Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Severe Behavior Disorders interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Severe Behavior Disorders Interview
Q 1. Describe the difference between positive and negative reinforcement.
Reinforcement, in behavioral terms, refers to anything that increases the likelihood of a behavior recurring. The key difference lies in what is added or removed.
Positive reinforcement involves adding something desirable to increase a behavior. Think of it like giving a dog a treat for sitting – the treat (something added) increases the likelihood of the dog sitting again. In working with individuals with severe behavior disorders, this could involve providing praise, access to preferred activities, or even a small edible reward for demonstrating a desired behavior like remaining calm during a stressful situation.
Negative reinforcement, conversely, involves removing something undesirable to increase a behavior. This isn’t punishment; it’s about removing something aversive. Imagine a child who whines until their parents give them candy to stop the whining. The removal of the whining (something undesirable) reinforces the whining behavior because it leads to a desired outcome. In a therapeutic setting, this might mean removing a demand or task when an individual exhibits self-injurious behavior, although this should be used cautiously and in conjunction with other strategies.
The crucial distinction is that both increase the probability of a behavior, but one does it through addition (positive) and the other through subtraction (negative). It’s vital to carefully consider the ethical and practical implications of each, as inappropriate use of negative reinforcement can be problematic.
Q 2. Explain the concept of functional behavioral assessment (FBA).
Functional Behavioral Assessment (FBA) is a systematic process used to understand why a challenging behavior is occurring. It’s not just about identifying the behavior itself but uncovering the function or purpose the behavior serves for the individual. Think of it as detective work – we’re trying to find the ‘case file’ on the behavior.
An FBA involves several steps:
- Identifying the behavior: Clearly define the specific behavior using observable and measurable terms (e.g., ‘hitting others’ rather than ‘acting out’).
- Collecting data: This involves observing the individual’s behavior across various settings and situations, noting the antecedents (what happens before the behavior), the behavior itself, and the consequences (what happens after the behavior). Direct observation, interviews with caregivers, and reviewing existing records are common data-gathering methods.
- Analyzing the data: This step involves identifying patterns in the data to determine the function of the behavior. For example, does the behavior lead to getting attention, escaping a task, accessing a preferred item, or self-regulation?
- Developing hypotheses: Based on the data analysis, hypotheses about the function of the behavior are formulated. For instance, a hypothesis might be: ‘The student hits others to escape a demanding task.’
- Developing interventions: Once the function of the behavior is understood, interventions can be developed to address the underlying need and replace the challenging behavior with more appropriate skills.
For instance, an FBA might reveal that a student’s screaming is a way to escape disliked academic tasks. Understanding this allows us to create a plan to teach coping mechanisms for frustration and make academic tasks more engaging. FBAs are crucial for creating effective and ethical behavior intervention plans.
Q 3. What are the key components of a behavior intervention plan (BIP)?
A Behavior Intervention Plan (BIP) is a document that outlines strategies to address challenging behaviors identified through an FBA. It’s essentially a roadmap for changing behavior.
Key components include:
- Operational definition of the target behavior: A clear and concise description of the behavior to be addressed. This must be measurable and observable.
- Antecedent interventions: Strategies to prevent the behavior from occurring in the first place (e.g., environmental modifications, proactive teaching).
- Replacement behaviors: Teaching the individual alternative, appropriate behaviors to meet the same need as the problem behavior. For example, teaching a child to ask for a break instead of hitting when frustrated.
- Consequence interventions: Strategies to manage the behavior when it does occur (e.g., reinforcement, ignoring, time-out, etc.). These need to be aligned with ethical considerations and should prioritize positive reinforcement whenever possible.
- Data collection methods: A plan for monitoring the effectiveness of the interventions through systematic data collection. This data helps determine if the BIP is working and allows for adjustments as needed.
- Review and revision schedule: The BIP should be regularly reviewed (e.g., monthly) to evaluate its effectiveness and make adjustments based on the collected data. This ensures ongoing support and adapts to the individual’s needs.
A well-designed BIP is data-driven, individualized, and focused on teaching appropriate replacement behaviors rather than solely punishing challenging behaviors.
Q 4. How do you differentiate between challenging behavior and developmental delays?
Differentiating between challenging behavior and developmental delays requires careful observation and assessment. While they can sometimes co-occur, they represent distinct concepts.
Challenging behavior refers to actions that are disruptive, dangerous, or interfere with learning or social interactions. It often serves a purpose for the individual, even if that purpose is not immediately apparent. Examples include aggression, self-injurious behavior, property destruction, and non-compliance.
Developmental delays, on the other hand, refer to lags in the acquisition of typical developmental milestones in areas such as communication, social skills, motor skills, or cognitive abilities. These delays may increase the likelihood of challenging behaviors, but the delays themselves are not the behaviors. Examples include delayed speech development, difficulty with fine motor skills, or challenges with social reciprocity.
A crucial distinction lies in the function of the behavior. Challenging behavior serves a purpose (to escape, gain attention, sensory input, etc.), whereas developmental delays are limitations in skill development. A comprehensive assessment, involving various professionals like psychologists, educators, and therapists, is necessary to accurately differentiate and develop appropriate interventions.
For example, a child with autism may exhibit aggression (challenging behavior) because they have difficulty communicating their needs (developmental delay). The intervention would therefore address both – teaching communication skills while simultaneously working on managing the aggression.
Q 5. What are some common antecedent interventions used to prevent problem behaviors?
Antecedent interventions focus on preventing problem behaviors before they occur. They aim to modify the environment or the individual’s state to reduce the likelihood of a challenging behavior.
Common strategies include:
- Environmental modifications: Changing the physical environment to minimize triggers. For example, rearranging a classroom to provide a quieter space for a student easily overwhelmed by noise.
- Structured schedules/visual supports: Providing clear visual schedules or routines to reduce anxiety and uncertainty. This can be particularly helpful for individuals with autism spectrum disorder.
- Proactive teaching: Teaching the individual skills needed to manage challenging situations. This could involve teaching communication skills, self-regulation techniques, or problem-solving strategies.
- Functional communication training (FCT): Teaching alternative ways for the individual to communicate their needs effectively. This could involve teaching sign language, using a communication board, or using picture exchange systems (PECS).
- Premack principle: Offering a preferred activity (high probability behavior) following the completion of a less preferred activity (low probability behavior). For example, allowing a child to play video games after completing their homework.
- Positive reinforcement of appropriate behaviors: Consistently rewarding and praising desired behaviors to strengthen them and make them more likely to occur.
For example, a child who frequently throws toys during transitions might benefit from a clear visual schedule showing the upcoming activities and receiving verbal reminders and praise for staying calm and following directions during transitions.
Q 6. Describe your experience with crisis de-escalation techniques.
Crisis de-escalation techniques are crucial for managing potentially dangerous situations. My experience involves a range of approaches, always prioritizing safety and de-escalation over control.
My approach emphasizes understanding the individual’s emotional state and triggers. I employ strategies like:
- Maintaining a calm and non-threatening demeanor: Speaking softly, using non-judgmental language, and maintaining a safe distance.
- Active listening and empathy: Attempting to understand the individual’s perspective and communicating that understanding.
- Providing clear and concise instructions: Giving simple, direct instructions, avoiding complex or confusing language.
- Offering choices: When appropriate, offering the individual choices to maintain a sense of control.
- Environmental modifications: Removing potential triggers or moving to a less stimulating environment.
- Physical interventions (only as a last resort): Only using physical interventions when necessary to ensure the safety of the individual and others, utilizing safe and appropriate restraint techniques trained and implemented as per established protocols.
I’ve found that building a trusting relationship with individuals is key to effective de-escalation. It allows for more effective communication and reduces the likelihood of crises. I’ve personally used these techniques numerous times successfully. One instance involved a young man in a high-stress residential setting who had displayed escalating physical aggression. By reducing environmental stimulation, utilizing calm communication, and offering simple choices, I managed to de-escalate the situation peacefully without physical intervention.
Q 7. How do you communicate effectively with individuals exhibiting severe behavior challenges?
Effective communication with individuals exhibiting severe behavior challenges requires patience, understanding, and a multi-faceted approach.
Key strategies I employ include:
- Using clear and concise language: Avoiding jargon, slang, or complex sentences. Speak simply and directly.
- Non-verbal communication: Paying close attention to body language and using calming gestures. Maintaining eye contact (when appropriate for the individual) can demonstrate engagement but must be balanced with sensitivity to potential triggers.
- Active listening: Paying close attention to what the individual is saying (verbally or non-verbally), reflecting back their feelings and concerns to show that you understand.
- Using visual supports: Pictures, symbols, or written words can aid understanding, particularly for individuals with communication difficulties.
- Collaborating with caregivers and other professionals: Working as part of a team to ensure consistent communication and intervention strategies.
- Positive reinforcement: Acknowledging and rewarding positive behaviors and attempts at communication.
- Patience and understanding: Remembering that challenging behaviors often stem from underlying needs or difficulties.
For example, I might use a communication board with pictures to allow a non-verbal individual to communicate their wants and needs, reducing frustration and avoiding potential behavioral outbursts. The approach is always tailored to the specific individual’s needs and communication style.
Q 8. Explain your understanding of differential reinforcement.
Differential reinforcement is a behavior modification technique where we reinforce desired behaviors while withholding reinforcement for undesired behaviors. It’s not about punishment; instead, it focuses on increasing the frequency of positive behaviors. Imagine it like this: you’re teaching a dog to sit. Every time the dog sits, you give it a treat (reinforcing the ‘sit’ behavior). You ignore the dog when it jumps up (withholding reinforcement for the undesired behavior). There are several types of differential reinforcement:
- Differential Reinforcement of Incompatible Behavior (DRI): Reinforcing a behavior that cannot occur simultaneously with the undesired behavior. For example, reinforcing a child sitting quietly (incompatible with running around) at their desk.
- Differential Reinforcement of Alternative Behavior (DRA): Reinforcing a behavior that is an alternative to the undesired behavior. For instance, if a child screams for attention, DRA might involve rewarding the child for asking politely for assistance instead.
- Differential Reinforcement of Other Behavior (DRO): Reinforcing the absence of the undesired behavior for a specified period. If a child hits others, DRO involves rewarding them for not hitting for a set time, even if they don’t exhibit any other specific behavior.
- Differential Reinforcement of Low Rates of Behavior (DRL): Reinforcing the undesired behavior when it occurs at a lower frequency than usual. This is used for behaviors that are not entirely undesirable, but need to be reduced, such as talking out of turn in class.
In practice, differential reinforcement requires careful observation, data collection, and consistent application. The key is to identify the function of the behavior – what is the individual gaining from the undesired behavior? Once we understand this, we can choose the most appropriate type of differential reinforcement and design a reinforcement system tailored to the individual’s needs and preferences.
Q 9. What are the ethical considerations when working with individuals with severe behavior disorders?
Ethical considerations in working with individuals with severe behavior disorders are paramount. Our primary obligation is to ensure the safety and well-being of the individual. This includes:
- Informed Consent: Obtaining informed consent from the individual (or their legal guardian) about all aspects of the intervention plan, including risks and benefits. This means ensuring they understand the procedures in a way they can comprehend.
- Least Restrictive Interventions: Prioritizing the least restrictive intervention that is effective. More intrusive interventions should only be considered when less intrusive ones have failed. This might involve trying positive reinforcement strategies before resorting to more restrictive techniques.
- Competence and Supervision: Ensuring that all professionals involved are adequately trained and supervised, with ongoing professional development to maintain competency in the latest ethical and evidence-based practices.
- Confidentiality and Privacy: Maintaining strict confidentiality and respecting the individual’s right to privacy, adhering to all relevant laws and regulations.
- Avoiding Coercion or Punishment: While some behavior management techniques might involve consequences, these should never be punitive or coercive. The focus should be on teaching replacement behaviors and promoting positive interactions.
- Cultural Sensitivity: Being mindful of the individual’s cultural background, beliefs, and values and adapting interventions accordingly to ensure cultural sensitivity.
- Ongoing Evaluation and Monitoring: Regularly reviewing the effectiveness of interventions and making adjustments as needed, always ensuring client progress is the priority.
Ethical dilemmas can arise frequently. For example, deciding whether to use a restrictive procedure even if it’s the most effective option requires careful ethical deliberation, often involving a multidisciplinary team and consultation with ethical review boards.
Q 10. How do you maintain accurate data collection and analysis for behavior programs?
Accurate data collection and analysis are the bedrock of effective behavior programs. We use various methods, often combining several to obtain a comprehensive picture of behavior.
- Direct Observation: This involves systematically observing and recording the target behavior. We might use various recording methods, such as frequency counts (how many times the behavior occurs), duration recording (how long the behavior lasts), latency recording (the time between a cue and the behavior), or interval recording (recording whether the behavior occurs within specific time intervals). Data is typically recorded on a data sheet or using dedicated behavior tracking software.
- ABC Data Collection: This method records the Antecedent (what happened before the behavior), Behavior (the target behavior itself), and Consequence (what happened after the behavior). This helps to identify patterns and potential triggers.
- Data Analysis: Once data is collected, we analyze it graphically (using line graphs, scatter plots, etc.) to identify trends, patterns, and the effectiveness of interventions. We might use statistical methods (e.g., to determine statistical significance of changes). We’ll also look at the rate of behavior change, variability in the data, and the overall improvement in the individual’s daily life.
Maintaining accuracy requires meticulous attention to detail, inter-rater reliability checks (multiple observers independently recording data to ensure consistency), and regular reviews of the data collection procedures. The data informs treatment decisions, ensuring that we’re making data-driven adjustments to maximize effectiveness and client progress.
Q 11. Describe your experience with shaping and chaining behaviors.
Shaping and chaining are fundamental behavior modification techniques. Shaping involves reinforcing successive approximations of a target behavior. Imagine teaching a child to write their name. We don’t expect perfect handwriting initially. Instead, we might reinforce them for making any attempt, then for forming recognizable letters, and gradually shaping the behavior toward writing their name neatly and legibly. Chaining involves breaking down a complex behavior into smaller, manageable steps (links in the chain) and teaching each step sequentially until the entire sequence is learned. For instance, teaching someone to make a sandwich involves chaining together steps like getting the bread, spreading the butter, adding fillings, and wrapping the sandwich.
Example of Shaping: A child with autism is learning to make eye contact. Initially, any glance in the general direction of the therapist’s face is reinforced. Then, only direct eye contact for a fraction of a second is reinforced. The duration of eye contact gradually increases until the desired behavior (maintaining eye contact for several seconds) is achieved.
Example of Chaining: Teaching a person with intellectual disabilities to brush their teeth. Each step – picking up the toothbrush, adding toothpaste, brushing each section of the teeth, rinsing, etc. – is taught independently, and then combined sequentially. Backward chaining – starting with the last step and working backward – is often more effective in teaching complex tasks.
In practice, shaping and chaining often work best in conjunction with other techniques, such as differential reinforcement, to encourage the desired behaviors.
Q 12. How do you adapt interventions based on data analysis and client progress?
Data analysis is the compass guiding our interventions. We constantly monitor client progress through regular data review meetings. If the data show that an intervention isn’t effective, we need to adapt. This might involve:
- Modifying the intervention: Changing the reinforcers used, adjusting the schedule of reinforcement, or altering the criteria for reinforcement.
- Changing the target behavior: If the chosen target behavior isn’t producing the desired results, it might be necessary to re-evaluate the problem behavior and select a different, more impactful target. This would require reassessing the functional analysis.
- Adding new interventions: Combining the current intervention with other techniques (e.g., adding social skills training alongside a behavior modification program).
- Consulting with colleagues: Seeking feedback and expertise from other professionals to gain fresh perspectives and develop new strategies.
- Re-evaluating the functional assessment: If the data suggest a change in the function of the behavior, a thorough reassessment of the underlying reasons for the behavior is crucial to inform adjustments to the intervention plan.
Regular progress reviews with the client and their family are essential for understanding their perspective and maintaining collaboration. Adaptability is vital; we must be prepared to adjust our approach based on the unique needs and response of each individual.
Q 13. Explain your familiarity with various assessment tools used in severe behavior disorders.
Assessment tools for severe behavior disorders are diverse and selected based on the individual’s needs and the goals of the assessment. Some common tools include:
- Functional Behavior Assessments (FBAs): These are crucial for understanding the function of a behavior (what purpose it serves for the individual). FBAs involve direct observation, interviews with caregivers, and analysis of antecedent-behavior-consequence patterns. Different methods exist within FBAs such as descriptive assessments, indirect assessments, and functional analysis.
- Developmental Scales: Tools like the Vineland Adaptive Behavior Scales assess adaptive functioning in areas like communication, daily living skills, and socialization. They help understand developmental delays.
- Behavioral Rating Scales: These are questionnaires completed by caregivers or teachers to assess the frequency and severity of specific behaviors. Examples include the Child Behavior Checklist (CBCL) and the Aberrant Behavior Checklist (ABC).
- Cognitive Assessments: These tools evaluate cognitive abilities, such as intelligence, attention, and memory, which can inform intervention strategies. Examples are the Wechsler Intelligence Scale for Children (WISC) and the Stanford-Binet Intelligence Scales.
- Adaptive Behavior Scales: These measure adaptive skills necessary for daily living and social interaction. The Vineland Adaptive Behavior Scales and the Adaptive Behavior Assessment System (ABAS) are commonly used.
The selection and interpretation of assessment tools require specialized training and expertise. The results guide the development of individualized intervention plans tailored to the specific needs of the individual.
Q 14. Describe your experience with working with diverse populations.
Experience working with diverse populations is essential in this field. It’s crucial to understand and appreciate the varied cultural, linguistic, and socioeconomic backgrounds of the individuals we serve. This necessitates cultural sensitivity and humility, understanding that what might be considered acceptable behavior in one culture may not be in another. I’ve worked with individuals from a range of ethnic and racial backgrounds, various socioeconomic strata, and different linguistic capabilities. This has involved adapting interventions and assessment strategies, including:
- Using interpreters or translators: Ensuring effective communication when language barriers exist.
- Incorporating culturally relevant materials and methods: Tailoring interventions to resonate with the individual’s cultural values and beliefs.
- Collaborating with family members and community resources: Building partnerships to create a supportive and culturally competent treatment environment.
- Utilizing culturally sensitive assessment tools: Selecting or adapting tools to minimize cultural bias and ensure valid and reliable assessments.
- Educating myself continually: Staying informed about cultural nuances and best practices in working with diverse populations.
Understanding these differences allows me to provide more effective and culturally sensitive care, building trust and strong therapeutic relationships with individuals and their families.
Q 15. How do you collaborate with families and interdisciplinary teams?
Collaboration is the cornerstone of effective intervention for severe behavior disorders. I believe in a truly collaborative approach, involving families as active partners and working seamlessly with interdisciplinary teams. With families, I prioritize open communication, active listening, and shared decision-making. This includes regular meetings, providing clear explanations of the child’s behavior and treatment plan, and actively seeking their input and perspectives. I utilize methods like family-based interventions, teaching parents strategies they can use at home to reinforce positive behaviors and manage challenging behaviors consistently. With interdisciplinary teams – including psychiatrists, psychologists, occupational therapists, educators, and social workers – I facilitate regular case conferences, ensuring clear communication and coordinated efforts. We share information, discuss progress, address challenges collaboratively, and collectively adjust the treatment plan as needed. For example, in a recent case involving a child with autism and severe aggression, collaboration with the school psychologist led to the implementation of a sensory-regulation strategy in the classroom, significantly reducing the frequency of outbursts.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is your approach to managing aggression and self-injurious behaviors?
Managing aggression and self-injurious behaviors (SIB) requires a multi-faceted approach rooted in safety, understanding the function of the behavior, and implementing evidence-based interventions. Safety is paramount; we use de-escalation techniques and, when necessary, physical interventions trained to safety protocols, ensuring minimal restriction and prioritizing the client’s well-being. Functional behavior assessments (FBAs) are crucial in determining the ‘why’ behind the behavior – what triggers it, what the child gains from it (attention, escape, sensory stimulation). Once the function is identified, we develop behavior support plans (BSPs) using principles of applied behavior analysis (ABA). These plans focus on teaching replacement behaviors (adaptive ways to meet the same need) and providing positive reinforcement for desired behaviors. For instance, if SIB is used to escape a task, the BSP might involve teaching the child a calm-down strategy and gradually increasing task demands while providing frequent positive reinforcement. We also involve all stakeholders—family, school staff, etc.—to ensure consistent implementation across settings. Data collection is essential for tracking progress and making adjustments to the BSP. This is an iterative process, regularly reviewed and refined based on ongoing assessment.
Q 17. Explain your understanding of the principles of applied behavior analysis (ABA).
Applied Behavior Analysis (ABA) is a scientific approach to understanding and changing behavior. It’s based on the principles of learning theory, focusing on observable behaviors and their environmental determinants. The core principles include:
- Reinforcement: Increasing the likelihood of a behavior by providing a consequence the individual finds rewarding (positive reinforcement, e.g., praise; negative reinforcement, e.g., removing a demand).
- Punishment: Decreasing the likelihood of a behavior by introducing an aversive consequence (positive punishment, e.g., reprimand; negative punishment, e.g., removal of privileges). Ethical considerations dictate that punishment is used sparingly and only when absolutely necessary, and never involving physical harm.
- Extinction: Gradually decreasing the likelihood of a behavior by withholding reinforcement that previously maintained it.
- Shaping: Reinforcing successive approximations of a desired behavior until the target behavior is achieved.
- Generalization: Ensuring that learned behaviors are performed across different settings and situations.
ABA is not about punishment; it’s about identifying what motivates behavior and then using those motivations to guide positive changes. It’s data-driven, relying on objective measurement to track progress and make adjustments to the intervention plan. For example, using a reward chart system to reinforce appropriate classroom behavior is a simple application of ABA.
Q 18. How do you ensure the safety and wellbeing of clients and staff?
Ensuring safety and well-being is paramount. This starts with thorough risk assessments for both clients and staff. For clients, we identify potential triggers for challenging behaviors and develop safety plans addressing potential risks like self-harm or aggression towards others. This includes physical environment modifications (e.g., removing potentially harmful objects) and staff training on de-escalation techniques. For staff, this involves providing comprehensive training on behavior management strategies, de-escalation techniques, crisis intervention, and physical intervention (when necessary and ethically appropriate), always prioritizing safety and minimizing restraint. Regular staff meetings provide a platform to discuss safety concerns, review incidents, and ensure consistent implementation of safety procedures. We also conduct regular environmental safety audits to identify and mitigate hazards. Finally, we ensure access to appropriate supervision and support for staff, promoting their well-being and reducing burnout.
Q 19. What are your strategies for dealing with challenging behavior in different settings?
Managing challenging behaviors varies depending on the setting. In school, collaboration with teachers and educators is key to implementing consistent strategies. For example, modifying the classroom environment to reduce sensory overload, utilizing visual supports, and providing structured routines can be highly effective. At home, involving parents in the development and consistent implementation of the behavior plan is vital, using strategies that work within the family structure. In community settings, adapting interventions to suit the environment while ensuring consistent application of techniques is crucial. For instance, in a community park, alternative activities might be used to redirect a challenging behavior. In all settings, using positive reinforcement, functional communication training, and proactive strategies to prevent challenging behaviors are prioritized. Flexibility is key—adapting approaches based on the context while adhering to the core principles of the behavior plan.
Q 20. Describe your experience with developing and implementing individualized behavior plans.
Developing and implementing individualized behavior plans is a core component of my practice. This starts with a thorough functional behavior assessment (FBA) involving direct observation, interviews with caregivers, and data collection to identify the triggers, function, and consequences of the challenging behavior. Based on the FBA results, I collaborate with the family and team to develop a behavior support plan (BSP) that outlines specific goals, interventions, and data collection methods. The BSP is individualized, considering the client’s age, developmental level, strengths, and preferences. For example, a BSP for a child with autism might include visual schedules, social skills training, and reinforcement strategies. I use a variety of techniques such as positive reinforcement, antecedent interventions (modifying the environment to prevent triggering events), and teaching replacement behaviors. The BSP is not static; it’s regularly reviewed and updated based on data collected and progress monitoring. I maintain detailed documentation of the plan, its implementation, and the client’s progress, ensuring transparency and accountability.
Q 21. How do you handle situations where client progress plateaus or regresses?
When client progress plateaus or regresses, it necessitates a thorough re-evaluation of the behavior support plan. This involves reviewing the data, examining the consistency of implementation, considering potential environmental changes (e.g., stress at home or school), and exploring whether the intervention strategies are still appropriate. It may require re-assessing the function of the behavior to ensure the interventions continue to address the underlying needs. For example, a plateau might indicate a need to increase the intensity or frequency of reinforcement, or to modify the intervention based on new information gained. Regression often points to unforeseen stressors, or requires a revisiting of antecedent strategies to prevent triggers. This might involve adjusting the environment, introducing new teaching strategies, and increasing collaboration with other professionals or family members. This is an opportunity to further refine the plan, ensuring it remains effective and responsive to the client’s changing needs. Flexibility, continuous monitoring, and collaborative problem-solving are essential in handling these situations.
Q 22. Describe your understanding of evidence-based practices in severe behavior disorders.
Evidence-based practices (EBPs) in severe behavior disorders are interventions and strategies supported by rigorous scientific research demonstrating their effectiveness in reducing challenging behaviors and improving outcomes. They aren’t simply ‘best guesses’ but methods proven to work through controlled studies. This means interventions aren’t implemented randomly; they are selected based on the individual’s specific needs and the available data on what works best for similar cases.
- Functional Behavior Assessment (FBA): This is the cornerstone of EBP. An FBA systematically investigates the function (the reason) behind a behavior. Why is the individual engaging in this behavior? Is it to get attention, escape a task, access something desired, or due to sensory issues? Understanding the function allows for targeted interventions.
- Positive Behavior Support (PBS): PBS focuses on teaching and reinforcing positive behaviors while minimizing reliance on punishment. It involves proactive strategies like teaching alternative behaviors, providing choices, and creating a supportive environment. It’s about teaching *what to do* instead of just focusing on stopping *what not to do*.
- Applied Behavior Analysis (ABA): ABA uses principles of learning to modify behaviors. This involves careful observation, data collection, and systematic intervention to change behavior. Techniques like positive reinforcement (rewarding desired behaviors) and extinction (removing reinforcement for undesirable behaviors) are common elements of ABA.
- Cognitive Behavioral Therapy (CBT): CBT helps individuals understand the thoughts and feelings that contribute to their behavior. By identifying and changing negative thought patterns, CBT aims to improve self-regulation and reduce challenging behaviors.
For example, a child engaging in aggression might have an FBA revealing it’s to escape a demanding task. A PBS approach would teach the child coping strategies for frustration and provide breaks. ABA could involve reinforcing calm behavior during tasks, and CBT might address the child’s negative self-talk about the task.
Q 23. What are some common misconceptions about severe behavior disorders?
Many misconceptions surround severe behavior disorders. It’s crucial to address these to promote understanding and effective support:
- Misconception 1: It’s all about ‘bad’ behavior and lack of discipline. Reality: Challenging behaviors are often communication attempts or responses to underlying needs or disabilities. Lack of discipline isn’t the root cause; it’s often a symptom of something else.
- Misconception 2: People with severe behavior disorders are inherently dangerous or violent. Reality: While some individuals may exhibit aggressive behaviors, this isn’t representative of the entire group. Most individuals with severe behavior disorders are not violent and respond well to appropriate support.
- Misconception 3: There’s a quick fix or a single solution. Reality: Effective intervention requires comprehensive, individualized plans and often involves a multi-disciplinary team approach. There’s no one-size-fits-all solution.
- Misconception 4: It’s solely the responsibility of the family or caregivers. Reality: Effective support requires collaboration between families, educators, healthcare professionals, and community agencies. Shared responsibility and resources are essential.
Consider the example of a child with autism exhibiting self-injurious behavior. It’s not a matter of poor parenting; it might stem from sensory sensitivities or communication difficulties. A multidisciplinary team including therapists, educators, and the family needs to collaborate for effective support.
Q 24. How do you ensure confidentiality and comply with relevant regulations?
Confidentiality and compliance with regulations are paramount. I adhere strictly to HIPAA (Health Insurance Portability and Accountability Act) and FERPA (Family Educational Rights and Privacy Act) guidelines, as well as any state-specific regulations. This means:
- Only authorized individuals have access to client information: Information is shared only with those directly involved in the individual’s care and with their informed consent.
- Data security measures are employed: Client records are stored securely, both electronically and physically, using appropriate passwords and access controls.
- Informed consent is obtained: Before any interventions or assessments are carried out, informed consent is obtained from the individual or their legal guardian.
- Strict adherence to reporting procedures: Mandatory reporting requirements, such as reporting suspected abuse or neglect, are followed diligently.
- Maintaining accurate and up-to-date records: Client files are meticulously maintained to reflect the interventions, progress, and any significant events.
For example, I would never discuss a client’s case with an unauthorized person, even a family member not directly involved in care. All communications would be conducted in a secure manner, and consent would be obtained before sharing any information.
Q 25. What are the legal and ethical considerations regarding restraint and seclusion?
Restraint and seclusion are serious interventions with significant legal and ethical implications. Their use should always be a last resort, and only when all other less restrictive methods have failed to ensure the safety of the individual or others.
- Legal Considerations: Laws regarding restraint and seclusion vary by state and setting. However, generally, these interventions require documented justification, use of the least restrictive method possible, and continuous monitoring. Improper use can lead to legal repercussions, including lawsuits.
- Ethical Considerations: Ethical principles emphasize respecting individual autonomy and dignity. Restraint and seclusion can be traumatic and infringe on an individual’s rights. Therefore, careful consideration must be given to the potential risks and benefits. Ethical guidelines suggest that use should be minimized, carefully documented, and reviewed by a multidisciplinary team.
Before using restraint or seclusion, the situation needs to be thoroughly assessed, documented, and steps to minimize the need for such intervention explored. Following the intervention, comprehensive debriefing and documentation are crucial. Regular reviews of restraint and seclusion protocols are also vital to ensure they align with current best practice and legal requirements.
Q 26. Describe your experience with behavior management in various settings (e.g., school, home, community).
My experience with behavior management spans various settings, requiring adaptability and tailored approaches.
- Schools: In school settings, I’ve collaborated with teachers, administrators, and support staff to develop Individualized Education Programs (IEPs) for students with severe behavior disorders. This involved functional behavior assessments, implementing positive behavior support plans, and training staff on de-escalation techniques. I’ve worked to create inclusive classroom environments where students can thrive.
- Homes: Working with families, I’ve provided in-home support and training, helping parents understand the functions of their child’s behavior and develop consistent, positive behavior management strategies. This includes teaching parenting skills and providing emotional support to families.
- Community: In community-based settings, I’ve worked with individuals in group homes or day programs, focusing on skill building, social interaction, and community integration. This often involves collaboration with community agencies and supporting individuals’ participation in community activities.
For example, in a school setting, I helped a student with autism who frequently engaged in disruptive behaviors by implementing a visual schedule and teaching him alternative communication methods. In a home setting, I worked with a family to address their child’s aggression by using positive reinforcement techniques and helping the family create a consistent routine.
Q 27. How do you identify and address potential triggers for challenging behaviors?
Identifying and addressing triggers is crucial. This involves careful observation and data collection to determine patterns and precursors to challenging behaviors.
- Functional Behavior Assessment (FBA): As mentioned earlier, the FBA is key to identifying triggers. It helps determine what precedes the behavior (antecedents) and what maintains it (consequences).
- Environmental Modifications: Once triggers are identified, changes can be made to the environment to minimize their occurrence. This might involve adjusting the sensory environment, structuring the day more predictably, or removing specific stimuli.
- Skill Building: Sometimes, challenging behaviors occur because an individual lacks the skills to cope with specific situations. Teaching alternative behaviors (e.g., communication skills, coping strategies) can help reduce reliance on challenging behaviors.
- Medication Review (if applicable): If medication is part of the treatment plan, its effectiveness in managing triggers needs to be regularly evaluated.
For example, if a student’s aggression is triggered by loud noises, the school environment can be modified by reducing noise levels or providing the student with noise-canceling headphones. Teaching the student coping mechanisms for dealing with sensory overload would further address the underlying cause of the behaviour.
Q 28. Explain your experience working with specific diagnostic categories (e.g., autism, intellectual disability).
My experience includes working with individuals across a range of diagnoses, understanding that each diagnosis presents unique challenges and requires specialized interventions.
- Autism Spectrum Disorder (ASD): Working with individuals with ASD often involves addressing communication difficulties, sensory sensitivities, and repetitive behaviors. Interventions might include ABA, social skills training, and sensory integration strategies.
- Intellectual Disability (ID): Individuals with ID might require support with adaptive skills, communication, and social interaction. Interventions might focus on teaching functional skills, promoting independence, and providing supportive environments.
- Other Diagnoses: I also have experience with other disorders that can present with severe behavioral challenges, such as Oppositional Defiant Disorder (ODD), Conduct Disorder (CD), and Attention-Deficit/Hyperactivity Disorder (ADHD). Interventions are tailored to the specific needs of each individual, often involving a combination of therapeutic approaches.
For example, a child with autism and self-injurious behavior might benefit from an ABA program to reduce self-harm and replace it with more adaptive ways of communicating distress. A person with intellectual disabilities might need support with daily living skills and community integration, using a person-centered approach to maximize their independence and quality of life.
Key Topics to Learn for Severe Behavior Disorders Interview
- Understanding the Diagnostic Spectrum: Develop a strong grasp of various severe behavior disorders, including their diagnostic criteria, symptoms, and comorbidities (e.g., Autism Spectrum Disorder, Oppositional Defiant Disorder, Conduct Disorder, Intermittent Explosive Disorder).
- Behavioral Assessment and Intervention Strategies: Familiarize yourself with different assessment tools and methodologies used to evaluate behavior, and master various evidence-based intervention strategies such as Applied Behavior Analysis (ABA), Dialectical Behavior Therapy (DBT), and Positive Behavior Support (PBS). Understand the importance of functional behavior assessments (FBAs) and behavior intervention plans (BIPs).
- Crisis Management and De-escalation Techniques: Practice and understand various techniques for managing crisis situations and de-escalating aggressive or self-harming behaviors. This includes understanding the importance of safety planning and environmental modifications.
- Ethical Considerations and Legal Frameworks: Be prepared to discuss ethical considerations in working with individuals with severe behavior disorders, including confidentiality, informed consent, and mandated reporting. Understand relevant legal frameworks and regulations.
- Collaboration and Teamwork: Demonstrate understanding of the importance of collaboration with families, caregivers, educators, and other professionals involved in the care of individuals with severe behavior disorders.
- Data Collection and Analysis: Know how to effectively collect, analyze, and interpret behavioral data to inform treatment decisions and measure the effectiveness of interventions.
- Cultural Considerations: Demonstrate awareness and sensitivity to cultural factors that may influence the presentation and treatment of severe behavior disorders.
- Trauma-Informed Care: Understand the impact of trauma on behavior and the importance of incorporating trauma-informed principles into assessment and intervention.
Next Steps
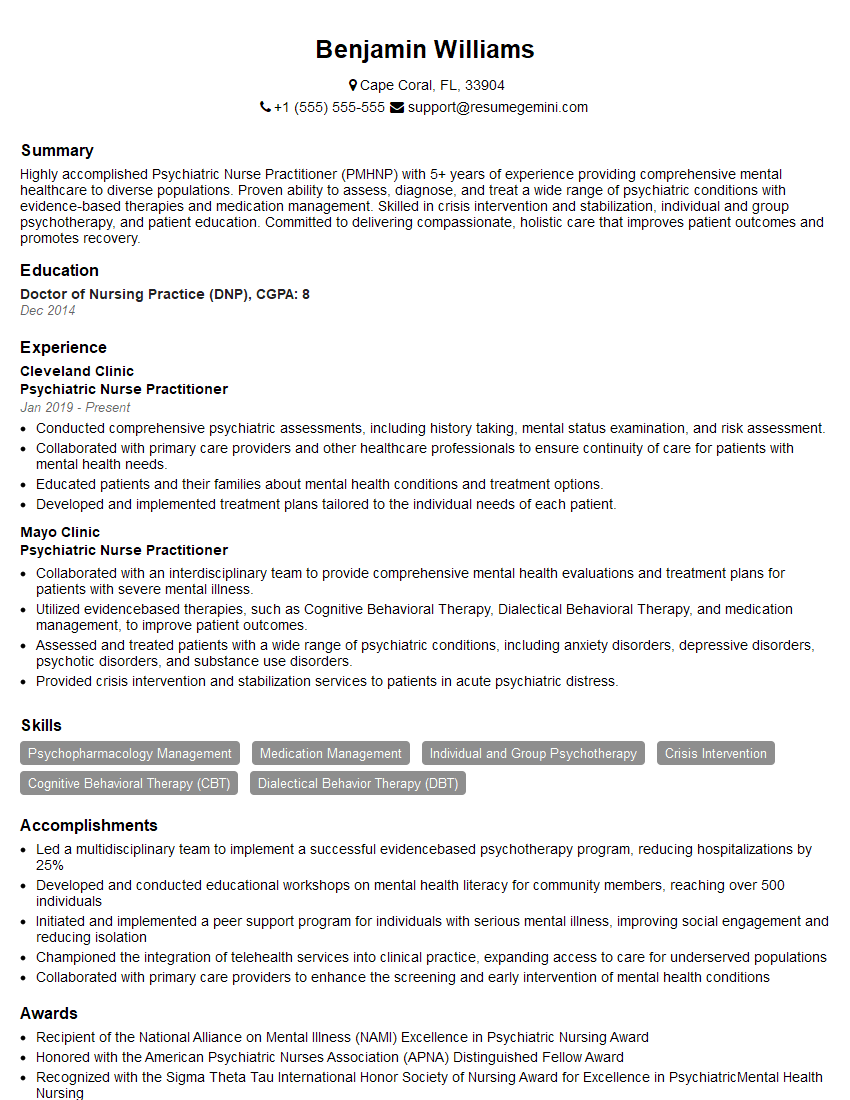
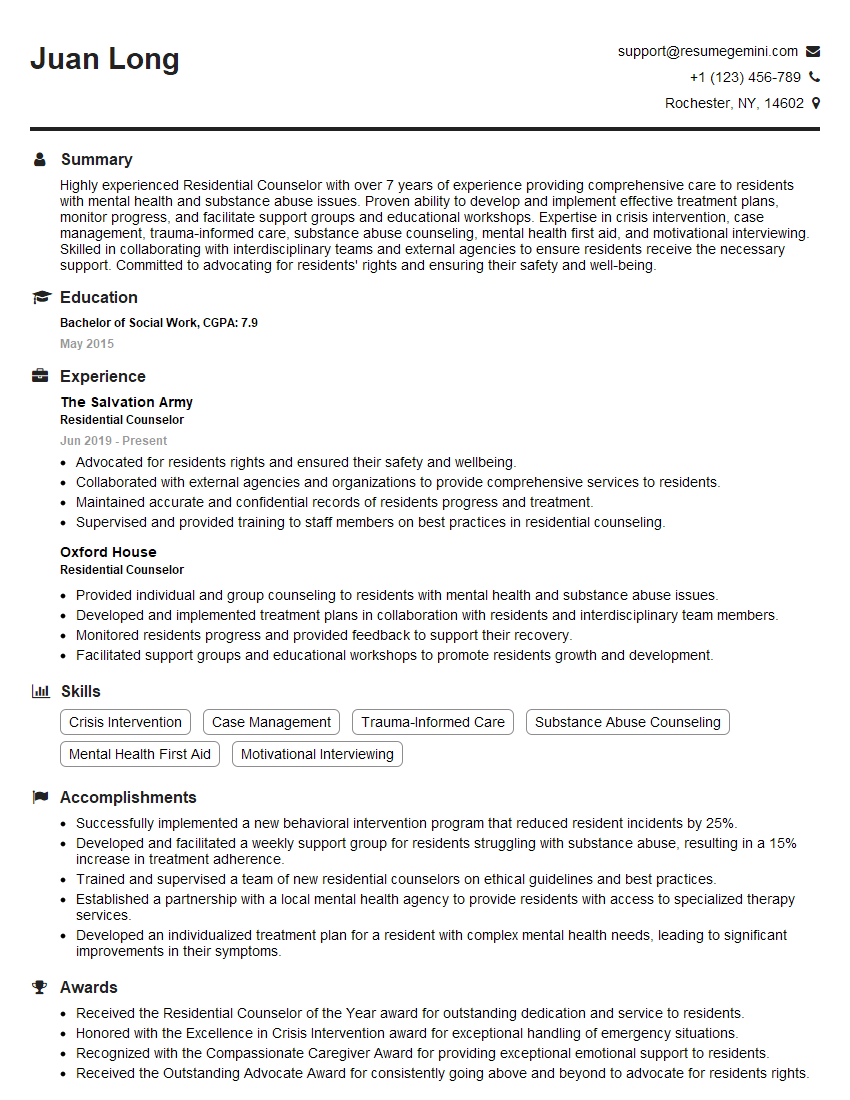
Mastering the complexities of Severe Behavior Disorders significantly enhances your career prospects in mental health, paving the way for specialized roles and leadership opportunities. To maximize your job search success, it’s crucial to create a compelling and ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource to help you build a professional resume that stands out. Use their tools to craft a document showcasing your expertise; examples of resumes tailored to Severe Behavior Disorders are available to guide you. Investing time in a strong resume is an investment in your future career.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO