Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Diagnostic Equipment Use and Interpretation interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Diagnostic Equipment Use and Interpretation Interview
Q 1. Explain the principles of X-ray imaging.
X-ray imaging relies on the principle of differential absorption of X-rays by different tissues in the body. An X-ray tube generates a beam of X-rays that passes through the patient. Denser tissues, like bone, absorb more X-rays, resulting in fewer X-rays reaching the detector. Less dense tissues, like soft tissue, absorb fewer X-rays, allowing more to reach the detector. This difference in absorption creates a contrast in the resulting image, allowing us to visualize the internal structures.
Imagine shining a flashlight through your hand. Your bones will block more light than your soft tissues, creating shadows. X-ray imaging works similarly, but with invisible X-rays and a specialized detector that converts the X-ray signal into an image visible to us. The image is then displayed on a monitor, showing a grayscale representation of the internal structures, with whiter areas representing denser tissues and darker areas representing less dense tissues.
Q 2. Describe the different types of ultrasound transducers and their applications.
Ultrasound transducers are the heart of ultrasound imaging. They convert electrical energy into mechanical energy (sound waves) and vice versa. Different types cater to various applications:
- Linear array transducers: These produce a rectangular image with high resolution, ideal for superficial structures like skin, muscles, and breasts. Think of them as a high-detail camera for close-up views.
- Curvilinear array transducers: These offer a wider field of view and are commonly used for abdominal and pelvic imaging. They are like a wide-angle lens, allowing for a broader scan area.
- Phased array transducers: These are often used for cardiac imaging (echocardiography) because they allow for real-time visualization of the beating heart. They’re adaptable and can focus the beam quickly, crucial for a moving target.
- Endocavity transducers: These are designed for internal imaging and are inserted into body cavities like the rectum or vagina for detailed examination of organs. These allow for very close-up and detailed imaging.
The choice of transducer depends entirely on the region of interest and the desired image quality. For example, a high-frequency linear array transducer is ideal for visualizing superficial skin lesions, while a lower-frequency curvilinear array is better suited for examining deep abdominal structures.
Q 3. What are the safety precautions for operating an MRI machine?
MRI machine safety is paramount. Precautions include:
- Screening for contraindications: Patients with metallic implants (certain pacemakers, aneurysm clips), ferromagnetic foreign bodies, or claustrophobia require careful assessment before undergoing an MRI scan. These metallic objects can be dangerous and can even move within the body due to the strong magnetic field.
- Proper shielding: The MRI room must be shielded to prevent interference with other equipment and to contain the strong magnetic field. Specialized rooms prevent external magnetic fields from disrupting the scan, and also ensure that the strong magnetic field doesn’t disrupt nearby equipment.
- Patient monitoring: Continuous monitoring is essential during the scan to detect any adverse reactions or emergencies. This includes checking for any discomfort, distress, or any abnormal physiological parameters.
- Emergency protocols: Staff must be trained in emergency procedures to address any potential problems, such as a patient experiencing claustrophobia or a power outage. This training helps medical professionals react swiftly and efficiently to any potential complications.
- RF safety: Radiofrequency (RF) energy is used during MRI, and precautions are taken to minimize exposure to the patient. The intensity and duration of RF pulses are carefully controlled to maintain patient safety.
Ignoring these precautions can lead to serious injury or even death.
Q 4. How do you troubleshoot a malfunctioning ECG machine?
Troubleshooting a malfunctioning ECG machine involves a systematic approach:
- Check connections: Ensure all leads are properly connected to both the patient and the machine. Loose or faulty connections are a common cause of ECG artifacts.
- Inspect the leads: Look for any damage to the leads, such as broken wires or cracked connectors. Damaged leads can lead to inaccurate readings or no signal at all.
- Verify machine settings: Check that the machine is properly calibrated and that the appropriate settings are selected for the patient’s age and size. Incorrect settings can affect the quality and interpretation of the ECG.
- Assess the ECG tracing: Analyze the ECG tracing for artifacts, such as muscle tremor, wandering baseline, or 60-Hz interference. These artifacts can indicate problems with the machine’s settings, the patient’s connection to the device or electrical interference.
- Perform a self-test: Many ECG machines have a self-test function. Running this test can help identify internal problems within the machine itself.
- Consult the manual: The machine’s operating manual will provide detailed troubleshooting information for specific error codes or problems.
- Seek professional help: If the problem persists, contact a qualified biomedical technician for repair. It’s important to only allow qualified personnel to work on or repair the equipment.
A methodical approach, combined with a solid understanding of ECG principles and the machine’s functionality, is key to effective troubleshooting.
Q 5. Explain the process of image acquisition in CT scanning.
CT image acquisition involves the use of X-rays and a rotating gantry. The patient lies on a table that moves through the gantry. The X-ray tube and detectors rotate around the patient, acquiring data from multiple angles. As the X-ray beam passes through the patient, different tissues absorb different amounts of X-rays, similar to a standard X-ray. However, instead of a single image, many X-ray projections are obtained from various angles.
A computer then uses sophisticated algorithms (reconstruction algorithms) to process these projections and generate cross-sectional images (slices) of the body. These slices are then stacked together to create a three-dimensional representation of the internal anatomy. The entire process is very fast, often completed in a matter of seconds.
Think of it like taking many photographs of an object from different angles and then using a computer to assemble a 3D model from these 2D images. This process allows for detailed visualization of both soft tissues and bone.
Q 6. Describe the differences between CT and MRI imaging.
CT and MRI are both powerful medical imaging techniques, but they use fundamentally different principles:
- CT (Computed Tomography): Uses X-rays to create cross-sectional images. It’s excellent for visualizing bone, lung, and some soft tissues, providing high spatial resolution. It’s relatively fast and less expensive than MRI.
- MRI (Magnetic Resonance Imaging): Employs a strong magnetic field and radio waves to create images based on the response of hydrogen atoms in the body. It’s superior for visualizing soft tissues, including the brain, spinal cord, muscles, and ligaments. It provides exquisite soft tissue contrast but is slower and more expensive than CT.
In essence, CT is like a detailed blueprint showing the structure of a building, while MRI is like a highly detailed photograph showing the building’s interior textures and compositions. The choice between them depends on the clinical question and the type of information required.
Q 7. What are the artifacts that can occur in ultrasound images?
Several artifacts can degrade the quality of ultrasound images, hindering accurate interpretation:
- Acoustic shadowing: This occurs when sound waves are completely blocked by a highly reflective or attenuating structure (like a stone in the gallbladder). This creates a dark shadow behind the structure, obscuring the underlying anatomy.
- Acoustic enhancement: The opposite of shadowing, this appears as a brighter area behind a fluid-filled structure (like a cyst). Sound waves travel faster through fluid, resulting in increased intensity behind the structure.
- Reverberation: Multiple reflections of sound waves between two strong reflectors (e.g., air-tissue interfaces) create multiple spurious echoes, making the image appear cluttered.
- Refraction: Bending of sound waves as they pass between tissues with different acoustic impedances can distort the image, causing objects to appear in an incorrect location.
- Motion artifacts: Patient movement during the scan can blur the image or cause misrepresentation of structures.
Recognizing these artifacts is crucial for accurate interpretation of ultrasound images. Experience and careful scanning techniques can minimize their occurrence.
Q 8. How do you ensure the quality of images obtained from diagnostic equipment?
Ensuring high-quality diagnostic images involves a multi-faceted approach encompassing equipment maintenance, proper technique, and image processing. Think of it like baking a cake – you need the right ingredients (equipment), the correct recipe (technique), and the right oven temperature (processing) to get a perfect result.
- Regular Equipment Calibration and Maintenance: Diagnostic equipment, like X-ray machines and ultrasound scanners, needs routine calibration and preventative maintenance to ensure optimal performance. This involves checking for things like consistent output levels, accurate spatial resolution, and the absence of any artifacts (unwanted features).
- Proper Patient Positioning and Technique: Correct patient positioning is critical. For example, in chest X-rays, slight rotation can obscure lung fields. The technologist’s skill in positioning and choosing the correct imaging parameters (e.g., kVp and mAs in X-ray) directly impacts image quality. We’re aiming for the clearest view possible, minimizing motion blur, and maximizing detail.
- Image Processing and Post-processing Techniques: Software tools allow us to optimize images after acquisition. This can include adjusting brightness and contrast, removing noise, and applying various filters to enhance visibility of specific structures. It’s like digitally enhancing a slightly blurry photograph to reveal more detail.
- Quality Control Programs: Most radiology departments have robust QC programs including regular phantom tests (using standardized objects) to ensure equipment is performing within acceptable limits. This helps detect subtle degradations in performance before they impact patient care.
Q 9. What are the limitations of each modality (X-ray, CT, MRI, Ultrasound)?
Each modality has strengths and limitations. Choosing the right modality depends on the clinical question.
- X-ray: Excellent for visualizing bone fractures and detecting foreign bodies. Limitations: Overlapping structures can obscure detail (think of how your ribs might obscure a lung lesion), and it has limitations in soft tissue visualization. It also uses ionizing radiation.
- CT (Computed Tomography): Provides detailed cross-sectional images of the body. Limitations: Higher radiation dose than X-ray, and not ideal for patients with metal implants or claustrophobia. Also more expensive than X-ray.
- MRI (Magnetic Resonance Imaging): Superior for soft tissue visualization, ideal for brain and spine imaging. Limitations: Expensive, time-consuming, contraindicated in patients with certain metal implants (pacemakers), and prone to artifacts from patient motion.
- Ultrasound: Non-ionizing, portable, and relatively inexpensive. Excellent for visualizing real-time organ movement and blood flow. Limitations: Image quality is operator-dependent and limited by the presence of bone or gas which attenuates the ultrasound waves (think of sound waves not penetrating a thick wall).
Q 10. Describe the role of PACS (Picture Archiving and Communication System).
PACS (Picture Archiving and Communication System) is the digital backbone of modern radiology departments. It’s essentially a sophisticated digital filing system for medical images and reports. Think of it as a highly secure and organized digital library specifically designed for medical images.
- Image Storage and Retrieval: PACS stores images from various modalities (X-ray, CT, MRI, ultrasound) in a central database, allowing quick and easy access by authorized personnel.
- Image Distribution and Sharing: Images can be quickly sent to referring physicians, consultants, and other healthcare professionals, facilitating timely diagnosis and treatment decisions.
- Workflow Optimization: PACS streamlines the workflow, reducing the time it takes to get images to radiologists and other clinicians. This improves efficiency and reduces potential delays in patient care.
- Enhanced Collaboration: PACS facilitates collaboration among radiologists and other healthcare providers by allowing them to view and share images and reports from a central location.
Q 11. Explain the ALARA principle in radiation protection.
ALARA stands for “As Low As Reasonably Achievable.” It’s the guiding principle in radiation protection. It emphasizes minimizing radiation exposure to patients and personnel while still obtaining diagnostically useful images. It’s a balance between safety and the need for information.
- Justification: We only order imaging when it is medically necessary and the benefits outweigh the risks.
- Optimization: We use the lowest radiation dose possible while still achieving diagnostic quality. This includes optimizing imaging parameters (like mAs and kVp in X-ray) and using radiation-reducing techniques.
- Limitation: We limit exposure time, and we use shielding (like lead aprons) whenever possible.
For example, if a patient needs a chest X-ray, we’ll carefully adjust the settings to obtain a clear image with the minimum possible radiation dose. We might also use a low-dose CT scan instead of a conventional one, when appropriate.
Q 12. How do you interpret a normal ECG tracing?
Interpreting a normal ECG tracing involves analyzing the different waves, segments, and intervals. It’s like reading a musical score – each wave represents a specific electrical event in the heart.
A normal ECG shows a regular rhythm, with a consistent rate (typically 60-100 beats per minute). The P wave represents atrial depolarization (contraction), the QRS complex represents ventricular depolarization, and the T wave represents ventricular repolarization. The intervals between these waves are also important; abnormalities in these can indicate different heart conditions.
Understanding normal ECG intervals and amplitudes is crucial for recognizing abnormalities. Any deviations from the normal pattern can suggest conditions like arrhythmias, myocardial infarction (heart attack), or electrolyte imbalances.
Q 13. How would you handle a situation where the equipment malfunctions during a procedure?
Equipment malfunction during a procedure is a serious event that requires immediate and calm action. The priority is always patient safety.
- Patient Safety First: If the malfunction poses an immediate risk to the patient (e.g., an unstable X-ray machine), immediately stop the procedure and ensure the patient’s safety.
- Assess the Situation: Determine the nature of the malfunction. Is it a minor glitch or a major equipment failure?
- Follow Department Protocol: Each department has specific protocols for dealing with equipment malfunctions. These protocols often include contacting biomedical engineering, reporting the incident to the supervisor, and documenting the event.
- Consider Alternatives: If possible, explore alternative imaging modalities or procedures to complete the diagnostic task safely.
- Document Thoroughly: Document all aspects of the malfunction, including the time of the event, the nature of the problem, actions taken, and the patient’s condition.
For example, if the ultrasound machine malfunctions during an abdominal exam, we might try rebooting the machine. If this fails, we’d follow our department’s protocol, possibly contacting biomedical engineering for repair, and explaining the situation to the referring physician while exploring alternative approaches to diagnosis.
Q 14. What is the importance of patient positioning in diagnostic imaging?
Patient positioning is crucial for obtaining high-quality diagnostic images and is essential for minimizing radiation exposure. It’s like setting up a stage play; you want the actors (organs) to be in the correct position for the best view. Incorrect positioning can lead to image artifacts and misinterpretations.
- Minimizing Overlap and Obscuration: Correct positioning ensures that the area of interest is clearly visualized, without significant overlap from other structures. For example, in a chest X-ray, proper positioning prevents the heart from obscuring lung fields.
- Reducing Radiation Dose: Proper positioning can significantly minimize radiation dose by ensuring that only the necessary area is exposed.
- Improving Image Quality: Accurate positioning is essential for reducing image artifacts and distortions, leading to improved image quality and diagnostic accuracy.
- Anatomical Landmark Identification: Many imaging protocols use anatomical landmarks (like the spine, ribs, or iliac crest) as references for optimal positioning. For example, positioning for a lateral chest X-ray requires proper alignment of the patient’s spine to ensure proper visualization of the lungs.
Q 15. Describe your experience with quality control procedures for diagnostic equipment.
Quality control (QC) for diagnostic equipment is crucial for ensuring accurate and reliable results. It involves a multifaceted approach encompassing preventative maintenance, regular testing, and meticulous record-keeping. Think of it as a comprehensive health check for your machines, ensuring they remain in peak condition.
- Preventative Maintenance: This includes regular servicing, lubrication, and replacement of worn parts as recommended by the manufacturer. For example, X-ray tubes have a limited lifespan and require scheduled replacement to maintain optimal performance and image quality.
- Performance Testing: We use standardized phantoms – objects mimicking human anatomy – to assess image quality, resolution, and accuracy. For ultrasound, this might involve testing the machine’s ability to accurately measure distances and differentiate tissue types. For X-ray, we’d evaluate factors like contrast and spatial resolution using a dedicated phantom.
- Quality Control Records: Detailed logs meticulously document all QC procedures, results, and any corrective actions taken. These records are essential for compliance with regulatory standards and for tracking the long-term performance of the equipment. Failure to keep accurate records could lead to serious consequences, including compromised patient care and legal ramifications.
Consistent QC is not just about avoiding malfunctions; it’s about ensuring patient safety and the reliability of diagnostic information, leading to more effective treatment plans.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you maintain patient confidentiality when handling diagnostic images?
Maintaining patient confidentiality when handling diagnostic images is paramount and is governed by strict regulations like HIPAA in the US. We adhere to a multi-layered approach:
- Access Control: Image storage systems are password-protected, with access limited only to authorized personnel who need the information for patient care. We use role-based access control (RBAC) which ensures only appropriate individuals can view specific images.
- Secure Data Transmission: When transferring images electronically, we use encrypted channels, such as DICOM (Digital Imaging and Communications in Medicine) over secure networks, preventing unauthorized interception.
- Physical Security: Physical access to areas where images are stored is restricted to authorized personnel. This includes locked rooms, secure servers, and appropriate physical barriers.
- Data Anonymization: Whenever possible, we de-identify images before using them for teaching or research purposes. This involves removing any patient identifiers, such as names and medical record numbers, protecting their privacy.
Breaches of confidentiality can have severe consequences, both professionally and legally. Therefore, diligent adherence to these protocols is non-negotiable.
Q 17. Explain your understanding of radiation safety regulations.
Radiation safety regulations are crucial to minimizing the risks associated with ionizing radiation used in diagnostic imaging. These regulations vary slightly depending on location but share a common goal: protecting both patients and healthcare workers from unnecessary exposure.
- ALARA Principle: This fundamental principle – ‘As Low As Reasonably Achievable’ – guides all radiation practices. We strive to use the lowest possible radiation dose while still achieving diagnostic quality images. This involves optimizing exposure parameters, using appropriate shielding, and employing advanced imaging techniques that reduce radiation dose.
- Radiation Safety Officer (RSO): Many facilities have an RSO responsible for overseeing radiation safety programs, ensuring compliance with regulations, and providing training to staff. This role is crucial for maintaining a safe environment.
- Equipment Calibration and Maintenance: Regular calibration of imaging equipment ensures that radiation output is accurately controlled and within safety limits. Proper maintenance helps to prevent malfunctions that could lead to unnecessary radiation exposure.
- Personnel Monitoring: Healthcare workers who routinely work with ionizing radiation wear dosimeters to monitor their cumulative radiation exposure. This ensures that exposure levels remain well within safety limits and helps to identify potential problems early.
Ignoring radiation safety regulations can have serious health consequences for patients and staff, leading to increased risk of cancer and other radiation-related illnesses. Adherence to these regulations is therefore a critical aspect of our work.
Q 18. What is your experience with different image processing techniques?
Image processing techniques are essential for enhancing the diagnostic quality of medical images. These techniques vary depending on the modality but often include:
- Contrast Enhancement: This involves adjusting the brightness and contrast of an image to improve the visibility of subtle details. This is particularly helpful in identifying small lesions or subtle changes in tissue density.
- Noise Reduction: Medical images are often subject to noise – random variations in signal intensity. Noise reduction techniques help to suppress this noise, improving image clarity and diagnostic accuracy. Techniques like filtering can be very effective.
- Image Sharpening: Sharpening enhances the edges and details in an image, improving the visibility of fine structures. This can be particularly useful in detecting small fractures or subtle tissue changes.
- Image Reconstruction: For techniques like CT and MRI, complex algorithms reconstruct the image from the raw data. Different reconstruction techniques can significantly affect the image quality and diagnostic information.
- 3D Reconstruction: Advanced techniques allow us to create three-dimensional models from multiple two-dimensional images, which can be extremely useful for surgical planning and visualization of complex anatomical structures.
The choice of image processing technique depends heavily on the specific imaging modality and the clinical question at hand. Over-processing can introduce artifacts, so careful selection and application are crucial.
Q 19. Describe a time you had to troubleshoot a complex equipment problem.
During a routine MRI scan, the machine suddenly malfunctioned, displaying a critical error message and halting the procedure mid-scan. The patient was safely removed, but the immediate concern was data recovery and equipment repair.
My troubleshooting involved a systematic approach:
- Safety First: Ensuring patient safety was the priority, so we confirmed the patient was unharmed and the machine was safely powered down.
- Error Code Analysis: We reviewed the error message, which indicated a potential hardware failure in the gradient coil system.
- Manufacturer Contact: We immediately contacted the manufacturer’s technical support team. Their initial remote diagnostics pointed towards a faulty component within the gradient amplifier.
- Component Replacement: The manufacturer dispatched a technician who replaced the faulty component. This required specialized tools and expertise beyond the scope of our in-house team.
- System Testing: After the repair, we performed comprehensive system tests to verify proper functionality and image quality before resuming patient scans.
This experience highlighted the importance of having a well-defined protocol for equipment troubleshooting, including readily accessible manufacturer support and a trained team capable of handling technical issues effectively.
Q 20. How do you ensure accurate image documentation and reporting?
Accurate image documentation and reporting are essential for maintaining a high standard of care. This involves a meticulous process:
- DICOM Standards: We use DICOM standards for image storage and transmission, ensuring interoperability between different systems and the inclusion of essential patient and image metadata.
- Image Labeling and Annotation: Images are meticulously labeled with patient identifiers, date, time, and relevant clinical information. Any findings, such as lesions or abnormalities, are clearly annotated directly on the image or within the associated report.
- Structured Reporting: We utilize structured reporting templates to ensure consistency and completeness in the radiological reports. These templates guide the radiologist in documenting their findings in a clear and concise manner.
- Quality Assurance Review: Reports are often subjected to quality assurance review by a senior radiologist or other qualified professionals, ensuring accuracy and consistency before being sent to the referring physician. This step is crucial in identifying and correcting potential errors.
- Archiving: Images and reports are stored securely and for a long period according to regulatory guidelines and institutional policies, ensuring access for future reference and patient care.
Errors in documentation can have serious consequences, potentially leading to misdiagnosis and inappropriate treatment. Therefore, meticulous attention to detail is vital.
Q 21. Explain the difference between ionizing and non-ionizing radiation.
The key difference between ionizing and non-ionizing radiation lies in their ability to ionize atoms. Ionizing radiation has enough energy to remove electrons from atoms, creating ions. Non-ionizing radiation does not possess this capability.
- Ionizing Radiation: This includes X-rays, gamma rays, and some forms of ultraviolet radiation. Because they can ionize atoms, they can cause damage to DNA and other biological molecules, potentially leading to cellular damage and increased risk of cancer. This is why radiation safety protocols are crucial when using these types of radiation for diagnostic purposes.
- Non-ionizing Radiation: This includes radio waves, microwaves, infrared radiation, visible light, and some forms of ultraviolet radiation. These forms of radiation have lower energy levels and cannot directly ionize atoms. While they can still cause some biological effects, such as heating, they are generally considered less hazardous than ionizing radiation. Examples of medical imaging using non-ionizing radiation include ultrasound and magnetic resonance imaging (MRI).
Understanding this fundamental distinction is critical for appreciating the different safety considerations associated with different medical imaging techniques. Ionizing radiation necessitates stringent safety protocols to mitigate potential risks, while non-ionizing radiation carries significantly lower risks.
Q 22. What are the various types of contrast agents used in diagnostic imaging?
Contrast agents, also known as contrast media, are substances used in diagnostic imaging to enhance the visibility of internal structures and organs. They work by altering the signal intensity of tissues, making them appear brighter or darker on images, depending on the modality. Different imaging techniques utilize different types of contrast agents.
- Iodine-based contrast agents: These are the most common type, used primarily in X-ray, CT, and fluoroscopy. They absorb X-rays more efficiently than surrounding tissues, creating a clear distinction. For example, during a CT scan of the abdomen, iodine contrast helps visualize the blood vessels and organs more clearly.
- Barium sulfate: This is a radiopaque agent used primarily in gastrointestinal imaging. It’s ingested or administered rectally to coat the digestive tract, making the lining visible on X-rays. It’s relatively safe because it’s insoluble and doesn’t get absorbed by the body.
- Gadolinium-based contrast agents (GBCA): These are paramagnetic agents used in MRI. They shorten the relaxation time of water molecules, increasing the signal intensity of tissues and enhancing the image contrast. They are crucial for visualizing subtle differences in tissue characteristics, often used in brain imaging or to evaluate blood flow.
- Air or gas: These are negative contrast agents, meaning they appear dark on X-rays. They are used to highlight certain structures by creating a contrast with surrounding tissues. For instance, air can be introduced into the abdomen during a procedure to help visualize abdominal organs.
The choice of contrast agent depends on the specific imaging modality and the clinical question being addressed.
Q 23. Describe the potential risks and benefits associated with contrast media.
Contrast media, while essential for improved image quality, do carry potential risks and benefits. Benefits include significantly improved diagnostic accuracy, leading to better clinical decision-making and patient care. For example, a clear visualization of a blockage in an artery during an angiogram allows for prompt intervention to prevent a stroke.
However, risks exist, mainly concerning allergic reactions. Iodine-based agents are notorious for causing reactions, ranging from mild (rash, itching) to severe (anaphylaxis, a life-threatening allergic reaction). The risk increases with pre-existing allergies, kidney problems, or asthma. Patients are often pre-screened for these risks. Gadolinium-based agents, while less commonly associated with severe allergic reactions, have also shown potential for long-term retention in patients with compromised kidney function. This is a critical area of ongoing research.
Careful patient history, pre-medication when necessary, close monitoring during and after contrast administration, and having emergency protocols in place are essential to mitigate these risks. The benefits of improved diagnostics must always be carefully weighed against potential adverse effects, with a thorough discussion with the patient before any procedure.
Q 24. What is your experience with image archiving and retrieval systems?
I have extensive experience with various Picture Archiving and Communication Systems (PACS). PACS are the digital repositories for medical images, allowing for easy storage, retrieval, and sharing of images across different departments and even different healthcare facilities. My experience encompasses both the practical use of PACS for viewing and interpreting images and also the technical understanding of image management, including data security and workflow optimization. I’m proficient in using PACS to access previous studies, compare images over time, and generate reports. I understand the importance of robust image quality assurance processes and the maintenance of DICOM standards for compatibility across systems. For example, in one situation, access to a patient’s previous CT scan through PACS enabled me to identify subtle changes not immediately apparent in the current scan, leading to an earlier diagnosis and intervention.
Q 25. How do you prioritize tasks during a busy workday involving multiple patients?
Prioritizing tasks during a busy workday requires a structured approach. I typically use a combination of urgency and importance to prioritize. I use a system where I assess each task based on:
- Urgency: How quickly does this task need to be completed? (e.g., a patient experiencing acute chest pain needs immediate attention).
- Importance: What is the potential impact of completing (or not completing) this task? (e.g., reviewing a critical MRI scan before surgery is crucial).
I often use a visual tool, like a prioritized list or a Kanban board, to keep track of my tasks and their status. This approach ensures that time-sensitive and high-impact tasks are addressed first, while less urgent ones are handled efficiently without compromising patient care. Furthermore, effective communication with colleagues and team members ensures efficient workflow and prevents bottlenecks.
Q 26. What are your knowledge and experience with different types of medical imaging software?
My experience with medical imaging software is broad, encompassing various modalities and applications. I am proficient in using software for image acquisition, processing, and analysis across different platforms. This includes:
- DICOM viewers: I’m skilled in using various DICOM viewers to access, manipulate, and interpret medical images from different modalities (CT, MRI, X-ray, etc.).
- Image processing software: I have experience with software that allows for image enhancement, measurement, and analysis, including tools for 3D reconstruction and volume rendering. This is vital for tasks like measuring tumor size or analyzing bone density.
- Specialized software packages: My experience also includes the use of specialized software packages designed for specific clinical applications, such as cardiovascular image analysis, neuroimaging, and musculoskeletal imaging. These packages often have advanced tools for quantitative analysis.
I’m always keen to learn and adapt to new technologies to improve my efficiency and the quality of my interpretations. Continuous professional development is crucial in this rapidly evolving field.
Q 27. Explain your understanding of the principles of image reconstruction.
Image reconstruction is the process of creating a diagnostic image from raw data acquired by imaging modalities such as CT, MRI, and PET. It’s a complex process involving sophisticated mathematical algorithms. In essence, these algorithms take the raw signals from the detectors and transform them into a visual representation of the anatomy. Different modalities utilize different reconstruction techniques.
For instance, in CT, the raw data are attenuation values along numerous X-ray beams. These values are used in a process called Filtered Back Projection, or more advanced iterative techniques, to reconstruct a cross-sectional image of the body. Similarly, MRI uses complex Fourier transforms to convert the raw data into images that show different tissue characteristics based on the relaxation times of the water molecules. The choice of reconstruction algorithm significantly impacts the image quality, resolution, and noise level. Optimizing these parameters is essential for producing high-quality diagnostic images.
A basic analogy would be assembling a jigsaw puzzle: The raw data are like the individual pieces, and the reconstruction algorithm is the process that combines these pieces to create a coherent picture. The quality of the final image depends on the accuracy and efficiency of the ‘assembly’ process.
Q 28. Describe how you would handle a situation involving a patient who is claustrophobic during an MRI scan.
Managing a claustrophobic patient during an MRI scan requires a sensitive and empathetic approach, prioritizing patient comfort and safety. My strategy involves a multi-pronged approach:
- Pre-scan preparation: A thorough discussion before the scan is crucial. I’d explain the procedure in detail, addressing the patient’s concerns about claustrophobia. I’d offer options like open MRI systems (if available), sedation if appropriate, or the use of relaxation techniques like deep breathing exercises.
- During the scan: I’d ensure the patient feels in control. This may involve allowing them to choose their preferred music, providing earplugs to dampen the scanner noise, and keeping the room well-lit. Maintaining open communication is essential. I’d reassure the patient throughout the scan, checking in regularly to ensure their comfort level. In severe cases, halting the scan is always an option.
- Post-scan care: Once the scan is complete, I’d provide a supportive and comforting environment, allowing the patient to recover at their own pace. In the event of a panic attack or significant distress, it’s vital to have access to appropriate medical assistance and medication.
The key is to establish trust and create a safe space for the patient. By acknowledging their fears and implementing strategies to alleviate anxiety, we can often successfully complete the MRI scan while ensuring patient well-being.
Key Topics to Learn for Diagnostic Equipment Use and Interpretation Interview
- Equipment Operation & Maintenance: Understanding the principles of operation, calibration, and troubleshooting for various diagnostic equipment (e.g., X-ray machines, ultrasound systems, ECG machines). This includes practical knowledge of safety protocols and quality control procedures.
- Image Acquisition & Optimization: Mastering techniques for acquiring high-quality diagnostic images, including patient positioning, parameter settings, and artifact reduction. This involves understanding the limitations of each modality and how to optimize image quality for accurate interpretation.
- Image Interpretation & Analysis: Developing the ability to critically analyze diagnostic images, identifying key anatomical structures, recognizing normal and abnormal findings, and differentiating between various pathologies. This requires a strong understanding of anatomy, physiology, and pathology.
- Report Writing & Communication: Learning to effectively communicate findings through concise and accurate reports, clearly articulating observations, conclusions, and recommendations to collaborating healthcare professionals. This includes adherence to professional standards and ethical considerations.
- Radiation Safety & Protection: Understanding and applying radiation safety principles and ALARA (As Low As Reasonably Achievable) practices to minimize patient and operator exposure during procedures. This includes proper shielding techniques and radiation safety regulations.
- Quality Assurance & Control: Knowing the importance of quality assurance and control procedures to maintain the accuracy and reliability of diagnostic equipment and results. This covers preventative maintenance, calibration checks, and quality control testing.
- Troubleshooting & Problem Solving: Developing the ability to identify and resolve technical issues related to diagnostic equipment, employing systematic troubleshooting strategies to minimize downtime and ensure optimal performance.
Next Steps
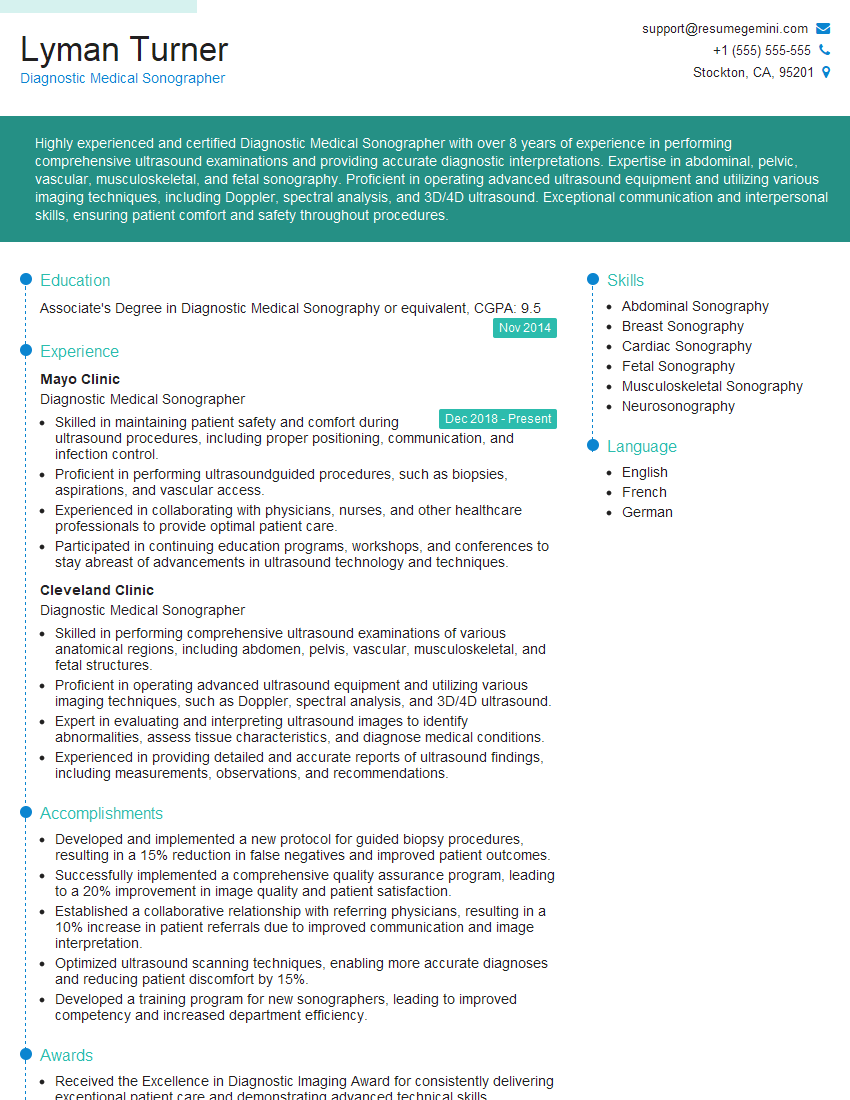
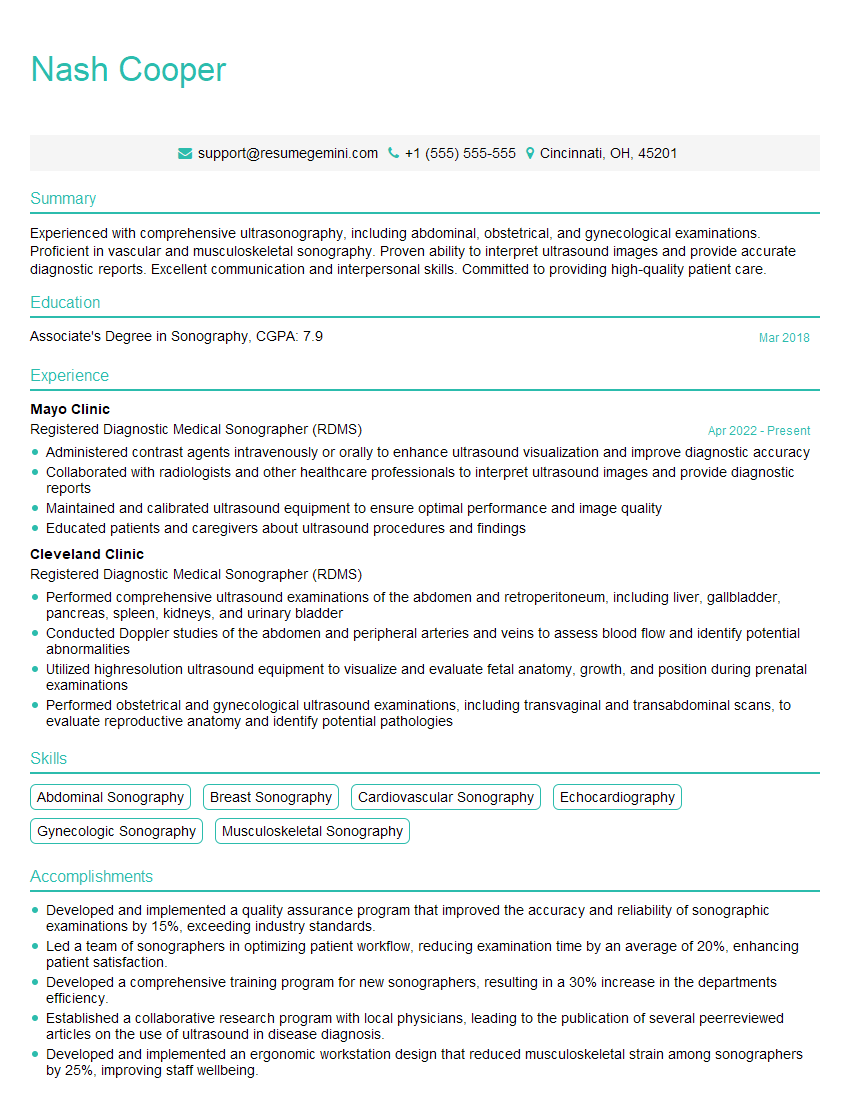
Mastering Diagnostic Equipment Use and Interpretation is crucial for career advancement in healthcare. A strong understanding of these principles demonstrates your technical expertise and opens doors to exciting opportunities and increased earning potential. To maximize your job prospects, it’s essential to create a resume that highlights your skills and experience effectively, particularly for Applicant Tracking Systems (ATS). ResumeGemini is a trusted resource that can help you build a professional and ATS-friendly resume that showcases your qualifications. Examples of resumes tailored to Diagnostic Equipment Use and Interpretation are available to help guide your process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO