Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Sensory Integration for Students with Mental Handicaps interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Sensory Integration for Students with Mental Handicaps Interview
Q 1. Describe the principles of Sensory Integration therapy.
Sensory Integration (SI) therapy is based on the principle that the brain needs organized sensory input to develop and function effectively. It posits that our brains constantly receive and process sensory information from our bodies and the environment (touch, sight, sound, smell, taste, movement, and balance). This information is integrated to create meaningful experiences and guide our actions. When this integration process is inefficient, sensory processing difficulties arise. SI therapy aims to provide carefully planned sensory experiences to help the brain organize and interpret sensory input more effectively, leading to improved behavior, learning, and participation in daily life. Think of it like building a strong foundation for a house: if the foundation (sensory processing) is weak, the entire structure (behavior and functioning) is at risk.
Q 2. Explain the difference between sensory modulation, sensory discrimination, and sensory-based motor skills.
These three concepts are interconnected aspects of sensory processing:
- Sensory Modulation: This refers to the brain’s ability to regulate its response to sensory input. It’s about the intensity of the response, not the accuracy. For example, someone with poor modulation might overreact to a light touch (hyper-responsive) or be completely oblivious to a loud noise (hypo-responsive).
- Sensory Discrimination: This is the brain’s ability to accurately distinguish between different sensory stimuli. It’s about accuracy of perception. For instance, someone with poor discrimination might struggle to tell the difference between two textures or identify the source of a sound.
- Sensory-Based Motor Skills: These are motor skills that rely on sensory information for planning, execution, and feedback. Examples include posture, balance, coordination, and fine motor skills. The brain uses sensory information (e.g., proprioception – awareness of body position) to guide movements.
In essence, you need good sensory modulation to handle the level of sensory input, good sensory discrimination to make sense of the information received, and efficient sensory-based motor skills to act on that information appropriately.
Q 3. How would you assess a student’s sensory processing needs?
Assessing a student’s sensory processing needs involves a multi-faceted approach. It’s not just about observing behaviors; it’s about understanding the underlying sensory challenges. The process typically includes:
- Parent/Teacher Interviews: Gathering information about the child’s sensory behaviors at home and school. This includes what triggers reactions, the types of sensory sensitivities, and the impact on daily functioning.
- Observations: Observing the student in different environments and during various activities to identify sensory seeking or avoiding behaviors, and their responses to different sensory inputs. For example, does the student seek out intense movement or avoid certain textures?
- Standardized Assessments: Using standardized sensory assessments, like the Sensory Profile or the Sensory Processing Measure, to quantify sensory processing strengths and weaknesses. These tools help objectively measure responses to sensory input.
- Occupational Therapy Evaluation: A qualified occupational therapist performs a thorough evaluation incorporating the above methods. They use their expertise to interpret the collected information and create a personalized intervention plan.
It is crucial to remember that observations should be interpreted within the context of the student’s overall development and potential co-occurring conditions.
Q 4. What are the common signs of sensory processing disorder in students with mental handicaps?
Students with mental handicaps often experience sensory processing challenges that can manifest in various ways. The presence of a mental handicap doesn’t automatically indicate SPD, but it can increase the likelihood and complexity of sensory issues. Common signs include:
- Unusual responses to sensory input: This could be hyper- or hypo-reactivity to touch, sound, light, or movement. A student might be overly sensitive to tags on clothing or seem unaware of loud noises.
- Difficulties with self-regulation: They may struggle to manage their arousal levels, leading to outbursts, meltdowns, or withdrawal.
- Motor skill challenges: Poor coordination, balance problems, and difficulties with fine motor tasks are frequently observed.
- Difficulties with attention and focus: Over- or under-stimulation from their environment can impair their concentration.
- Social interaction challenges: Misinterpreting social cues, avoiding physical contact, or engaging in repetitive movements can stem from sensory processing challenges.
It’s important to note that these signs can overlap with other developmental disabilities, so a thorough assessment is crucial.
Q 5. What are some adaptive strategies you would implement for a student with tactile defensiveness?
Tactile defensiveness, an aversion to touch, requires a gradual and systematic approach. Here are some adaptive strategies:
- Gradual desensitization: Begin with light, gentle touch and slowly introduce heavier pressure over time. This could involve using different textured brushes or fabrics.
- Deep pressure: Provide deep pressure through hugs, weighted blankets, or heavy work activities like pushing or pulling heavy objects. Deep pressure can be calming and organizing.
- Predictable touch: Always warn the student before touching them, giving them a chance to prepare. A simple, ‘I’m going to touch your arm now’ can make a big difference.
- Positive sensory experiences: Pair positive sensory experiences with touch, like playing with playdough with a pleasant scent or using textured paints.
- Environmental modifications: Adjust the classroom environment by removing potentially irritating textures or fabrics.
Remember, patience and consistency are key. The goal isn’t to eliminate tactile defensiveness completely, but to make the student more comfortable with a broader range of tactile experiences.
Q 6. How would you create a sensory-friendly classroom environment?
Creating a sensory-friendly classroom minimizes overstimulation and supports students’ sensory needs. Strategies include:
- Minimize visual clutter: Keep the classroom organized, use calming colors, and reduce bright or flashing lights.
- Reduce auditory distractions: Use sound-absorbing materials, control noise levels, and provide quiet areas for breaks. Minimize sudden loud noises.
- Provide tactile choices: Offer a variety of textured materials for fidgeting or self-regulation, such as stress balls, putty, or textured blankets.
- Create movement breaks: Incorporate opportunities for movement into the day, such as short walks, stretches, or sensory-motor activities.
- Provide a calm-down area: Designate a quiet space with comfortable seating and calming sensory tools for students who need a break from the stimulating environment.
- Lighting adjustments: Use soft, diffused lighting and provide options for dimming lights or using lamps as needed.
Creating a predictable and structured environment helps students feel safe and secure, which is particularly important for students with mental handicaps.
Q 7. Explain different sensory diets and their application.
A sensory diet is a personalized plan of sensory activities that helps regulate a student’s sensory system. It’s not a diet in the traditional sense; it’s a customized program of sensory input designed to support optimal functioning. Examples include:
- Proprioceptive activities: Activities that involve body awareness and weight-bearing, such as heavy work (pushing, pulling, lifting), yoga, or carrying objects. This helps to ground and organize the body.
- Vestibular activities: Activities that stimulate the inner ear, such as swinging, rocking, or spinning. These can be calming or energizing depending on the type of movement and the individual’s needs.
- Tactile activities: Activities that stimulate the sense of touch, such as playing with playdough, using textured brushes, or working with different materials. These can help desensitize or provide sensory input.
- Auditory activities: Using calming or stimulating sounds, like nature sounds or rhythmic music. This can help regulate arousal levels.
- Visual activities: Using calming visual aids, like bubble tubes or calming visuals. These are used to modulate visual stimulation.
Sensory diets are customized based on an individual’s sensory profile and should be implemented in consultation with an occupational therapist. The goal is to create a balanced sensory experience throughout the day, preventing sensory overload or under-stimulation and supporting the child’s optimal learning and well-being.
Q 8. How do you differentiate between sensory seeking and sensory avoiding behaviors?
Differentiating between sensory seeking and sensory avoiding behaviors requires careful observation and understanding of the student’s responses to sensory input. Sensory seeking behaviors are characterized by an active search for sensory stimulation. These students might crave intense sensations, constantly seeking movement, pressure, or loud noises. They might appear restless, fidgety, and always in motion. In contrast, sensory avoiding behaviors involve actively avoiding sensory input. These students might be highly sensitive to certain textures, sounds, or lights, retreating from them to reduce overwhelming stimulation. They might exhibit behaviors like covering their ears, avoiding crowds, or exhibiting strong negative reactions to unexpected touches.
Example: A sensory-seeking student might repeatedly jump on a trampoline, while a sensory-avoiding student might cover their eyes during a flash mob dance performance.
It’s crucial to remember that both behaviors are strategies the student uses to regulate their nervous system. Understanding the *why* behind the behavior is critical to effective intervention. We must consider the student’s developmental level and sensory profile to effectively differentiate between the two.
Q 9. How would you adapt sensory activities for students with various cognitive abilities?
Adapting sensory activities for students with various cognitive abilities requires careful consideration of their individual needs and capabilities. We need to adjust the complexity, duration, and sensory input to match their cognitive level. For students with lower cognitive abilities, activities should be simple, highly structured, and focused on one or two sensory modalities at a time. For instance, a simple activity might involve repeatedly squeezing a stress ball or listening to calming music. We can gradually increase complexity as they become comfortable and proficient. For students with higher cognitive abilities, activities can be more complex, engaging multiple sensory modalities, and requiring problem-solving or sequencing skills. These students might enjoy activities that incorporate different materials, sensory challenges, and complex cognitive elements. We can incorporate these challenges into a play-based setting to engage the child’s interest.
Example: For a student with lower cognitive abilities, a weighted blanket might provide comfort, while a student with higher cognitive abilities might benefit from a complex sensory bin incorporating different textures, weights and objects which require problem solving and exploration.
In all cases, careful observation and frequent reassessment of the student’s response to the activities are critical to ensure optimal engagement and avoid sensory overload or under-stimulation.
Q 10. Describe how you would collaborate with other professionals (e.g., OT, PT, teachers) in providing sensory integration support.
Collaboration is fundamental to effective sensory integration support. I establish strong communication channels with occupational therapists (OTs), physical therapists (PTs), and teachers to share information and coordinate interventions. This involves regular meetings to discuss the student’s progress, challenges, and treatment goals. We develop a shared understanding of the student’s sensory profile and collaboratively design individualized intervention plans. The OT might focus on fine motor skills and adaptive techniques, while the PT addresses gross motor skills and movement planning. Teachers provide valuable insights into classroom behavior and learning challenges, which can help us contextualize the sensory integration strategies within the educational setting. This collaborative approach allows for comprehensive support and a consistent approach to address the student’s needs across all environments.
Example: The OT might work on improving hand strength through play-based activities, while the PT addresses posture and balance, and I design activities which incorporate both aspects and can be implemented within the classroom environment, such as active games involving movement and object manipulation.
Q 11. What are the ethical considerations when working with students and their families regarding sensory integration?
Ethical considerations are paramount when working with students and their families. Informed consent is essential; I ensure families understand the intervention’s purpose, procedures, benefits, and potential risks before starting any therapy. Confidentiality is strictly maintained. I respect the family’s values, beliefs, and cultural background when developing intervention plans. I am transparent and honest in my communication, explaining progress, challenges, and any modifications to the treatment plan. Culturally sensitive practices are crucial, and I make every effort to tailor my approach to the family’s specific needs and preferences.
Example: If a family has religious objections to certain types of touch, I would adapt the sensory activities to respect their beliefs while still achieving the therapeutic goals. I always ensure the family is empowered in the decision-making process regarding their child’s care.
Q 12. How would you document and measure progress in sensory integration therapy?
Documenting and measuring progress involves a multi-faceted approach. I use a combination of observational data, standardized assessments, and parent/teacher reports. Observational data is collected during therapy sessions, noting the student’s responses to different sensory activities, their level of engagement, and any changes in behavior. Standardized assessments, such as the Sensory Profile or the Sensory Integration and Praxis Tests, provide quantifiable measures of sensory processing skills. Regular parent and teacher reports provide valuable insight into the student’s progress in different settings. This holistic approach allows for a comprehensive understanding of the student’s progress and guides adjustments to the treatment plan as needed. I use a progress report form to clearly document changes, using graphs and tables to illustrate improvement.
Example: If a student initially showed signs of tactile defensiveness, I would document the frequency and intensity of these behaviors initially and compare this to subsequent observations as well as through standardized tests.
Q 13. Explain the use of specific sensory tools and equipment in your practice.
My practice utilizes a variety of sensory tools and equipment tailored to individual student needs. These include weighted blankets or vests for providing deep pressure input and promoting calmness, therapy balls and swings for vestibular stimulation, and various textured materials to explore tactile input. I also use visual aids, auditory tools (calming music, noise-canceling headphones), and specialized equipment like a balance board to address postural control and coordination. The choice of tools is always dictated by the student’s sensory profile and the therapeutic goals. The safety and comfort of the student remain my primary focus when selecting equipment.
Example: A student with difficulty focusing might benefit from a weighted lap pad, while a student with low muscle tone might benefit from activities on a therapy ball to improve core strength and balance.
Q 14. Describe your experience using different sensory integration assessment tools.
My experience encompasses various sensory integration assessment tools. The Sensory Profile is a valuable tool for understanding a student’s sensory processing patterns, providing valuable insight into their sensory preferences, sensitivities, and behavioral responses. The Sensory Integration and Praxis Test (SIPT) offers a more comprehensive, standardized assessment of sensory motor skills. In addition to formal assessments, I also conduct informal observations and utilize checklists, rating scales, and parent/teacher interviews to gather a comprehensive picture of the student’s sensory needs. The choice of assessment is dependent on the student’s age, cognitive abilities, and the specific questions guiding the assessment. Combining different approaches ensures a more accurate and thorough understanding of the student’s sensory profile.
Example: For a younger student, I might use a parent interview and informal observation, while for an older student with good communication skills, the Sensory Profile might be appropriate.
Q 15. How would you handle a situation where a student’s sensory needs disrupt the classroom?
When a student’s sensory needs disrupt the classroom, the key is proactive, individualized intervention. It’s not about silencing the student, but understanding and addressing the root cause of the disruption. First, I’d conduct a thorough sensory profile to identify specific sensory sensitivities – is it auditory overload, tactile defensiveness, visual distractions, or something else? This involves observation, parent/teacher input, and potentially formal assessment tools.
Once the triggers are pinpointed, we create a personalized sensory diet. This isn’t a diet in the traditional sense, but rather a structured plan incorporating sensory activities throughout the day to regulate the student’s sensory system. For example, a student sensitive to loud noises might benefit from noise-canceling headphones during certain activities or designated quiet areas. A student with tactile defensiveness might need different textured materials during art projects or prefer certain clothing textures.
Classroom modifications are crucial. This might include adjusting lighting, rearranging seating to minimize distractions, providing fidget toys for self-regulation, or establishing clear visual schedules. Communication with the teacher and other staff is vital for consistent implementation. The goal is to create a predictable and supportive environment that reduces sensory overwhelm and promotes the student’s ability to focus and learn.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How would you address challenging behaviors related to sensory overload or under-responsivity?
Challenging behaviors stemming from sensory overload or under-responsivity require a careful and compassionate approach. It’s essential to remember that these behaviors are often communicative; the student is expressing their sensory needs through challenging actions. We need to decode this communication.
First, we analyze the behavior. When does it occur? What are the antecedents (what precedes the behavior)? What are the consequences (what follows the behavior)? This functional behavioral assessment (FBA) helps us understand the function of the behavior – is it to escape a sensory input, gain attention, or access something desired?
Based on the FBA, we design an intervention plan. This might involve teaching alternative communication strategies (e.g., using a visual schedule, picture cards, or a communication device), proactively providing sensory breaks or calming activities, and modifying the environment to minimize sensory triggers. Positive reinforcement for appropriate behaviors is crucial. For example, if a student is exhibiting self-injurious behavior due to tactile defensiveness, we might offer weighted blankets or provide opportunities for deep pressure through therapeutic activities.
Collaboration with the student’s therapists, teachers, and parents is critical for consistency and success. Regular monitoring and adjustments to the plan are necessary to ensure its effectiveness. The aim is not just to suppress the behavior, but to teach the student adaptive coping mechanisms for managing their sensory experiences.
Q 17. What are the limitations of Sensory Integration Therapy?
While Sensory Integration Therapy (SIT) is highly beneficial for many, it’s important to acknowledge its limitations. Firstly, it’s not a cure-all. It’s not effective for all individuals, particularly those with severe cognitive impairments or medical conditions that significantly impact sensory processing. The effectiveness of SIT also depends on the child’s engagement and motivation. If the child is resistant to participation, progress will be limited.
Secondly, SIT requires a specialized therapist with advanced training and experience. Access to qualified therapists can be a significant barrier, both geographically and financially. The intensity and duration of therapy required can also be substantial, making it challenging for some families.
Finally, while SIT can improve sensory processing and related skills, it doesn’t address all difficulties a student might face. It may need to be combined with other therapeutic approaches, such as occupational therapy, speech therapy, or behavioral therapy, to address the student’s overall needs. It’s crucial to have realistic expectations about what SIT can accomplish.
Q 18. Describe a time you successfully implemented a sensory integration strategy with a student.
I worked with a young boy, Alex, who had significant difficulties with auditory processing and displayed significant anxiety in noisy environments. He would often cover his ears, cry, and withdraw during group activities. His sensory profile revealed hypersensitivity to loud sounds and rapid changes in auditory stimulation.
We implemented a multifaceted strategy. First, we created a quiet corner in the classroom equipped with noise-canceling headphones and soft lighting. We also developed a visual schedule indicating noisy and quiet times. Alex participated in auditory desensitization exercises, starting with very soft sounds and gradually increasing the volume and complexity of auditory stimuli. This involved activities like listening to calming nature sounds and progressively adding other sounds at a low volume.
We also taught him self-regulation strategies, such as deep breathing and using a weighted lap pad for grounding. Alex’s parents were actively involved, implementing similar strategies at home. The combination of environmental modifications, therapeutic activities, and self-regulation skills greatly improved Alex’s ability to manage auditory input, reducing his anxiety and improving his participation in the classroom.
Q 19. How do you adapt sensory strategies for students with various levels of mental handicaps?
Adapting sensory strategies requires careful consideration of the student’s individual cognitive and physical abilities. For students with mild mental handicaps, we might use more complex strategies involving verbal instruction and problem-solving. We can adjust the difficulty level of activities to ensure appropriate challenge and engagement. Visual supports, such as picture schedules and social stories, are highly beneficial.
For students with more significant cognitive impairments, we focus on simpler, more concrete interventions. We might use highly structured routines and physical prompts to guide their participation in sensory activities. The activities themselves should be simpler and more repetitive, with a focus on sensory exploration and tactile feedback. We utilize adaptive equipment and adjust the sensory input to suit their individual needs and tolerance levels. Communication with caregivers is paramount; ensuring consistency between home and school environments is crucial for success.
In all cases, the focus is on finding the right balance between providing sensory input that’s stimulating enough to be engaging, but not overwhelming to the point of causing distress. The sensory diet is constantly evaluated and adapted based on the student’s response and progress.
Q 20. What is your understanding of the Ayres Sensory Integration® approach?
The Ayres Sensory Integration® approach is a widely recognized and research-based approach to sensory integration therapy developed by Dr. Jean Ayres. It’s a specialized form of occupational therapy that focuses on enhancing the brain’s ability to organize and interpret sensory information from the body and the environment. The core principle is that the brain’s organization of sensory input impacts motor skills, cognitive abilities, and social-emotional functioning.
Ayres Sensory Integration® utilizes carefully designed activities that are tailored to the individual’s sensory needs and challenges. These activities aim to challenge the student’s sensory systems in a playful and engaging way, promoting adaptive responses and the development of more efficient neural pathways. The therapist acts as a facilitator, observing the child’s reactions and adapting the activities as needed to provide just the right amount of sensory stimulation. A key aspect is the emphasis on the child’s active participation and self-directed play.
The approach does not involve passive sensory stimulation, but rather challenges the child to actively participate and organize sensory information, which is crucial for improving adaptive behavior and cognitive skills.
Q 21. Explain the importance of parent/guardian involvement in sensory integration therapy.
Parent/guardian involvement is absolutely vital to the success of sensory integration therapy. Consistency is key, and what we do in the therapeutic setting needs to be reinforced at home. Parents are the primary caregivers and spend the most time with the child, making them invaluable partners in the therapeutic process.
Active parent involvement starts with understanding the child’s sensory profile and the therapeutic goals. This typically involves collaboration between the therapist and parents to establish a home sensory diet that complements the therapy sessions. Parents learn how to implement sensory strategies at home, such as providing opportunities for specific sensory activities, modifying the home environment, and identifying and addressing sensory triggers.
Furthermore, parents can provide invaluable feedback to the therapist about the child’s progress and challenges outside of therapy sessions. This collaborative approach facilitates a holistic and more effective therapeutic plan, improving outcomes and enhancing the child’s overall well-being. Regular communication and ongoing support are essential to achieve sustained positive changes in the child’s sensory processing and daily functioning.
Q 22. How do you ensure the safety of students during sensory integration activities?
Safety is paramount in sensory integration therapy. We prioritize a risk-assessment approach for each student, carefully considering their individual sensory profiles and potential challenges. This means adapting the environment and activities to minimize risks. For example, if a student has a strong aversion to touch, we’ll avoid activities that involve unexpected physical contact. For students with potential self-injurious behaviors, we’ll implement strategies to prevent access to harmful objects or create a calming space to reduce the likelihood of outbursts. We also ensure appropriate adult-to-student ratios, depending on the students’ needs and the activity, and thoroughly train staff on safe handling techniques and emergency procedures. The environment itself is designed with safety in mind – well-padded surfaces, secured equipment, and clear pathways to prevent falls or collisions. We frequently review and update safety protocols to meet the evolving needs of our students.
Think of it like building a playground: we carefully select age-appropriate equipment, check for any potential hazards, and ensure the ground is soft enough to cushion any falls. Similarly, we adapt the sensory environment to be safe and supportive for each child.
Q 23. Discuss the role of play in sensory integration therapy.
Play is the cornerstone of sensory integration therapy, providing a natural and engaging context for therapeutic intervention. It’s how children learn and process sensory information organically. Through play, students explore various textures, sounds, movements, and visual stimuli, developing their sensory processing skills without feeling like they’re ‘doing therapy’. For example, a student struggling with proprioceptive input (body awareness) might engage in activities like swinging, climbing, or playing with weighted blankets. A child hypersensitive to sound might find comfort in a quiet corner with noise-canceling headphones. The therapist carefully selects toys and activities to target specific sensory needs while simultaneously promoting social and emotional development through collaborative play.
Consider a child who’s constantly fidgeting in class. Through play, we can incorporate activities that provide just the right amount of movement and tactile stimulation to help them regulate their sensory system, improving their ability to focus and participate in class. The structured, playful environment allows for a more organic approach to sensory integration.
Q 24. How would you incorporate sensory integration strategies into the student’s Individualized Education Program (IEP)?
Sensory integration strategies should be explicitly incorporated into the student’s IEP, making it a collaborative process involving parents, educators, and the sensory integration therapist. The IEP goals should clearly outline specific, measurable, achievable, relevant, and time-bound (SMART) objectives. For example, a goal might be: “To improve bilateral coordination and hand-eye coordination for improved handwriting skills within three months, as measured by a decrease in writing errors and an increase in writing speed.” Sensory activities chosen for the IEP would directly address the stated goals. These activities might include weighted utensils for writing, activities that promote vestibular input (balance and movement) for postural control, and tactile activities that promote hand strength and fine motor skills. The IEP also documents the frequency, duration, and setting for these interventions, specifying who will deliver the therapy (therapist, teacher, or aide). Regular progress monitoring is critical and should be reflected in IEP reviews.
For instance, an IEP might include a goal to decrease tactile defensiveness. To achieve this, the IEP would outline specific sensory activities that gradually introduce different textures to the student, starting with preferred textures and gradually introducing less preferred ones. The progress toward this goal would be regularly assessed.
Q 25. How do you monitor and evaluate the effectiveness of sensory integration interventions?
Monitoring and evaluating the effectiveness of sensory integration interventions is an ongoing process, not a one-time event. We use a variety of methods, including observation, standardized assessments, and informal measures. Observations during therapy sessions are vital, noting the student’s responses to different activities, their level of engagement, and any changes in behavior. Standardized assessments, such as the Sensory Profile or the Sensory Integration and Praxis Test, provide quantitative data on sensory processing skills. Informal measures, like checklists completed by teachers or parents, track progress in the classroom or at home. We also utilize qualitative data by conducting regular meetings with the child, parents, and educators to obtain feedback and adjust our approach as necessary.
Imagine tracking a student’s ability to sit still during circle time. We might start by observing how long they can sit before fidgeting. Over time, we’ll chart the duration, noting improvements resulting from sensory integration interventions. The combination of objective data from assessments and subjective feedback from stakeholders ensures a comprehensive evaluation of the intervention’s impact.
Q 26. What professional development have you pursued related to sensory integration?
My professional development in sensory integration has been continuous and multifaceted. I’ve completed a comprehensive certification program in Sensory Integration and Praxis Tests, and regularly attend workshops and conferences presented by leading experts in the field. I actively seek continuing education credits to stay abreast of current research and best practices. I’m also a member of relevant professional organizations that provide access to research and peer-reviewed publications in sensory processing disorders. This ensures my practice is informed by the latest evidence-based strategies and techniques. Furthermore, I maintain ongoing professional relationships with other professionals, such as occupational therapists specializing in sensory integration, allowing for knowledge-sharing and case consultation.
I view professional development as an ongoing commitment. It’s not just about earning credits; it’s about staying current and providing the best possible care to my students.
Q 27. What are your strengths and weaknesses in working with students with sensory processing challenges?
One of my greatest strengths is my ability to build rapport with students and create a trusting therapeutic relationship. This is crucial for success in sensory integration therapy because it allows students to feel safe enough to explore new sensations and challenges. I’m also adept at adapting my approach to meet the unique needs of each student, demonstrating flexibility in my interventions. However, like all professionals, I have areas for growth. One area I’m actively working on is further developing my expertise in working with students who have complex comorbid conditions, such as autism spectrum disorder in combination with sensory processing challenges. I actively participate in professional development to refine this skill.
Think of it as a musician always striving to improve their technique. While I’m proficient, I continually seek opportunities to hone my skills and expand my repertoire.
Q 28. Describe your experience using technology to support sensory integration.
Technology plays an increasingly important role in supporting sensory integration. I’ve used various technologies to enhance the therapeutic process. For example, interactive software programs can help students improve fine motor skills and visual-motor integration. Virtual reality (VR) can be used to create immersive sensory experiences to address specific sensory needs. Motion-tracking systems can provide objective data on movement patterns to guide interventions and track progress. I also use apps and digital platforms to communicate with parents and other professionals involved in the student’s care, sharing updates and progress reports efficiently.
For example, we’ve used a virtual reality program to simulate a calming ocean environment to help a student manage anxiety associated with overstimulation. The use of tech helps make therapy engaging and highly effective.
Key Topics to Learn for Sensory Integration for Students with Mental Handicaps Interview
- Understanding Sensory Processing: Differentiate between sensory modulation, sensory discrimination, and sensory-based motor performance. Explore how atypical sensory processing impacts learning and behavior in students with mental handicaps.
- Assessment and Evaluation: Learn various assessment tools and strategies used to identify sensory processing difficulties in this population. Understand the importance of observational skills and interpreting assessment data to inform intervention planning.
- Intervention Strategies: Explore a range of therapeutic approaches, including sensory diets, environmental modifications, and adaptive techniques. Understand the principles behind creating a supportive and stimulating learning environment.
- Collaboration and Communication: Discuss the importance of working collaboratively with parents, teachers, and other professionals. Master effective communication strategies for explaining sensory integration principles and intervention plans to diverse audiences.
- Individualized Education Program (IEP) Development: Understand how sensory integration needs are addressed within the IEP framework. Learn how to write measurable goals and objectives related to sensory processing and participation in educational activities.
- Ethical Considerations: Familiarize yourself with ethical practices related to assessment, intervention, and data privacy within the context of working with students with mental handicaps and their families.
- Data Collection and Analysis: Understand the importance of data-driven decision-making. Learn how to collect, analyze, and interpret data to demonstrate the effectiveness of interventions.
Next Steps
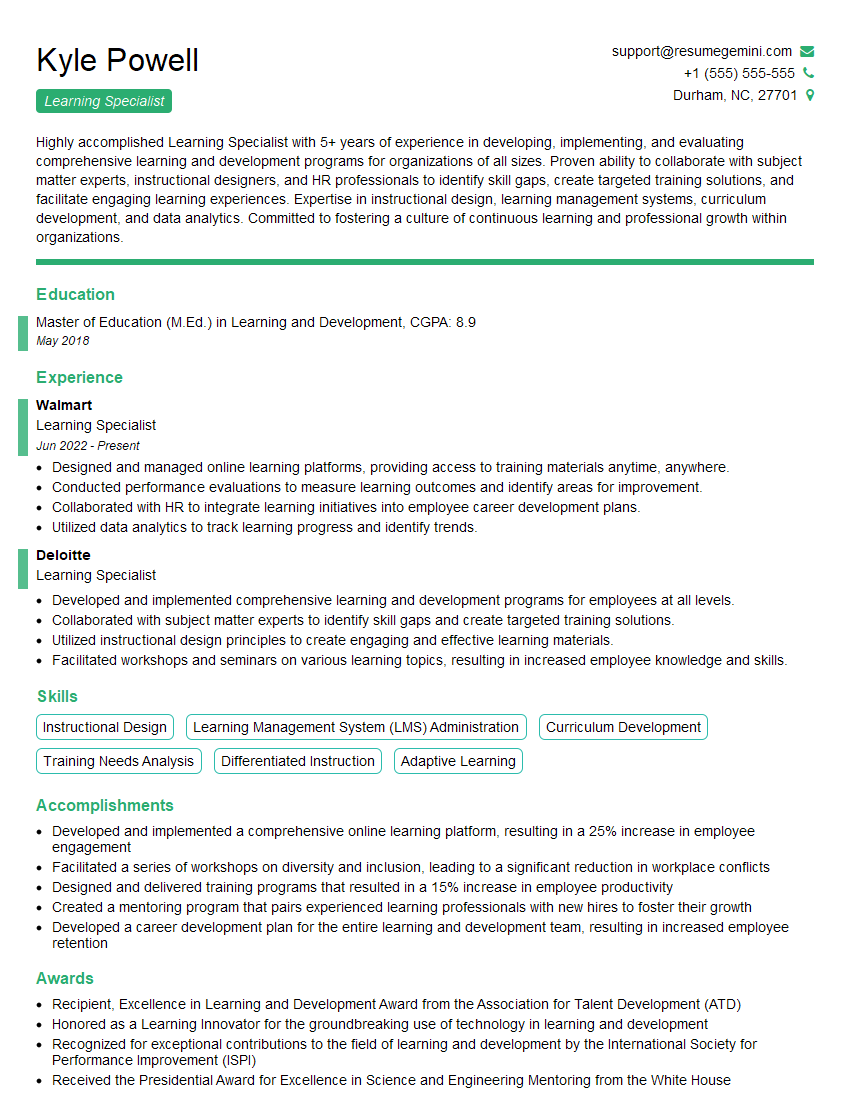
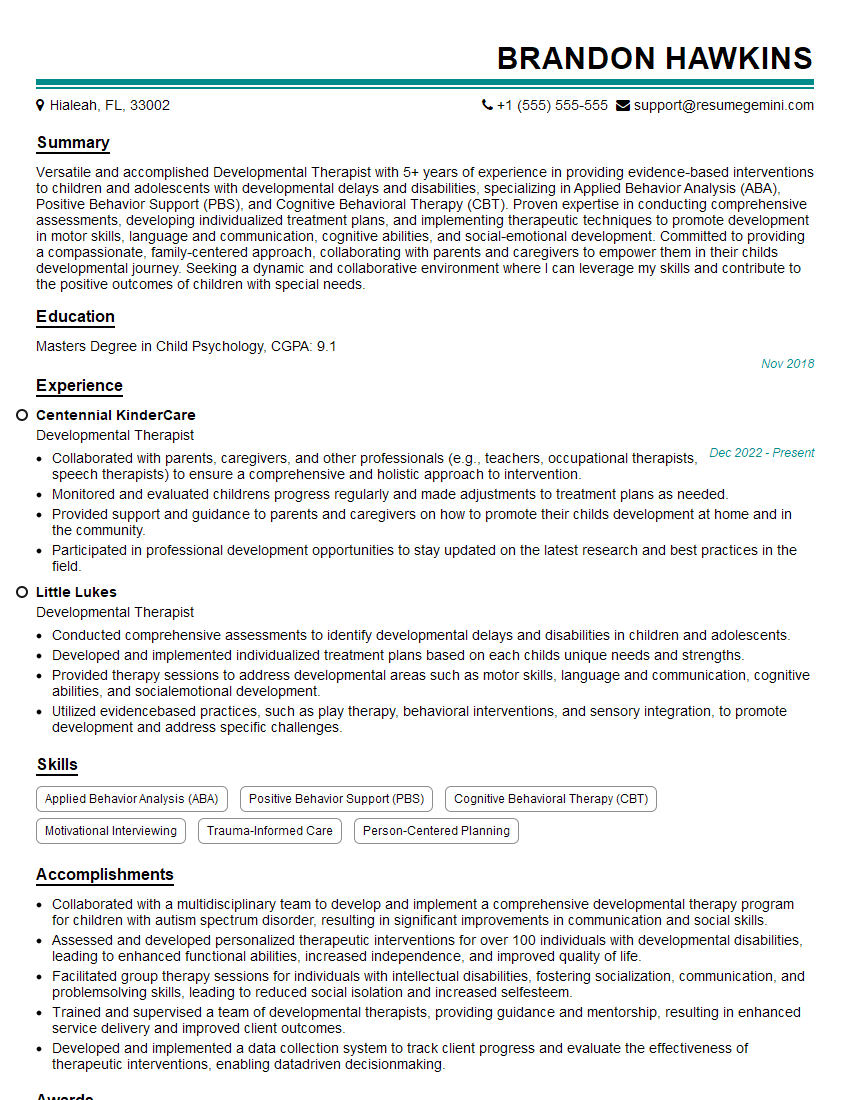
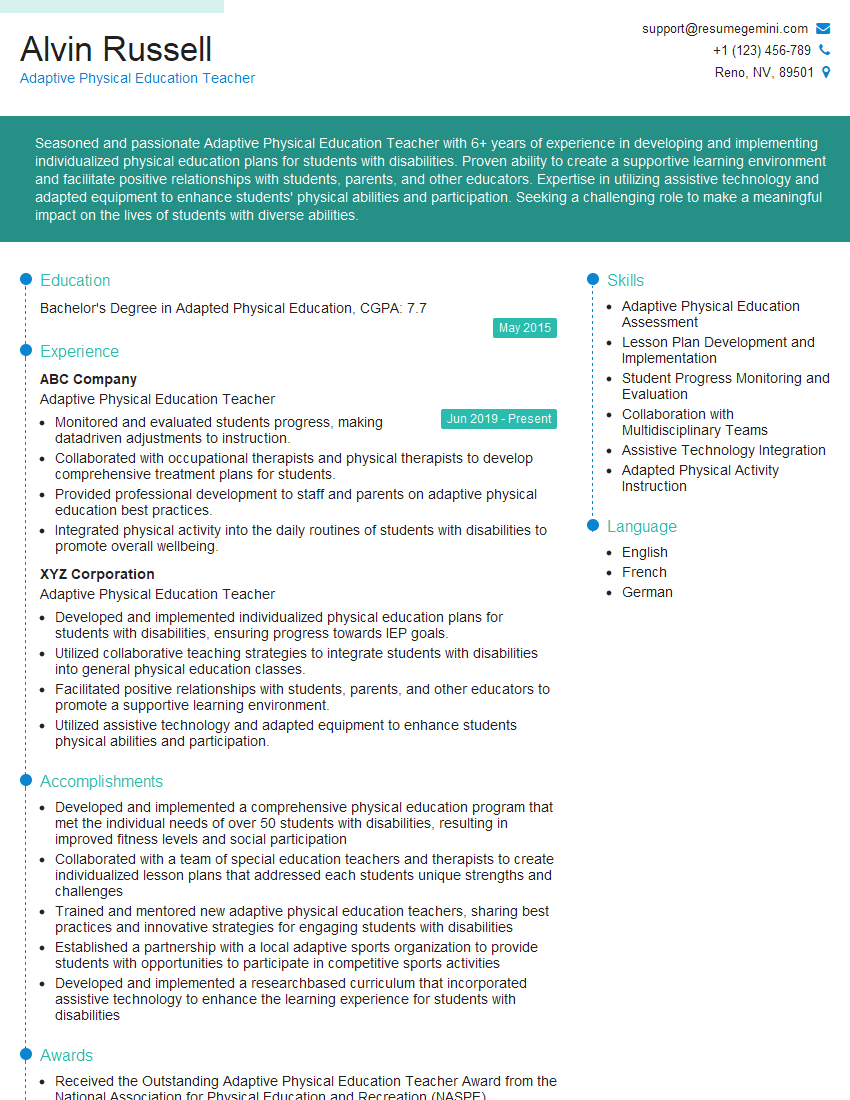
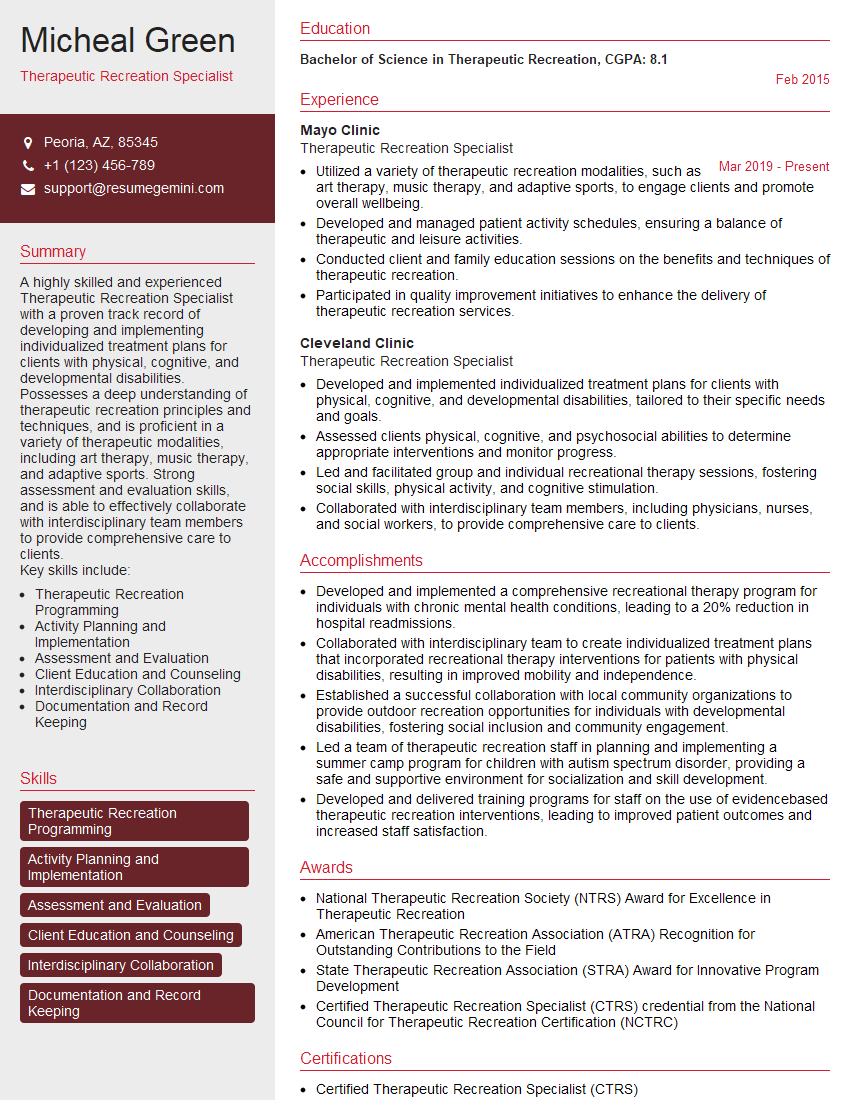
Mastering Sensory Integration for Students with Mental Handicaps opens doors to rewarding careers impacting the lives of vulnerable children. To maximize your job prospects, a strong, ATS-friendly resume is crucial. ResumeGemini offers a powerful tool to build a professional resume that highlights your skills and experience effectively. We provide examples of resumes tailored specifically to Sensory Integration for Students with Mental Handicaps to give you a head start. Take the next step in your career journey and create a resume that showcases your expertise.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO