Unlock your full potential by mastering the most common Prenatal Education interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Prenatal Education Interview
Q 1. Describe the stages of labor and delivery.
Labor and delivery is a multi-stage process. Understanding these stages helps expectant parents prepare and manage their expectations.
- Stage 1: Latent Phase – This is the beginning of labor, characterized by mild, irregular contractions that gradually become more frequent and intense. The cervix begins to dilate (open) from 0 to 4 centimeters. This phase can last for hours, even days, especially for first-time mothers. Think of it as the body’s gentle preparation for the main event.
- Stage 1: Active Phase – Contractions become stronger, longer, and more frequent. Cervical dilation progresses from 4 to 7 centimeters. This is where pain management techniques might be explored and implemented. This phase typically progresses faster than the latent phase.
- Stage 1: Transition Phase – This is the most intense part of labor, with strong contractions occurring very close together. Cervical dilation reaches 7 to 10 centimeters, fully opening the cervix for the baby to pass through. Many women describe this as the most challenging part of labor due to the increased intensity of contractions.
- Stage 2: Pushing Stage – Once the cervix is fully dilated, the mother begins pushing with each contraction to help deliver the baby. This stage can last from a few minutes to a few hours. It’s crucial for the mother to follow her healthcare provider’s instructions to help the baby safely descend through the birth canal.
- Stage 3: Delivery of the Placenta – After the baby is born, the placenta (afterbirth) detaches from the uterine wall and is delivered. This typically happens within 30 minutes of the baby’s birth. It’s a relatively short and less intense stage.
Each stage varies in length and intensity depending on individual factors such as previous pregnancies, baby’s position, and the mother’s overall health. It’s vital for expectant parents to attend prenatal classes to learn coping mechanisms and understand what to expect during each stage.
Q 2. Explain the benefits of breastfeeding.
Breastfeeding offers numerous benefits for both mother and baby. It’s a natural and ideal way to nourish a newborn.
- For the Baby: Breast milk is perfectly tailored to a baby’s nutritional needs. It contains antibodies that protect against infections, promotes healthy gut bacteria, and is easily digestible. It’s associated with lower risks of allergies, asthma, and ear infections. Breastfeeding also supports optimal brain development and strengthens the bond between mother and child.
- For the Mother: Breastfeeding releases hormones that promote uterine contraction, helping the uterus return to its normal size after delivery. It can also reduce the risk of postpartum hemorrhage and certain types of cancers. The physical act of breastfeeding can also release endorphins, which can help alleviate stress and promote relaxation. It can also contribute to weight loss.
While breastfeeding is highly beneficial, it’s important to remember that it’s not always easy. Support from healthcare professionals, family, and friends is crucial to overcome challenges. It’s also essential to acknowledge that formula feeding is a perfectly acceptable alternative when breastfeeding isn’t possible or desired.
Q 3. What are the common discomforts experienced during pregnancy, and how can they be managed?
Pregnancy brings about various discomforts, most of which are manageable. Understanding these issues and having coping strategies is key to a more comfortable pregnancy.
- Nausea and Vomiting (Morning Sickness): This commonly occurs during the first trimester. Small, frequent meals, avoiding strong odors, and ginger can help alleviate symptoms. Severe cases should be addressed by a healthcare provider.
- Heartburn: Hormonal changes and the growing uterus can lead to heartburn. Eating smaller meals, avoiding spicy foods, and elevating the head of the bed can provide relief.
- Back Pain: The extra weight of the pregnancy puts strain on the back. Maintaining good posture, engaging in low-impact exercise like swimming or prenatal yoga, and using supportive maternity belts can help.
- Swelling (Edema): Fluid retention can cause swelling in the ankles, feet, and hands. Elevating the legs, avoiding prolonged standing, and staying hydrated can help manage this. Severe swelling warrants immediate medical attention.
- Fatigue: Pregnancy is physically demanding. Prioritizing rest, getting enough sleep, and eating a nutritious diet are crucial.
- Constipation: Hormonal changes and reduced mobility contribute to constipation. Increasing fiber intake, staying hydrated, and gentle exercise can help.
It’s crucial to communicate any discomfort with your healthcare provider to rule out any serious complications and receive appropriate guidance.
Q 4. Discuss the importance of prenatal nutrition.
Prenatal nutrition is paramount to both the mother’s and baby’s health. A balanced diet provides essential nutrients for fetal growth and development, and supports the mother’s well-being.
- Folic Acid: Crucial for preventing neural tube defects. Found in leafy greens, legumes, and fortified cereals.
- Iron: Prevents anemia and supports oxygen delivery to the fetus. Found in red meat, spinach, and lentils.
- Calcium: Essential for bone development in the baby. Found in dairy products, leafy greens, and fortified foods.
- Protein: Supports tissue growth and development. Found in meat, poultry, fish, beans, and lentils.
- Omega-3 Fatty Acids: Supports brain development. Found in fatty fish like salmon, flaxseeds, and walnuts.
Prenatal vitamins often supplement the diet, ensuring the intake of crucial nutrients. A registered dietitian or healthcare provider can create a personalized nutrition plan based on individual needs and preferences. Focusing on whole, unprocessed foods is key.
Q 5. How would you teach expectant parents about newborn care?
Teaching expectant parents about newborn care involves a multi-faceted approach, focusing on practical skills and emotional preparedness.
- Feeding: Demonstrating proper latch techniques for breastfeeding or preparing formula appropriately.
- Diapering: Showing the proper way to change diapers, addressing potential skin irritations, and recognizing signs of diaper rash.
- Bathing: Demonstrating a safe and gentle bathing technique, emphasizing the importance of maintaining a warm and comfortable environment.
- Swaddling: Showing how to swaddle the baby securely, promoting a sense of safety and comfort.
- Soothing Techniques: Teaching parents various soothing techniques, such as skin-to-skin contact, rocking, or white noise, to calm a fussy baby.
- Recognizing Signs of Illness: Educating parents on recognizing signs of illness, such as fever, lethargy, or difficulty breathing, and emphasizing prompt medical attention when necessary.
- Safe Sleep Practices: Instructing parents on safe sleep practices, such as placing the baby on their back on a firm surface, and removing loose bedding from the crib.
Hands-on practice and demonstrations are crucial during newborn care classes. Creating a safe space for questions and concerns is also vital. Encouraging parents to ask for help when needed is also important.
Q 6. What are the signs of postpartum depression?
Postpartum depression (PPD) is a serious condition affecting mothers after childbirth. It’s essential to be aware of the symptoms.
- Persistent Sadness or Low Mood: A prolonged period of sadness or hopelessness beyond the typical ‘baby blues’.
- Loss of Interest in Activities: No longer enjoying activities once found pleasurable.
- Changes in Appetite or Sleep: Significant changes in eating habits or sleep patterns, such as insomnia or oversleeping.
- Fatigue and Low Energy: Extreme tiredness and lack of energy, making even simple tasks challenging.
- Anxiety and Irritability: Feeling anxious, irritable, or easily agitated.
- Feelings of Worthlessness or Guilt: Negative thoughts about oneself and one’s ability to care for the baby.
- Difficulty Bonding with the Baby: Struggling to connect with the baby emotionally.
- Thoughts of Self-Harm or Harm to the Baby: This is a serious sign requiring immediate professional help.
If any of these symptoms persist for more than two weeks, it’s crucial to seek professional help immediately. Treatment options include therapy, medication, and support groups.
Q 7. Explain the different birthing positions.
Various birthing positions offer different benefits and can influence the labor process. The choice of position depends on several factors including individual preferences, medical considerations, and the stage of labor.
- Upright Positions: Standing, squatting, walking, or using a birthing ball. These positions can help gravity assist the baby’s descent, promote uterine contractions, and provide comfort to the mother.
- Semi-Recumbent Positions: Sitting up in bed, leaning against something, or using a side-lying position. These positions provide a more comfortable resting position during labor and allow for easier monitoring of the mother’s and baby’s vital signs.
- Hands and Knees Position: This position is often recommended for back labor, as it helps alleviate pressure and pain.
- Lateral Position (Side-lying): This position can be helpful during the later stages of labor, especially if an epidural is in place, allowing better blood circulation.
- Water Birth: Labor and delivery in a warm water bath can provide pain relief and relaxation.
Choosing a birthing position is a collaborative decision between the mother and her healthcare provider. It’s crucial to discuss various options and make an informed choice based on the mother’s needs and circumstances.
Q 8. Describe the benefits of skin-to-skin contact after birth.
Skin-to-skin contact, also known as kangaroo care, offers a multitude of benefits for both newborns and parents immediately after birth. It’s about placing the baby directly onto the parent’s bare chest, promoting a feeling of closeness and security.
- For the baby: Skin-to-skin contact helps regulate the baby’s temperature, heart rate, and blood sugar. It also aids in establishing healthy breathing patterns and promotes bonding. The baby benefits from the mother’s natural microbiome transfer, contributing to a healthy gut and immune system development. For premature babies, it’s especially crucial as it can improve oxygen saturation and reduce stress.
- For the parent: The release of oxytocin, the ‘love hormone,’ during skin-to-skin contact fosters a strong emotional bond between parent and child. It can also help with postpartum depression and anxiety by promoting feelings of calm and well-being. For mothers, it helps stimulate milk production and facilitates successful breastfeeding.
For instance, I’ve seen firsthand how anxious new mothers become immediately after delivery. Placing the baby on their chest, promoting skin-to-skin, visibly calms both mother and baby, leading to smoother breastfeeding initiation and a more relaxed transition to parenthood.
Q 9. How would you address a parent’s concerns about pain management during labor?
Addressing a parent’s concerns about pain management during labor requires a compassionate and informative approach. It’s crucial to acknowledge their fears and validate their feelings. Many women fear the intensity of labor pain, and it’s vital to empower them with knowledge and options.
I begin by explaining the various pain management techniques available, ensuring the parents understand the benefits and limitations of each. These options range from non-pharmacological methods (e.g., breathing techniques, massage, hydrotherapy, movement) to pharmacological interventions (e.g., epidurals, narcotics, nitrous oxide). I emphasize that the choice is entirely theirs and tailor recommendations to individual preferences, medical history, and risk factors. A collaborative approach, where the parent actively participates in decision-making, is paramount.
For example, a woman who fears medication might benefit from learning different breathing and relaxation techniques. Conversely, a woman with a high pain tolerance might opt for only minimal intervention. Open communication and respect for her autonomy are key to ensuring a positive birthing experience.
Q 10. What are the risks associated with premature birth?
Premature birth, defined as birth before 37 weeks of gestation, carries significant risks for the infant. The earlier the birth, the greater the potential for complications.
- Respiratory problems: Premature babies often lack fully developed lungs, leading to respiratory distress syndrome (RDS) and an increased risk of bronchopulmonary dysplasia (BPD).
- Brain and neurological issues: Premature babies are at higher risk of cerebral palsy, learning disabilities, and other neurological problems due to underdeveloped brain structures.
- Heart problems: Premature babies may have heart defects or irregularities.
- Feeding difficulties: They may struggle with sucking and swallowing, requiring special feeding techniques or assistance.
- Infection: Premature babies have a weaker immune system, making them vulnerable to infections.
- Gastrointestinal issues: They may experience feeding difficulties like necrotizing enterocolitis (NEC).
- Long-term developmental delays: Many premature babies require ongoing medical care and interventions, potentially facing developmental delays.
The severity of these risks depends largely on the gestational age at birth and the baby’s overall health. NICU (Neonatal Intensive Care Unit) care often becomes necessary, providing specialized medical support.
Q 11. How would you teach about infant sleep safety?
Teaching infant sleep safety is crucial for reducing the risk of Sudden Infant Death Syndrome (SIDS). I emphasize the ABCs of safe sleep: Alone, on their Back, in a Crib.
- Alone: The baby should always sleep alone, without toys, pillows, blankets, or bumpers in the crib. Sharing a bed with the parents significantly increases SIDS risk.
- On their Back: Babies should always be placed on their backs to sleep. Side or stomach sleeping increases the risk of suffocation.
- In a Crib: A firm, flat sleep surface is recommended. Avoid soft surfaces such as sofas, armchairs, or waterbeds.
Additionally, I advise parents to maintain a smoke-free environment, avoid overheating the baby, and ensure regular breastfeeding or bottle-feeding. Breastfeeding, particularly for the first six months, is linked to a reduced risk of SIDS. Finally, I encourage them to create a consistent sleep routine, facilitating better sleep patterns for the baby. Every prenatal class includes a thorough demonstration and discussion of safe sleep practices.
Q 12. What are the key components of a healthy prenatal diet?
A healthy prenatal diet is essential for the growth and development of the fetus and the mother’s well-being. It’s characterized by a balance of essential nutrients.
- Folic acid: Crucial for preventing neural tube defects. Sources include leafy greens, legumes, and fortified cereals.
- Iron: Prevents anemia in the mother and supports fetal development. Sources include red meat, spinach, lentils, and iron-fortified foods.
- Calcium: Essential for bone development in both mother and baby. Sources include dairy products, leafy greens, and fortified foods.
- Protein: Provides building blocks for fetal growth. Sources include lean meats, poultry, fish, beans, lentils, and eggs.
- Iodine: Supports thyroid function. Sources include iodized salt and seafood.
- Vitamin D: Important for bone health and immune function. Sources include fatty fish, egg yolks, and fortified foods.
- Omega-3 fatty acids: Support brain development. Sources include fatty fish and flaxseed.
I advise pregnant women to consume a variety of nutrient-rich foods from all food groups. Limiting processed foods, sugary drinks, and excessive caffeine intake is critical. Regular prenatal check-ups allow for monitoring of nutritional intake and addressing potential deficiencies.
Q 13. Discuss the importance of prenatal exercise.
Prenatal exercise offers numerous benefits for both mother and baby. It’s crucial to consult with a healthcare provider before starting any new exercise routine, especially during pregnancy.
- Improved cardiovascular health: Exercise strengthens the heart and improves blood circulation, benefitting both mother and fetus.
- Weight management: Helps manage weight gain within healthy limits during pregnancy.
- Reduced back pain and improved posture: Strengthening core muscles can alleviate common pregnancy-related discomforts.
- Improved mood and reduced stress: Physical activity releases endorphins, which can improve mood and reduce anxiety and depression.
- Increased energy levels: Regular exercise can boost energy levels, combating pregnancy-related fatigue.
- Shorter labor: Some studies suggest that regular exercise can lead to shorter labor times.
I recommend moderate-intensity activities like brisk walking, swimming, or prenatal yoga. It’s crucial to avoid strenuous exercises or activities with a high risk of falls. Listening to the body and resting when needed is paramount.
Q 14. Explain the various types of childbirth classes you’re familiar with.
I’m familiar with several types of childbirth classes designed to prepare expectant parents for labor, delivery, and the postpartum period. These classes differ in their focus and approach.
- Lamaze classes: These classes focus on relaxation techniques, breathing exercises, and pain management strategies based on the Lamaze philosophy, emphasizing the mother’s ability to cope with labor pain through conscious relaxation and controlled breathing.
- Bradley method classes: These classes emphasize natural childbirth with a focus on partner support and relaxation techniques. They often promote a holistic approach, integrating physical exercise, nutrition, and emotional preparation.
- Hypnobirthing classes: These classes use guided imagery and hypnosis to help the mother achieve deep relaxation during labor. The aim is to reduce pain perception through deep relaxation and self-hypnosis techniques.
- Infant care and breastfeeding classes: These classes provide education on newborn care, including diapering, bathing, feeding, and swaddling. They also cover breastfeeding techniques, latch, positioning, and common breastfeeding challenges.
- Sibling preparation classes: For families with older children, these classes help prepare siblings for the arrival of a new baby, addressing their potential concerns and feelings.
The choice of class often depends on personal preferences and birthing philosophy. I believe a combination of classes that include pain management, breastfeeding preparation, and newborn care is ideal, enabling parents to feel well-equipped for the journey ahead.
Q 15. How would you adapt your teaching style to different learning styles?
Effective prenatal education requires catering to diverse learning styles. My approach involves incorporating a variety of teaching methods to ensure all parents feel engaged and understood.
- Visual Learners: I utilize charts, diagrams, videos, and visual aids to illustrate complex concepts like fetal development or breastfeeding techniques. For example, I might use a 3D model of a fetus to show growth at different stages.
- Auditory Learners: I incorporate lectures, discussions, and group activities. I also encourage questions and provide opportunities for parents to verbally share their experiences and concerns. Podcasts on relevant topics would also be recommended.
- Kinesthetic Learners: I incorporate hands-on activities, like demonstrating baby massage techniques or practicing safe baby handling. Role-playing scenarios, such as practicing diaper changes, can be particularly helpful.
- Reading/Writing Learners: I provide detailed handouts, supplemental reading materials, and encourage note-taking during sessions. I’d offer printable checklists or summaries of key information.
By employing a multi-sensory approach, I aim to create an inclusive learning environment where every parent feels comfortable participating and absorbing information in their preferred way.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How would you handle a parent’s questions about a controversial topic like vaccination?
Vaccination is a sensitive topic, and my approach focuses on providing accurate, unbiased information and respecting parental autonomy.
I begin by acknowledging that it’s a deeply personal decision and creating a safe space for open dialogue. I then present evidence-based information from reputable sources like the CDC and WHO, emphasizing the proven benefits of vaccinations in preventing serious childhood illnesses. I explain the risks and benefits clearly, emphasizing that the risks associated with not vaccinating are often far greater than the rare side effects of vaccines. I avoid judgmental language and focus on empowering parents to make an informed decision. If a parent expresses strong reservations, I connect them with resources that offer diverse perspectives, emphasizing the importance of consulting with their pediatrician to develop a personalized vaccination plan.
It’s crucial to remember that I am not a medical professional and cannot give medical advice. My role is to equip parents with the information they need to make their own choices in partnership with their healthcare provider.
Q 17. Describe your experience working with diverse populations.
Throughout my career, I have worked with a diverse range of expectant parents from various cultural, socioeconomic, and ethnic backgrounds. This has enriched my understanding of the unique challenges and needs that families face.
For example, I’ve adapted my teaching style to accommodate language barriers by using visual aids and translators. I’ve also learned to be sensitive to cultural differences in parenting practices and beliefs about childbirth. I’ve worked with families experiencing financial hardship, ensuring the information is accessible and relevant to their circumstances. I’ve had opportunities to work with LGBTQ+ families, ensuring inclusive language and materials reflect the diversity of family structures. I always strive to create an environment where every parent feels respected, valued, and empowered, regardless of their background.
This experience has been invaluable in developing my cultural competence and has enabled me to tailor my approach to best meet the needs of each individual family.
Q 18. What resources would you recommend to expectant parents?
Expectant parents benefit from a variety of resources. I recommend a multi-faceted approach.
- Books and Articles: Evidence-based books and articles from reputable organizations such as the American Academy of Pediatrics or La Leche League International offer practical information on various aspects of pregnancy, childbirth, and newborn care. I always make sure to recommend materials that are up-to-date and accurate.
- Online Resources: Websites and apps from trusted sources can provide valuable information, but it is crucial to always validate information with a healthcare provider. I recommend only using credible sources.
- Classes and Workshops: Prenatal classes cover a range of topics from childbirth education to newborn care and breastfeeding. I guide them to reputable organizations offering these courses.
- Support Groups: Connecting with other expectant parents provides emotional support and a sense of community. Online and in-person support groups are highly recommended.
- Healthcare Providers: Regular visits with their obstetrician or midwife are crucial for monitoring the health of the mother and baby. I stress the importance of building a strong relationship with their medical team.
By combining these resources, parents can gain a comprehensive understanding of pregnancy and parenthood, enhancing their preparedness and confidence.
Q 19. How would you address a conflict between the parents-to-be regarding birth preferences?
Conflicts regarding birth preferences are common, and it’s essential to guide couples towards a mutually agreeable plan.
My approach involves facilitating open and respectful communication. I begin by creating a safe and non-judgmental space for both parents to express their desires and concerns without interruption. I use active listening techniques to ensure each partner feels heard and understood. Then, I help them explore their reasons for their preferences, identifying potential compromises or alternatives.
For instance, if one parent desires a natural birth while the other prefers an epidural, I guide them in discussing the pros and cons of each approach, emphasizing the importance of shared decision-making. I help them research different pain management options and explore strategies for incorporating elements from both preferences into a plan that works for both of them. Ultimately, the goal is to empower the couple to make a joint decision that reflects their shared values and priorities.
Q 20. What is your understanding of the role of a doula?
A doula provides continuous physical, emotional, and informational support to a person before, during, and just after childbirth. They are not medical professionals but offer crucial non-medical support.
Doulas provide education and evidence-based information about childbirth options and pain management techniques. They offer emotional support to both the birthing person and their partner, helping to reduce stress and anxiety. They provide physical comfort measures like massage, counter-pressure, and positioning techniques. They also advocate for the birthing person’s wishes and preferences within the medical setting.
Essentially, a doula acts as a continuous source of support and empowerment, helping to create a more positive and personalized birth experience. I often recommend doula services as a valuable addition to prenatal education and preparation for childbirth.
Q 21. What are the signs of potential complications during pregnancy?
Recognizing potential complications during pregnancy is vital for ensuring maternal and fetal well-being.
- Severe Headaches or Vision Changes: These could indicate pre-eclampsia, a serious condition characterized by high blood pressure.
- Sudden Swelling in the Face, Hands, or Feet: This, combined with high blood pressure, is another warning sign of pre-eclampsia.
- Vaginal Bleeding: Bleeding at any point during pregnancy should be reported immediately as it could indicate placental problems or other complications.
- Severe Abdominal Pain: Pain could signify preterm labor, placental abruption, or other serious issues.
- Decreased Fetal Movement: A significant reduction in fetal movement might indicate fetal distress.
- High Fever: A high fever could indicate infection.
- Persistent Vomiting: Excessive vomiting could lead to dehydration and malnutrition.
It is crucial to stress that this is not an exhaustive list, and any concerning symptoms warrant immediate medical attention. I emphasize the importance of regular prenatal checkups and open communication with healthcare providers to ensure prompt identification and management of potential complications.
Q 22. How would you explain the importance of regular prenatal checkups?
Regular prenatal checkups are crucial for ensuring a healthy pregnancy and delivery for both the mother and baby. These visits aren’t just about monitoring weight gain; they’re a comprehensive assessment of the mother’s overall well-being and the baby’s development.
- Early detection of complications: Regular checkups allow healthcare providers to identify potential problems like gestational diabetes, preeclampsia (high blood pressure during pregnancy), or infections early on, when treatment is most effective. For example, early detection of gestational diabetes allows for dietary and lifestyle modifications, or medication if needed, to manage blood sugar levels and prevent complications for both mother and baby.
- Monitoring fetal growth and development: Ultrasound scans and other assessments during these visits track the baby’s growth, ensuring it’s developing as expected. If any developmental concerns arise, intervention can be implemented promptly.
- Addressing maternal health concerns: Prenatal care addresses the mother’s overall health, including blood pressure, weight, and nutritional status. It also provides an opportunity to address any existing health conditions or concerns, such as managing chronic illnesses like asthma or hypertension.
- Education and support: Checkups offer valuable opportunities for education on topics such as nutrition, exercise, labor and delivery, and newborn care. The consistent support of a healthcare provider helps alleviate anxiety and empowers expectant parents to make informed decisions.
In short, regular prenatal checkups are an investment in a healthy pregnancy and a healthy baby. They provide proactive care, early intervention, and invaluable support for expectant parents throughout their journey.
Q 23. Describe your experience with developing and delivering educational materials.
I have extensive experience creating and delivering engaging prenatal education materials. My approach prioritizes evidence-based information presented in an accessible and relatable manner.
- Development: I’ve developed comprehensive curriculum for childbirth education classes, including interactive workshops, presentations using visual aids like videos and infographics, and handouts summarizing key information. I also tailor my materials to suit different learning styles and cultural contexts. For example, one class I developed incorporated interactive games and role-playing exercises to help parents practice coping techniques for labor.
- Delivery: My delivery style is characterized by a combination of informative lectures, interactive discussions, practical demonstrations (such as babywearing techniques), and Q&A sessions. I create a safe space for open communication and encourage participation from all attendees. This includes acknowledging differing experiences and perspectives among the expectant parents.
- Formats: I’ve worked with a variety of formats, including in-person classes, online webinars, and downloadable resources. This ensures wider reach and accessibility for expectant parents who may have different preferences or logistical constraints.
My goal is always to empower parents with the knowledge and skills they need to navigate pregnancy, childbirth, and the postpartum period with confidence. I regularly solicit feedback to ensure the materials remain relevant, engaging, and effective.
Q 24. How do you stay updated on the latest research and best practices in prenatal care?
Staying current in prenatal care requires a multi-faceted approach. I regularly engage with various resources to ensure I’m delivering the most up-to-date and evidence-based information.
- Professional organizations: I’m a member of [mention relevant professional organizations, e.g., American College of Nurse-Midwives, Association of Prenatal and Perinatal Psychology and Health]. These memberships provide access to journals, conferences, and continuing education opportunities, keeping me abreast of the latest research findings and clinical guidelines.
- Peer-reviewed journals: I actively read peer-reviewed journals such as the American Journal of Obstetrics and Gynecology and other reputable publications to stay informed about new research on pregnancy, childbirth, and postpartum care.
- Conferences and workshops: Attending conferences and workshops allows me to network with other professionals in the field, learn about innovative practices, and engage in discussions on emerging trends.
- Continuing education courses: I consistently participate in continuing education courses to maintain and enhance my expertise. These courses often cover topics such as new techniques in childbirth education, advancements in fetal monitoring, and addressing specific maternal health concerns.
This commitment to lifelong learning is vital in this constantly evolving field, ensuring I provide the highest quality education and support to expectant parents.
Q 25. What strategies do you use to build rapport with expectant parents?
Building rapport with expectant parents is crucial for creating a supportive and trusting environment. I utilize several strategies to achieve this.
- Active listening: I pay close attention to their concerns, questions, and anxieties, demonstrating empathy and understanding. This involves not interrupting, summarizing their points to ensure accurate understanding, and responding with genuine care.
- Creating a safe space: I foster a non-judgmental and inclusive environment where parents feel comfortable sharing their experiences, even if they are challenging or unconventional. I emphasize the diversity of birthing experiences and avoid imposing my own personal opinions or beliefs.
- Respecting individual preferences: I honor parents’ choices regarding their birth plans, respecting their autonomy and acknowledging that they are the ultimate decision-makers. I offer information and guidance, but avoid imposing my recommendations.
- Empathy and validation: I acknowledge the emotional and physical changes expectant parents are undergoing, validating their feelings and providing support. A simple gesture like acknowledging the stress of pregnancy or the excitement of anticipating the arrival of a baby can go a long way.
- Humor and approachability: I use appropriate humor and maintain a friendly, approachable demeanor to create a relaxed and comfortable atmosphere. Sharing personal anecdotes (where appropriate) can help build connection.
By focusing on empathy, respect, and open communication, I aim to build strong, trusting relationships with expectant parents, creating a positive learning environment.
Q 26. How would you handle a situation where a parent is experiencing anxiety about childbirth?
Anxiety about childbirth is extremely common. My approach focuses on understanding the source of the anxiety and providing evidence-based coping strategies.
- Validate their feelings: First, I acknowledge and validate their feelings, emphasizing that anxiety is a normal response to the significant life change of childbirth. I avoid minimizing or dismissing their concerns.
- Identify the source of anxiety: Through open-ended questions, I help them pinpoint the specific aspects of childbirth that are causing them anxiety. This could be fear of pain, complications, or the unknown.
- Provide education and information: I offer accurate information about labor and delivery, dispelling myths and providing realistic expectations. For example, I might explain different pain management techniques and the likelihood of various complications.
- Teach coping mechanisms: I teach evidence-based coping mechanisms, such as relaxation techniques (e.g., deep breathing, progressive muscle relaxation), visualization, and mindfulness. I also introduce them to resources like hypnobirthing or other evidence based birthing techniques.
- Connect them with support: If necessary, I connect them with other resources like a therapist or support groups specializing in perinatal mental health.
Ultimately, the goal is to empower them with knowledge and skills to manage their anxiety and approach childbirth with greater confidence and self-efficacy.
Q 27. How would you teach about safe babywearing?
Teaching safe babywearing involves both theoretical knowledge and practical demonstration. My approach combines both.
- T.I.C.K.S. guideline: I begin by introducing the T.I.C.K.S. guideline, a widely accepted mnemonic for safe babywearing: Tight—the wrap or carrier should be snug enough that you can only fit two fingers between the carrier and your baby’s back; In view at all times—keep your baby close enough to kiss; Close enough to kiss—the baby’s chin should be up and not tucked into their chest; Keep baby’s back straight—the baby should be in a natural, upright position; Secure—the wrap or carrier should be properly adjusted and fastened securely.
- Different carrier types: I demonstrate various babywearing options, such as slings, wraps, structured carriers, and mei tais. I explain the pros and cons of each, considering factors like ease of use, adjustability, and suitability for different stages of infant development.
- Proper positioning and fitting: I provide hands-on instruction on proper fitting and positioning to ensure the baby is securely and ergonomically supported. I emphasize the importance of proper positioning to avoid hip dysplasia and other potential issues.
- Safety precautions: I discuss safety precautions, including avoiding activities that might compromise the baby’s safety (such as strenuous exercise or activities that might cause the baby to fall) and the importance of careful selection of a safe carrier from reputable manufacturers.
- Practice and Q&A: I encourage parents to practice babywearing with supervision and offer a Q&A session to address any questions or concerns they may have.
By combining theoretical knowledge with practical demonstrations and emphasizing safety precautions, I aim to empower parents to use babywearing safely and confidently.
Q 28. What are your strengths and weaknesses as a prenatal educator?
As a prenatal educator, my strengths lie in my ability to connect with expectant parents on a personal level, fostering a safe and supportive environment.
- Strengths: Strong communication skills, empathy, active listening, ability to create engaging educational materials, adaptability to various teaching formats, and a deep understanding of evidence-based practices in prenatal and postnatal care. I’m also very organized and adept at managing my time effectively.
- Weaknesses: While I strive for perfection, sometimes I need to remind myself that it’s okay to delegate tasks. Overly cautious and sometimes takes on too much responsibility. I’m also working on becoming even more fluent in incorporating technological innovations into my teaching methods. I’m actively addressing this by attending relevant workshops and webinars.
I’m committed to continuous improvement and actively seek feedback to identify areas for growth and development. I believe in self-reflection and continuous professional development as essential aspects of maintaining my expertise in this field.
Key Topics to Learn for Prenatal Education Interview
- Physical Changes During Pregnancy: Understanding the physiological changes a woman experiences throughout pregnancy, including hormonal shifts, weight gain, and bodily adaptations. Consider practical applications like explaining these changes to expectant parents in an accessible way.
- Fetal Development: Comprehensive knowledge of fetal growth and development, week by week, including milestones and potential complications. Be prepared to discuss how this knowledge informs prenatal care strategies and patient education.
- Nutrition During Pregnancy: Mastering the nutritional needs of pregnant women, including essential vitamins, minerals, and dietary recommendations. Practice explaining the importance of healthy eating habits and addressing common nutritional concerns.
- Prenatal Exercise and Wellness: Familiarize yourself with safe and effective exercise routines during pregnancy, as well as strategies for promoting overall well-being and stress management. Be ready to discuss the benefits and limitations of different exercise approaches.
- Common Pregnancy Concerns and Complications: Develop a thorough understanding of common pregnancy-related issues like morning sickness, gestational diabetes, and preeclampsia, including early detection and management strategies. Practice explaining these complexities to clients in a reassuring manner.
- Childbirth Education and Preparation: Gain knowledge of different childbirth methods, pain management techniques, and postpartum care. Consider how to tailor educational materials to diverse client needs and preferences.
- Postpartum Care and Support: Understand the physical and emotional changes women experience postpartum and the resources available for support. Be prepared to discuss the importance of breastfeeding, postpartum depression, and newborn care.
- Communication and Counseling Skills: Develop strong interpersonal skills to effectively communicate complex medical information, provide emotional support, and build rapport with expectant parents. Consider how to handle challenging conversations and emotional situations.
- Ethical Considerations in Prenatal Care: Understand the ethical dilemmas that may arise in prenatal education, such as informed consent, patient autonomy, and confidentiality. Be ready to discuss these issues with a nuanced understanding.
Next Steps
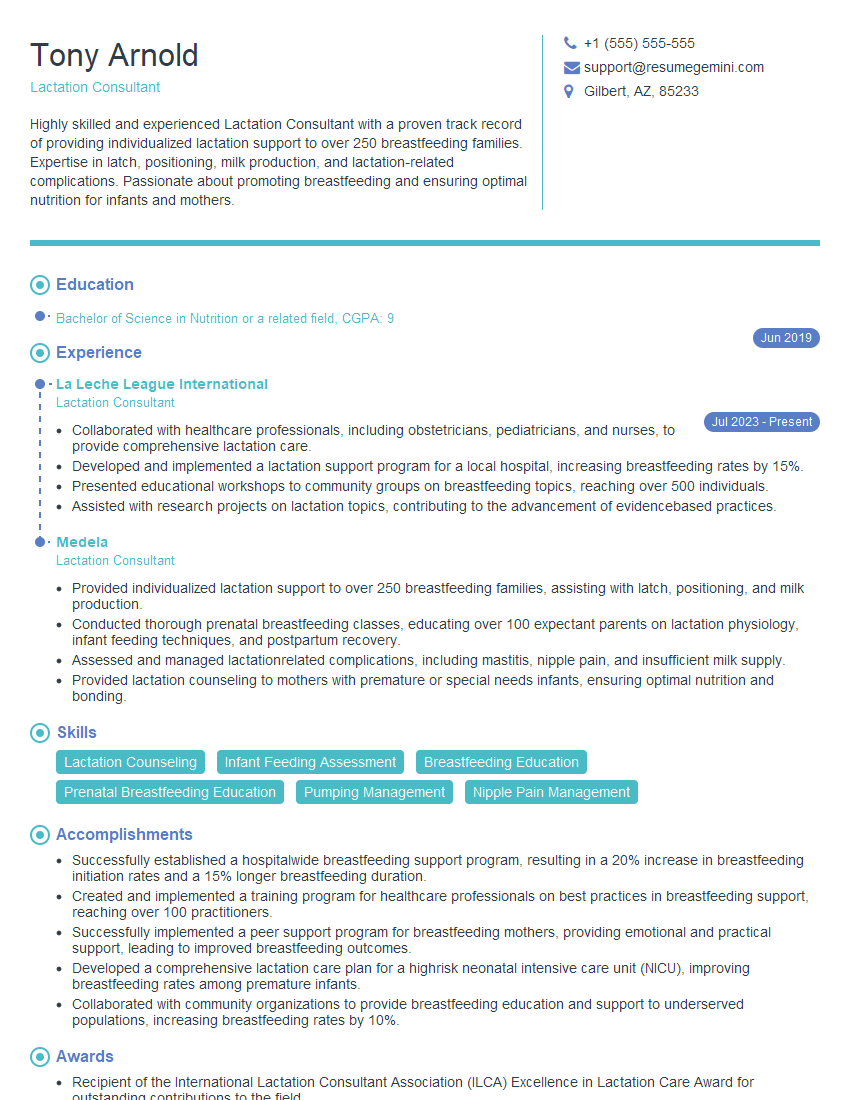
Mastering Prenatal Education opens doors to a rewarding career helping expectant parents navigate this incredible journey. To significantly increase your job prospects, crafting a strong, ATS-friendly resume is crucial. ResumeGemini is a trusted resource to help you build a professional and impactful resume that highlights your skills and experience. Examples of resumes tailored specifically to Prenatal Education are available to guide you. Invest time in creating a compelling resume – it’s your first impression and a key to unlocking your career goals.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO