.
My approach to working with families of children with CP is built on collaboration, empathy, and shared decision-making. I believe that families are the heart of the child’s care, and their involvement is crucial for successful outcomes. My approach includes:
- Active listening: Understanding the family’s concerns, hopes, and aspirations is paramount. Each family’s experience is unique.
- Shared decision-making: I work collaboratively with families to develop individualized treatment plans that align with their values and priorities.
- Education and support: I provide education about CP, its management, and available resources. Emotional support and practical advice are vital parts of the process.
- Empowerment: I strive to empower families to become active participants in their child’s care, building confidence in their ability to manage their child’s needs.
- Ongoing communication: Maintaining open and consistent communication ensures that the family feels heard and supported throughout the journey.
Building strong, trusting relationships with families is essential for creating a supportive environment that optimizes the child’s development and quality of life.
Q 8. How do you adapt your therapy techniques based on the individual needs of a child with CP?
Adapting therapy for a child with Cerebral Palsy (CP) requires a highly individualized approach. CP is not a one-size-fits-all condition; its impact varies greatly depending on the affected brain areas, the severity of the impairments, and the child’s unique strengths and challenges. My approach begins with a thorough assessment, encompassing physical examination, developmental milestones, and functional abilities. This assessment informs the development of a personalized treatment plan.
For instance, a child with predominantly spastic diplegia (affecting the legs more than the arms) will require different interventions than a child with athetoid CP (characterized by involuntary movements). The former might benefit more from strengthening exercises and bracing, while the latter might need therapy focusing on improving motor control and reducing involuntary movements. We also consider the child’s cognitive abilities, communication skills, and participation in daily activities to tailor the therapy approach. We utilize a variety of techniques including physiotherapy, occupational therapy, speech therapy, and sometimes assistive technology to address specific needs. Regular monitoring and adjustments to the plan are crucial to ensure its ongoing effectiveness and relevance.
For example, one child I worked with had significant difficulties with fine motor skills impacting handwriting. We incorporated adaptive writing tools, alongside targeted exercises to strengthen hand muscles and improve hand-eye coordination. We also used play-based therapy to make the sessions engaging and fun. Another child benefited significantly from hippotherapy (therapy using horses) to improve balance and coordination.
Q 9. What are some common communication challenges in children with CP, and how do you address them?
Communication challenges are common in children with CP, varying widely in nature and severity. The challenges can stem from difficulties with articulation (speaking clearly), receptive language (understanding what others are saying), expressive language (expressing thoughts and needs), or a combination of these. Some children may have apraxia of speech, a neurological disorder affecting the ability to plan and execute the motor movements involved in speech. Others may have dysarthria, which affects the physical aspects of speech production, resulting in slurred or unclear speech.
Addressing these challenges requires a multi-pronged approach. Speech therapy is paramount, focusing on improving articulation, language comprehension, and expressive language skills. Augmentative and alternative communication (AAC) methods, such as picture exchange systems (PECS), sign language, or speech-generating devices, are often incorporated to enhance communication effectiveness. We work closely with the child’s family to ensure consistent communication strategies across all environments, including home and school. Early intervention is particularly important to maximize the child’s communication potential. The aim is not just to improve communication skills but also to empower the child to participate fully in social interactions and learning activities.
For example, we successfully employed a combination of speech therapy and sign language for a child with significant speech difficulties, enabling him to communicate effectively his needs and preferences.
Q 10. Describe your experience with Botox injections or other medical interventions for spasticity in CP.
Botox injections and other medical interventions are sometimes necessary to manage spasticity in children with CP. Botox, a neurotoxin, temporarily weakens overactive muscles, reducing spasticity and improving range of motion. The injections are typically administered in targeted muscle groups, and their effects usually last for several months. I have extensive experience in collaborating with medical professionals, including neurologists and physiatrists, to determine if Botox is a suitable intervention for a given child.
Other medical interventions may include oral medications to manage spasticity, surgical procedures such as selective dorsal rhizotomy (SDR) to reduce spasticity in the legs, and orthopedic surgeries to correct skeletal deformities resulting from muscle imbalances. The decision regarding which intervention is most appropriate is made on a case-by-case basis, considering the child’s specific needs, the severity of spasticity, and potential risks and benefits. We always prioritize the least invasive interventions first and consider the child’s overall health and well-being in the decision making process. Careful monitoring of side effects and effectiveness is crucial after any medical intervention.
For example, one child I worked with experienced significant improvement in mobility and gait after receiving Botox injections in his leg muscles. This allowed him to participate more fully in physical therapy and improve his overall quality of life. We regularly review treatment plans and adjust as necessary to optimize outcomes for each child.
Q 11. How do you measure the effectiveness of your interventions?
Measuring the effectiveness of interventions in CP is a multifaceted process. We utilize a range of outcome measures, both subjective and objective, to track progress. Objective measures might include standardized tests assessing motor skills, such as the Gross Motor Function Measure (GMFM) or the Pediatric Evaluation of Disability Inventory (PEDI). These tests provide quantifiable data that allow for comparison over time and between different interventions.
Subjective measures involve input from the child, parents, and caregivers through questionnaires and observational assessments. These measures capture improvements in areas like participation in daily activities, functional independence, quality of life, and social engagement. We also monitor improvements in range of motion, muscle strength, and coordination, along with any reduction in spasticity or pain. Regular assessments are vital to monitor progress and make adjustments to the therapy plan as needed. Combining both objective and subjective data allows for a comprehensive evaluation of the overall effectiveness of the interventions.
For instance, tracking a child’s progress on the GMFM alongside qualitative feedback from parents about their ability to participate more in family outings provides a holistic view of the impact of therapy.
Q 12. What are some strategies for promoting participation and inclusion for children with CP?
Promoting participation and inclusion for children with CP requires a collaborative effort involving families, educators, and community members. Creating an inclusive environment involves removing physical barriers such as inaccessible buildings or playgrounds and ensuring that accommodations are available as needed. This might involve using ramps, adaptive equipment, or assistive technology. It is also crucial to address attitudinal barriers; education and awareness programs can help foster understanding and acceptance within the community.
Early intervention is key. By providing support and resources early in a child’s development, we can help ensure they have the opportunity to fully participate in educational, social, and recreational activities. Individualized education programs (IEPs) in schools play a crucial role in providing tailored support for academic achievement. We also encourage participation in age-appropriate activities that foster social interaction and skill development, such as adapted sports programs and inclusive community events. Adaptive technology and assistive devices can greatly enhance a child’s ability to participate in activities.
For example, a child with CP might benefit from using a specialized wheelchair to navigate their school and participate in extracurricular activities alongside their peers.
Q 13. How do you collaborate with other healthcare professionals in managing a child with CP?
Managing a child with CP requires a collaborative team approach. I work closely with a variety of healthcare professionals, including neurologists, physiatrists, orthopedic surgeons, occupational therapists, speech therapists, and educators. Regular team meetings are essential to coordinate care and share information, ensuring a holistic approach to the child’s needs. Effective communication and shared decision-making are crucial for the successful management of this complex condition.
For example, we regularly hold case conferences to discuss a child’s progress, review assessment data, and coordinate interventions between different therapists. I also maintain close communication with families and schools to ensure a consistent approach across all environments. This multidisciplinary approach ensures that we address all aspects of the child’s well-being, physical, cognitive, emotional, and social. This collaborative approach also optimizes the efficacy of interventions and improves the overall quality of life for both the child and family.
Q 14. Discuss your knowledge of the latest advancements in Cerebral Palsy research.
Cerebral palsy research is constantly evolving, with exciting advancements in several areas. There’s ongoing research into the genetic basis of CP to better understand the causes and identify potential preventative measures. New diagnostic tools and techniques are being developed for earlier and more accurate diagnosis. Advancements in assistive technologies, such as robotic exoskeletons and brain-computer interfaces, are offering new possibilities for improving mobility and functional independence.
Pharmacological research is focusing on developing new medications to more effectively manage spasticity and other CP-related symptoms. Stem cell therapies are a promising area of investigation, although they are still in the early stages of development. Regenerative medicine approaches show potential for repairing damaged brain tissue and improving motor function. These ongoing advancements provide hope for improving the lives of individuals with CP and for reducing the burden of the condition on families and healthcare systems. Staying abreast of the latest research findings is essential to ensure that I provide the best possible care for my patients and advocate for their needs.
Q 15. Describe your experience with constraint-induced movement therapy (CIMT).
Constraint-induced movement therapy (CIMT) is a powerful rehabilitation technique used to improve motor function in children with cerebral palsy (CP). It’s based on the principle of forcing the affected limb to be used through constraint of the unaffected limb. For example, if a child has weakness in their right arm, we might use a mitt or sling to restrict the use of their left arm, forcing them to use the weaker right arm for everyday tasks.
My experience with CIMT involves extensive application across varying severities of CP. I’ve worked with children using both the traditional CIMT approach and modified versions tailored to individual needs and capabilities. We carefully assess each child to determine the feasibility and appropriate intensity of the therapy. This includes factors like the child’s age, cognitive abilities, and the specific type and severity of their motor impairments. We always prioritize safety and monitor for signs of fatigue or frustration to ensure the therapy remains positive and effective. I’ve seen remarkable improvements in dexterity, coordination, and overall functional abilities in children who have undergone CIMT, enabling them to participate more fully in daily life activities like dressing, writing, and playing.
Success often hinges on a comprehensive approach that includes not just the therapy sessions but also the child’s motivation, family involvement, and carry-over activities practiced at home. We provide detailed instructions and support to families to maximize the effectiveness of the CIMT program.
Career Expert Tips:
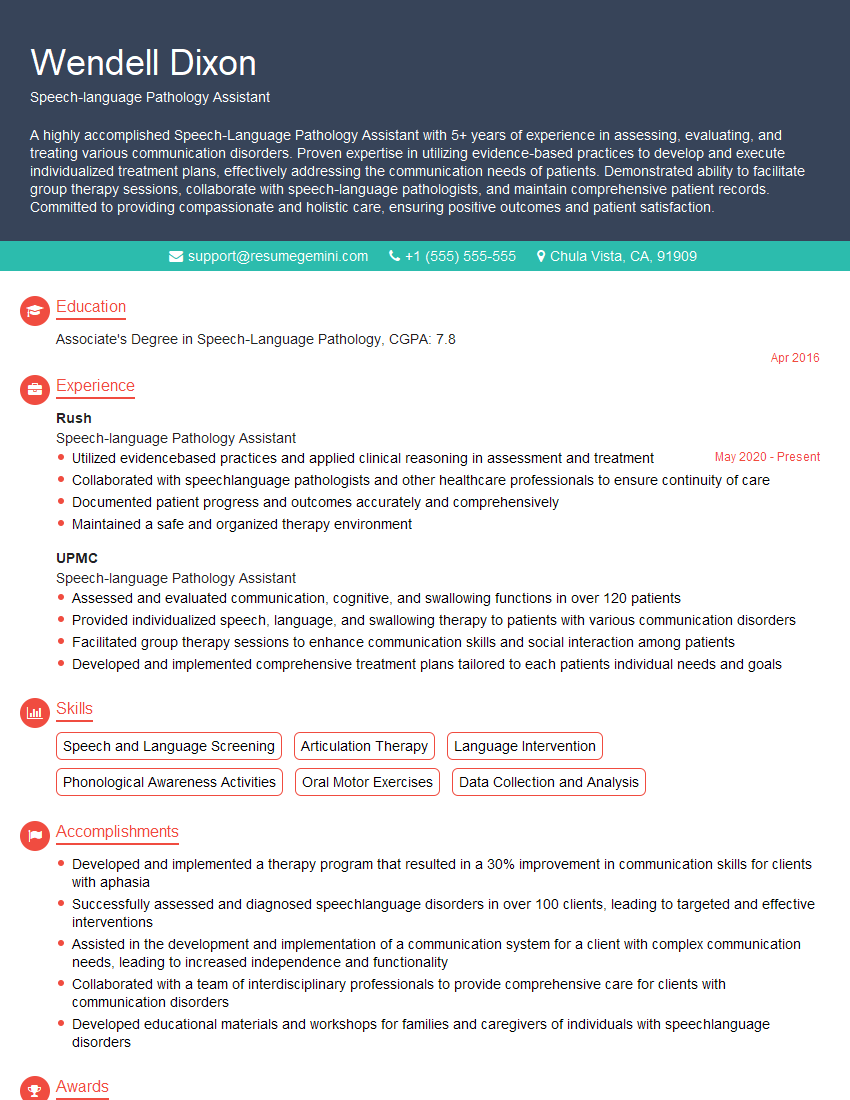
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you manage the emotional and psychological well-being of children with CP?
Managing the emotional and psychological well-being of children with CP is crucial and integrated into every aspect of their care. Many children with CP and their families face significant challenges, including physical limitations, social stigma, and the emotional toll of ongoing therapies. My approach involves a multi-pronged strategy.
- Open Communication: Establishing a safe space for open communication with both the child and their family is paramount. This allows us to identify and address anxieties, frustrations, or feelings of isolation.
- Individualized Support: We recognize that each child’s emotional needs are unique. Some may benefit from play therapy, while others might require counseling or support groups. We collaborate with psychologists, therapists, and social workers to provide tailored support.
- Family Involvement: Supporting the family is essential. Parents often experience emotional distress and need guidance and resources to cope with the challenges of raising a child with CP. We offer workshops, individual counseling, and peer support groups to address their needs.
- Positive Reinforcement: Focusing on the child’s strengths and celebrating their achievements, no matter how small, is vital for building confidence and self-esteem. This might involve goal setting, positive feedback, and acknowledging their efforts.
Creating a positive and supportive therapeutic environment where children feel empowered and celebrated is key to promoting their overall well-being.
Q 17. What is your approach to family education and training related to CP?
Family education and training are cornerstones of successful CP management. We believe that families are integral members of the therapeutic team and equip them with the knowledge and skills to actively participate in their child’s care. Our approach is comprehensive and multifaceted.
- Initial Assessment and Education: We begin by providing a thorough explanation of CP, its implications, and the various treatment options available. We address any misconceptions and answer family’s questions.
- Practical Training: We provide hands-on training on techniques like positioning, handling, and assisting with daily routines. This might include demonstrations, practice sessions, and visual aids.
- Developmental Milestones: We educate families about typical developmental milestones and help them understand how these might be affected by CP. This empowers them to monitor their child’s progress and identify any potential delays or concerns.
- Resource Provision: We connect families with relevant resources, including support groups, advocacy organizations, and financial assistance programs.
- Ongoing Support: We provide ongoing support through regular check-ins, follow-up appointments, and access to our team for any questions or concerns.
Empowering families with knowledge and skills allows them to actively participate in their child’s care, resulting in improved outcomes and enhanced family well-being.
Q 18. Describe your experience with selective dorsal rhizotomy (SDR).
Selective dorsal rhizotomy (SDR) is a surgical procedure that can reduce spasticity in children with CP. It involves selectively cutting some of the sensory nerve roots entering the spinal cord. My experience involves thorough pre-operative evaluation and post-operative rehabilitation planning. The decision to proceed with SDR is made only after careful consideration of the child’s condition, potential benefits, and risks. Not all children with CP are candidates for SDR.
Pre-operatively, we conduct extensive assessments, including neurological examinations, muscle strength testing, and functional evaluations. We collaborate with the surgical team and discuss the potential benefits and risks with the family, emphasizing that SDR is not a cure but a tool that may improve function. Post-operatively, an intensive rehabilitation program is crucial for maximizing the benefits of the surgery. This includes physical therapy, occupational therapy, and potentially other therapies, tailored to the individual child’s needs.
It’s important to note that SDR is a complex procedure with potential complications, and success varies. Close monitoring and ongoing rehabilitation are essential for optimal outcomes.
Q 19. How do you use evidence-based practice in your work with children with CP?
Evidence-based practice (EBP) is the cornerstone of my work with children with CP. It means integrating the best available research evidence with clinical expertise and patient values to make informed decisions about treatment.
I consistently review the latest research on CP treatments, including new therapies, medications, and surgical techniques. I actively participate in professional development activities to stay updated on the latest evidence and best practices. For instance, I might incorporate findings from recent studies on the effectiveness of certain exercise regimens or assistive devices into my treatment plans. When making decisions regarding a child’s care, I consider not only the scientific evidence but also the individual child’s unique needs, preferences, and family values. The treatment plan will often evolve in response to the child’s progress and changing needs.
Maintaining a commitment to EBP ensures that I provide the highest quality care and continuously improve my clinical practice based on the best available evidence.
Q 20. Explain your understanding of the developmental milestones of children with CP.
Understanding the developmental milestones of children with CP requires considering that their development may be delayed or atypical compared to typically developing children. However, they still follow developmental trajectories, albeit often at a different pace and with variations depending on the type and severity of their CP.
We assess progress based on established developmental scales, modified to account for their physical limitations. For example, a child with significant motor impairments might achieve sitting independently later than their peers, but we’d still track their progress toward that goal. We may use adaptive assessments to evaluate developmental domains like gross motor skills (e.g., sitting, crawling, walking), fine motor skills (e.g., grasping, writing), language, and cognitive development. We adapt our assessment and therapies to account for the specific challenges a child faces.
It’s important to remember that each child with CP is unique, and their developmental trajectory will vary. Regular monitoring and individualized interventions are essential to support their development and maximize their potential.
Q 21. Describe the difference between hypotonia and hypertonia in CP.
Hypotonia and hypertonia are two contrasting muscle tone abnormalities often associated with cerebral palsy.
- Hypotonia: This refers to decreased muscle tone or floppiness. Children with hypotonia often have difficulty maintaining posture, and their movements may appear weak and sluggish. They might have difficulty with head control, sitting, or walking. Think of a rag doll – it has very little resistance to movement.
- Hypertonia: This refers to increased muscle tone or stiffness. Children with hypertonia may exhibit spasticity, where muscles are constantly tense and resistant to movement. This can lead to contractures (shortening of muscles), difficulty with range of motion, and abnormal postures. Think of a tightly wound spring – it resists being moved.
Both hypotonia and hypertonia can significantly impact a child’s motor development and functional abilities. The type of muscle tone abnormality significantly influences the type of therapeutic interventions required. For example, a child with hypotonia may benefit from strengthening exercises, while a child with hypertonia may require stretching, splinting, and possibly medication or surgery to manage spasticity.
Q 22. What are the long-term implications of CP, and how do you help families prepare for the future?
Cerebral palsy (CP) is a lifelong condition, so understanding its long-term implications is crucial for families. These implications vary greatly depending on the type and severity of CP, but can include physical limitations affecting mobility, dexterity, and independence; communication challenges ranging from mild articulation difficulties to severe speech impairments; cognitive differences, which can impact learning and daily living skills; and potential secondary conditions like scoliosis, epilepsy, or visual impairments.
To help families prepare, we utilize a holistic approach. This includes comprehensive assessments to understand the child’s specific needs and potential trajectory. We then work collaboratively with families, creating individualized plans that address immediate concerns and proactively plan for the future. This might involve connecting them with resources like specialized education programs, assistive technology services, and support groups. We also help families learn about available financial assistance, long-term care options, and advocacy resources. For example, we might guide a family toward exploring options for accessible housing as their child grows, or assist them in navigating the process of obtaining durable medical equipment. Open communication and realistic goal setting are key to empowering families to navigate the future with confidence and hope.
Q 23. How do you create a safe and supportive therapeutic environment for children with CP?
Creating a safe and supportive therapeutic environment for children with CP is paramount. Safety involves minimizing fall risks, securing furniture, and modifying the environment to accommodate the child’s mobility challenges. For example, using soft mats on the floor, installing grab bars in the bathroom, and ensuring appropriate wheelchair accessibility.
Support involves creating an atmosphere of acceptance, understanding, and encouragement. This requires a multidisciplinary approach, with therapists working collaboratively to provide a consistent, integrated therapeutic plan. We focus on promoting the child’s independence and self-esteem through play-based therapy, adaptive activities, and goal-oriented exercises. For instance, we might use adaptive toys that encourage fine motor skills, modify game rules to facilitate participation, and celebrate even the smallest milestones. Communication with caregivers is essential, sharing progress, concerns, and suggestions to ensure consistency between therapy sessions and home life. A positive, encouraging environment fosters the child’s motivation and participation, maximizing the effectiveness of therapy.
Q 24. Describe your experience with baclofen pumps or other implantable devices for spasticity management.
I have extensive experience with baclofen pumps and other implantable devices for spasticity management in children with CP. A baclofen pump delivers medication directly to the spinal cord, reducing muscle spasms and improving function. The decision to use a baclofen pump involves careful consideration of the child’s condition, potential benefits, and risks. Before implantation, a thorough assessment is done to determine candidacy. Post-implantation, close monitoring is vital, including regular adjustments to medication dosage and managing potential side effects. Other implantable devices, such as selective dorsal rhizotomy (SDR), a surgical procedure to reduce spasticity, are also considered in appropriate cases.
The success of these procedures depends on a comprehensive approach involving physical therapy, occupational therapy, and ongoing medical management. For instance, following SDR surgery, intense physical and occupational therapy are crucial to maximize the benefits of the reduced spasticity. Each case is unique, and the decision about which intervention is best is made on a case-by-case basis in close collaboration with the family and a multidisciplinary team of specialists.
Q 25. How do you adapt your communication style to meet the needs of individuals with CP?
Adapting communication styles is crucial when working with individuals with CP. This involves understanding that communication challenges can vary widely, from mild articulation difficulties to more significant impairments requiring augmentative and alternative communication (AAC) methods. I always begin by observing the individual’s communication methods and preferences.
For children with limited verbal skills, I might use visual aids, such as picture cards or communication boards. For those with more advanced verbal skills, I use clear, concise language, avoiding jargon and complex sentence structures. I also use active listening techniques, paying close attention to nonverbal cues like facial expressions and body language. Patience and empathy are essential. It’s important to allow ample time for the individual to communicate, avoiding interrupting or rushing them. Collaboration with speech-language pathologists is crucial to ensure the implementation of effective communication strategies and, where necessary, the selection and training on appropriate AAC methods.
Q 26. Explain your understanding of the ethical considerations when working with children with disabilities.
Ethical considerations are paramount when working with children with disabilities. These revolve around ensuring the child’s best interests are always prioritized, promoting autonomy and participation in decision-making to the greatest extent possible, respecting the family’s values and beliefs, maintaining confidentiality, and ensuring equitable access to resources and opportunities.
For example, informed consent from parents or guardians is crucial before initiating any interventions. When the child is old enough, we gradually involve them in decision-making processes appropriate to their developmental level, fostering their sense of agency. We strive to create an inclusive and non-discriminatory environment, recognizing that each child possesses unique strengths and abilities. Navigating ethical dilemmas may require consultations with ethics committees or colleagues to ensure the child’s rights and welfare are consistently protected. Transparency and open communication with families are key to maintaining trust and ethical practice.
Q 27. Describe your experience with different types of adaptive equipment for CP.
My experience encompasses a wide range of adaptive equipment for CP. This includes mobility devices like wheelchairs (manual and powered), walkers, and gait trainers; seating systems that provide proper postural support and pressure relief; communication aids such as speech-generating devices and communication boards; and adaptive utensils, toys, and clothing to enhance independence in daily living.
Selecting the right equipment is a collaborative process involving the child, family, therapists, and other professionals. We consider the child’s specific needs, functional abilities, and preferences. For instance, we might assess the child’s posture and mobility needs to select an appropriate wheelchair. We would also consider the child’s age, interests, and lifestyle to select adaptive toys that are engaging and promote skill development. Regular assessment and adjustments are crucial to ensure the equipment continues to meet the child’s evolving needs throughout their growth and development.
Q 28. What are some common challenges in assessing cognitive function in children with CP?
Assessing cognitive function in children with CP presents unique challenges. Motor impairments can interfere with standardized cognitive tests that require fine motor skills or verbal responses. For example, a child with severe motor limitations might struggle to manipulate objects required in a traditional IQ test, leading to an underestimation of their true cognitive abilities.
To overcome these challenges, we use a combination of standardized and non-standardized assessments. We might adapt standardized tests or use alternative assessment methods that rely less on fine motor skills. Observational measures, parent/caregiver reports, and functional assessments are vital for gaining a holistic understanding of the child’s cognitive abilities. We look for adaptive strategies the child may be using to compensate for motor limitations. For instance, we might observe how the child engages in play, solves problems, and interacts with others. Collaboration with other professionals, such as psychologists and educators, is crucial for a comprehensive evaluation and informed intervention planning.
Key Topics to Learn for Cerebral Palsy Expertise Interview
- Classifications of Cerebral Palsy: Understand the different types of CP (spastic, athetoid, ataxic, mixed), their characteristics, and associated challenges.
- Diagnosis and Assessment: Familiarize yourself with common diagnostic methods, including neurological examinations, imaging techniques (MRI, CT), and developmental assessments.
- Therapeutic Interventions: Explore various therapeutic approaches like physiotherapy, occupational therapy, speech therapy, and assistive technology. Be prepared to discuss their applications and effectiveness.
- Pharmacological Management: Understand the role of medication in managing symptoms such as spasticity, pain, and seizures. Be aware of common medications and their potential side effects.
- Surgical Interventions: Gain knowledge of surgical options available for individuals with CP, such as selective dorsal rhizotomy and orthopedic surgeries. Understand the indications and potential outcomes.
- Developmental Milestones and Support: Familiarize yourself with typical developmental milestones and how CP can affect their achievement. Discuss strategies for supporting development across various domains.
- Family and Caregiver Support: Understand the crucial role of family and caregivers in the management of CP and the importance of providing comprehensive support and education.
- Adaptive Equipment and Assistive Technology: Be prepared to discuss the various types of adaptive equipment and assistive technologies that can improve independence and quality of life.
- Ethical Considerations: Understand ethical issues related to diagnosis, treatment, and decision-making in CP, such as informed consent and resource allocation.
- Current Research and Future Directions: Stay updated on the latest research advancements in the field, including potential therapies and technological innovations.
Next Steps
Mastering Cerebral Palsy Expertise significantly enhances your career prospects in healthcare, research, or education. A strong understanding of this complex field demonstrates commitment and specialized knowledge highly valued by employers. To maximize your job search success, it’s crucial to create an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional and impactful resume, ensuring your application gets noticed. Examples of resumes tailored to Cerebral Palsy Expertise are available to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO