The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Speech and Language Therapy Assistance interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Speech and Language Therapy Assistance Interview
Q 1. Describe your experience assisting with speech and language assessments.
Assisting with speech and language assessments involves a multifaceted approach, ranging from observation to formal testing. My experience includes administering standardized tests like the Goldman-Fristoe Test of Articulation or the Clinical Evaluation of Language Fundamentals (CELF), as well as conducting informal assessments tailored to the individual’s needs. This involves observing spontaneous speech samples, assessing receptive and expressive language skills, and evaluating oral-motor skills. I meticulously document findings, noting strengths and weaknesses in areas such as articulation, phonology, fluency, grammar, vocabulary, and pragmatics. For example, with a young child, I might use play-based activities to elicit language samples while assessing their ability to follow instructions or engage in conversation. For adults, I’ve utilized more formal testing methods to identify underlying causes for communication difficulties, such as after a stroke or traumatic brain injury. Ultimately, the goal is to provide the Speech-Language Pathologist (SLP) with a comprehensive profile to inform diagnosis and treatment planning.
Q 2. Explain your understanding of articulation disorders.
Articulation disorders are difficulties producing speech sounds correctly. These difficulties can range from mild to severe and affect intelligibility. There are several types: substitutions (saying ‘wabbit’ for ‘rabbit’), omissions (leaving out sounds like saying ‘cat’ for ‘scat’), distortions (producing sounds imprecisely), and additions (adding extra sounds like saying ‘buh-lue’ for ‘blue’). The causes can vary widely, ranging from developmental delays to structural issues like cleft palate, hearing loss, or neurological conditions. I understand the importance of differentiating articulation disorders from phonological disorders, where the underlying sound system is affected, rather than just the motor production of individual sounds. For instance, a child with a phonological disorder might consistently simplify consonant clusters, like saying ‘top’ instead of ‘stop’, indicating a pattern rather than isolated sound errors. My role involves carefully documenting observed errors, helping to distinguish between these different types of speech sound disorders.
Q 3. How do you support clients with fluency disorders?
Supporting clients with fluency disorders, such as stuttering, requires a compassionate and individualized approach. My support involves creating a calm and encouraging environment where clients feel comfortable expressing themselves without pressure. I assist the SLP by implementing strategies such as easy onset techniques (starting words with a softer, less tense sound), slow and controlled speech rate, and pausing strategically. We might use techniques like ‘pull-outs’ (stopping mid-stutter to gently ease into the next sound), or ‘preparatory sets’ (mentally rehearsing a sentence before saying it). I also help to track the client’s progress and document responses to therapy. Further, I help with educating the client and their family about fluency disorders, helping to alleviate anxieties and promote positive self-perception. For example, I’ve helped design and run group sessions focused on building self-esteem and coping skills for adults who stutter, emphasizing the importance of self-acceptance and finding strategies that work for each individual.
Q 4. What are some common language delays you’ve encountered?
Common language delays I’ve encountered include difficulties with vocabulary acquisition (limited word knowledge for their age), expressive language (struggles formulating sentences and expressing ideas), receptive language (difficulty understanding spoken language), and pragmatic language (challenges with social use of language, such as turn-taking in conversation). For example, a preschooler might have a small vocabulary and use simple, telegraphic sentences, while an older child might struggle to understand complex instructions or engage in sustained conversations. These delays can manifest differently depending on the child’s age and developmental stage. My role in identifying these delays involves actively listening to spontaneous speech samples, engaging in interactive play activities, and carefully observing the child’s communication attempts. These observations contribute vital information for the SLP to assess the nature and severity of the delay, leading to targeted intervention.
Q 5. Describe your experience working with augmentative and alternative communication (AAC) devices.
My experience with augmentative and alternative communication (AAC) devices encompasses a range of technologies, from low-tech options like picture exchange systems (PECS) to high-tech devices such as speech-generating devices (SGDs). I’ve assisted in training clients and their families on how to effectively use these devices, adapting the training to their individual needs and cognitive abilities. This involves explaining the functionality of the device, creating personalized communication boards or systems, and providing ongoing support and troubleshooting assistance. For instance, I helped a non-verbal child learn to use a PECS system to communicate his wants and needs. With another client, I assisted in programming an SGD with appropriate vocabulary and phrases for effective communication. A key aspect of my role is ensuring the device becomes a truly effective communication tool, integrated into the client’s daily life.
Q 6. How do you adapt your approach for clients with different cognitive abilities?
Adapting my approach for clients with varying cognitive abilities is crucial for effective communication and therapy. I work closely with the SLP to understand the client’s cognitive profile and tailor activities accordingly. For clients with mild cognitive impairments, we might use more complex tasks and activities, while for those with more significant cognitive challenges, we might employ simpler, more concrete methods, focusing on functional communication skills. This includes using visual aids, simplifying instructions, breaking down tasks into smaller steps, and utilizing repetition to reinforce learning. It’s vital to be patient and celebrate even the smallest achievements, focusing on building confidence and promoting successful communication. For example, I might use visual schedules to help a client with cognitive impairment understand the daily routine, or utilize hands-on activities to promote language learning for a client with developmental delays.
Q 7. Explain your knowledge of developmental milestones in speech and language.
Understanding developmental milestones in speech and language is essential for identifying potential delays or disorders. These milestones are age-related benchmarks that indicate typical progress. For example, infants are expected to babble around 6 months, produce first words around 12 months, and begin combining words into simple sentences by 18-24 months. Preschoolers should be expanding their vocabulary, developing more complex sentence structures, and improving their narrative skills. School-aged children continue to refine their language abilities, developing more sophisticated vocabulary, grammar, and pragmatic skills. Deviation from these expected milestones might indicate a potential need for intervention. I utilize my knowledge of these milestones to assist in the early identification of potential delays, by helping the SLP compare a child’s actual performance against expected abilities, contributing crucial information for early intervention.
Q 8. How do you maintain client confidentiality?
Maintaining client confidentiality is paramount in speech and language therapy. It’s not just a professional obligation; it’s the cornerstone of trust and a crucial element in fostering a therapeutic relationship. I adhere to strict confidentiality protocols, starting with secure storage of all client records – both physical and electronic. This includes password-protected electronic files stored on HIPAA-compliant servers and locked filing cabinets for paper records. I never discuss client information with anyone outside the treatment team unless legally required to do so.
For instance, if a client shares sensitive information during a session, I would never repeat it casually to a colleague or family member. I always anonymize case details when discussing them for educational or supervisory purposes. Ethical considerations guide my actions, always prioritizing client privacy above all else.
Q 9. Describe your experience with data collection and reporting in speech therapy.
Data collection and reporting are essential for tracking progress, measuring treatment effectiveness, and making informed decisions. My experience involves a multi-faceted approach. I use a variety of tools, including standardized assessments (like the CELF-5 or Goldman-Fristoe Test of Articulation) which provide objective data on specific speech and language skills. I also incorporate informal measures, like observational notes and frequency counts, to capture more nuanced aspects of a client’s performance in natural settings.
For reporting, I prepare clear and concise summaries that highlight key findings, goals achieved, and remaining challenges. I use graphs and charts to visually represent progress over time. This data is then shared with the speech-language pathologist and relevant stakeholders, such as parents or educators. Imagine charting a child’s articulation progress – a graph showing a clear increase in correct consonant production over several sessions paints a vivid picture of success and motivates both the child and the therapist.
Q 10. How do you document client progress effectively?
Effective documentation is the backbone of successful speech therapy. I utilize a combination of methods to ensure comprehensive and accurate progress notes. Firstly, I document session objectives and the methods used to achieve them. Then I meticulously record the client’s responses, including both quantitative and qualitative data. Quantitative data might include the number of correct responses on a specific task; qualitative data might encompass observations about their engagement, effort, and emotional responses.
For example, I wouldn’t simply write ‘Client practiced producing /s/ sounds.’ Instead, I might write, ‘Client practiced producing /s/ sounds in initial, medial, and final positions. Accuracy improved from 60% to 75% compared to last session. Client showed increased frustration during the blending task but was encouraged to continue through positive reinforcement.’ This level of detail provides the speech-language pathologist with a comprehensive understanding of the session’s progress and allows for informed decision-making.
Q 11. Explain your understanding of different therapeutic techniques used in speech therapy.
My understanding of therapeutic techniques spans a broad range, adapting to individual client needs. For articulation disorders, I utilize techniques like modeling, prompting, and shaping to help clients produce correct sounds. For language disorders, I employ approaches like focused stimulation, recasting, and parallel talk to expand vocabulary and improve sentence structure. I’m also proficient in augmentative and alternative communication (AAC) strategies for individuals with significant communication challenges.
For example, with a child struggling with articulation, I might use a combination of visual aids, tactile cues, and verbal feedback. For a client with aphasia (language impairment), I might use melodic intonation therapy to enhance their expressive language. The key is selecting the techniques best suited to the client’s specific diagnosis and communication profile. Therapy is a personalized journey, not a one-size-fits-all solution.
Q 12. How do you collaborate effectively with speech-language pathologists?
Collaboration with speech-language pathologists is integral to providing the best possible client care. My role involves actively contributing to the therapeutic process by implementing the treatment plan developed by the SLP, providing detailed progress reports, and actively participating in team meetings. I maintain open and frequent communication, reporting any observations or concerns promptly. I view myself as an extension of the SLP, working seamlessly to achieve common goals.
For instance, if I notice a client is responding particularly well to a specific technique or struggling with a particular aspect of the treatment plan, I’ll immediately communicate this to the SLP. This collaborative approach ensures the treatment remains effective, adaptive, and tailored to the client’s evolving needs.
Q 13. How do you handle challenging client behaviors?
Handling challenging client behaviors requires patience, understanding, and a well-structured approach. I begin by analyzing the underlying cause of the behavior. Is it a result of frustration, anxiety, sensory overload, or something else? Once the cause is identified, I collaborate with the SLP to develop strategies to address it. This may involve modifying the therapy environment, adjusting the activity, incorporating breaks, using positive reinforcement, or implementing behavior management techniques. Documentation of these strategies and their effectiveness is crucial.
For example, if a client is exhibiting disruptive behaviors due to frustration with a task, I might break the task into smaller, more manageable steps, provide frequent positive reinforcement, or introduce a visual schedule to reduce anxiety. The goal is to create a supportive and therapeutic environment where the client feels safe and empowered to participate actively.
Q 14. Describe your experience working with diverse populations.
I have extensive experience working with diverse populations, encompassing various age groups, cultural backgrounds, and communication needs. This involves sensitivity to cultural differences in communication styles, adapting my approach to accommodate diverse learning styles, and ensuring materials are culturally relevant. I understand that effective communication transcends language and involves understanding non-verbal cues, individual learning preferences, and respecting cultural nuances.
For example, when working with a client from a different cultural background, I’d take time to learn about their cultural values and communication norms. This might involve researching their culture beforehand or discussing their preferences and expectations during our initial sessions. My approach is always person-centered, prioritizing the individual’s unique strengths and needs regardless of their background.
Q 15. How do you ensure a safe and therapeutic environment for clients?
Creating a safe and therapeutic environment for clients is paramount. It’s about fostering a space where they feel comfortable, respected, and empowered to participate fully in therapy. This involves several key elements:
- Physical Safety: This includes ensuring the therapy area is free from hazards, well-lit, and appropriately furnished. For example, removing tripping hazards, securing loose objects, and providing appropriate seating that caters to individual needs (e.g., wheelchairs, adaptive seating).
- Emotional Safety: This is crucial. Building rapport, active listening, and demonstrating empathy are key. I always start sessions by checking in with the client about their emotional state and adjust the session accordingly. If a client is feeling anxious, we might start with a calming activity before tackling more challenging tasks. Maintaining confidentiality is also essential.
- Sensory Considerations: We need to consider the sensory environment. For clients with sensory sensitivities (e.g., autism spectrum disorder), minimizing distractions like loud noises or bright lights is crucial. We might use calming sensory tools, like weighted blankets or fidget toys, to create a more comfortable space.
- Privacy and Confidentiality: I always ensure sessions take place in a private space where conversations cannot be overheard. I explicitly explain confidentiality policies and their implications at the start of therapy.
Ultimately, a safe and therapeutic environment is a collaborative effort. It’s about actively listening to client feedback and adapting the space and approach to meet their individual needs.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your knowledge of HIPAA regulations.
HIPAA (Health Insurance Portability and Accountability Act) regulations are critical for protecting patient privacy. I understand that protected health information (PHI) – which includes anything that can be used to identify a client and relates to their past, present, or future physical or mental health, including their provision of healthcare – must be handled with the utmost care. My understanding covers:
- Confidentiality: I am meticulous about not discussing client information with anyone who isn’t directly involved in their care. I never leave client files unattended, and I use secure methods for storing and transmitting data.
- Access Control: Only authorized individuals have access to client records, and access is logged for auditing purposes. This aligns with HIPAA’s rules on who is allowed to see a patient’s information.
- Data Security: I use secure systems for electronic health records (EHRs) and follow best practices for data encryption and password protection. I also know the importance of appropriate disposal methods for physical records, such as shredding.
- Breach Notification: I understand the procedures for handling a potential breach of PHI, including immediate reporting to appropriate authorities and affected individuals.
Essentially, HIPAA compliance is not just about following rules; it’s about demonstrating a commitment to responsible data handling and respecting clients’ privacy rights.
Q 17. Describe your experience with different types of therapy materials and equipment.
My experience encompasses a wide array of therapy materials and equipment, tailored to different age groups and communication needs.
- Articulation therapy: I use articulation cards, mirrors, and apps to target specific sounds. For example, I might use picture cards featuring words beginning with the /s/ sound to practice articulation.
- Language therapy: I utilize picture books, board games, and storytelling activities to enhance vocabulary, grammar, and narrative skills. Role-playing scenarios, often involving puppets or dolls, are also incorporated to practice social communication.
- Augmentative and alternative communication (AAC): I am experienced in using various AAC systems, including picture exchange systems (PECS), speech-generating devices (SGDs), and sign language. The selection of AAC depends entirely on the individual’s needs and preferences.
- Voice therapy: This often involves specialized equipment, such as voice recorders and visual feedback tools. These help clients track their vocal parameters and monitor their progress.
- Fluency therapy: Relaxation techniques and pacing boards are employed to assist individuals who stutter.
My selection of materials is always client-centered. I carefully consider the client’s age, diagnosis, interests, and learning style to ensure the therapy is engaging and effective.
Q 18. How do you prioritize tasks and manage your time effectively?
Effective time management and task prioritization are critical in a busy speech therapy practice. I use a combination of strategies:
- Prioritization Matrix: I use a system like the Eisenhower Matrix (urgent/important) to categorize tasks. This helps me focus on high-priority activities first, ensuring efficient use of my time.
- Scheduling and Planning: I maintain a detailed schedule for client appointments and allocate specific time slots for documentation, report writing, and continuing education activities. I use a digital calendar to ensure I stay on track.
- Time Blocking: I dedicate specific blocks of time for focused work, minimizing interruptions. This allows for deeper concentration on complex tasks.
- Delegation (where applicable): In a team environment, I effectively delegate tasks that can be handled by others, optimizing overall team efficiency.
- Regular Review and Adjustment: I regularly review my schedule and prioritize tasks based on client needs and deadlines. If needed, I adjust my schedule to maintain optimal workflow and prevent burnout.
Proactive planning and flexible adaptation are key to effective time management in this dynamic field.
Q 19. How do you stay current with best practices in speech therapy?
Staying current with best practices in speech therapy is ongoing. I actively engage in several strategies:
- Professional Development Courses: I regularly attend workshops, conferences, and webinars related to speech-language pathology, focusing on areas such as new treatment techniques, technologies, and research findings.
- Journal Reading: I subscribe to relevant professional journals like the American Journal of Speech-Language Pathology and regularly review published research and clinical reports to stay updated on the latest evidence-based practices.
- Membership in Professional Organizations: Active membership in organizations like the American Speech-Language-Hearing Association (ASHA) provides access to resources, publications, and networking opportunities.
- Continuing Education Units (CEUs): I complete required CEUs to maintain my professional license and enhance my skills. I choose courses that align with my clinical interests and address gaps in my knowledge.
- Networking with Colleagues: I actively engage in discussions with fellow speech-language pathologists to learn from their experiences and share knowledge.
Continuous learning is not merely a requirement; it’s a passion. It ensures I can provide the best possible care to my clients, incorporating the most effective and up-to-date techniques.
Q 20. Describe your experience with electronic health records (EHRs).
I have extensive experience with electronic health records (EHRs). I’m proficient in using EHR systems to:
- Document client sessions: I accurately record assessment findings, treatment plans, progress notes, and session details, ensuring data integrity and providing a comprehensive record of the client’s journey.
- Manage client information: I use EHRs to securely store and access client demographic data, medical history, and other relevant information.
- Generate reports: I’m adept at creating reports for insurance companies, schools, and other stakeholders, summarizing client progress and justifying treatment needs. I understand the importance of compliant reporting.
- Schedule appointments: EHR systems streamline appointment scheduling and provide reminders for clients and myself.
- Track billing and insurance: Many EHR systems are integrated with billing functions, simplifying claims submission and insurance processes.
Beyond proficiency, I appreciate the efficiency and data management benefits of EHRs. They help maintain organized records, facilitate collaboration, and improve the overall quality of care.
Q 21. How do you handle emergencies or unexpected situations?
Handling emergencies or unexpected situations requires preparedness and quick thinking. My approach involves:
- Immediate Assessment: I prioritize assessing the situation and identifying the immediate needs. This could be anything from a client experiencing a medical emergency to an unexpected disruption in the therapy session.
- Prioritized Action: Depending on the situation, I might implement first aid, seek medical assistance, or adapt the therapy session to address the unexpected event. For example, if a client experiences an anxiety attack, I would implement calming techniques, such as deep breathing exercises, before resuming therapy. If a client shows signs of a medical emergency (difficulty breathing, chest pain), I will call for medical assistance immediately.
- Communication: In case of a significant incident, I will clearly and effectively communicate with the client’s family, relevant healthcare providers, and my supervisor.
- Documentation: A thorough record of the incident, including the actions taken, is crucial for legal and clinical purposes.
- Post-Incident Debriefing: After the emergency has passed, a self-reflection and possible debriefing with my supervisor or colleagues allows for learning and improvement in handling future situations.
Preparation through training and experience helps in effectively managing unexpected challenges, ensuring client safety, and minimizing disruption to the therapy process.
Q 22. Explain your understanding of the roles and responsibilities of an SLPA.
As a Speech-Language Pathology Assistant (SLPA), my role is to work under the supervision of a licensed Speech-Language Pathologist (SLP). We are a vital part of the therapy team, providing direct client services and contributing to the overall treatment plan. My responsibilities encompass a wide range of tasks, all designed to support the SLP’s goals and improve client outcomes.
- Direct Client Services: This includes implementing the treatment plans created by the SLP, conducting individual and group therapy sessions, and practicing targeted skills with clients. I might work on articulation, fluency, language, or social communication depending on the client’s needs.
- Data Collection and Documentation: I meticulously record client progress, noting responses to therapy interventions. This detailed documentation helps the SLP monitor progress and make necessary adjustments to the treatment plan.
- Material Preparation and Organization: I create and organize materials needed for therapy sessions, ensuring a well-structured and engaging learning environment. This could include creating games, worksheets, or adapting existing materials to suit a client’s specific needs.
- Collaboration and Communication: Effective communication with the supervising SLP, clients, parents/guardians, and other professionals involved in the client’s care is crucial. I provide regular updates to the SLP and actively participate in team meetings.
- Continuing Education: I am committed to ongoing professional development to stay current with best practices in speech-language pathology.
Essentially, I act as an extension of the SLP, carrying out the prescribed therapy and providing valuable support in achieving the client’s communication goals.
Q 23. How do you build rapport and trust with clients and their families?
Building rapport and trust with clients and their families is fundamental to successful therapy. I prioritize creating a safe, non-judgmental, and welcoming environment. I achieve this through several strategies:
- Active Listening and Empathy: I actively listen to their concerns, perspectives, and experiences. Showing genuine empathy helps them feel understood and valued.
- Positive Reinforcement and Encouragement: I consistently provide positive reinforcement, celebrating even small successes to build confidence and motivation. Encouragement fosters a sense of accomplishment and reinforces positive behaviors.
- Clear and Open Communication: I maintain clear and open communication with families, explaining therapy goals and progress in a way that is easy to understand. Regular updates and opportunities for questions keep everyone informed and involved.
- Cultural Sensitivity: I am mindful of cultural differences and tailor my approach to respect individual beliefs and practices. This might involve adapting communication styles or using culturally relevant materials.
- Building Personal Connections: I make an effort to connect with clients and their families on a personal level, within professional boundaries. Sharing relevant experiences (while maintaining confidentiality) can help build a sense of trust and understanding.
For example, I once worked with a young child who was initially hesitant to participate in therapy. By playing games that he enjoyed and consistently praising his efforts, I gradually built his trust and confidence, leading to significant progress.
Q 24. Describe a time you had to adapt your approach based on a client’s needs.
I once worked with a teenager who had selective mutism, a condition where they chose not to speak in certain situations. The structured approaches that worked well with other clients were ineffective. I realized I needed to adapt my strategies to respect his comfort levels while still encouraging communication.
Instead of direct verbal interaction, I started by using visual aids, written prompts, and interactive technology. We focused on building his confidence gradually. We started with simple tasks involving pointing or nodding. Then, we moved to writing short messages and finally progressed to more verbal interaction. This personalized, gradual approach, focused on his comfort and progress, eventually led to significant improvements in his communication skills. This experience highlighted the importance of flexibility and individualized therapeutic strategies in speech therapy.
Q 25. How do you provide feedback to clients in a constructive and supportive way?
Providing constructive and supportive feedback is crucial for client progress and motivation. I focus on being specific, positive, and encouraging.
- Specific and Observable Behaviors: I describe specific behaviors and avoid vague generalizations. For instance, instead of saying “You did well,” I might say, “I noticed you used your ‘s’ sound correctly five times during our session today.”
- Positive and Encouraging Language: I emphasize strengths and celebrate achievements. I focus on progress made, not just areas needing improvement.
- Goal-Oriented Feedback: I connect feedback directly to the client’s goals and show how their efforts are contributing to progress. This helps them understand the purpose of their work and increases motivation.
- Collaborative Approach: I encourage clients to participate in the feedback process and share their own observations. This fosters a sense of ownership and involvement.
- Constructive Suggestions: I offer specific suggestions for improvement, focusing on strategies rather than criticizing the client’s efforts. For example, “Let’s try practicing this word in a sentence next time to help you remember it better.”
By providing feedback in this way, I aim to empower clients, increase their self-efficacy, and encourage continued effort toward their communication goals.
Q 26. Explain your understanding of the ethical considerations involved in speech therapy.
Ethical considerations in speech therapy are paramount. My practice is guided by principles of beneficence (acting in the best interest of the client), non-maleficence (avoiding harm), autonomy (respecting client choices), justice (fair and equitable treatment), and fidelity (maintaining trust and loyalty).
- Confidentiality: Maintaining client confidentiality is paramount. I only share information with authorized individuals and follow all HIPAA regulations.
- Informed Consent: I ensure clients and their families understand the nature of the therapy, its potential benefits and risks, and their right to refuse treatment.
- Competence: I only perform tasks within my scope of practice and under the supervision of a licensed SLP. I recognize my limitations and seek guidance when needed.
- Cultural Competence: I am aware of and sensitive to cultural differences and ensure that my practice is culturally appropriate and respectful.
- Professional Boundaries: I maintain appropriate professional boundaries with clients and their families to prevent conflicts of interest and maintain trust.
Ethical dilemmas might arise, and it’s vital to seek guidance from the supervising SLP and adhere to professional codes of ethics to ensure the best outcome for the client.
Q 27. How do you maintain professional boundaries with clients?
Maintaining professional boundaries is essential for ethical practice and client well-being. This means establishing and respecting clear limits in the therapist-client relationship.
- Professional Role: I consistently maintain my role as a therapist, avoiding familiarity or personal relationships.
- Confidentiality: I never disclose client information outside of the therapeutic context and adhere strictly to confidentiality guidelines.
- Appropriate Communication: I limit communication to therapy-related topics and avoid casual or social interaction outside of therapy sessions.
- Physical Space and Contact: I maintain appropriate physical distance and avoid unnecessary physical contact. All physical contact is therapeutic and documented.
- Gift Giving: I politely decline gifts from clients and their families to avoid compromising the professional relationship.
- Social Media: I do not connect with clients on social media.
By adhering to these boundaries, I ensure a safe and effective therapeutic environment for clients.
Q 28. Describe your problem-solving skills in a clinical setting.
Problem-solving is a daily part of my work as an SLPA. I utilize a structured approach:
- Identify the Problem: First, I clearly define the problem. For example, a client might be struggling with a specific articulation sound or demonstrating difficulty with a particular language skill.
- Gather Information: I gather relevant data. This may include reviewing client files, discussing concerns with the SLP, and observing the client’s performance in various settings.
- Generate Solutions: I brainstorm several potential solutions. This might involve adapting existing therapy materials, modifying therapy techniques, or implementing new strategies.
- Evaluate Solutions: I consider the feasibility, effectiveness, and ethical implications of each potential solution.
- Implement and Monitor: I implement the chosen solution and closely monitor its effectiveness. I keep detailed records and discuss progress with the supervising SLP.
- Adjust as Needed: I’m prepared to adapt or modify the solution if it proves ineffective. The therapeutic process is iterative and requires flexibility.
For instance, if a client was struggling with a particular articulation exercise, I might try different approaches such as using visual aids, incorporating more interactive games, or adjusting the intensity and frequency of the exercise. Regular monitoring and communication with the SLP ensures we consistently adapt the therapy plan to best suit the client’s needs.
Key Topics to Learn for Speech and Language Therapy Assistance Interview
- Understanding Communication Disorders: Develop a strong grasp of various speech and language disorders affecting children and adults, including articulation disorders, fluency disorders, language disorders, and social communication disorders. Consider the developmental aspects of these disorders.
- Therapeutic Techniques and Activities: Familiarize yourself with common therapeutic approaches used by Speech-Language Pathologists (SLPs). This includes understanding the practical application of activities and strategies to support communication development and remediation. Think about how you would adapt techniques based on individual client needs.
- Client Interaction and Support: Practice explaining therapeutic goals and progress to clients and their families in a clear and compassionate manner. Prepare to discuss your approach to building rapport and fostering a positive therapeutic environment.
- Data Collection and Documentation: Understand the importance of accurate and thorough documentation of client sessions, including progress notes, data tracking, and reporting to the SLP. Consider the ethical implications of maintaining accurate records.
- Collaboration and Teamwork: Discuss your experience working collaboratively within a multidisciplinary team. Highlight your ability to contribute effectively and communicate clearly with SLPs, other therapists, and caregivers.
- Professionalism and Ethics: Review ethical guidelines for healthcare professionals and demonstrate your understanding of maintaining client confidentiality and professional boundaries.
- Assistive Technology and Adaptive Strategies: Familiarize yourself with various assistive technologies and adaptive strategies used to support communication, such as augmentative and alternative communication (AAC) systems. Be prepared to discuss their application.
Next Steps
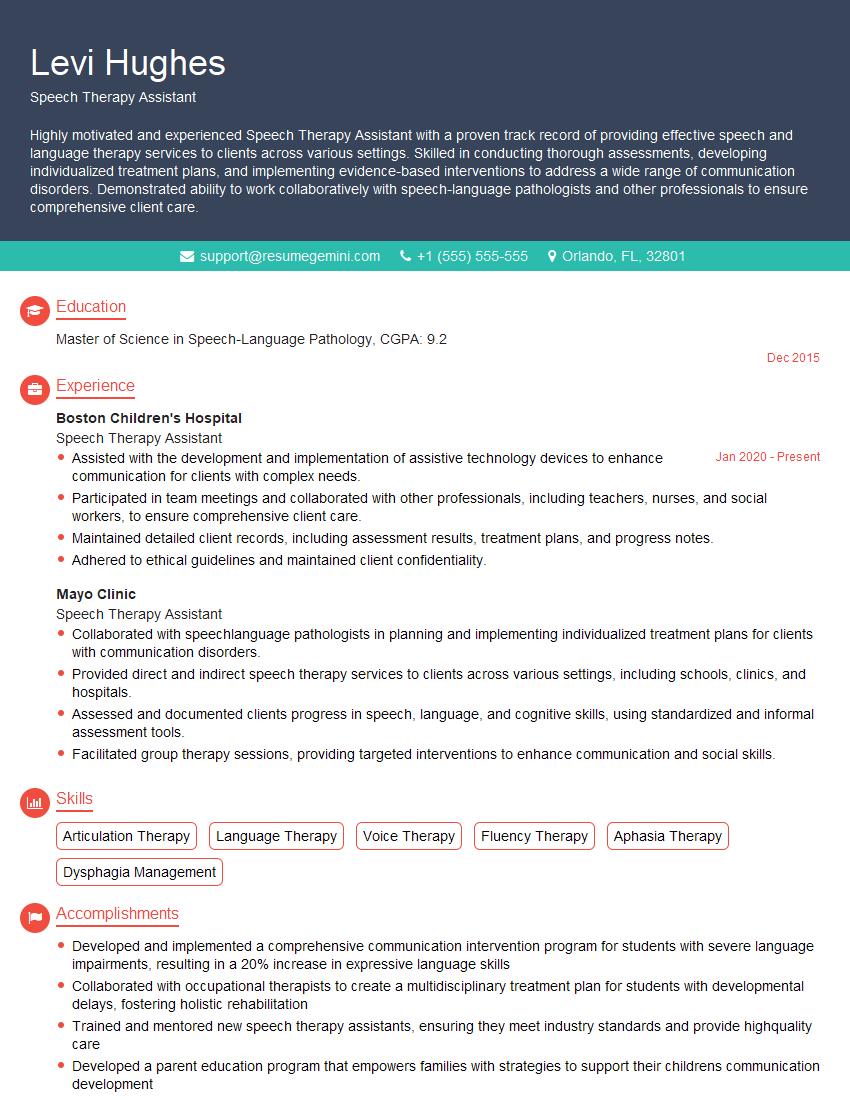
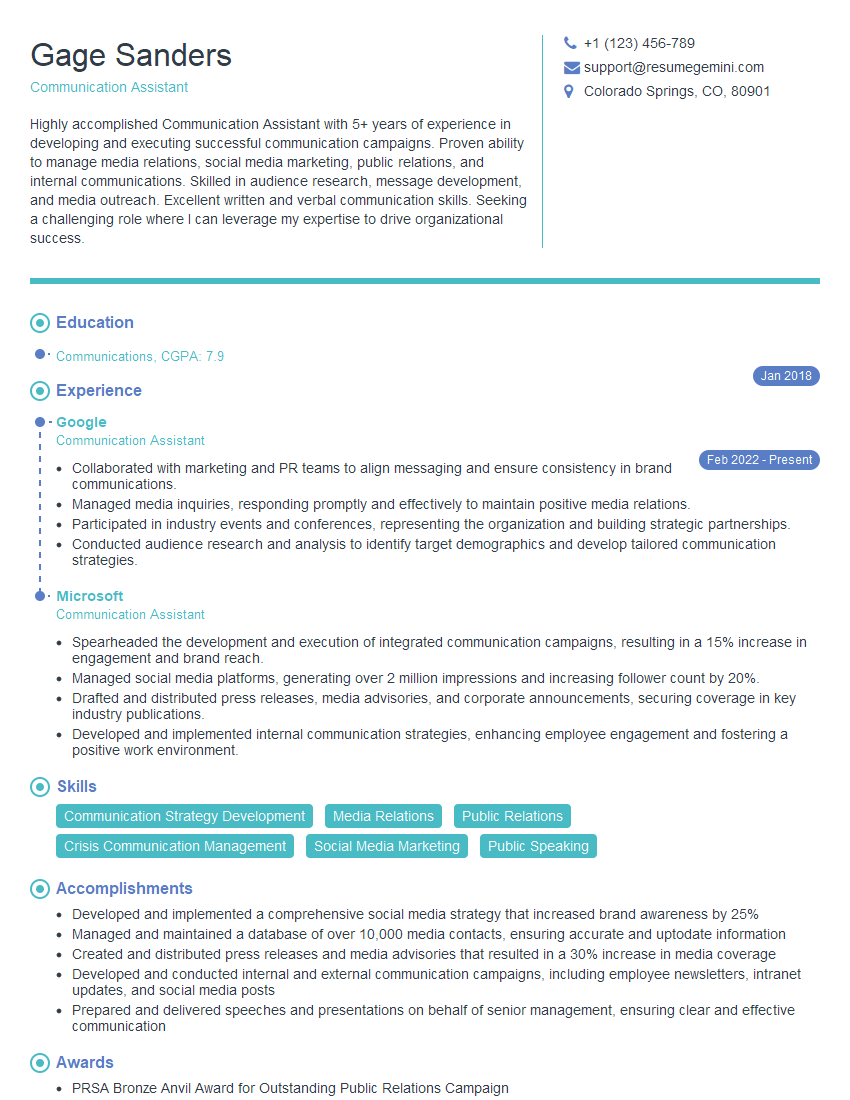
Mastering the fundamentals of Speech and Language Therapy Assistance is crucial for building a successful and rewarding career. Your skills are highly valued in providing essential support to clients and Speech-Language Pathologists. A strong resume is your key to unlocking exciting opportunities. Creating an ATS-friendly resume will significantly increase your chances of getting your application noticed. ResumeGemini is a trusted resource to help you build a professional and impactful resume. We provide examples of resumes tailored to Speech and Language Therapy Assistance to help you get started. Invest in crafting a resume that showcases your skills and experience effectively – it’s your first impression on potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO