Interviews are more than just a Q&A session—they’re a chance to prove your worth. This blog dives into essential First Response Procedures interview questions and expert tips to help you align your answers with what hiring managers are looking for. Start preparing to shine!
Questions Asked in First Response Procedures Interview
Q 1. Describe the steps you would take upon arriving at a scene of a motor vehicle accident.
Arriving at a motor vehicle accident scene requires a systematic approach prioritizing safety and patient care. My first step would always be to ensure my own safety and the safety of others at the scene. This involves surveying the area for hazards like downed power lines, leaking fuel, or further potential vehicle movement. I would then activate emergency services if not already done (or provide further details to dispatch if I am the first responder).
- Scene Size-Up: A quick assessment of the overall situation, including the number of vehicles, apparent injuries, and environmental hazards.
- Establish Safety Zone: Using warning lights and cones to create a safe perimeter around the accident to prevent further incidents.
- Initial Patient Assessment: Approaching the victims cautiously, checking for responsiveness and signs of life. Prioritizing immediate life threats such as airway obstruction, severe bleeding, or shock.
- Requesting Assistance: Calling for additional resources such as ambulances, fire services, and law enforcement as needed, providing precise location and the number of patients.
- Patient Care: Initiating basic life support, such as CPR or controlling bleeding, until more advanced medical personnel arrive. Maintaining patient dignity and privacy.
For example, I once responded to an accident where a car had flipped over. Before approaching the vehicle, I ensured the area was safe, securing the scene with warning cones. Then, I confirmed the patient’s responsiveness and immediately addressed a significant leg injury before calling for additional support.
Q 2. Explain the importance of scene safety in first response procedures.
Scene safety is paramount in first response. It’s the foundation upon which all other interventions are built. Without a safe environment, responders risk becoming casualties themselves, hindering effective patient care and potentially worsening the situation. Scene safety measures protect not just first responders but also victims, bystanders, and even the environment itself.
- Protecting Responders: Prevents injuries to first responders from secondary collisions, fire, hazardous materials, or other dangers.
- Protecting Victims: Minimizes the risk of further injury to patients by controlling traffic, stabilizing vehicles, and preventing bystander interference.
- Protecting Bystanders: Keeps onlookers from entering the hazardous zone, preventing them from becoming casualties.
- Preserving Evidence: Careful scene management helps maintain the integrity of the scene for investigation purposes.
Imagine a car accident with a fuel leak. If responders aren’t cautious, a spark could ignite a fire. Scene safety procedures—establishing a safe zone, using appropriate protective gear, and calling specialized hazmat teams—are crucial to prevent such scenarios.
Q 3. How do you prioritize multiple casualties in a mass casualty incident?
In a mass casualty incident (MCI), efficient triage is crucial to maximize survival rates. We utilize a triage system, often the START (Simple Triage And Rapid Treatment) method, to quickly categorize patients based on their immediate needs. This involves systematically assessing patients and assigning them to one of four categories: Immediate, Delayed, Minimal, or Expectant.
- Immediate: Patients with life-threatening injuries requiring immediate attention (e.g., airway obstruction, severe bleeding).
- Delayed: Patients with serious injuries but not immediately life-threatening (e.g., fractures, major burns).
- Minimal: Patients with minor injuries who can wait for treatment (e.g., abrasions, minor lacerations).
- Expectant: Patients with injuries so severe that survival is unlikely, even with immediate intervention.
The START method prioritizes those who have the highest chance of survival with immediate intervention. This ensures resources are allocated effectively, maximizing the number of lives saved. In practice, it’s a fast-paced, high-pressure situation demanding quick thinking and efficient teamwork.
Q 4. What are the key elements of a thorough patient assessment?
A thorough patient assessment is a systematic process of gathering information about a patient’s condition to guide treatment. It’s often broken down into the components of the ABCDEs (Airway, Breathing, Circulation, Disability, Exposure).
- Airway: Assessing for patency (openness) and ensuring a clear airway.
- Breathing: Checking respiratory rate, depth, and effort; observing for signs of respiratory distress.
- Circulation: Assessing heart rate, blood pressure, and capillary refill; checking for signs of shock or bleeding.
- Disability: Evaluating neurological status by checking level of consciousness, pupil response, and motor function.
- Exposure: Carefully removing clothing to examine the patient’s entire body for injuries; maintaining patient warmth and privacy.
Beyond the ABCDEs, a comprehensive assessment includes taking a history (SAMPLE – Symptoms, Allergies, Medications, Past Medical History, Last Meal, Events leading to injury) and performing a focused physical exam based on the initial findings. This information allows for an accurate diagnosis and the appropriate treatment plan.
Q 5. Describe your experience with CPR and AED usage.
I am certified in both CPR (Cardiopulmonary Resuscitation) and AED (Automated External Defibrillator) usage. My training includes adult, child, and infant CPR techniques, as well as the proper application of an AED. I regularly participate in refresher courses to maintain my skills and proficiency. I have extensive experience performing CPR and using AEDs in various scenarios, including simulated drills and real-life emergencies.
In a practical setting, I follow a structured approach, adhering to the current guidelines. For example, when using an AED, I ensure the device is properly turned on, the pads are correctly placed, and I follow the voice prompts to deliver a shock only when indicated. Maintaining composure under pressure during such an event is as critical as the procedural steps themselves.
Q 6. Explain the differences between stable and unstable patients.
The difference between stable and unstable patients lies in their physiological status and the potential for their condition to deteriorate rapidly.
- Stable Patient: A patient whose vital signs are within normal limits, and their condition is not expected to worsen significantly in the immediate future. They are alert and oriented, breathing comfortably, and their circulation is strong.
- Unstable Patient: A patient whose vital signs are abnormal, and their condition may worsen rapidly. They might be unconscious or confused, experiencing respiratory distress, showing signs of shock, or have uncontrolled bleeding.
Think of it like this: a stable patient is like a car running smoothly, while an unstable patient is like a car with a failing engine—immediate attention is required to prevent a complete breakdown.
Q 7. How would you handle a patient who is refusing medical treatment?
Handling a patient refusing medical treatment requires a delicate balance of respecting their autonomy while ensuring their safety. My approach would involve:
- Clear Communication: Understanding their reasons for refusal through calm and empathetic conversation. Establishing rapport and addressing any concerns.
- Explaining Risks: Clearly explaining the potential risks and consequences of refusing treatment, using non-judgmental language.
- Documenting Everything: Meticulously documenting the conversation, including the patient’s statements, any concerns, and the explanation of risks. Witnessing the refusal is also important.
- Offering Alternatives: If appropriate, exploring alternative treatment options that align with the patient’s wishes.
- Seeking Assistance: Involving a supervisor or a social worker if the patient remains adamant despite the risks and explanations.
- Legal Considerations: Being aware of the legal and ethical implications of respecting patient autonomy even in situations where refusal could have serious consequences.
It’s important to remember that a competent adult has the right to refuse medical treatment, even if that decision seems unwise. Our role is to provide information and support, respecting their choice within the boundaries of the law and ethical practice.
Q 8. Describe your understanding of the START triage system.
The START triage system (Simple Triage And Rapid Treatment) is a rapid assessment method used in mass casualty incidents (MCIs) to prioritize victims based on their immediate need for medical attention. It’s designed to be quick and efficient, allowing first responders to quickly identify and treat the most critically injured individuals first. The system categorizes patients into four priority categories: Immediate, Delayed, Minimal, and Expectant.
- Immediate: These patients require immediate life-saving intervention. Think airway obstruction, uncontrolled bleeding, or shock.
- Delayed: These individuals have injuries that require medical attention, but it can be delayed. Examples include stable fractures or less severe burns.
- Minimal: These patients have minor injuries and can typically wait for treatment. Think minor lacerations or bruises.
- Expectant: Sadly, these patients have injuries so severe that they are unlikely to survive, even with immediate medical intervention. This category prioritizes resource allocation to those with a higher chance of survival.
Imagine a bus accident with multiple casualties. START triage helps responders quickly assess each person—checking respiration, perfusion, and mental status—to sort them into these categories, ensuring the most critically injured get help first.
Q 9. What is your experience with managing various types of bleeding?
Managing various types of bleeding is crucial in first response. My experience encompasses addressing arterial, venous, and capillary bleeds. The approach depends entirely on the type and severity of the bleeding.
- Capillary bleeding: This is the most common type, usually characterized by oozing. Direct pressure with a clean dressing usually suffices.
- Venous bleeding: This is characterized by a dark red, steady flow of blood. Again, direct pressure is key, but sometimes elevation of the injured limb can assist.
- Arterial bleeding: This is the most dangerous type. Blood is bright red and spurts with each heartbeat. Immediate, direct pressure is crucial. Tourniquets are often necessary to control this type of bleeding, but should only be applied as a last resort and by trained personnel.
In my experience, proper training and the use of appropriate equipment (like tourniquets and pressure dressings) are crucial. I’ve dealt with scenarios from minor cuts and scrapes to severe trauma involving significant blood loss. Maintaining a calm demeanor while applying techniques effectively is critical to patient care.
Q 10. How do you communicate effectively during a crisis situation?
Effective communication during a crisis is paramount. It involves clear, concise messaging, active listening, and adapting to the situation. My approach involves:
- Clear and Concise Language: Avoid jargon. Use simple, direct language easily understood by everyone involved, regardless of their background.
- Active Listening: Listen carefully to what others are saying and confirm understanding to avoid miscommunication.
- Use of Standard Operating Procedures (SOPs): Following established procedures ensures consistent and efficient communication among team members.
- Appropriate Technology: Utilizing radios, phones, and other communication tools effectively and understanding their limitations.
- Maintaining Calm: Projecting calm helps diffuse anxiety and facilitates clearer communication amongst everyone.
For example, during a building fire, I would use clear radio communication to relay critical information—location of victims, severity of injuries, and resource needs—to dispatch and other responders, while simultaneously providing reassurance to victims.
Q 11. Explain your understanding of incident command systems.
Incident Command Systems (ICS) provide a standardized, on-scene, management structure for coordinating emergency response. It’s a flexible, adaptable system that ensures effective control and coordination of multiple agencies and personnel during emergencies. ICS uses a hierarchical structure with clearly defined roles and responsibilities.
- Incident Commander: Overall leader, responsible for all aspects of the incident.
- Operations Section Chief: Manages the tactical operations to control the incident.
- Planning Section Chief: Gathers and analyzes information, develops strategies.
- Logistics Section Chief: Manages resources, supplies, and equipment.
- Finance/Administration Section Chief: Manages financial and administrative aspects of the response.
ICS is crucial for efficient resource allocation, effective communication, and overall successful management of any incident, large or small. I’ve worked within ICS structures in various exercises and real-world scenarios, understanding the importance of each role and the seamless integration of teams.
Q 12. How would you handle a situation involving a hazardous material spill?
Handling a hazardous material spill involves a multi-step process prioritizing safety. The first step is always to ensure the safety of myself and others. This includes establishing a perimeter to prevent further exposure and evacuating the area.
- Identify the Material: If possible, identify the hazardous material using placards, shipping papers, or other available information.
- Assess the Situation: Determine the extent of the spill, its potential dangers, and the affected area.
- Contact Emergency Services: Notify appropriate authorities immediately, providing them with all relevant information.
- Establish a Perimeter: Create a safety zone around the spill, restricting access to prevent further exposure.
- Utilize Appropriate PPE: Wear appropriate personal protective equipment based on the identified hazardous material.
- Contain the Spill: If possible and safe to do so, attempt to contain the spill to prevent further spread.
- Decontamination: Establish a decontamination zone to remove any hazardous materials from affected individuals and equipment.
This process requires proper training, familiarity with different hazardous materials, and adherence to established safety protocols. Prioritizing safety and proper communication is paramount in this type of emergency.
Q 13. Describe your experience with using personal protective equipment (PPE).
Experience with personal protective equipment (PPE) is essential for first responders. My experience includes using various types of PPE, such as gloves, eye protection, respirators, and protective suits, depending on the nature of the hazard.
- Gloves: Nitrile gloves are commonly used for general protection, while specialized gloves are required for hazardous materials.
- Eye Protection: Safety glasses or goggles protect the eyes from splashes or impact.
- Respirators: These are critical for protection from airborne hazards and are selected based on the specific contaminant.
- Protective Suits: These provide full-body protection from hazardous materials, varying in level of protection.
Proper donning and doffing (putting on and taking off) procedures are critical to prevent contamination. I’ve undergone extensive training in the proper use and selection of PPE, ensuring my safety and the safety of others during emergency responses.
Q 14. What is your experience with documentation and reporting in emergency situations?
Accurate and thorough documentation and reporting are critical after any emergency situation. This ensures accountability, facilitates learning from experiences, and supports future planning and improvements.
- Incident Reports: Detailed accounts of the incident, including timelines, actions taken, and outcomes.
- Patient Care Records: Documentation of patient assessments, treatments, and transportation information.
- Equipment Logs: Tracking the use and maintenance of equipment.
- Photographs and Videos: Visual records of the scene and any injuries or damage.
My experience includes creating comprehensive reports, accurately recording patient information, and adhering to all relevant reporting guidelines. This ensures the information is easily accessible, legally sound, and beneficial for all involved parties.
Q 15. How do you manage stress and maintain composure in high-pressure environments?
Managing stress and composure in high-pressure situations is paramount in first response. It’s not about eliminating stress, but about developing coping mechanisms to function effectively under duress. My approach is multifaceted:
- Preemptive Stress Management: This includes maintaining a healthy lifestyle – regular exercise, sufficient sleep, and a balanced diet. It also involves proactive mental health strategies like mindfulness or meditation to build resilience.
- Controlled Breathing Techniques: In the heat of the moment, deep, slow breaths can significantly reduce heart rate and anxiety. I practice diaphragmatic breathing regularly.
- Situational Awareness: Maintaining focus on the immediate task at hand, prioritizing actions based on the patient’s needs, and avoiding distractions helps me stay centered.
- Teamwork and Communication: Effective communication with my team reduces individual pressure. Clearly delegating tasks and requesting support when needed prevents feeling overwhelmed.
- Post-Incident Debriefing: Critical after every major incident, debriefing allows processing emotions, identifying areas for improvement, and preventing burnout.
For example, during a multi-vehicle accident, the scene was chaotic. By focusing on the most critically injured patient first and clearly communicating with my team, we effectively stabilized multiple casualties without losing composure.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your understanding of medical ethics and legal considerations in first response.
Medical ethics and legal considerations are intertwined and fundamental to first response. Ethical practice centers on patient autonomy, beneficence (acting in the patient’s best interest), non-maleficence (avoiding harm), and justice (fair and equitable treatment). Legally, we must adhere to informed consent, patient confidentiality (HIPAA), and proper documentation. Failure to do so can lead to serious consequences.
For instance, treating a patient without their consent, even if it seems life-saving, is both unethical and illegal. Similarly, breaching patient confidentiality or improperly documenting actions can result in malpractice lawsuits or disciplinary actions. Maintaining detailed, accurate records and obtaining proper consent are crucial for ethical and legal compliance.
Q 17. How do you work effectively as part of a team in an emergency response setting?
Effective teamwork is crucial in emergency response. It’s built on clear communication, mutual respect, and understanding each team member’s role. I prioritize:
- Active Listening: Attentively listening to the team, understanding their perspectives, and incorporating their expertise into decision-making.
- Clear Communication: Using concise and precise language, avoiding jargon, and actively confirming understanding to prevent misinterpretations.
- Delegation: Assigning tasks based on individual skills and abilities to optimize efficiency and utilize everyone’s strengths.
- Leadership and Followership: Adapting my role as needed, providing direction when necessary and readily following instructions from senior responders.
- Conflict Resolution: Addressing conflicts constructively, focusing on problem-solving, and maintaining a respectful atmosphere.
During a building fire, efficient teamwork allowed us to quickly assess the situation, locate and extract the victims, and coordinate with other emergency services seamlessly.
Q 18. Describe a time you had to make a critical decision under pressure.
During a severe storm, a car accident occurred with a driver trapped inside a submerged vehicle. Making a quick decision was crucial due to the rapidly rising water levels. I had to assess the situation, weighing the risks of immediate extraction against the potential for further injury if we acted too hastily.
After quickly assessing the patient’s condition and the structural integrity of the vehicle, I decided to prioritize immediate extraction despite the risks of causing additional spinal injuries. My team and I worked quickly and efficiently, successfully rescuing the patient before the vehicle was completely submerged. Post-incident, while the extraction was successful, a review of the techniques used highlighted areas for improvement in how we manage such high-risk extractions.
Q 19. How do you adapt your approach to different types of emergencies?
Adaptability is key in emergency response. My approach varies significantly depending on the type of emergency. For example:
- Trauma: Focus is on stabilizing the patient, controlling bleeding, and addressing life-threatening injuries, rapidly assessing the mechanism of injury to guide treatment.
- Cardiac Arrest: Immediate CPR, defibrillation, and advanced life support are paramount; teamwork and speed are critical.
- Medical Emergencies (e.g., stroke, diabetic emergency): Assessment involves focusing on symptoms, recognizing specific signs, and administering appropriate treatments.
- Hazardous Material Incidents: Emphasis shifts to scene safety, understanding the nature of the hazard, and utilizing specialized equipment and procedures.
The core principle remains prioritizing patient safety and well-being while adapting actions to the specific needs of the situation.
Q 20. Explain your understanding of different types of shock.
Shock is a life-threatening condition where the body isn’t getting enough blood flow. Different types of shock have various causes but share common symptoms like low blood pressure, rapid pulse, and altered mental status. These include:
- Hypovolemic Shock: Caused by significant blood loss (e.g., severe bleeding).
- Cardiogenic Shock: The heart’s inability to pump enough blood (e.g., heart attack).
- Obstructive Shock: Blocked blood flow (e.g., pulmonary embolism).
- Distributive Shock: Blood vessels dilate excessively, reducing blood pressure (e.g., septic shock, anaphylactic shock).
Recognizing the type of shock is crucial for effective treatment. For example, treating hypovolemic shock involves fluid resuscitation while cardiogenic shock might require medication to support heart function.
Q 21. How would you handle a situation involving an unresponsive patient?
Handling an unresponsive patient requires a systematic approach:
- Assess the scene for safety: Ensure the area is safe for both the patient and responders.
- Check for responsiveness: Tap the patient’s shoulder and shout, ‘Are you okay?’
- Activate the emergency response system (911): Immediately call for backup.
- Check for breathing and pulse: Assess for breathing and a carotid pulse.
- Initiate CPR if necessary: Begin chest compressions and rescue breaths if the patient isn’t breathing or has no pulse.
- Use an AED if available: Follow the AED prompts to analyze the heart rhythm and deliver a shock if necessary.
- Continue CPR until advanced medical help arrives: Maintain CPR until relieved by paramedics or EMTs.
Following this protocol ensures the patient receives immediate and appropriate care, maximizing their chances of survival.
Q 22. Describe your experience with spinal immobilization techniques.
Spinal immobilization is a critical procedure in first response, aiming to prevent further injury to the spinal cord following a trauma. It involves carefully stabilizing the head, neck, and spine to minimize movement. My experience encompasses various techniques, from manual stabilization using cervical collars and long backboards to the use of vacuum mattresses and Kendrick extrication devices.
For instance, I’ve had to manually stabilize a patient with suspected cervical spine injury after a motor vehicle accident, using a rigid cervical collar and ensuring proper alignment before securing them to a long backboard. The process requires a methodical approach, starting with a thorough assessment of the patient’s condition, followed by gentle handling and proper alignment. Incorrect technique can exacerbate the injury, so ongoing training is essential. I also have experience using vacuum mattresses, which conform to the patient’s body, providing a more comfortable and secure immobilization, particularly useful in situations with suspected spinal injuries coupled with other injuries requiring careful handling.
The choice of immobilization technique depends on several factors, including the mechanism of injury, the patient’s presentation, and the available resources. It’s crucial to always prioritize patient safety and follow established protocols.
Q 23. How do you recognize and respond to signs of a stroke?
Recognizing a stroke is crucial for timely intervention. The acronym FAST is a widely used and effective tool: Facial drooping, Arm weakness, Speech difficulty, and Time to call emergency services. Facial drooping might involve one side of the face being unable to form a smile symmetrically. Arm weakness could manifest as difficulty raising one arm. Speech difficulty can range from slurred speech to complete inability to speak. The ‘Time’ element emphasizes the urgency; every minute counts in stroke treatment.
My response involves immediately calling for emergency medical services (EMS). While waiting for EMS, I would closely monitor the patient’s vital signs, maintain their airway, and provide reassurance. I would also document the onset time of symptoms as accurately as possible, as this information is crucial for medical professionals.
I remember one case where a patient presented with sudden slurred speech and weakness on one side of their body. By utilizing the FAST mnemonic, I quickly recognized the signs of a stroke and immediately contacted EMS. Their swift arrival and subsequent treatment proved vital in minimizing long-term effects. This experience highlighted the importance of rapid recognition and action in stroke management.
Q 24. Explain your understanding of oxygen administration techniques.
Oxygen administration is a life-saving intervention for patients experiencing respiratory distress or hypoxia. I’m proficient in using various oxygen delivery devices, including nasal cannulae, simple face masks, non-rebreather masks, and bag-valve masks (BVMs).
A nasal cannula provides low flow oxygen, ideal for mild respiratory issues. Simple face masks deliver higher flow rates. Non-rebreather masks provide the highest oxygen concentration achievable without intubation. The BVM is used in emergency situations where the patient is not breathing adequately, providing positive pressure ventilation. Accurate oxygen flow rates are monitored using a flow meter, ensuring the patient receives the appropriate level of oxygen supplementation.
For example, I’ve utilized a non-rebreather mask on a patient experiencing shortness of breath following a severe asthma attack, achieving a significant improvement in their respiratory status. Proper assessment of the patient’s condition and selecting the appropriate oxygen delivery device are essential for effective and safe oxygen administration. Moreover, I am trained to monitor for signs of oxygen toxicity and complications.
Q 25. Describe your experience with using various types of medical equipment.
My experience encompasses a wide range of medical equipment commonly used in first response. This includes automated external defibrillators (AEDs), suction devices, splints, bandages, cervical collars, backboards, intravenous (IV) cannulae (under appropriate medical direction), and various monitoring devices such as pulse oximeters and blood pressure cuffs.
I’m adept at using AEDs for defibrillation in cases of cardiac arrest, ensuring proper placement of electrodes and following the device prompts. I’m comfortable with suctioning airways to clear obstructions and using splints for fracture immobilization. Regular training and practice sessions maintain my proficiency in utilizing this equipment effectively and safely.
I have specific experience in using a pulse oximeter to continuously monitor a patient’s oxygen saturation levels after a traumatic incident. This information helped to inform my decision-making process and guide my oxygen administration strategy. Understanding the capabilities and limitations of each piece of equipment is crucial for providing effective patient care.
Q 26. How do you maintain your skills and knowledge in first response procedures?
Maintaining proficiency in first response requires continuous professional development. I actively participate in regular continuing medical education (CME) courses and workshops, focusing on advanced life support (ALS) techniques, trauma management, and updates on medical protocols. I also participate in simulated scenarios and practical drills to hone my skills in a safe, controlled environment.
Staying updated on the latest research and guidelines is critical. I subscribe to professional journals and actively participate in professional organizations, attending conferences and networking with colleagues to stay abreast of the latest advancements in the field. Regular self-assessment and peer review further enhance my knowledge and skills.
For instance, I recently completed a course on the management of severe allergic reactions (anaphylaxis), reinforcing my knowledge of epinephrine administration and other critical interventions. This approach ensures that I remain at the forefront of best practices and provide the highest quality of care.
Q 27. What are your professional goals in the field of first response?
My professional goals are centered on continuous improvement and enhancing my contributions to the first response community. I aspire to expand my expertise in advanced life support techniques, particularly in the management of critical traumas and complex medical emergencies. I’m also interested in pursuing leadership roles, mentoring newer first responders and contributing to the development of training programs. Ultimately, I aim to make a significant positive impact on patient outcomes and enhance the overall quality of pre-hospital emergency care. My long-term vision includes a leadership position within a reputable EMS organization.
Key Topics to Learn for First Response Procedures Interview
- Incident Assessment and Prioritization: Understanding the criticality of different incidents and applying appropriate triage protocols. Practical application: Differentiating between a minor injury and a life-threatening emergency.
- Emergency Communication and Dispatch: Mastering clear and concise communication techniques for effective incident reporting and resource allocation. Practical application: Practicing concise descriptions of incidents while under simulated pressure.
- Safety Procedures and Personal Protective Equipment (PPE): Knowing when and how to utilize appropriate PPE to ensure personal safety and the safety of others. Practical application: Understanding the limitations and proper usage of various types of PPE.
- First Aid and Basic Life Support (BLS): Demonstrating proficiency in administering first aid and BLS techniques, including CPR and AED usage. Practical application: Practicing and reviewing BLS protocols regularly.
- Incident Documentation and Reporting: Understanding the importance of accurate and complete incident documentation for legal and operational purposes. Practical application: Practicing writing clear and concise incident reports.
- Teamwork and Collaboration: Highlighting your ability to work effectively within a team to manage emergencies. Practical application: Describing experiences of effective teamwork in stressful situations.
- Ethical Considerations and Legal Responsibilities: Understanding the legal and ethical implications of first response actions. Practical application: Discussing scenarios requiring ethical decision-making under pressure.
- Post-Incident Debriefing and Critical Incident Stress Management (CISM): Understanding the importance of debriefing and stress management techniques for both individual and team well-being. Practical application: Describing your ability to manage stress and support others after a critical incident.
Next Steps
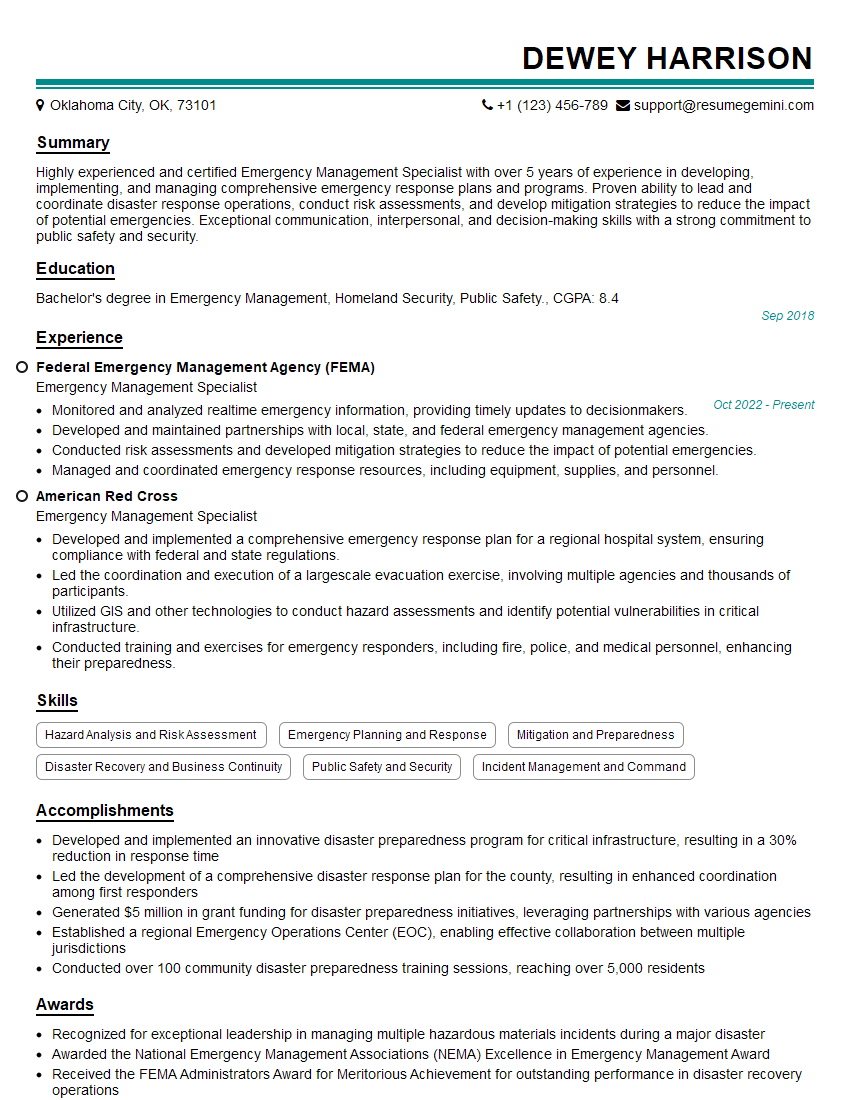
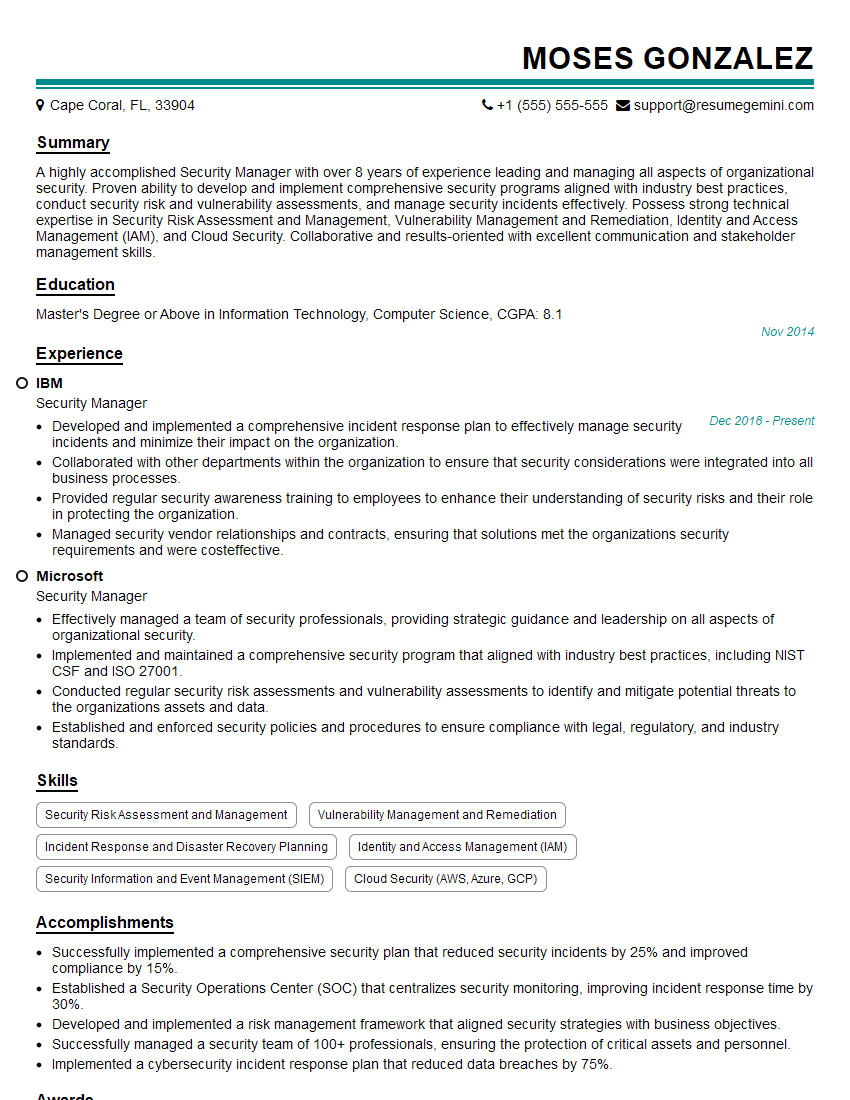
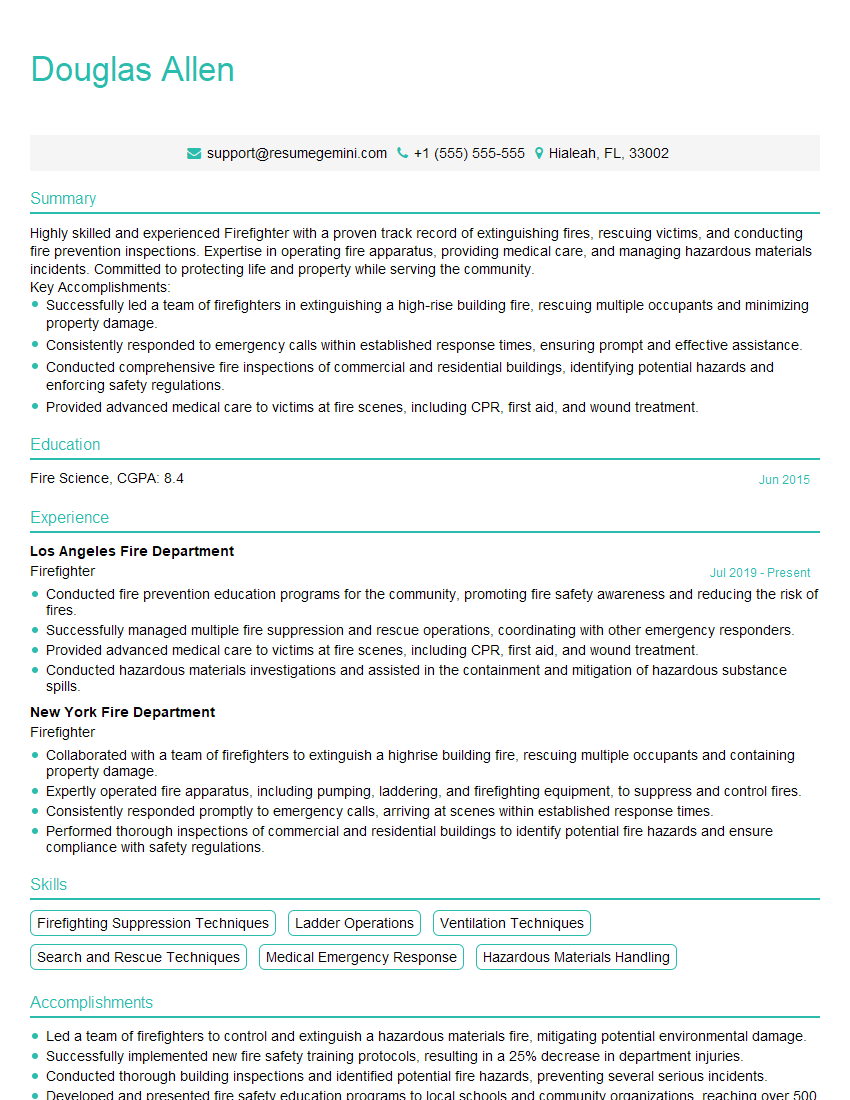
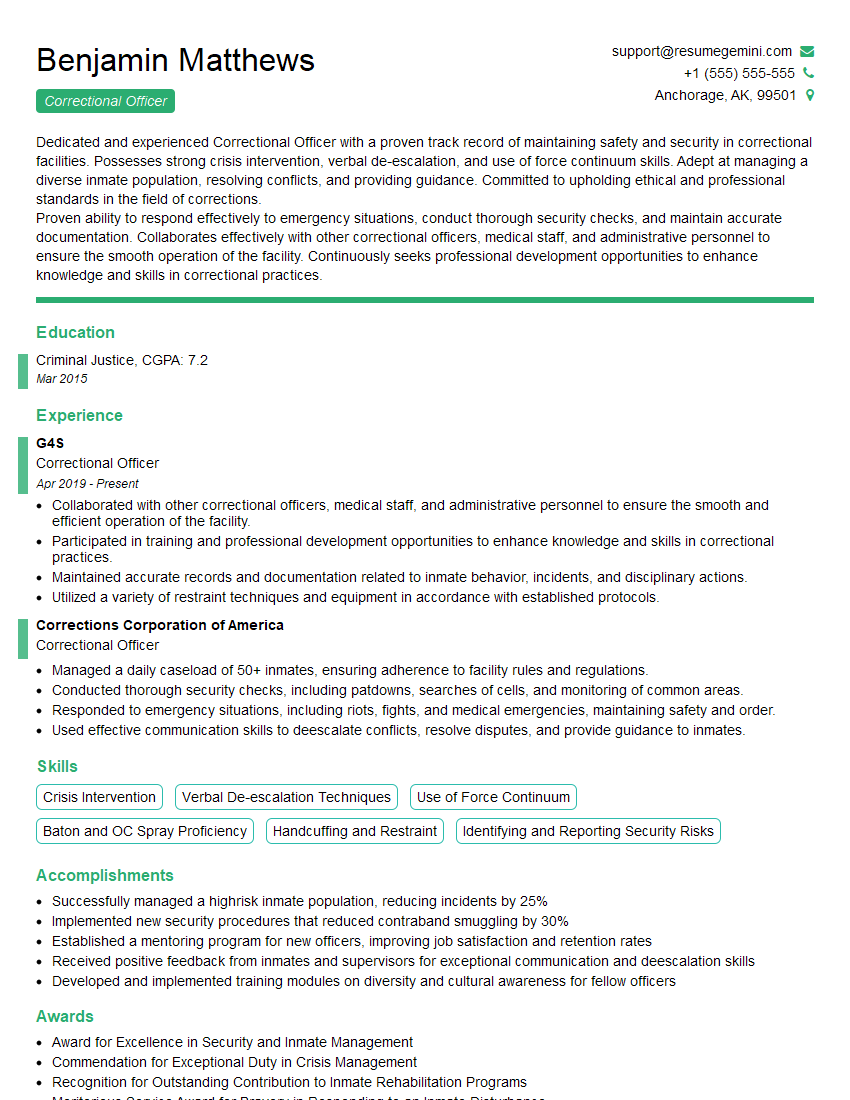
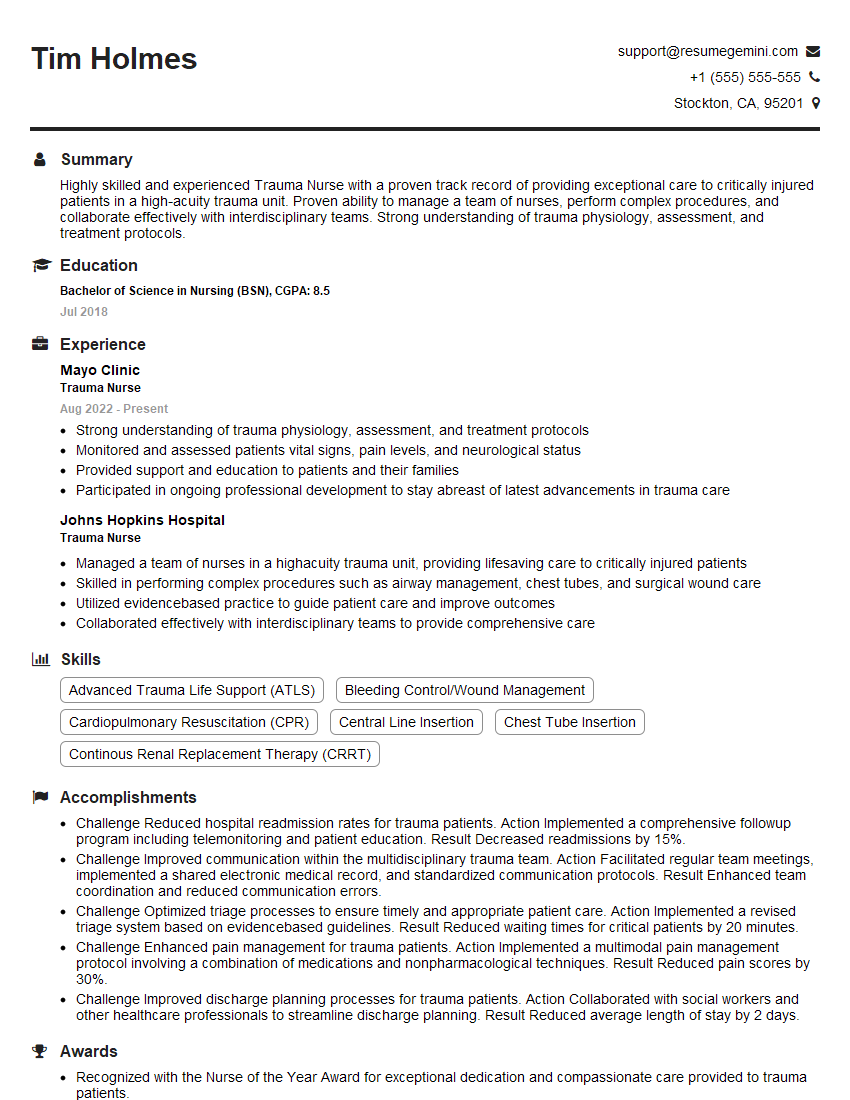
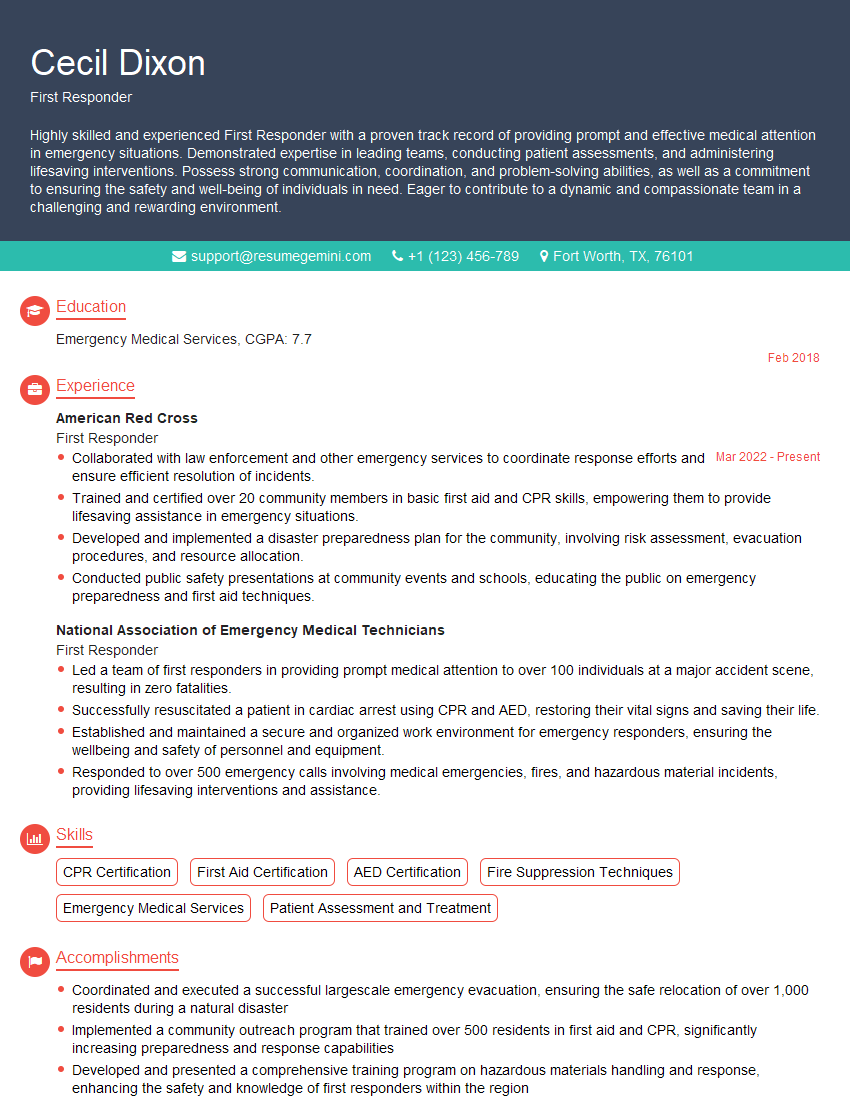
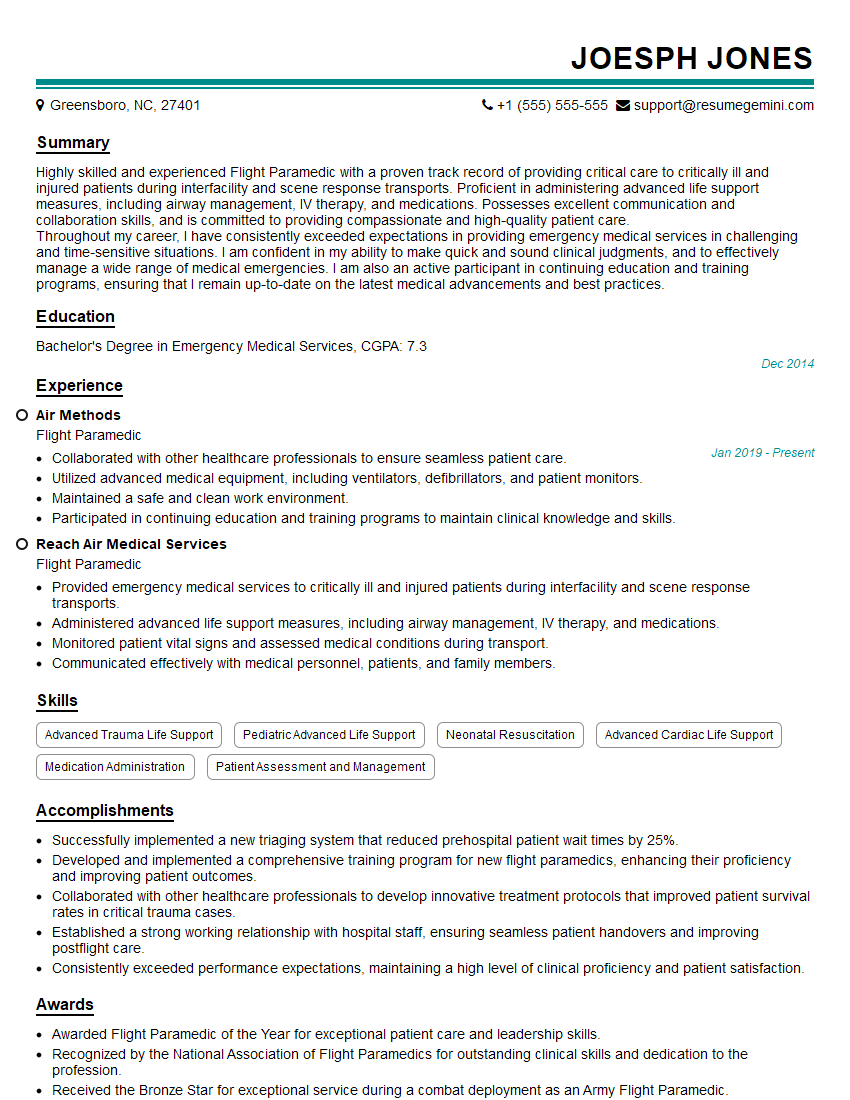
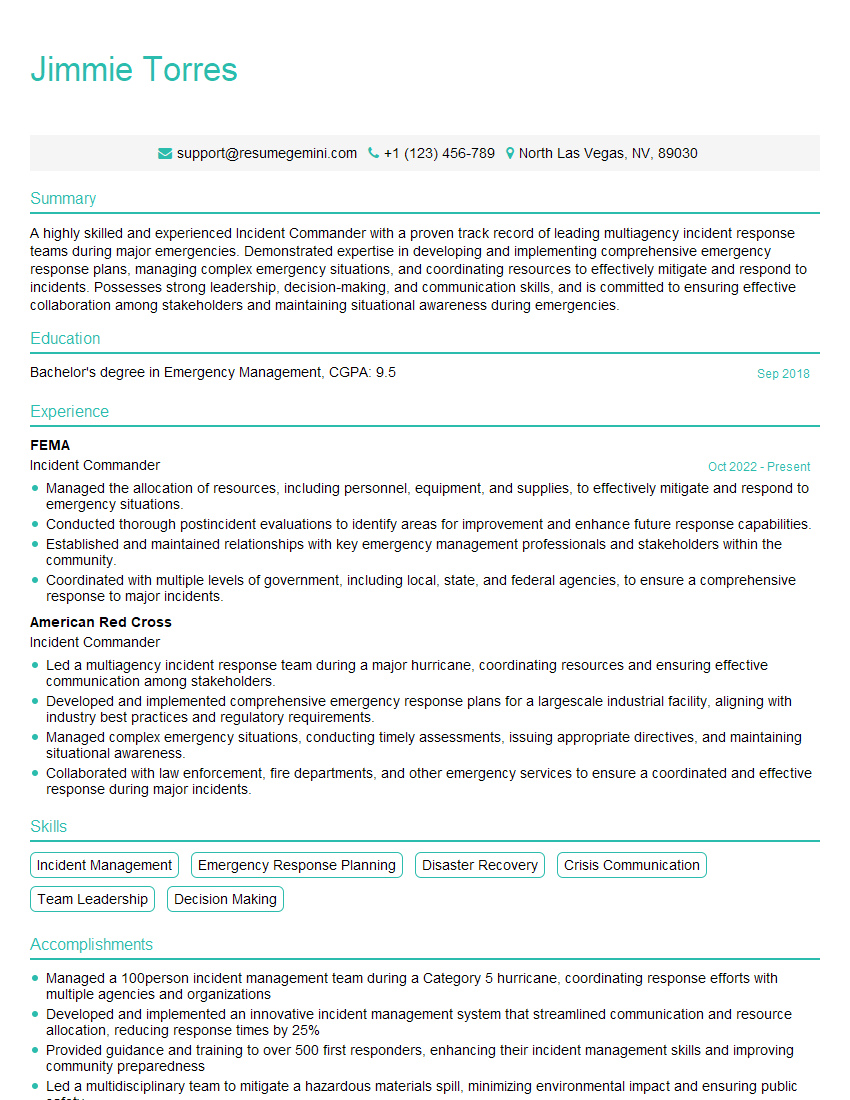
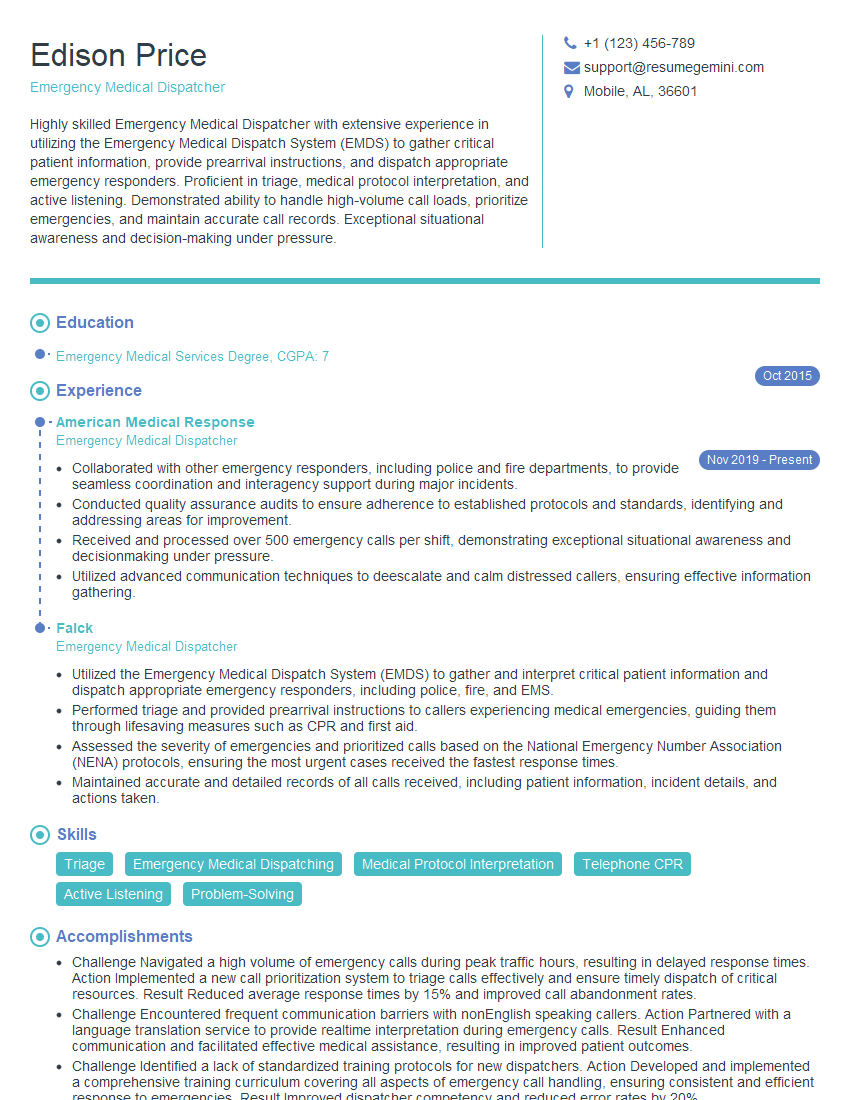
Mastering First Response Procedures is crucial for career advancement in this demanding field. It demonstrates a commitment to safety, efficiency, and professionalism. To significantly improve your job prospects, create a compelling and ATS-friendly resume that highlights your skills and experience. ResumeGemini is a trusted resource to help you build a professional resume that showcases your qualifications effectively. We provide examples of resumes tailored to First Response Procedures to help guide you. Invest time in crafting a strong resume; it’s your first impression on potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO