Interviews are more than just a Q&A session—they’re a chance to prove your worth. This blog dives into essential Newborn Care interview questions and expert tips to help you align your answers with what hiring managers are looking for. Start preparing to shine!
Questions Asked in Newborn Care Interview
Q 1. Describe the APGAR scoring system and its significance.
The APGAR score is a quick assessment of a newborn’s physical condition done at 1 and 5 minutes after birth. It helps determine how well the baby is adapting to life outside the womb. The score is based on five parameters, each rated 0, 1, or 2, for a total score ranging from 0 to 10.
- Appearance (Skin color): 0 – Blue or pale all over; 1 – Body pink, extremities blue; 2 – Pink all over
- Pulse (Heart rate): 0 – Absent; 1 – Below 100 bpm; 2 – Above 100 bpm
- Grimace (Reflex irritability): 0 – No response; 1 – Grimace; 2 – Cough or sneeze
- Activity (Muscle tone): 0 – Limp; 1 – Some flexion; 2 – Active motion
- Respiration (Breathing): 0 – Absent; 1 – Slow, irregular; 2 – Good, crying
A score of 7-10 indicates a healthy baby, while a score below 7 suggests the need for immediate medical attention. For instance, a baby with a low APGAR score might require resuscitation or extra monitoring. The APGAR score is a vital tool for immediate newborn assessment and guides early interventions.
Q 2. Explain the proper procedure for measuring an infant’s temperature.
Measuring an infant’s temperature accurately is crucial to detect fever or hypothermia. The most reliable method is using a digital thermometer placed in the axillary (armpit) area.
- Preparation: Gather a digital thermometer and ensure it’s clean.
- Positioning: Gently place the baby on their back and carefully place the thermometer tip under the armpit, ensuring good skin contact.
- Measurement: Hold the baby’s arm securely against their body to ensure the thermometer stays in place. Follow the thermometer’s instructions for reading the temperature.
- Interpretation: A normal axillary temperature ranges from 36.5°C to 37.5°C (97.7°F to 99.5°F). Any temperature outside this range should be reported immediately to a healthcare professional.
Axillary temperature is preferred because it’s less invasive and less likely to cause discomfort compared to rectal measurements. Remember to always follow aseptic techniques and monitor the baby’s reaction. In cases where axillary temperature is difficult, a temporal artery thermometer can be a viable alternative.
Q 3. What are the signs of newborn jaundice, and what actions should be taken?
Newborn jaundice is a yellowish discoloration of the skin and whites of the eyes caused by an excess of bilirubin, a byproduct of red blood cell breakdown. It’s common in newborns, but excessive jaundice requires attention.
- Signs: Yellowing of the skin, especially noticeable on the face, sclera (whites of the eyes), and palms/soles of the feet. The yellowing typically starts on the face and spreads downward.
Actions to take:
- Immediate medical consultation: If jaundice appears within the first 24 hours of life, or if the yellowing is intense or spreading rapidly, seek immediate medical attention.
- Phototherapy: This treatment involves placing the baby under special lights to help break down bilirubin.
- Exchange transfusion: In severe cases, an exchange transfusion may be necessary to remove bilirubin from the baby’s blood.
- Regular monitoring: Even if jaundice is considered physiological (mild and resolves within a few weeks), regular monitoring by a healthcare professional is essential.
Early detection and intervention are crucial to prevent potential complications associated with high bilirubin levels. A simple blood test can measure bilirubin levels and guide treatment decisions.
Q 4. How would you assess a newborn’s respiratory rate and what is considered normal?
Assessing a newborn’s respiratory rate involves observing the rise and fall of their chest for one full minute. It’s best done while the baby is sleeping or resting quietly to obtain an accurate count.
Procedure: Observe the baby’s chest movements for one minute. Each rise and fall of the chest constitutes one breath.
Normal respiratory rate: A normal respiratory rate in newborns ranges from 30 to 60 breaths per minute. Anything outside this range, especially abnormally rapid or slow breathing, requires immediate medical evaluation.
Example: If you count 45 breaths in a minute, this falls within the normal range. However, if you observe gasping breaths, labored breathing, or rates significantly above or below this range, immediate medical attention is crucial.
Q 5. What are the key signs of newborn hypothermia and hyperthermia?
Maintaining a stable temperature is vital for newborn health. Both hypothermia (low body temperature) and hyperthermia (high body temperature) pose serious risks.
Hypothermia (Low Body Temperature):
- Signs: Cool skin to the touch, lethargy (low energy), poor feeding, weak cry, mottled skin (blotchy appearance), and possibly a low axillary temperature (<36.5°C or 97.7°F).
Hyperthermia (High Body Temperature):
- Signs: Hot skin to the touch, excessive sweating, lethargy, rapid breathing, and possibly a high axillary temperature (>37.5°C or 99.5°F).
Immediate Action: Both hypothermia and hyperthermia require prompt intervention. Hypothermia often requires warming measures such as skin-to-skin contact, warm blankets, or an incubator. Hyperthermia may require cooling measures, such as removing excess clothing and providing a cool environment. Always consult a medical professional for accurate diagnosis and treatment.
Q 6. Explain the different types of newborn feeding methods (breastfeeding, bottle-feeding).
Newborn feeding involves two primary methods: breastfeeding and bottle-feeding.
Breastfeeding: This involves feeding the baby directly from the mother’s breast. Breast milk provides optimal nutrition and immunity for the newborn. It is recommended exclusively for the first six months of life.
- Benefits: Contains ideal nutrients, promotes bonding, provides passive immunity, and reduces the risk of several illnesses.
Bottle-feeding: This method involves feeding the baby with formula milk using a bottle and nipple. Formula milk is designed to mimic the composition of breast milk.
- Benefits: Provides nutrition when breastfeeding is not possible or chosen. It allows for shared feeding responsibilities.
- Considerations: Requires careful preparation to avoid contamination. The type of formula should be carefully selected based on the baby’s needs.
Both methods require proper hygiene, appropriate feeding techniques and monitoring the baby’s weight gain and growth to ensure adequate nutrition. Consulting with lactation specialists or healthcare professionals can provide guidance and support for optimal feeding practices.
Q 7. Describe the signs of successful breastfeeding and latch.
Successful breastfeeding and latch are crucial for effective feeding and infant growth. Here’s how to identify a good latch:
- Signs of a good latch: The baby’s mouth covers a significant portion of the areola (the dark area around the nipple), not just the nipple itself. The baby’s chin touches the breast. You should hear swallowing sounds during feeding. The baby’s cheeks are rounded, and they appear relaxed and comfortable.
- Signs of successful breastfeeding: The baby is feeding for a satisfactory duration (around 10-15 minutes per breast, often varying), gains weight appropriately, has regular bowel movements (usually after each feed initially), and appears content and satisfied after feedings. The mother’s breasts feel softer after feeding, indicating milk removal.
Troubleshooting: If the baby is struggling to latch or is not feeding effectively, seek help from a lactation consultant or healthcare professional. They can assess the latch, advise on positioning, and address any underlying issues.
Q 8. What are the signs of dehydration in a newborn?
Dehydration in newborns is a serious concern, as they lose fluids rapidly. Recognizing the signs early is crucial. Look for these key indicators:
- Sunken fontanelles: The soft spots on the baby’s head will appear sunken.
- Dry mouth and tongue: A lack of saliva will make the mouth and tongue look dry and sticky.
- Decreased wet diapers: Fewer wet diapers than usual, signifying reduced urine output, is a major warning sign. A newborn should have at least 6-8 wet diapers per day.
- No tears when crying: This is a clear indicator of dehydration.
- Lethargy and irritability: A dehydrated baby will be less active and more irritable than usual. They may also appear listless or floppy.
- Sunken eyes: The eyes may appear slightly sunken into the sockets.
If you notice any of these signs, immediately contact your pediatrician. Dehydration can quickly become life-threatening for a newborn.
Q 9. How would you address umbilical cord care?
Umbilical cord care is essential to prevent infection. Here’s the proper approach:
- Keep it clean and dry: Gently clean the area around the cord with warm water and a soft cloth once or twice a day. Avoid using alcohol or any harsh antiseptic unless specifically instructed by your doctor.
- Fold diaper below the cord: Ensure the diaper doesn’t rub against the cord, allowing for proper air circulation.
- Observe for signs of infection: Watch for redness, swelling, pus, or a foul odor. These are signs of infection and require immediate medical attention.
- The cord will fall off naturally: Usually within 10-21 days. Do not try to pull it off.
- Once it falls off, continue hygiene: Keep the area clean and dry until it is fully healed. If there is bleeding after the cord falls off, apply gentle pressure with a clean gauze pad.
Proper umbilical cord care is vital in preventing serious complications. If in doubt, always consult your healthcare provider.
Q 10. What are the common newborn skin conditions and their treatment?
Newborns are prone to various skin conditions. Here are some common ones:
- Cradle cap (Seborrheic dermatitis): This is a scaly, flaky condition on the scalp. Treatment involves gentle cleansing with a mild shampoo and occasionally using a small amount of mineral oil to soften the scales.
- Diaper rash: Caused by prolonged exposure to wet or soiled diapers. Treatment focuses on frequent diaper changes, barrier creams (like zinc oxide), and allowing the skin to air dry.
- Milia: These are tiny white bumps commonly seen on the face. They are harmless and usually disappear within a few weeks. Avoid squeezing or picking them.
- Erythema toxicum neonatorum: This rash, characterized by small red bumps with white or yellow centers, is common and usually disappears without treatment within a few days.
- Acne neonatorum: Newborn acne often appears on the face and resolves on its own within weeks or months.
If a rash persists, worsens, or seems unusual, consult a pediatrician. Proper identification and treatment are essential for preventing complications.
Q 11. Explain the importance of swaddling and safe sleep practices.
Swaddling and safe sleep practices are crucial for a newborn’s well-being and safety. Swaddling, wrapping a baby snugly in a blanket, mimics the feeling of being held, promoting calmness and reducing the startle reflex. This can lead to longer sleep periods. However, it’s crucial to follow safe swaddling practices:
- Use a lightweight blanket: Avoid overheating.
- Arms should be swaddled at the side: Do not swaddle the arms above the baby’s head.
- Ensure the baby can’t wiggle free: Check that the swaddle is snug but not restrictive. The baby should be able to move their legs freely.
- Stop swaddling once the baby shows signs of rolling: Swaddling can increase the risk of Sudden Infant Death Syndrome (SIDS) once the baby can roll over.
Safe sleep practices also include:
- Place the baby on their back to sleep: Always place the baby on their back on a firm surface, free from loose blankets, pillows, bumpers, or toys.
- Room-sharing, not bed-sharing: Keep the baby in the same room as you for at least the first six months, but not in the same bed.
- Breastfeeding: It has been linked to reduced SIDS risk.
- Immunizations: Regular immunizations provide important protection against various illnesses.
Following these guidelines significantly reduces the risk of SIDS and promotes healthy sleep habits.
Q 12. How would you recognize and respond to signs of newborn respiratory distress?
Newborn respiratory distress is a serious condition requiring immediate medical attention. Signs include:
- Rapid breathing (tachypnea): More than 60 breaths per minute.
- Grunting: A baby makes grunting sounds during exhalation, trying to keep the lungs open.
- Nasal flaring: The nostrils widen with each breath.
- Retractions: The skin between the ribs or below the ribs may sink in with each breath.
- Cyanosis (bluish discoloration): This is particularly noticeable around the mouth and lips.
- Wheezing or gasping: Unusual breathing sounds.
Response: If you observe any of these signs, immediately seek medical help. Do not attempt to treat it yourself. Early intervention is vital in preventing serious complications.
Q 13. What are the vital signs to monitor in a newborn?
Regular monitoring of vital signs is essential for a newborn’s well-being. These include:
- Heart rate: Normally 120-160 beats per minute (bpm). This can fluctuate with activity and sleep.
- Respiratory rate: Normally 30-60 breaths per minute.
- Temperature: Maintaining a stable temperature between 97.7°F (36.5°C) and 99.5°F (37.5°C) is crucial.
- Blood pressure: Monitored regularly, especially if there are any concerns.
- Oxygen saturation (SpO2): Measures the percentage of oxygen in the blood. A reading below 95% usually indicates a need for intervention.
The specific frequency of monitoring depends on the baby’s health status and any existing conditions. Always follow the guidelines provided by your healthcare provider.
Q 14. How do you assess for potential developmental delays in a newborn?
Assessing for potential developmental delays in newborns is an ongoing process that begins at birth and continues throughout infancy. While a definitive diagnosis often requires time and observation, certain red flags can signal the need for further evaluation:
- Poor head control: Inability to hold the head up at 3 months of age.
- Lack of response to sounds or light: A newborn should generally respond to stimuli by turning their head or eyes.
- Difficulty feeding or sucking: Persistent problems with latching or sucking can be a concern.
- Limited eye contact: Infants typically begin engaging in prolonged eye contact.
- Persistent irritability or unusual fussiness: While some fussiness is normal, excessive and persistent irritability could signal a problem.
- Absent milestones: Failure to achieve typical developmental milestones such as rolling over, sitting up, or crawling within a reasonable timeframe.
These are just potential signs and do not necessarily indicate a delay. Regular checkups with a pediatrician are essential for monitoring the baby’s development. Early intervention is crucial if delays are detected. A developmental specialist can provide a thorough assessment and develop appropriate interventions.
Q 15. Describe the procedure for administering medication to a newborn.
Administering medication to a newborn is a critical procedure requiring precision and safety. It’s crucial to follow strict protocols to minimize risks. First, always verify the doctor’s orders against the medication’s label – three times! This ensures the correct medication, dosage, and route of administration. Second, accurately calculate the dose based on the baby’s weight. Newborns’ dosages are often significantly smaller than adult dosages and a simple miscalculation can have serious consequences. Third, gather all necessary supplies: medication, syringe (appropriate size for the dosage), clean wipes, and possibly a pacifier if the baby is fussy. Fourth, gently position the baby. For oral medications, use a syringe to slowly administer the medicine to the inside of the cheek, allowing the baby to swallow at their own pace. Avoid squirting it directly into the throat to prevent choking. For injections, the procedure should only be performed by trained medical professionals following established protocols for intramuscular or subcutaneous administration. Always document the medication, dosage, time, and route of administration meticulously in the baby’s medical record.
Example: Let’s say a newborn needs 0.5ml of medication. You’d carefully draw 0.5ml into the syringe, check it again against the order, and slowly administer it to the baby’s cheek, allowing them to swallow gradually. Post-administration, you would observe the baby for any adverse reactions like rash, vomiting, or respiratory distress.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain the importance of newborn hearing screenings.
Newborn hearing screenings are incredibly important because early detection of hearing loss allows for timely intervention, significantly improving a child’s developmental trajectory. Untreated hearing loss can lead to delays in speech, language, and cognitive development. These delays can have lasting impacts on a child’s educational and social life. The screening itself is quick and painless; it usually involves placing small sensors in the baby’s ear to measure the response to various sounds. There are two main types of screenings: auditory brainstem response (ABR) and otoacoustic emissions (OAE). ABR measures brainwave activity in response to sound, while OAE tests the inner ear’s ability to produce sound. If a screening identifies a potential problem, further testing is conducted to confirm the diagnosis and determine the type and extent of hearing loss.
Practical Application: Early intervention, such as hearing aids or cochlear implants, can significantly enhance a child’s ability to hear and develop language skills, minimizing the long-term consequences of hearing impairment. This early intervention can make a profound difference in a child’s quality of life.
Q 17. What are the signs of newborn infection?
Recognizing the signs of newborn infection is crucial for prompt medical attention. Infections can range from mild to life-threatening, so it’s essential to be vigilant. Signs can vary depending on the type of infection, but some common indicators include:
- Temperature instability: Fever (rectal temperature above 38°C or 100.4°F) or hypothermia (low body temperature).
- Lethargy or irritability: The baby may be unusually sleepy or difficult to console.
- Poor feeding: The baby may be feeding poorly or refusing to feed altogether.
- Vomiting or diarrhea: These symptoms indicate a potential gastrointestinal infection.
- Jaundice: Yellowing of the skin and whites of the eyes.
- Respiratory distress: Rapid breathing, grunting, or nasal flaring.
- Rash: A rash may appear on the skin.
- Discharge from the eyes or nose: This could indicate a localized infection.
Important Note: Any of these signs should prompt immediate medical attention. Early diagnosis and treatment significantly increase the chances of a positive outcome.
Q 18. How do you handle a situation where a newborn is exhibiting signs of distress?
Responding to a distressed newborn requires a calm, swift, and systematic approach. First, assess the baby’s ABCs (Airway, Breathing, Circulation). Check for airway obstruction (check mouth and nose for any blockage). Observe their breathing rate and depth. If the breathing is shallow or rapid, or if there are pauses, you may need to assist with breathing. Assess the baby’s heart rate; a weak or absent pulse requires immediate action. Second, identify the cause of distress. Is the baby hungry, cold, uncomfortable, in pain, or exhibiting signs of illness? Third, provide appropriate intervention based on the cause. If hungry, offer a feeding. If cold, wrap the baby warmly. If in pain, provide comfort measures like skin-to-skin contact or swaddling. If exhibiting signs of illness, seek immediate medical attention. Fourth, monitor the baby’s response to the intervention. Continue to observe their vital signs and overall condition. If the distress doesn’t resolve, seek further medical help immediately.
Example: If a baby is crying inconsolably, try feeding, changing the diaper, and offering comfort measures. If the crying persists or the baby displays other signs of distress like rapid breathing or bluish discoloration of the skin, seek immediate medical attention.
Q 19. What are the common newborn reflexes and their significance?
Newborn reflexes are involuntary movements that are present at birth and typically disappear within the first few months of life. These reflexes are important indicators of neurological development. Some common reflexes include:
- Rooting reflex: When you stroke the baby’s cheek, they turn their head towards the touch and open their mouth, preparing to latch on for feeding.
- Sucking reflex: When something touches the roof of the baby’s mouth, they automatically begin to suck.
- Grasp reflex: When you place your finger in the baby’s palm, they will grasp it tightly.
- Moro reflex (startle reflex): When the baby is startled by a loud noise or sudden movement, they will extend their arms and legs outwards and then bring them back in, as if embracing.
- Stepping reflex: When held upright with their feet touching a surface, the baby will move their legs as if attempting to walk.
- Babinski reflex: When the sole of the foot is stroked, the baby’s toes will fan out.
Significance: The presence and strength of these reflexes help assess the integrity of the baby’s nervous system. Absence or abnormalities in these reflexes could indicate potential neurological problems requiring further evaluation.
Q 20. Describe the process for preventing and managing diaper rash.
Diaper rash is a common problem in newborns, but it’s largely preventable and manageable. Prevention is key! The cornerstone is frequent diaper changes, ideally as soon as the diaper becomes wet or soiled. This minimizes skin contact with urine and feces, both irritants. Gentle cleansing with warm water or a mild, fragrance-free cleanser is crucial; avoid harsh soaps. Thorough drying of the skin, patting gently, is important to prevent moisture buildup. Applying a barrier cream, like petroleum jelly or zinc oxide ointment, creates a protective layer to prevent further irritation. Exposure to air can also help the skin heal; allow the baby some diaper-free time in a safe environment. If a rash develops despite these measures, it’s vital to treat it effectively. Mild cases may respond well to continued diligent hygiene, barrier creams, and air exposure. For more severe rashes, consult a pediatrician who might recommend antifungal or corticosteroid creams.
Example: A parent can implement a routine of changing the baby’s diaper every 2-3 hours, cleaning the area gently with water, applying a barrier cream after each change, and ensuring the baby has some diaper-free time every day.
Q 21. What are the differences between breast milk and formula?
Breast milk and formula offer different nutritional compositions and benefits for newborns. Breast milk is considered the gold standard due to its unique blend of nutrients and antibodies perfectly tailored to the infant’s needs. It contains antibodies that protect the baby from infections, digestive enzymes aiding nutrient absorption, and live cells promoting gut health. It adapts over time to the baby’s changing needs, providing a perfect balance of nutrients as the baby grows. Formula, while a suitable alternative, attempts to mimic breast milk but lacks the dynamic composition and the immunological benefits. Formulations vary, but generally, they provide adequate protein, carbohydrates, and fats needed for infant growth and development. The choice between breast milk and formula is often a personal decision, guided by medical advice and the mother’s circumstances.
Key Differences Summarized:
- Antibodies & Immunological factors: Breast milk is rich in antibodies and factors boosting the immune system, something formula cannot completely replicate.
- Digestibility: Breast milk is easier to digest than formula, often leading to fewer digestive issues in babies.
- Live Cells & Nutrients: Breast milk contains live cells and bioactive components that promote gut health and development that are not found in formula.
- Cost: Breastfeeding is typically less expensive than using formula.
Ultimately, the best choice should be made in consultation with a healthcare professional to ensure the baby’s optimal nutrition and health.
Q 22. How would you respond to a parent who is struggling with breastfeeding?
Breastfeeding challenges are incredibly common, and I approach each situation with empathy and a problem-solving mindset. My first step is to listen carefully to the parent’s concerns, understanding their specific struggles – is it latch difficulties, milk supply issues, pain, or something else?
I’d then conduct a thorough assessment, observing the baby’s latch, assessing the mother’s breast anatomy, and checking for any signs of tongue-tie or other anatomical issues. I utilize various techniques to improve latch, including positioning guidance (e.g., football hold, cradle hold), and skin-to-skin contact to encourage bonding and milk release.
For milk supply concerns, I might suggest strategies like increasing nursing frequency, ensuring adequate hydration and nutrition, and possibly recommending galactagogues (herbs or medications to increase milk production), always in consultation with a physician. Pain management is crucial; I’d advise on proper latch techniques, nipple shields if necessary, and recommend pain relievers only when medically appropriate. Finally, I offer ongoing support and regular follow-ups, perhaps connecting them with a lactation consultant for specialized guidance.
For example, I recently worked with a mother who experienced significant nipple pain. By carefully assessing her latch, we found that the baby wasn’t fully opening their mouth, causing friction and pain. Adjusting the baby’s position and guiding the mother on correct latch techniques resolved the issue within a week.
Q 23. Explain the safety protocols for handling newborns.
Newborn safety is paramount. Hand hygiene is the cornerstone of our protocol – thorough handwashing with soap and water or using an alcohol-based hand rub before and after handling each baby is mandatory.
We maintain a warm, stable environment, ensuring the baby is appropriately dressed and protected from drafts or extreme temperatures. Safe sleep practices are strictly adhered to: babies should always be placed on their backs on a firm, flat surface without loose bedding, toys, or bumpers.
Identification protocols are crucial to prevent mix-ups; we use unique identifiers (e.g., wristbands) throughout their stay. We carefully monitor vital signs (heart rate, respiratory rate, temperature) regularly, and any concerning changes trigger immediate intervention.
Infection control measures include rigorous cleaning and sterilization of equipment and surfaces. We carefully monitor for signs of infection (e.g., fever, lethargy, poor feeding) and promptly isolate newborns suspected of having an infectious disease. We also educate parents on proper hygiene practices for themselves and their baby.
Q 24. What are the risks associated with premature babies?
Premature babies face a heightened risk of various complications due to their underdeveloped organ systems. Respiratory distress syndrome (RDS) is a significant concern, as their lungs may lack surfactant, a crucial substance for proper breathing. This can lead to respiratory failure requiring mechanical ventilation.
- Respiratory Problems: RDS, bronchopulmonary dysplasia (BPD), apnea (periods of stopped breathing).
- Brain Problems: Intraventricular hemorrhage (bleeding in the brain), periventricular leukomalacia (damage to white matter in the brain), necrotizing enterocolitis (NEC).
- Heart Problems: Patent ductus arteriosus (PDA), a condition where a blood vessel connecting the aorta and pulmonary artery fails to close after birth.
- Infection: Premature babies have weaker immune systems, making them vulnerable to infections.
- Feeding Difficulties: Difficulty sucking, swallowing, and digesting, often requiring feeding tubes or specialized formulas.
- Temperature Regulation Problems: They struggle to regulate their body temperature, requiring specialized incubators or warmers.
The severity of these risks depends on the degree of prematurity. The earlier the baby is born, the greater the risk of complications.
Q 25. Describe your experience with newborn resuscitation.
I have extensive experience in newborn resuscitation, having participated in numerous successful resuscitations. My training includes the Neonatal Resuscitation Program (NRP), and I am proficient in the use of various resuscitation equipment, including bag-valve masks, endotracheal tubes, and suction devices.
My approach follows the NRP guidelines, focusing on a systematic assessment and intervention. This includes immediately establishing airway patency, providing positive pressure ventilation if necessary, and performing chest compressions if the heart rate remains low. I’m meticulous about monitoring the newborn’s response to interventions and adapting my approach based on their response. Documentation is crucial, recording every step taken during the resuscitation process.
For example, I once successfully resuscitated a newborn who was born with severe respiratory distress. Quick action, including immediate bag-valve mask ventilation and subsequent intubation, ensured the baby’s survival and subsequent healthy development.
Q 26. What is your experience with different types of infant monitors?
My experience encompasses various types of infant monitors, including pulse oximeters (to monitor oxygen saturation), cardiorespiratory monitors (to monitor heart rate and breathing), and apnea monitors (to detect periods of stopped breathing). I am familiar with both bedside and remote monitoring systems.
I understand the limitations and potential issues associated with each type. For example, pulse oximeters can be affected by factors such as poor perfusion, while apnea monitors can generate false alarms. I know how to troubleshoot these issues and interpret the data accurately.
My knowledge extends to the proper placement and maintenance of these devices, ensuring they provide reliable data. I also educate parents about the use and limitations of these monitors, empowering them to participate in their baby’s care.
Q 27. How do you handle a crying infant?
A crying infant requires a calm and systematic approach. First, I’d assess the baby’s condition, checking for signs of hunger, discomfort (diaper change, clothing adjustment), illness (fever, lethargy), or overstimulation.
If the baby is hungry, I would offer a feeding. If a diaper change is needed, I’d ensure it is done promptly and efficiently. If the baby is overstimulated, I might try creating a calmer environment, reducing noise and light.
If the cause remains unclear, I would implement strategies such as swaddling, gentle rocking, or skin-to-skin contact. If the crying persists or worsens, I would consult with a physician to rule out any underlying medical conditions.
It is important to remember that parental intuition plays a critical role in soothing their baby, and I would encourage the parents’ active participation in comforting their infant.
For instance, I once dealt with a baby who cried inconsolably for several hours. After ruling out medical issues, we realized the baby was suffering from colic. By gently rocking and swaying the baby while employing white noise, we were able to soothe the baby and allow the parents some much-needed rest.
Q 28. Describe your knowledge of common newborn vaccinations.
My knowledge of common newborn vaccinations aligns with current recommendations from the Centers for Disease Control and Prevention (CDC) and the American Academy of Pediatrics (AAP).
I am well-versed in the schedule and administration techniques for vaccines such as HepB, rotavirus, DTaP, Hib, PCV13, IPV, and influenza (if appropriate for the season). I understand the purpose of each vaccine, potential side effects, and the importance of completing the vaccination series for optimal protection against various infectious diseases.
I always provide parents with thorough information about each vaccine, addressing their concerns and answering their questions honestly and transparently. I would explain potential side effects, emphasizing that these are usually mild and temporary, and would encourage parents to contact us with any concerns. Obtaining informed consent before administering any vaccine is a critical step in our process.
Key Topics to Learn for Newborn Care Interview
- Infant Physiological Needs: Understanding newborn vital signs (heart rate, respiration, temperature), feeding cues, and sleep patterns. Practical application: Recognizing signs of distress and implementing appropriate interventions.
- Safe Sleep Practices: Knowledge of safe sleep environments (e.g., back sleeping, firm surface, no loose bedding) and Sudden Infant Death Syndrome (SIDS) risk reduction strategies. Practical application: Educating parents on safe sleep guidelines and identifying potential hazards.
- Feeding and Nutrition: Breastfeeding support, bottle-feeding techniques, recognizing feeding difficulties, and nutritional needs of newborns. Practical application: Assisting parents with latch, positioning, and addressing common feeding challenges.
- Infant Hygiene and Skin Care: Diapering techniques, umbilical cord care, bathing, and addressing common skin issues (e.g., diaper rash). Practical application: Demonstrating proper hygiene practices and identifying signs of infection or irritation.
- Infant Development and Milestones: Understanding typical newborn development (motor skills, reflexes, sensory development), recognizing developmental delays, and appropriate stimulation techniques. Practical application: Assessing a newborn’s development and providing age-appropriate activities.
- Recognizing and Responding to Emergencies: CPR and first aid for infants, recognizing signs of illness or injury, and appropriate emergency response procedures. Practical application: Knowing when and how to seek immediate medical attention.
- Parent Education and Support: Effective communication with parents, providing emotional support, and fostering a positive and collaborative relationship. Practical application: Answering parent questions, addressing concerns, and providing reassurance.
- Infection Control and Prevention: Understanding and implementing infection control protocols to protect both the infant and caregivers. Practical application: Maintaining a clean and sterile environment and practicing proper hand hygiene.
Next Steps
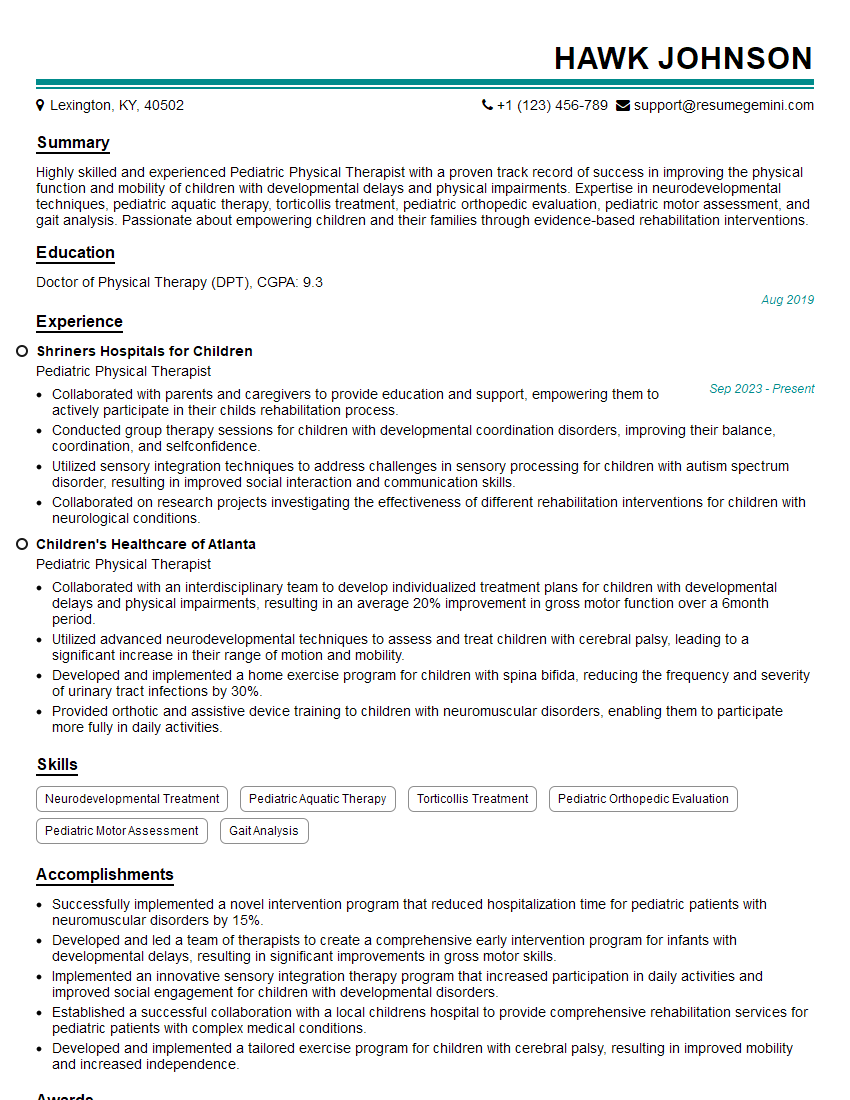
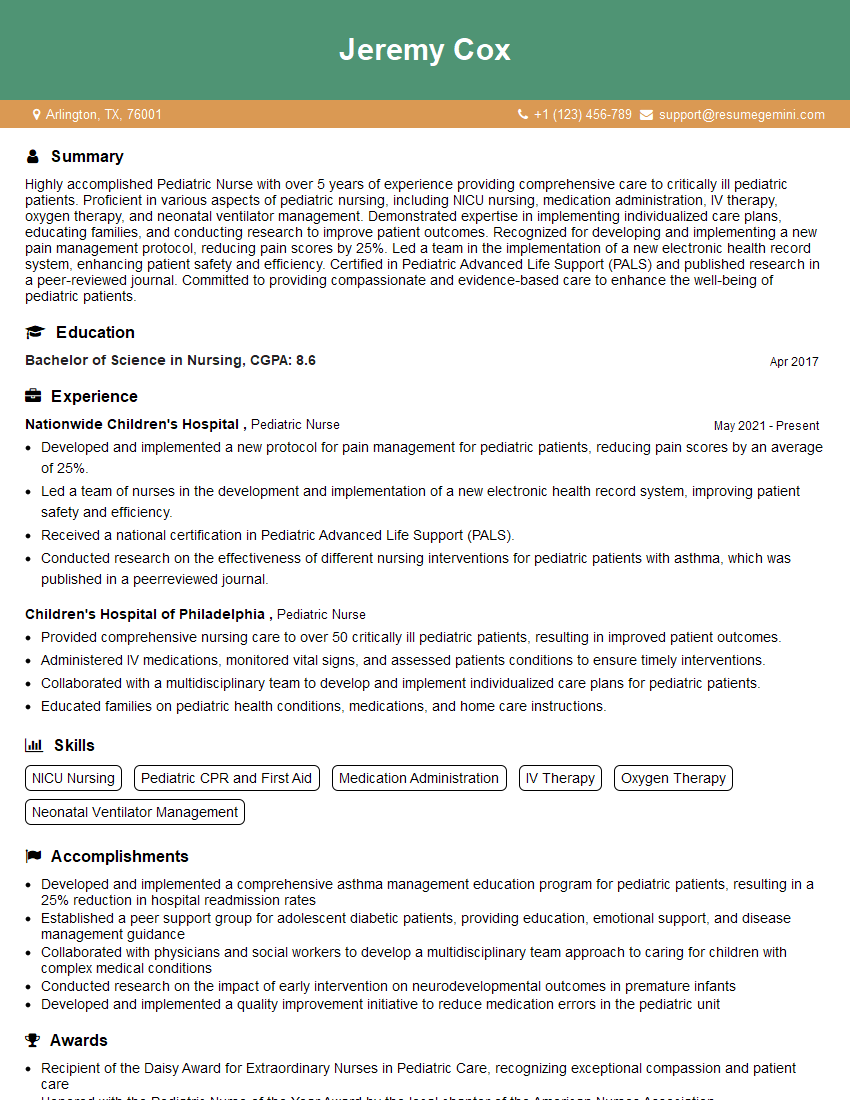
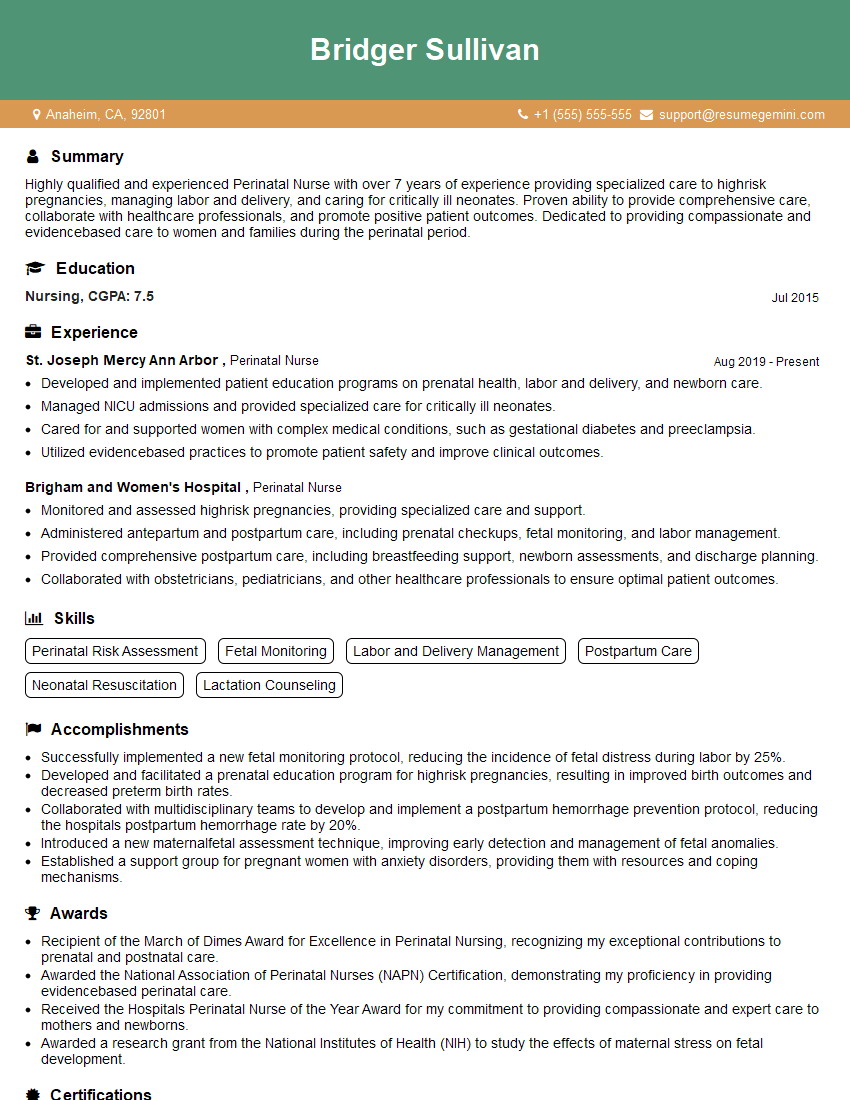
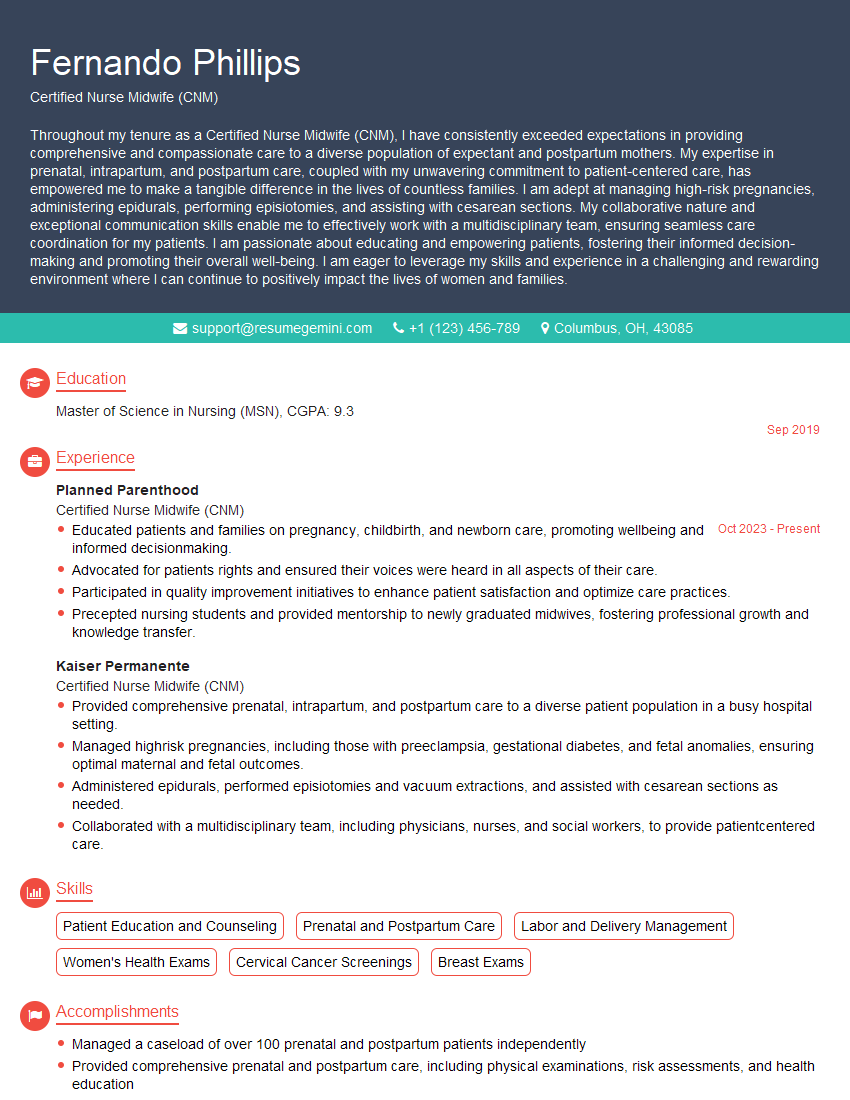
Mastering newborn care is crucial for a rewarding and impactful career. A strong foundation in these key areas will significantly enhance your interview performance and open doors to exciting opportunities. To maximize your job prospects, focus on crafting an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource for building professional resumes, and we provide examples tailored to the Newborn Care field to help you showcase your qualifications. This will help you stand out to potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO