The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Proficient in using diagnostic and testing equipment interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Proficient in using diagnostic and testing equipment Interview
Q 1. Describe your experience with troubleshooting malfunctioning diagnostic equipment.
Troubleshooting malfunctioning diagnostic equipment requires a systematic approach. I begin by observing the equipment for any obvious physical issues, such as loose connections or damaged components. Then, I consult the equipment’s manual for troubleshooting guides and error codes. I’ll check power supply, input signals, and output displays. For example, if a blood analyzer is displaying an ‘error 12’ code, the manual might indicate a problem with the reagent sensor. I would then inspect the sensor for blockages or contamination. If the problem persists after checking the obvious, I move on to more advanced diagnostics, potentially using a multimeter to check voltages and signal integrity or running diagnostic programs built into the device. I always meticulously document my steps, findings, and any repairs made.
In one instance, an ultrasound machine exhibited erratic behavior – inconsistent image display and intermittent power fluctuations. After carefully checking power cables and wall outlets, I discovered a loose internal connection near the power supply. Once tightened, the machine operated correctly. This highlights the importance of considering even minor issues before progressing to more complex solutions.
Q 2. Explain the process of calibrating a specific diagnostic instrument.
The calibration process varies depending on the specific instrument. Let’s take a blood glucose meter as an example. First, I would ensure the meter is turned off. Then, I would use control solutions with known glucose concentrations—typically provided by the manufacturer. I would run each control solution multiple times according to the manufacturer’s instructions, typically using multiple test strips. The meter’s readings are then compared against the known values. If the readings fall outside the acceptable range specified in the calibration guidelines, adjustments would need to be made, sometimes requiring specialized software or tools depending on the sophistication of the meter. If adjustments are not possible, the instrument needs to be serviced or replaced. Accurate calibration is crucial to ensure reliable and accurate test results—a miscalibrated meter could lead to incorrect diagnoses and potentially harmful treatment decisions for patients.
Q 3. What safety precautions do you follow when using diagnostic equipment?
Safety is paramount when using diagnostic equipment. I always follow the manufacturer’s safety guidelines and adhere to all relevant regulations. This includes wearing appropriate personal protective equipment (PPE), such as gloves and eye protection, whenever necessary, especially when dealing with potentially hazardous samples or materials. I also ensure proper grounding of the equipment to prevent electrical shocks. Before using any equipment, I carefully inspect it for any signs of damage or wear and tear. I make sure the work area is clean, organized, and free of obstacles. I’m always mindful of the potential hazards associated with the specific equipment, such as laser radiation from certain diagnostic tools or the potential for biological contamination from samples. A clear understanding and strict adherence to safety procedures are essential to protect both myself and others.
Q 4. How do you interpret the results from a diagnostic test?
Interpreting diagnostic test results requires a thorough understanding of the specific test and its limitations. I begin by reviewing the patient’s medical history and clinical presentation. Then, I analyze the numerical or visual data generated by the diagnostic test and compare it to the established reference ranges. This might involve identifying specific patterns or abnormalities. For example, an elevated white blood cell count might indicate an infection, while abnormal EKG readings could signify a cardiac issue. However, I always consider that test results should be interpreted within the context of the patient’s overall clinical picture. An isolated abnormal finding doesn’t automatically lead to a diagnosis. Often, I consult relevant literature and guidelines, and if necessary, discuss the results with other healthcare professionals to reach a comprehensive interpretation. I always emphasize the importance of critical thinking and the avoidance of making quick assumptions based on a single data point.
Q 5. What are the limitations of the diagnostic equipment you’ve used?
All diagnostic equipment has limitations. For instance, some blood tests might not detect all forms of a particular disease, resulting in false negatives. The sensitivity and specificity of a test, meaning its ability to correctly identify those with and without the condition, are always important factors. The accuracy of an imaging technique like X-ray can be affected by factors such as patient positioning and the presence of artifacts. Furthermore, equipment can be affected by environmental factors like temperature and humidity. Understanding these limitations is crucial for accurate interpretation of results. For example, a negative result on a screening test doesn’t rule out the presence of the disease entirely and may necessitate further diagnostic investigation. I meticulously document these limitations in my reports and always consider their impact when making clinical decisions.
Q 6. How do you ensure the accuracy and reliability of diagnostic test results?
Ensuring the accuracy and reliability of diagnostic test results involves several key steps. Regular calibration and maintenance of equipment are crucial, as described earlier. Using properly trained personnel is also important, as operator error can significantly affect results. Quality control procedures—like running control samples alongside patient samples—help identify any systematic issues with the equipment or reagents. Accurate sample handling and preparation are also vital. Furthermore, proper storage and handling of reagents are necessary to maintain their integrity and avoid contamination, which can lead to inaccurate results. Finally, meticulous record-keeping, including the proper labeling of samples and equipment maintenance logs, is crucial to maintaining traceability and transparency in the process.
Q 7. Describe a time you had to troubleshoot a complex diagnostic problem.
I once encountered a situation where a sophisticated hematology analyzer was producing inconsistent results, specifically concerning platelet counts. After initial troubleshooting steps, including checking reagents and calibration, the problem persisted. The discrepancy wasn’t related to the machine itself but involved the way blood samples were being processed. I realized that variations in the speed of centrifugation during sample preparation were affecting platelet aggregation, leading to inaccurate readings. The solution was straightforward, but it involved not only addressing the instrument but also reviewing the entire workflow. By implementing a standardized centrifugation protocol and ensuring meticulous adherence, we eliminated the variability, and the analyzer started producing consistent and reliable results. This experience underscored the importance of considering every step in the diagnostic process, not just the equipment itself.
Q 8. What software or systems are you proficient in for managing diagnostic data?
Managing diagnostic data effectively relies heavily on robust software and systems. My proficiency spans several platforms. I’m experienced with hospital information systems (HIS) like Epic and Cerner, which allow for seamless integration of diagnostic results into a patient’s overall medical record. These systems often include modules for managing radiology images (PACS – Picture Archiving and Communication Systems), laboratory results (LIS – Laboratory Information Systems), and cardiology data (including ECG and other cardiac studies). Beyond HIS/LIS/PACS, I’m also comfortable using dedicated diagnostic software packages specific to certain equipment, such as those provided by Siemens, GE, or Philips, which often have sophisticated data analysis and reporting features. For example, I’ve used Siemens’ syngo.via for advanced image processing and analysis in MRI and CT scans. Finally, I’m adept at using database management systems (DBMS) such as SQL to query and manipulate large diagnostic datasets for research and quality control purposes.
Q 9. Explain your experience with preventative maintenance on diagnostic equipment.
Preventative maintenance is crucial for ensuring the accuracy and longevity of diagnostic equipment. My approach is multifaceted and proactive. It begins with adhering strictly to the manufacturer’s recommended maintenance schedules, which often involve regular calibration checks, cleaning procedures, and software updates. I meticulously document all maintenance activities, including dates, procedures performed, and any findings. Beyond scheduled maintenance, I perform regular visual inspections for any signs of wear and tear, loose connections, or malfunctioning components. For instance, in working with ultrasound machines, I regularly check the probe for any damage and ensure proper transducer calibration. I’m also trained to identify potential problems before they escalate, using predictive maintenance techniques like analyzing equipment logs for unusual patterns or trends that might indicate impending failure. This allows for timely intervention and prevents costly downtime.
Q 10. How do you handle discrepancies or inconsistencies in diagnostic test results?
Inconsistencies in diagnostic test results demand a systematic approach. My first step is to meticulously review the entire testing process, looking for any procedural errors, such as incorrect patient identification, improper sample handling, or equipment malfunctions. I’ll cross-reference the results with the patient’s medical history and other relevant data to see if there are any confounding factors. If the discrepancy persists, I will repeat the test using a different piece of equipment, or if appropriate, a different testing method. For example, if an unusual blood test result arises, I might repeat the test and also request a different type of blood test to corroborate the findings. If the inconsistency still remains, I consult with other medical professionals, such as the attending physician or a specialist in the relevant field, to discuss potential causes and next steps. Thorough documentation is essential throughout this entire process.
Q 11. What are your preferred methods for documenting diagnostic test procedures and results?
My preferred methods for documenting diagnostic test procedures and results emphasize clarity, accuracy, and compliance. I use electronic medical record (EMR) systems extensively, entering all relevant information, including patient demographics, test requests, procedures performed, raw data, analyzed results, and any relevant interpretations. I adhere to standardized reporting formats to ensure consistency and readability. I also utilize image annotation tools within PACS systems to highlight key findings on radiological images, adding detailed textual descriptions when necessary. In cases where EMR systems are unavailable or insufficient, I rely on paper-based documentation following strict protocols that ensure legibility, accuracy, and chain of custody. Regardless of the method, my documentation always adheres to relevant regulatory standards such as HIPAA and other applicable guidelines.
Q 12. How do you stay current with the latest advancements in diagnostic technology?
Keeping up-to-date in the rapidly evolving field of diagnostic technology is a continuous process. I actively participate in professional development activities such as attending conferences and workshops. I regularly review peer-reviewed journals and reputable online resources to learn about new techniques, equipment, and software. I also engage in online continuing medical education (CME) courses specific to my areas of expertise. Moreover, I actively participate in professional organizations, such as the American Association for Clinical Chemistry (AACC) or the American College of Radiology (ACR), which offer access to educational materials, networking opportunities, and exposure to the latest advancements. In addition, I often collaborate with colleagues and vendors to gain insights and practical experience with the latest equipment and techniques.
Q 13. Describe your experience with different types of diagnostic equipment.
My experience encompasses a wide range of diagnostic equipment across various medical specialties. This includes extensive experience with imaging modalities such as X-ray, CT, MRI, ultrasound, and fluoroscopy. I’m also proficient in using laboratory equipment including automated analyzers for blood tests, microbiology equipment, and genetic testing platforms. In cardiology, I’m adept at operating and interpreting data from ECG machines, stress testing equipment, and echocardiography systems. My experience also extends to other areas, such as respiratory function testing equipment and neurodiagnostic tools. Each equipment type has its own nuances, requiring specific training and a deep understanding of its operational principles and limitations. My approach always prioritizes patient safety and accuracy of results.
Q 14. How do you determine which diagnostic test is appropriate for a specific situation?
Selecting the appropriate diagnostic test involves a careful consideration of several factors. First and foremost is the clinical question: What specific information are we trying to obtain? The patient’s medical history, presenting symptoms, and risk factors are all critical considerations. The availability of resources – such as the accessibility of specific equipment or testing facilities, as well as cost factors – needs to be weighed. I also factor in the test’s sensitivity and specificity, meaning its ability to correctly identify those with and without the condition in question. There are instances where multiple tests might be necessary to arrive at a definitive diagnosis. For example, if a patient presents with chest pain, I might consider an ECG, cardiac enzymes tests, and possibly a cardiac catheterization depending on the clinical context. It’s about a systematic process of gathering information that leads to the best possible care for the patient.
Q 15. How do you communicate diagnostic test results to non-technical personnel?
Communicating complex diagnostic test results to non-technical personnel requires clear, concise language and a focus on the practical implications. I avoid using technical jargon and instead employ analogies and visualizations to illustrate key findings. For instance, if explaining blood test results showing elevated cholesterol, instead of saying “HDL levels are below the optimal range,” I might say, “Your “good” cholesterol is a little low, which means your body isn’t clearing fat as efficiently as it should. This increases the risk of heart problems, similar to how a clogged drain slows water flow.”
I also emphasize the “so what?” – the significance of the results for the patient’s health and well-being. I present the information in a way that empowers the individual to understand their condition and participate actively in their care. This often involves providing a written summary alongside verbal explanation, using charts or graphs to visually represent data where appropriate. For example, a graph comparing current results against previous tests can highlight trends and changes.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is your experience with regulatory compliance related to diagnostic equipment?
My experience with regulatory compliance related to diagnostic equipment is extensive. I’m thoroughly familiar with regulations like CLIA (Clinical Laboratory Improvement Amendments), HIPAA (Health Insurance Portability and Accountability Act), and relevant ISO standards, particularly ISO 15189 for medical laboratories. I understand the importance of maintaining accurate records, ensuring equipment calibration and preventative maintenance are rigorously documented, and adhering to strict quality control procedures.
In my previous role, I was responsible for ensuring our laboratory’s compliance with all relevant regulations. This involved creating and maintaining detailed equipment logs, conducting regular quality control checks, and participating in internal audits. I have personally handled instances of equipment malfunction and followed established protocols to promptly report issues, conduct thorough investigations, and implement corrective actions, all while ensuring compliance with the relevant regulations. I am also familiar with the requirements for equipment validation, ensuring that any new equipment meets the required standards for accuracy and reliability before being put into service.
Q 17. How do you prioritize tasks when working with multiple pieces of diagnostic equipment?
Prioritizing tasks when managing multiple diagnostic instruments involves a structured approach. I utilize a system that combines urgency and importance. I employ a prioritization matrix where tasks are categorized based on their urgency (immediate, short-term, long-term) and importance (critical, high, medium, low) to the overall workflow.
For example, a malfunctioning instrument used for urgent patient samples would be prioritized above a routine maintenance check on another instrument, even if the latter is technically overdue. I also factor in factors like the number of patients affected and potential delays to their care. This system allows me to dynamically adjust my workload as circumstances change and maintain efficiency. Effective time management and the ability to delegate tasks (where possible) are also key components of this workflow.
Q 18. Describe your problem-solving approach when dealing with a malfunctioning diagnostic instrument.
My problem-solving approach when dealing with malfunctioning diagnostic instruments follows a systematic process. Firstly, I thoroughly assess the problem. This involves checking the instrument’s error codes, reviewing the operation log, and visually inspecting for any apparent physical damage. Then, I consult the equipment’s troubleshooting manual and manufacturer’s guidelines.
If the problem persists after following the manual’s steps, I systematically check the power supply, connections, and reagent supplies. If the problem still remains, I document all steps taken and escalate the issue to the appropriate technician or service provider. Throughout the process, I meticulously document each step, observation, and any attempted solutions. This detailed documentation is crucial for effective troubleshooting and minimizes downtime. I also prioritize patient safety, ensuring that any affected tests are repeated if necessary using backup equipment or an alternative method.
Q 19. What are the potential sources of error in diagnostic testing, and how do you mitigate them?
Potential sources of error in diagnostic testing are numerous and can be broadly categorized into pre-analytical, analytical, and post-analytical phases. Pre-analytical errors encompass issues like improper sample collection, storage, or transportation. Analytical errors involve instrument malfunction, reagent degradation, or incorrect calibration. Post-analytical errors might include data entry mistakes, reporting delays, or misinterpretation of results.
Mitigating these errors requires a multi-pronged strategy. This includes rigorous training of personnel on proper sample handling techniques, implementing quality control measures using control samples with known values, regularly calibrating and maintaining diagnostic equipment according to manufacturer recommendations, and establishing robust quality assurance protocols for data handling and reporting. Regular audits and review of standard operating procedures (SOPs) are also essential for ongoing process improvements and error reduction.
Q 20. How do you ensure the proper handling and storage of diagnostic equipment and samples?
Proper handling and storage of diagnostic equipment and samples are paramount for maintaining test accuracy and integrity. Equipment should always be handled according to the manufacturer’s instructions. This includes proper cleaning and disinfection protocols, careful handling to prevent damage, and following specific instructions for storage and transportation. Regular preventative maintenance is also vital.
Samples require careful handling based on their type and the specific test being performed. This includes adhering to specific temperature requirements (refrigeration, freezing, or room temperature), using appropriate collection and storage containers to prevent contamination, and minimizing exposure to light or extreme temperatures. Accurate labeling and meticulous record-keeping are crucial for maintaining sample traceability and integrity. The storage areas must meet environmental standards, and proper inventory management prevents sample degradation or loss.
Q 21. What is your understanding of quality control measures in diagnostic testing?
Quality control (QC) measures are the cornerstone of accurate and reliable diagnostic testing. QC encompasses various procedures and processes designed to ensure the accuracy and reliability of test results. This includes internal quality controls, where known samples (control samples) with expected results are tested alongside patient samples to monitor the performance of the instrument and reagents. External quality assessment (EQA) programs involve participating in proficiency testing where laboratories compare their results with those of other labs using the same tests to evaluate performance.
These QC measures help identify potential problems such as instrument malfunction, reagent degradation, or technician errors before they affect patient results. Documentation of QC activities, including results and corrective actions, is crucial for maintaining traceability and demonstrates compliance with regulatory standards. Furthermore, regular review and analysis of QC data provide opportunities for continuous improvement and optimization of laboratory procedures.
Q 22. Describe your experience with data analysis and interpretation from diagnostic equipment.
Data analysis from diagnostic equipment involves extracting meaningful insights from raw data to inform diagnoses and treatment plans. This process begins with understanding the equipment’s output format – be it numerical readings, waveforms, or images. I’m proficient in using various software packages and algorithms to process this data. For instance, in analyzing an electrocardiogram (ECG), I utilize software to identify abnormalities in heart rhythm, such as arrhythmias, by examining the amplitude, duration, and frequency of different waveforms. Similarly, with medical imaging, I utilize image processing techniques to enhance visualization, identify lesions, or quantify tissue characteristics. Interpretation requires a solid foundation in the underlying physiological principles and an understanding of the equipment’s limitations and potential sources of error. For example, artifacts in an ultrasound image could be misinterpreted as pathology if not carefully assessed. My experience includes analyzing data from a wide range of equipment including blood gas analyzers, X-ray machines, and various laboratory analyzers, always ensuring rigorous quality control measures are in place to validate results.
For example, in a recent case, I was able to detect a subtle but significant variation in the patient’s blood oxygen saturation levels using a pulse oximeter’s data trend analysis, leading to the early identification of a developing respiratory issue. This timely discovery enabled prompt intervention and improved patient outcomes. I frequently use statistical methods to analyze data sets, looking for trends and correlations that might indicate the need for further investigation.
Q 23. How do you identify and address potential safety hazards associated with diagnostic equipment?
Safety is paramount when working with diagnostic equipment. My approach involves a multi-faceted strategy focusing on proactive hazard identification and mitigation. This includes regular equipment inspections to identify potential issues like frayed wires, loose connections, or malfunctioning safety features. I’m meticulous about adhering to manufacturer’s safety guidelines and all relevant safety protocols. I’m trained in electrical safety, radiation safety (for X-ray and other ionizing radiation equipment), and laser safety, as appropriate to the equipment. Before using any equipment, I always check for proper grounding and ensure that safety interlocks are functional. I’m also trained in emergency procedures and know how to respond to electrical shocks, radiation exposure incidents, or equipment malfunctions. Furthermore, I regularly participate in safety training and refreshers to keep my knowledge up-to-date with evolving safety standards and best practices.
For instance, if I notice a malfunctioning ground connection on an ECG machine, I immediately isolate the device and report the issue. I never proceed with operation until the issue is addressed by a qualified technician. A well-defined reporting system is crucial for tracking potential hazards and preventing future incidents.
Q 24. Explain your familiarity with different types of sensors and transducers used in diagnostic systems.
Diagnostic systems rely heavily on a wide range of sensors and transducers to convert physical parameters into measurable signals. My familiarity spans various types, including:
- Temperature sensors: Thermistors, thermocouples, and infrared sensors are used in applications ranging from blood gas analyzers to thermal imaging.
- Pressure sensors: Piezoresistive, capacitive, and strain-gauge sensors are critical for blood pressure monitoring, respiratory function analysis, and other physiological measurements.
- Optical sensors: Photodiodes, photomultipliers, and CCD/CMOS sensors are employed in various imaging modalities, including X-ray, ultrasound, and endoscopy.
- Electrochemical sensors: These are widely used in blood gas analysis and other clinical chemistry applications to measure pH, blood gases (oxygen and carbon dioxide), and electrolytes.
- Ultrasound transducers: These piezoelectric devices convert electrical energy into ultrasonic waves and vice-versa, enabling the production and reception of ultrasound images.
Understanding the operating principles of different sensors and their limitations, such as sensitivity, accuracy, and response time, is essential for interpreting results accurately. I have experience working with both invasive and non-invasive sensing techniques. For example, I know the differences in signal processing requirements for a fiber-optic sensor vs. a conventional electrical sensor.
Q 25. How do you troubleshoot connectivity issues with diagnostic equipment and networks?
Troubleshooting connectivity issues requires a systematic approach. I start by verifying the most basic elements: Are the cables properly connected? Are the devices powered on? I check for obvious physical damage to cables or ports. Then, I progress to more advanced troubleshooting, utilizing diagnostic tools and techniques. This could involve examining network settings, IP addresses, subnet masks, and gateway configurations. I utilize network diagnostic tools such as packet analyzers and network scanners to identify network bottlenecks or connectivity problems. I also understand different network protocols like TCP/IP and various communication standards specific to medical equipment. With some diagnostic devices, specialized software may provide detailed logs about connectivity attempts and errors. Reviewing these logs can often pinpoint the root cause of the problem.
For example, if a diagnostic device isn’t communicating with the network, I would check its network configuration against the network’s configuration to identify any discrepancies. I’d then test the network cable using a cable tester and verify network connectivity from the device’s location using a ping command or a network scanner. Finally, I would consult the equipment’s manual for troubleshooting guidance and, if necessary, contact the manufacturer’s support.
Q 26. Describe your experience with different diagnostic protocols and standards.
My experience encompasses several diagnostic protocols and standards, including:
- DICOM (Digital Imaging and Communications in Medicine): This standard governs the storage, transmission, and display of medical images.
- HL7 (Health Level Seven): This standard facilitates the exchange of clinical and administrative data between healthcare systems.
- IEEE 1073 (Standard for Healthcare Devices): This standard defines communication protocols for medical devices.
- Various manufacturer-specific protocols: Different equipment manufacturers may use proprietary protocols, which I have experience working with.
Understanding these protocols is crucial for ensuring seamless data integration and interoperability between different diagnostic systems. Knowing the nuances of these standards allows me to analyze data from diverse sources, interpret results effectively, and manage data flow within complex healthcare information systems.
Q 27. What is your experience with performing routine checks and maintenance on diagnostic equipment?
Routine checks and maintenance are vital for ensuring the accuracy, reliability, and safety of diagnostic equipment. My experience includes performing preventative maintenance tasks such as cleaning and disinfecting equipment according to manufacturer guidelines, inspecting cables and connections for damage, and verifying the functionality of safety interlocks. I’m also skilled in performing calibrations and quality control checks using standardized procedures and reference materials. Calibration ensures the accuracy of measurements, while quality control checks help identify and correct any deviations from expected performance. I maintain detailed records of all maintenance activities, including dates, performed tasks, and any identified issues. This documentation is essential for tracking equipment history and ensuring regulatory compliance.
For example, I regularly calibrate blood glucose meters and other point-of-care testing devices using standardized controls to verify accuracy. I also adhere to stringent protocols for managing and disposing of biohazardous materials safely.
Q 28. How would you approach training a new technician on using specific diagnostic equipment?
Training a new technician involves a structured approach combining theoretical knowledge and hands-on experience. I would begin with a review of relevant safety protocols and regulations followed by an overview of the equipment’s operating principles. This would include explanations of how the equipment functions, its various components, and its intended applications. Then, I would move to hands-on training, gradually increasing the complexity of the tasks assigned. I’d start with simple tasks under my supervision before allowing the trainee to perform tasks independently. Throughout the training process, I would emphasize the importance of accuracy and attention to detail, and I would use both demonstration and practice sessions. Regular assessments are vital for gauging the trainee’s progress and addressing any knowledge gaps. I’d also encourage the trainee to ask questions and provide constructive feedback to ensure they’re comfortable and confident in their abilities. Finally, I would provide access to relevant documentation and resources to support their continued learning. The aim is to empower the technician with the competence and confidence to use the equipment safely and effectively.
For example, when training on an ultrasound machine, I would start with demonstrating basic image acquisition techniques on phantoms (simulated tissue models) before moving to actual patient cases under direct supervision.
Key Topics to Learn for Proficient in using diagnostic and testing equipment Interview
- Understanding Equipment Functionality: Thoroughly grasp the theoretical principles behind the operation of various diagnostic and testing equipment relevant to your field. This includes understanding how each piece of equipment works, its limitations, and potential sources of error.
- Calibration and Maintenance Procedures: Demonstrate knowledge of proper calibration techniques and routine maintenance procedures for optimal equipment performance. Be prepared to discuss troubleshooting common malfunctions and performing minor repairs.
- Data Interpretation and Analysis: Practice interpreting data generated by the equipment. Focus on identifying trends, anomalies, and drawing meaningful conclusions from the results. Develop strong data visualization skills to effectively communicate your findings.
- Safety Protocols and Regulations: Showcase your understanding of relevant safety regulations and protocols associated with the operation and maintenance of diagnostic and testing equipment. Highlight your commitment to safe work practices.
- Practical Application and Case Studies: Prepare examples from your experience where you successfully used diagnostic and testing equipment to solve problems or contribute to a project. Quantify your accomplishments whenever possible.
- Troubleshooting and Problem-Solving: Be ready to discuss your approach to troubleshooting equipment malfunctions. Describe your systematic problem-solving methodology, including how you identify the root cause of issues and implement effective solutions.
- Emerging Technologies and Trends: Stay updated on the latest advancements in diagnostic and testing equipment and technologies. Demonstrating awareness of new tools and techniques shows initiative and a commitment to professional development.
Next Steps
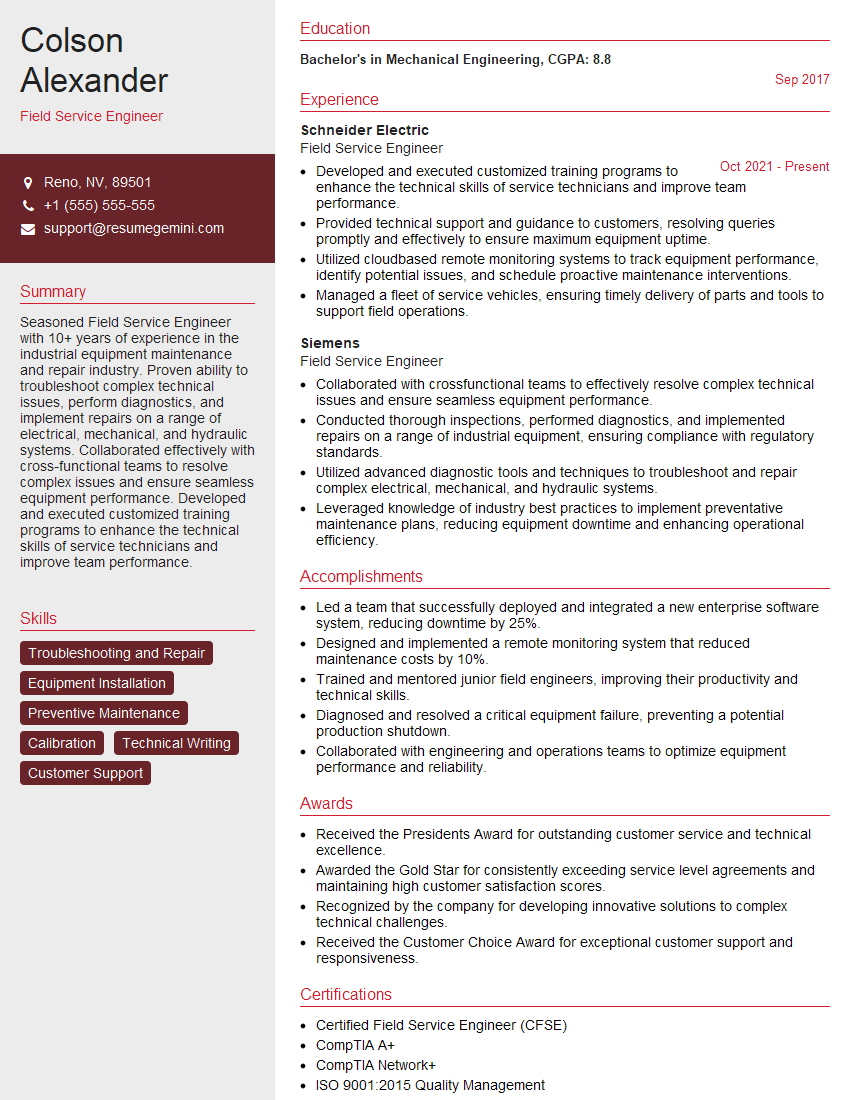
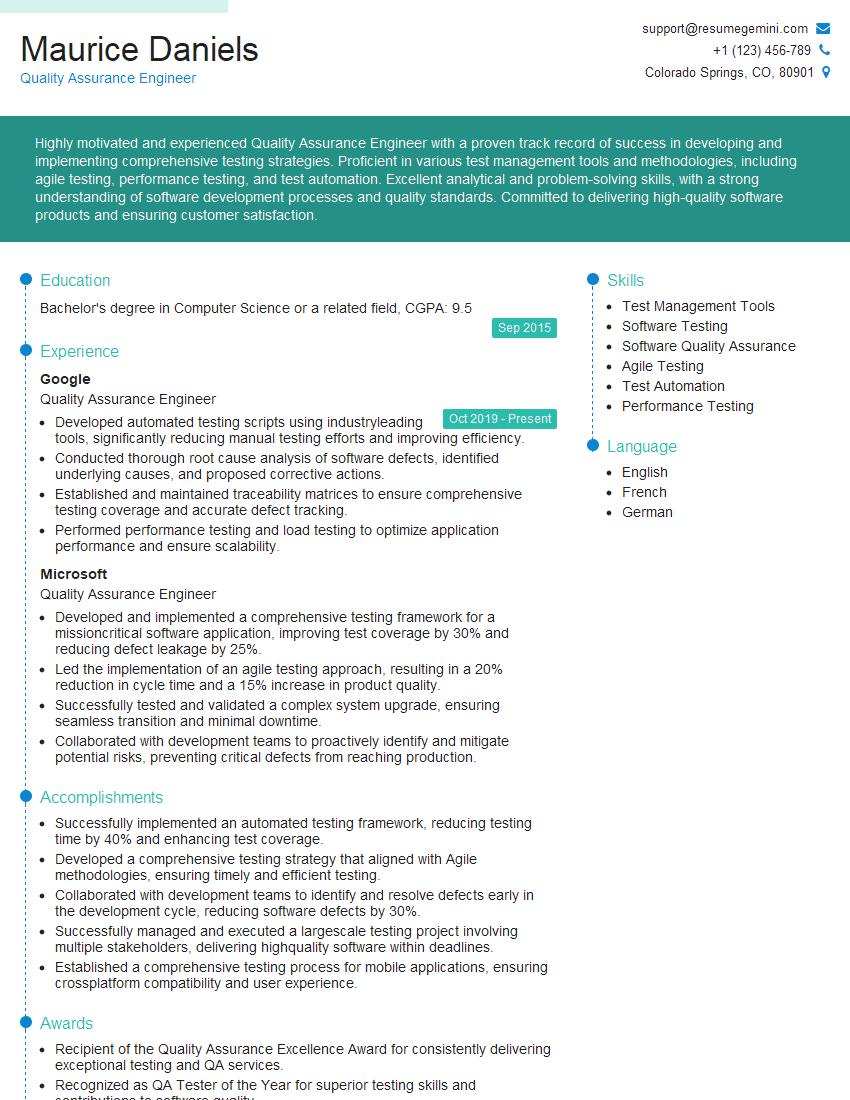
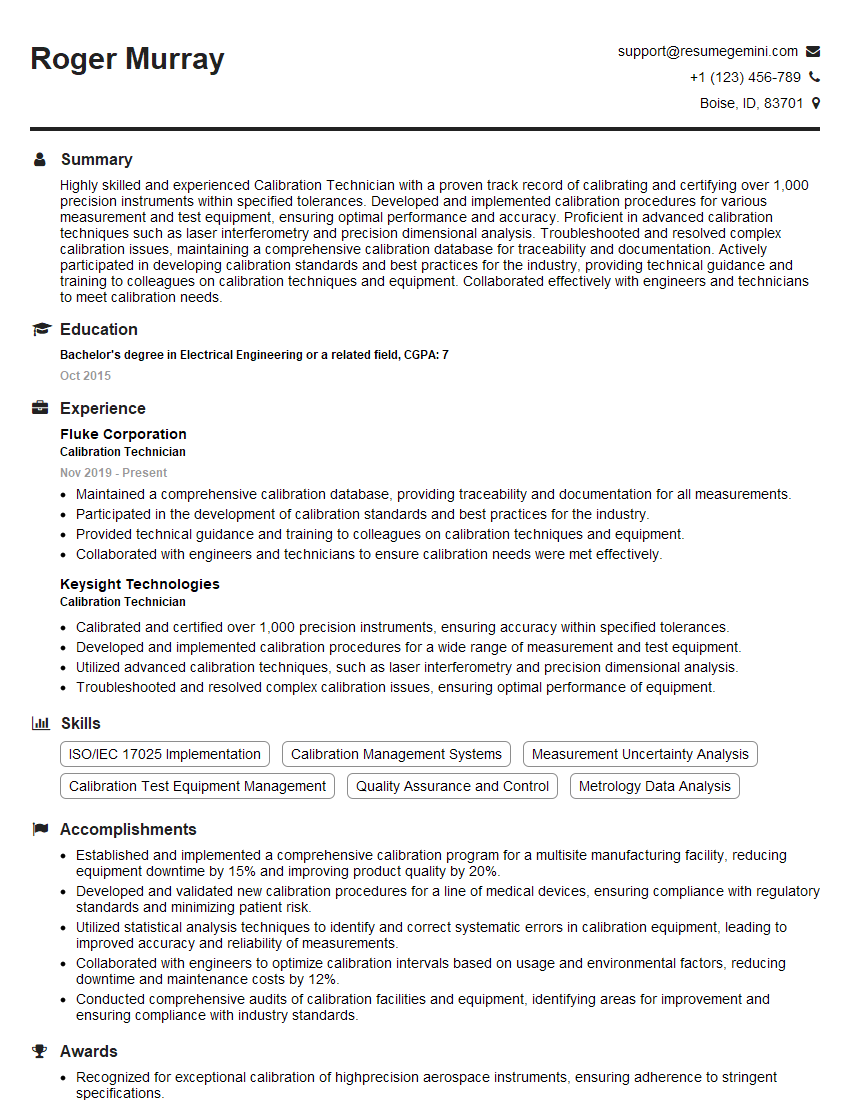
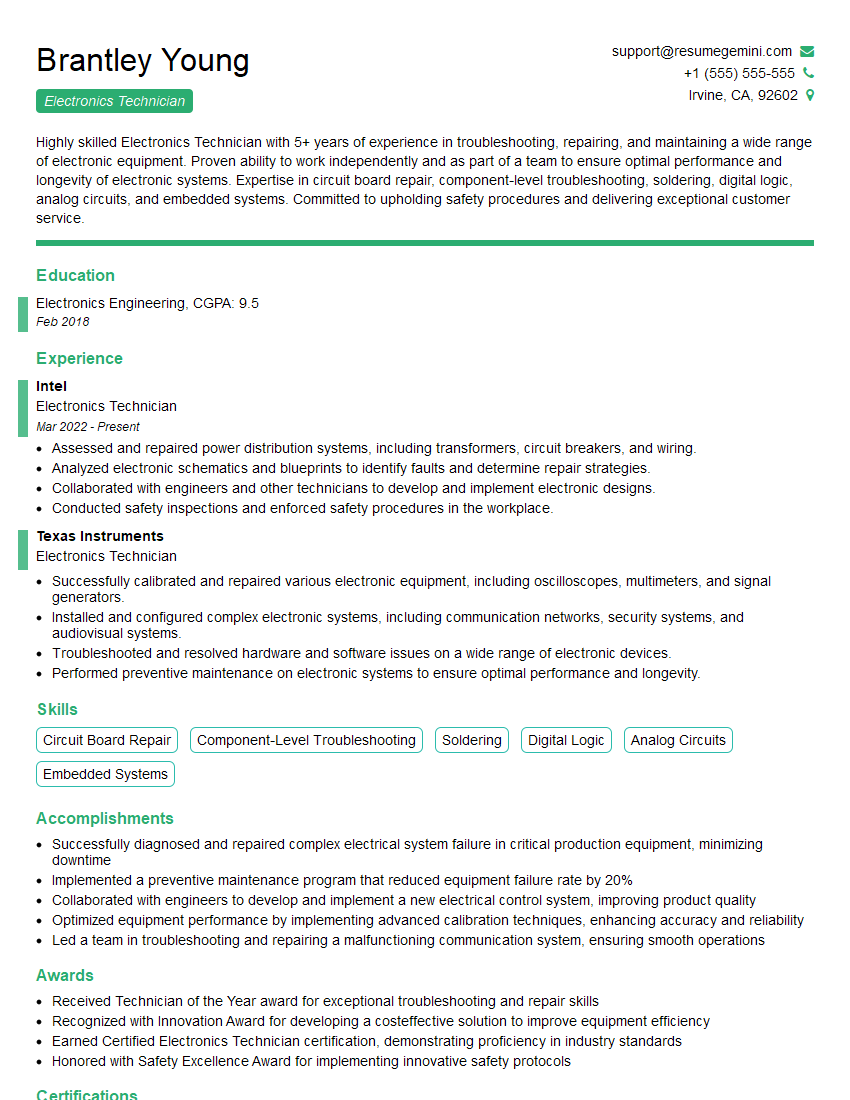
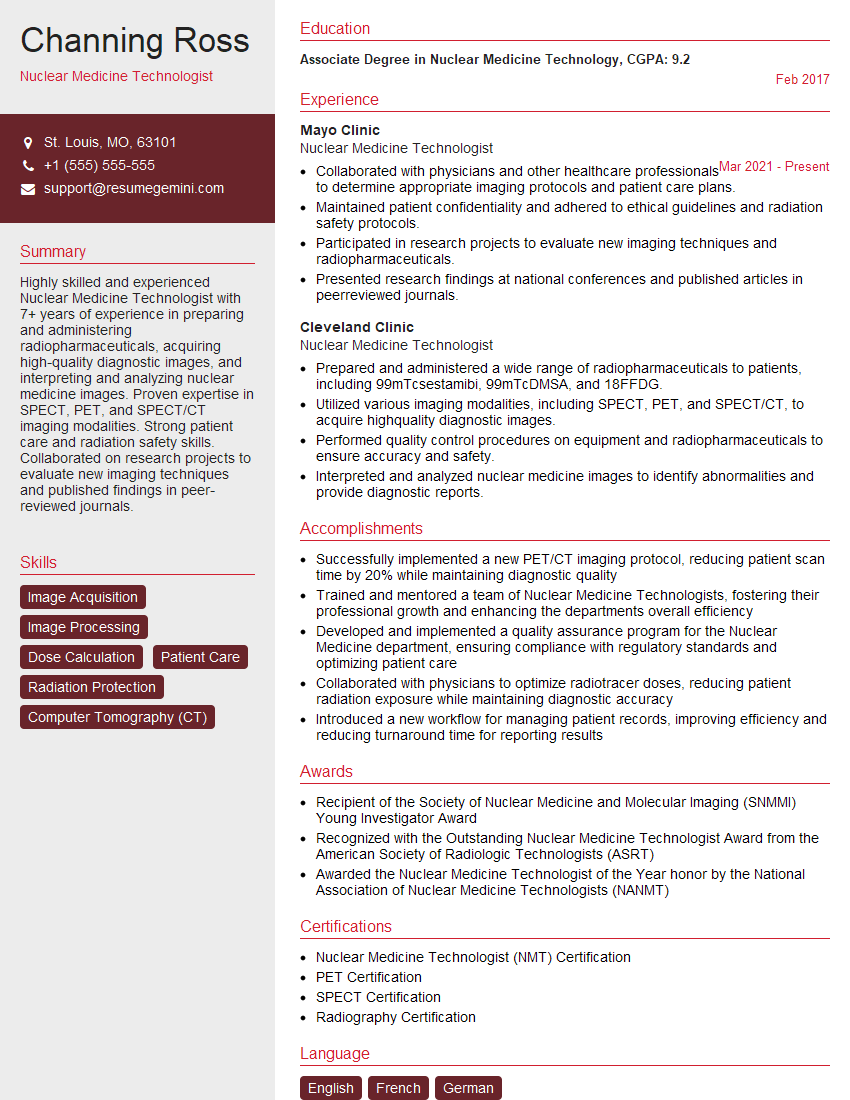
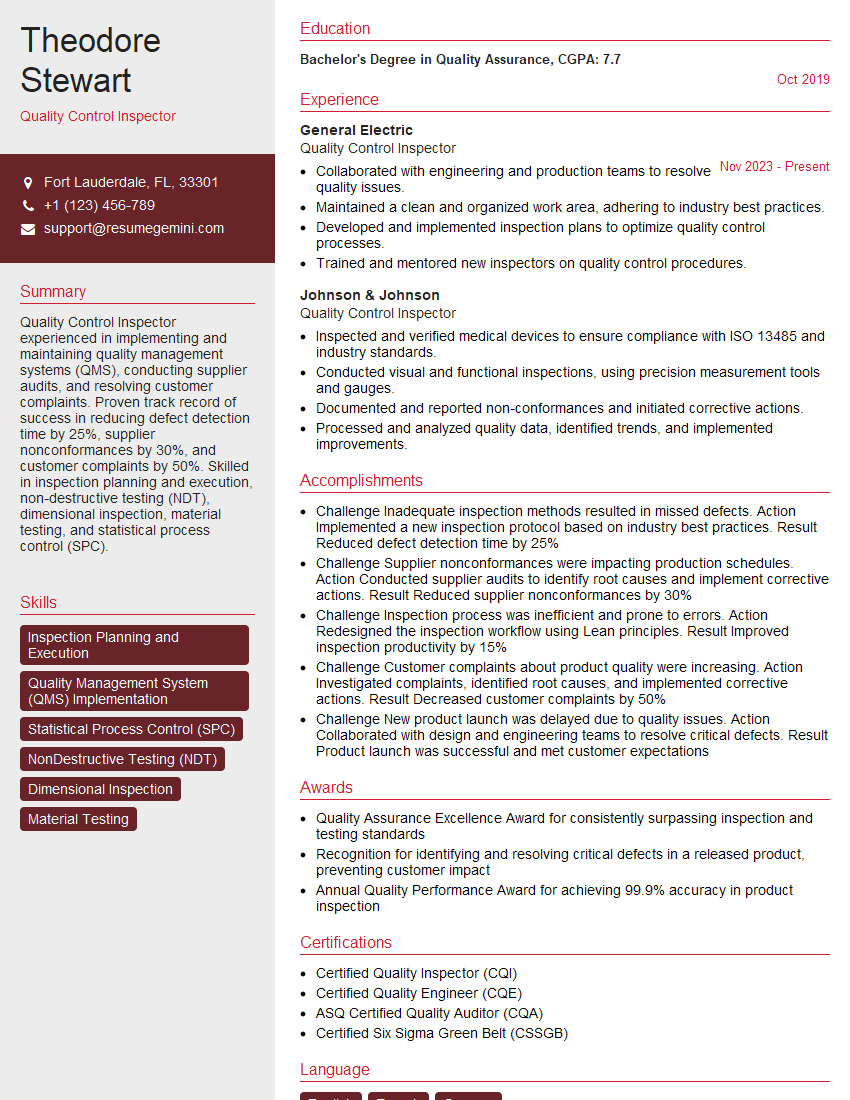
Mastering the use of diagnostic and testing equipment is crucial for career advancement in many fields. A strong command of this skillset opens doors to more challenging roles and higher earning potential. To maximize your job prospects, create a compelling and ATS-friendly resume that effectively highlights your expertise. ResumeGemini is a trusted resource that can help you build a professional resume that showcases your skills and experience. We offer examples of resumes tailored to “Proficient in using diagnostic and testing equipment” to guide you in creating a document that will impress potential employers. Invest the time to craft a strong resume – it’s your first impression and a critical step in landing your dream job.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO