Preparation is the key to success in any interview. In this post, we’ll explore crucial Reproductive Physiology interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Reproductive Physiology Interview
Q 1. Explain the hormonal control of the menstrual cycle.
The menstrual cycle is a complex interplay of hormones orchestrated primarily by the hypothalamus, pituitary gland, and ovaries. It’s a roughly 28-day cycle (although this varies significantly between individuals) that prepares the female body for potential pregnancy. Let’s break down the hormonal control:
- Follicular Phase (Days 1-14): This phase begins with menstruation (shedding of the uterine lining). The hypothalamus releases GnRH (gonadotropin-releasing hormone), stimulating the pituitary gland to release FSH (follicle-stimulating hormone) and a smaller amount of LH (luteinizing hormone). FSH promotes the growth of ovarian follicles, each containing an immature egg. As follicles mature, they produce increasing amounts of estrogen. Estrogen levels rise gradually, causing the uterine lining (endometrium) to thicken and prepare for potential implantation of a fertilized egg. The rising estrogen also triggers a surge in LH production towards the end of the follicular phase.
- Ovulation (Day 14): The LH surge triggers ovulation – the release of the mature egg from the follicle. This usually occurs around day 14, but can vary.
- Luteal Phase (Days 15-28): The ruptured follicle transforms into the corpus luteum, which produces significant amounts of progesterone and some estrogen. Progesterone further thickens the endometrium, making it receptive for implantation. If fertilization doesn’t occur, the corpus luteum degenerates, resulting in a decrease in progesterone and estrogen. This hormonal drop triggers menstruation, starting the cycle anew. If fertilization does occur, the corpus luteum is maintained by human chorionic gonadotropin (hCG), produced by the developing embryo. This prevents menstruation and sustains the pregnancy.
Think of it like this: FSH is the gardener preparing the soil (follicles), estrogen is the fertilizer promoting growth, LH is the trigger for harvesting (ovulation), and progesterone is the caretaker ensuring a healthy environment (endometrium) for potential implantation.
Q 2. Describe the process of oogenesis.
Oogenesis is the process of female gamete (egg) formation. Unlike spermatogenesis, which occurs continuously throughout a male’s reproductive life, oogenesis begins during fetal development and is largely completed by birth. The process involves:
- Prenatal Development: Oogonia, the primordial germ cells, undergo mitosis, producing millions of germ cells. Many of these then undergo meiosis I, stopping at prophase I. These are now called primary oocytes. They remain arrested in prophase I until puberty.
- Puberty and beyond: At puberty, the hypothalamus-pituitary-gonadal axis activates, and FSH stimulates the maturation of a few primary oocytes each menstrual cycle. Meiosis I resumes, resulting in a secondary oocyte and a first polar body (a small cell containing discarded genetic material). The secondary oocyte proceeds to metaphase II but arrests again until fertilization.
- Fertilization: If fertilization occurs, meiosis II completes, producing a mature ovum (egg) and a second polar body. The mature ovum then fuses with the sperm to form a zygote.
Essentially, oogenesis is a lengthy process, starting before birth and only completing if fertilization occurs. The unequal division of cytoplasm ensures that one cell receives the majority of the nutrients needed for embryonic development.
Q 3. Detail the stages of spermatogenesis.
Spermatogenesis is the process of sperm formation in the testes. It’s a continuous process throughout a male’s reproductive life, beginning at puberty and continuing until death. The process involves:
- Spermatocytogenesis: Spermatogonia (diploid germ cells) in the seminiferous tubules undergo mitosis, creating a pool of cells. Some spermatogonia differentiate into primary spermatocytes (diploid).
- Meiosis I: Primary spermatocytes undergo meiosis I, resulting in two haploid secondary spermatocytes.
- Meiosis II: Secondary spermatocytes undergo meiosis II, producing four haploid spermatids.
- Spermiogenesis: Spermatids undergo a complex differentiation process, transforming into mature spermatozoa (sperm). This includes the development of the head (containing the nucleus and acrosome), midpiece (containing mitochondria), and tail (for motility).
This intricate process ensures the continuous production of millions of sperm, each carrying half the genetic information required for fertilization. The efficiency of spermatogenesis is crucial for male fertility.
Q 4. What are the key differences between meiosis and mitosis in germ cell development?
Meiosis and mitosis are both types of cell division, but they have distinct roles in germ cell development. The key differences are:
- Number of Divisions: Mitosis involves one round of division, resulting in two identical diploid daughter cells. Meiosis involves two rounds of division (Meiosis I and Meiosis II), resulting in four genetically distinct haploid daughter cells.
- Genetic Variation: Mitosis produces genetically identical cells. Meiosis produces genetically diverse cells due to crossing over (exchange of genetic material between homologous chromosomes) during meiosis I and independent assortment (random alignment of homologous chromosomes) during metaphase I.
- Chromosome Number: Mitosis maintains the diploid chromosome number (2n). Meiosis reduces the chromosome number by half, producing haploid cells (n).
- Role in Germ Cell Development: Mitosis is involved in the proliferation of germ cells (e.g., spermatogonia and oogonia). Meiosis is essential for producing gametes (sperm and egg) with half the number of chromosomes, so that during fertilization, the diploid chromosome number is restored in the zygote.
In essence, mitosis creates copies, while meiosis generates diversity and reduces the chromosome number, both vital processes for sexual reproduction.
Q 5. Explain the role of the hypothalamus-pituitary-gonadal axis.
The hypothalamus-pituitary-gonadal (HPG) axis is the feedback loop that regulates the reproductive system in both males and females. It involves:
- Hypothalamus: Releases GnRH (gonadotropin-releasing hormone), which stimulates the pituitary gland.
- Pituitary Gland: Releases FSH (follicle-stimulating hormone) and LH (luteinizing hormone), which stimulate the gonads (testes or ovaries).
- Gonads (Testes/Ovaries): Produce sex hormones (testosterone in males, estrogen and progesterone in females), which exert feedback effects on the hypothalamus and pituitary, regulating hormone production. Negative feedback mechanisms maintain hormone levels within a specific range.
This intricate feedback system ensures appropriate hormone levels to maintain reproductive function. For example, high levels of testosterone will negatively feedback on the hypothalamus and pituitary to reduce GnRH, FSH, and LH release, thus regulating testosterone production. Disruptions in this axis can lead to various reproductive disorders.
Q 6. Describe the mechanisms of fertilization.
Fertilization is the fusion of a sperm and an egg, resulting in a zygote. The process is intricate and involves several steps:
- Sperm Capacitation: Sperm undergo changes in the female reproductive tract, increasing their motility and ability to fertilize the egg.
- Penetration of the Corona Radiata: Sperm use their motility to navigate through the corona radiata, a layer of follicular cells surrounding the egg.
- Acrosome Reaction: Enzymes from the acrosome (a cap-like structure on the sperm head) are released, digesting the zona pellucida, a glycoprotein layer surrounding the egg.
- Sperm-Egg Fusion: The sperm membrane fuses with the egg membrane, and the sperm nucleus enters the egg cytoplasm.
- Cortical Reaction: The egg undergoes changes to prevent polyspermy (fertilization by multiple sperm).
- Syngamy: The sperm and egg nuclei fuse, forming a zygote with a diploid chromosome number.
The entire process is finely tuned, and the failure of any of these steps can result in infertility. The acrosome reaction, for example, is critical for sperm penetration, and its failure is a common cause of infertility.
Q 7. What are the different types of infertility and their causes?
Infertility is defined as the inability to conceive after 12 months of regular unprotected intercourse. There are numerous causes, affecting both males and females. Here are some examples:
- Female Infertility:
- Ovulatory Dysfunction: Irregular or absent ovulation due to hormonal imbalances (e.g., PCOS), hypothalamic dysfunction, or premature ovarian failure.
- Tubal Blockage: Blockage of the fallopian tubes due to infection (e.g., pelvic inflammatory disease), endometriosis, or previous surgery.
- Endometriosis: Presence of endometrial tissue outside the uterus, interfering with ovulation and implantation.
- Uterine Factors: Structural abnormalities of the uterus (e.g., fibroids, polyps) or uterine scarring.
- Male Infertility:
- Low Sperm Count (Oligospermia): Reduced number of sperm in the ejaculate.
- Poor Sperm Motility (Asthenospermia): Reduced sperm movement.
- Abnormal Sperm Morphology (Teratospermia): High percentage of abnormally shaped sperm.
- Varicocele: Enlargement of the veins within the scrotum, leading to increased testicular temperature and impaired sperm production.
- Unexplained Infertility: No identifiable cause can be found after thorough investigation.
Diagnosis and treatment of infertility require a comprehensive evaluation of both partners. Treatments range from lifestyle changes and medication to assisted reproductive technologies (ART) such as IVF (in-vitro fertilization).
Q 8. Explain the process of in-vitro fertilization (IVF).
In-vitro fertilization (IVF) is a complex process that helps couples conceive when natural methods fail. Think of it as mimicking fertilization outside the body. The process begins with ovarian stimulation using fertility drugs to produce multiple mature eggs. These eggs are then retrieved from the ovaries using a needle guided by ultrasound. Simultaneously, a semen sample is collected from the partner or donor. In the lab, the eggs are carefully mixed with the sperm in a petri dish, allowing fertilization to occur. After a few days, one or more healthy embryos are selected and transferred back into the woman’s uterus using a thin catheter. Finally, a pregnancy test is performed several weeks later to determine if the procedure was successful. It’s crucial to note that each step requires careful monitoring and precise techniques for optimal success rates.
- Ovarian Stimulation: Involves administering medications to increase egg production.
- Egg Retrieval: A minimally invasive procedure using ultrasound guidance.
- Fertilization: Mixing eggs and sperm in a controlled laboratory setting.
- Embryo Transfer: Transferring selected embryos back into the uterus.
Q 9. Describe the techniques used in assisted reproductive technology (ART).
Assisted Reproductive Technology (ART) encompasses a range of procedures aimed at helping individuals or couples overcome infertility. IVF, as discussed above, is a prominent example. Other techniques include:
- Gamete Intrafallopian Transfer (GIFT): Eggs and sperm are placed directly into the fallopian tubes, allowing fertilization to occur naturally within the body.
- Zygote Intrafallopian Transfer (ZIFT): Similar to GIFT, but fertilized eggs (zygotes) are transferred into the fallopian tubes.
- Intracytoplasmic Sperm Injection (ICSI): A single sperm is directly injected into an egg to facilitate fertilization, often used when male factor infertility is a concern.
- Intrauterine Insemination (IUI): Sperm is directly introduced into the uterus, bypassing the cervix, increasing the chances of sperm reaching the egg.
- Preimplantation Genetic Testing (PGT): Genetic testing performed on embryos before implantation to screen for chromosomal abnormalities or genetic diseases.
The choice of ART technique depends on various factors, including the cause of infertility, the couple’s age, and their preferences. A fertility specialist will guide the couple in choosing the most appropriate option.
Q 10. What are the ethical considerations surrounding ART?
Ethical considerations surrounding ART are complex and multifaceted. Key concerns include:
- Multiple Births: The increased risk of multiple pregnancies with some ART procedures raises ethical questions regarding the health and well-being of both the mother and the babies.
- Embryo Selection and Disposition: Decisions about which embryos to implant and what to do with surplus embryos raise questions about the moral status of embryos.
- Genetic Screening and Selection: PGT allows for the selection of embryos based on genetic characteristics, potentially leading to concerns about genetic discrimination and designer babies.
- Access and Equity: The high cost of ART raises concerns about equitable access for all individuals and couples who need it.
- Third-Party Involvement: The use of egg donors, sperm donors, and gestational carriers raises complex ethical and legal issues regarding parental rights and responsibilities.
These ethical considerations are constantly debated and refined as technology advances. Open communication between healthcare providers, patients, and ethicists is crucial for navigating these challenges.
Q 11. Explain the role of hormones in implantation.
Hormones play a critical role in successful implantation. The process begins with the blastocyst (the early embryo) secreting factors that signal the uterine lining to prepare for implantation. Crucially, progesterone, secreted by the corpus luteum (a temporary gland in the ovary) and later by the placenta, is essential for maintaining the endometrium (uterine lining) in a receptive state. Estrogen, produced by the ovaries and placenta, also plays a supportive role in endometrial development. Other hormones like human chorionic gonadotropin (hCG), produced by the developing embryo, are essential for maintaining the pregnancy and triggering the corpus luteum to continue producing progesterone. A balance of these hormones is necessary for successful implantation and the subsequent maintenance of pregnancy.
Think of it like this: progesterone prepares the ‘soil’ (endometrium) while estrogen helps with its ‘fertility’. hCG then signals for the ‘gardeners’ (corpus luteum and later placenta) to keep nurturing the developing pregnancy.
Q 12. Describe the process of embryonic development.
Embryonic development is a remarkable process of cellular division, differentiation, and morphogenesis. Following fertilization, the zygote undergoes rapid cell divisions (cleavage) as it travels down the fallopian tube. This forms a morula, a solid ball of cells. The morula then develops into a blastocyst, a hollow sphere of cells with an inner cell mass (which will form the embryo) and an outer trophoblast (which will form the placenta). Implantation occurs when the blastocyst attaches to the uterine wall. Following implantation, the three germ layers (ectoderm, mesoderm, and endoderm) form, from which all organs and tissues will develop. This period of organogenesis is crucial for proper development and is highly susceptible to environmental influences and genetic factors. Subsequent development involves further differentiation, growth, and refinement of organ systems leading to the formation of a fetus.
Q 13. What are the key markers of pregnancy?
Key markers of pregnancy include:
- Missed Menstrual Period: The most common and earliest sign.
- Positive Pregnancy Test: Detects the presence of hCG in urine or blood.
- Morning Sickness: Nausea and vomiting, often in the first trimester.
- Breast Changes: Breast tenderness, swelling, and darkening of the areola.
- Fatigue: Increased tiredness and sleepiness.
- Frequent Urination: Due to increased blood volume.
- Ultrasound Confirmation: Visual confirmation of a developing fetus within the uterus.
It’s important to note that some of these symptoms can be caused by other factors; a positive pregnancy test is the most reliable indicator.
Q 14. Explain the hormonal changes during pregnancy.
Pregnancy is characterized by profound hormonal changes, primarily driven by the placenta. hCG levels rise dramatically early in pregnancy, maintaining the corpus luteum and stimulating progesterone production. Progesterone levels remain elevated throughout pregnancy, promoting the maintenance of the endometrium and suppressing uterine contractions. Estrogen levels also rise significantly, stimulating uterine growth and development of the mammary glands. Other hormonal changes include increased prolactin (for milk production), relaxin (to soften ligaments and prepare for childbirth), and cortisol (to regulate metabolism and stress response). These hormonal shifts orchestrate the complex physiological adaptations necessary to support fetal development and prepare the body for childbirth. Postpartum, there’s a dramatic decrease in these hormones, initiating the return to the non-pregnant state.
Q 15. Describe the physiological changes in the mother during pregnancy.
Pregnancy triggers profound physiological changes in the mother’s body to support fetal development. These changes affect nearly every organ system.
- Cardiovascular System: Blood volume increases significantly, increasing cardiac output to meet the demands of the growing fetus and placenta. This can lead to physiological anemia (dilution of red blood cells). Heart rate also increases.
- Respiratory System: Breathing rate and tidal volume increase to provide adequate oxygen for both the mother and fetus. The diaphragm is elevated due to the expanding uterus, impacting lung capacity.
- Renal System: Glomerular filtration rate increases to handle the increased blood volume and metabolic waste products. The kidneys work harder to excrete the extra fluid.
- Endocrine System: Dramatic hormonal changes occur, with significant increases in estrogen, progesterone, and human chorionic gonadotropin (hCG). These hormones regulate the development of the placenta, breasts, and uterus, and maintain pregnancy.
- Gastrointestinal System: Hormonal changes can cause nausea, vomiting, heartburn, and constipation. The growing uterus can also put pressure on the stomach and intestines.
- Musculoskeletal System: The mother’s body adapts to the weight of the growing fetus, often leading to changes in posture and back pain. Ligaments and joints relax in preparation for delivery.
- Integumentary System: Changes in skin pigmentation (chloasma, linea nigra) are common. Stretch marks may develop due to skin stretching.
Think of it like this: the mother’s body undergoes a complete remodeling process, a finely tuned orchestra of physiological adjustments orchestrated by hormones and the needs of the developing baby.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the common complications of pregnancy?
Pregnancy complications can range from mild to life-threatening. Some common complications include:
- Gestational Diabetes: A condition where the mother develops high blood sugar levels during pregnancy.
- Preeclampsia: A dangerous condition characterized by high blood pressure and protein in the urine, potentially leading to eclampsia (seizures).
- Preterm Labor: Labor that begins before 37 weeks of gestation.
- Postpartum Hemorrhage: Excessive bleeding after delivery.
- Placental Abruption: Premature separation of the placenta from the uterine wall.
- Placenta Previa: Placenta implants low in the uterus, partially or completely covering the cervix.
- Ectopic Pregnancy: Pregnancy outside of the uterus (usually in the fallopian tube).
- Gestational Hypertension: High blood pressure developing during pregnancy.
These complications highlight the importance of regular prenatal care, where these conditions can be identified and managed effectively.
Q 17. Explain the process of parturition.
Parturition, or childbirth, is a complex process involving the coordinated action of several factors. It’s triggered by a cascade of hormonal and neurological events that lead to uterine contractions and cervical dilation.
- Initiation of Labor: While the exact trigger is still not fully understood, factors include fetal maturation, placental aging, and hormonal changes (rise in oxytocin, prostaglandins, and a decrease in progesterone).
- Uterine Contractions: Powerful contractions of the uterine muscles push the baby down the birth canal.
- Cervical Dilation: The cervix, the opening of the uterus, gradually dilates to allow passage of the baby.
- Fetal Descent: The baby moves down through the birth canal.
- Delivery of the Placenta: After the baby is born, the placenta detaches from the uterine wall and is expelled.
Think of labor as a carefully orchestrated dance between the mother’s body and the fetus, ultimately culminating in the safe delivery of the baby.
Q 18. Describe the role of oxytocin in labor.
Oxytocin, often called the ‘love hormone,’ plays a crucial role in labor. It’s a powerful uterine stimulant, causing contractions to become stronger, more frequent, and more coordinated. This positive feedback loop is essential for effective labor progression.
Furthermore, oxytocin promotes the bonding process between mother and baby after birth, contributing to lactation and maternal behavior. Synthetic oxytocin (Pitocin) is often used medically to augment or induce labor, though it must be used cautiously to avoid complications.
Q 19. What are the stages of labor?
Labor is typically divided into three stages:
- First Stage: This is the longest stage, characterized by cervical dilation and effacement (thinning). It’s further divided into latent (early) and active phases, with increasing intensity of contractions.
- Second Stage: This stage begins when the cervix is fully dilated (10 cm) and ends with the delivery of the baby. This stage involves strong pushing efforts by the mother to expel the baby.
- Third Stage: This is the final stage, involving the delivery of the placenta.
Each stage has its own set of physiological changes and challenges, necessitating careful monitoring and support from healthcare providers.
Q 20. Explain the physiological changes in the postpartum period.
The postpartum period, the time after childbirth, is marked by significant physiological changes as the mother’s body returns to its pre-pregnancy state. This process, called involution, involves:
- Uterine Involution: The uterus shrinks back to its normal size, a process that takes several weeks. Afterpains, cramping sensations, are common during this period.
- Hormonal Changes: Hormone levels drop dramatically, particularly estrogen and progesterone. This can cause mood swings, fatigue, and postpartum depression in some women.
- Lochia: Postpartum bleeding, which gradually diminishes over several weeks.
- Cardiovascular System: Blood volume returns to pre-pregnancy levels.
- Weight Loss: Loss of excess fluids and weight gained during pregnancy.
The speed and extent of these changes vary between women, and appropriate postpartum care is essential to address any complications.
Q 21. Describe the process of lactation.
Lactation, or milk production, is a complex process regulated by hormones, primarily prolactin and oxytocin. Prolactin stimulates milk production in the mammary glands, while oxytocin triggers milk ejection (let-down) reflex.
- Initiation of Lactation: High levels of estrogen and progesterone during pregnancy inhibit milk production. After delivery, the drop in these hormones triggers prolactin release, initiating milk production.
- Milk Production: Prolactin acts on the mammary glands to synthesize milk components.
- Milk Ejection: The let-down reflex, triggered by suckling or the baby’s cry, releases oxytocin, causing the milk to flow.
- Milk Composition: Breast milk composition changes over time to meet the baby’s nutritional needs, from colostrum (first milk) to mature milk.
Successful lactation requires a proper diet and emotional support for the mother. Breastfeeding offers significant health benefits to both the mother and the baby.
Q 22. What are the hormonal factors involved in lactation?
Lactation, the process of milk production, is a complex interplay of hormones orchestrated primarily by prolactin and oxytocin.
Prolactin (PRL): This hormone, produced by the anterior pituitary gland, is the primary driver of milk synthesis. Elevated levels during pregnancy prepare the breasts for lactation, and after childbirth, continued PRL release sustains milk production. Think of prolactin as the ‘milk-making’ hormone. Levels are suppressed during pregnancy by estrogen and progesterone, and a drop in those hormones after delivery triggers the surge in prolactin.
Oxytocin: Secreted by the posterior pituitary gland, oxytocin is the ‘milk-ejection’ hormone. In response to suckling or other stimuli, it triggers the contraction of myoepithelial cells surrounding the alveoli in the mammary glands, causing milk to be released. It’s the hormone responsible for the ‘let-down’ reflex, allowing the baby to feed.
Other Hormones: Estrogen, progesterone, cortisol, insulin, and growth hormone also play supporting roles in lactation, influencing the development of the mammary glands, regulating milk composition, and affecting overall metabolic processes. For example, insulin helps regulate glucose uptake into the mammary glands for milk synthesis. These hormones work in a complex feedback loop, adjusting milk production based on infant demand.
Understanding these hormonal interactions is crucial for managing lactation challenges, such as insufficient milk production or difficulties with milk ejection. For instance, medications that affect prolactin levels can impact lactation. This knowledge is essential in providing tailored advice and support to breastfeeding mothers.
Q 23. Explain the different types of contraception and their mechanisms of action.
Contraception methods prevent pregnancy through various mechanisms. They can be broadly classified into hormonal methods, barrier methods, and permanent methods.
Hormonal Methods: These methods manipulate the hormonal environment to prevent ovulation or implantation. Examples include:
- Combined Oral Contraceptives (COCs): Contain estrogen and progesterone, suppressing ovulation and thickening cervical mucus.
- Progesterone-only Pills (POPs): Primarily thicken cervical mucus and may alter endometrial lining, thus hindering sperm transport and implantation.
- Hormonal Implants: Slowly release progesterone, suppressing ovulation.
- Hormonal Injections: Deliver progesterone over several months, similarly suppressing ovulation.
- Hormonal Patches: Deliver hormones through the skin, mimicking the action of COCs.
- Vaginal Rings: Release hormones locally, preventing ovulation.
Barrier Methods: These methods physically prevent sperm from reaching the egg. Examples include:
- Condoms (male and female): Create a physical barrier, preventing sperm from entering the vagina or uterus.
- Diaphragm and Cervical Cap: Barrier devices placed in the vagina to cover the cervix.
- Sponge: Contains spermicide and creates a barrier.
Permanent Methods: These methods permanently prevent pregnancy. Examples include:
- Tubal Ligation (female sterilization): Severing or blocking the fallopian tubes.
- Vasectomy (male sterilization): Severing or blocking the vas deferens.
Other Methods:
- Intrauterine Devices (IUDs): Can be hormonal or copper-releasing. Hormonal IUDs thicken the uterine lining, while copper IUDs create a hostile environment for sperm and eggs.
- Fertility Awareness Methods (FAMs): Rely on tracking menstrual cycles to identify fertile and infertile periods.
Choosing the right method depends on individual factors, health status, and preferences. It’s crucial to consult a healthcare professional to discuss options and potential risks and benefits.
Q 24. Describe the effects of specific hormones on reproductive organs.
Several hormones exert profound effects on reproductive organs. Let’s consider a few key players:
Estrogen: Primarily produced by the ovaries, estrogen stimulates the growth and development of the female reproductive tract. It promotes the thickening of the uterine lining (endometrium) during the menstrual cycle, preparing it for potential implantation. It also plays a critical role in breast development and the regulation of menstrual cycles. Estrogen deficiency can lead to symptoms like irregular periods, vaginal dryness, and reduced libido.
Progesterone: Also secreted by the ovaries, progesterone maintains the uterine lining and prepares it for a fertilized egg. It suppresses uterine contractions, helping to maintain pregnancy. Progesterone deficiency can lead to miscarriage or irregular periods.
Testosterone: The primary male sex hormone, produced mainly by the testes, is vital for the development and function of the male reproductive system. It stimulates sperm production (spermatogenesis), promotes the development of secondary sexual characteristics (muscle mass, hair growth), and influences libido.
Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH): These hormones, secreted by the anterior pituitary gland, regulate ovarian function in females and testicular function in males. In females, FSH stimulates follicle development in the ovaries, while LH triggers ovulation. In males, FSH stimulates sperm production, and LH stimulates testosterone production.
Gonadotropin-releasing hormone (GnRH): This hormone, produced by the hypothalamus, regulates the release of FSH and LH from the pituitary gland.
Hormonal imbalances can cause various reproductive disorders, emphasizing the importance of maintaining hormonal equilibrium for optimal reproductive health. For instance, polycystic ovary syndrome (PCOS) is linked to imbalances in LH and FSH.
Q 25. Discuss the genetic basis of reproductive disorders.
Genetic factors play a significant role in various reproductive disorders. These disorders can be inherited or arise from spontaneous mutations.
Inherited Disorders: Conditions like cystic fibrosis, Turner syndrome, Klinefelter syndrome, and fragile X syndrome can impact fertility. Cystic fibrosis, for example, affects the reproductive tract, leading to infertility. Chromosomal abnormalities like Turner syndrome (XO) and Klinefelter syndrome (XXY) affect gonadal development and function.
Genetic Mutations: Mutations in genes involved in hormone production, signaling, or gamete development can cause reproductive disorders. For example, mutations in genes encoding FSH or LH receptors can lead to impaired reproductive function. Many genes are involved in the complex processes of meiosis and gamete formation so defects in those genes can lead to infertility.
Genetic Testing: Genetic testing is increasingly used to identify genetic risk factors for reproductive disorders. This information helps in genetic counseling and reproductive decision-making. Preimplantation genetic diagnosis (PGD) can help identify embryos free of genetic defects before implantation in IVF.
Understanding the genetic basis of reproductive disorders is crucial for developing better diagnostic tools, treatment strategies, and genetic counseling for couples facing reproductive challenges.
Q 26. Explain the impact of environmental factors on reproductive health.
Environmental factors significantly impact reproductive health. Exposure to certain substances and conditions can negatively affect fertility and pregnancy outcomes.
Endocrine-disrupting chemicals (EDCs): These chemicals, found in plastics, pesticides, and industrial products, can interfere with hormonal systems, potentially affecting reproductive function. Exposure to EDCs during critical developmental stages can have long-lasting consequences.
Environmental toxins: Exposure to heavy metals (lead, mercury), pesticides, and air pollution has been linked to reduced fertility and increased risk of birth defects. These toxins can damage DNA, disrupt hormonal balance, and compromise reproductive function.
Lifestyle factors: Smoking, excessive alcohol consumption, and drug use negatively impact reproductive health. Smoking, for example, can reduce sperm count and increase the risk of ectopic pregnancy. Alcohol abuse is a cause of fetal alcohol syndrome and other reproductive complications.
Stress: Chronic stress can disrupt hormonal balance, leading to menstrual irregularities, reduced fertility, and increased risk of miscarriage. Managing stress levels through lifestyle modifications and stress-reduction techniques is essential for maintaining reproductive health.
Nutrition: Deficiencies in essential nutrients can impair reproductive function. A balanced diet rich in vitamins, minerals, and antioxidants is crucial for optimal reproductive health.
Minimizing exposure to environmental toxins, adopting a healthy lifestyle, and managing stress are vital for preserving reproductive health.
Q 27. Discuss the role of nutrition in reproductive health.
Nutrition plays a pivotal role in reproductive health, affecting fertility, pregnancy outcomes, and postpartum recovery. A balanced diet provides essential nutrients for the proper functioning of the reproductive system.
Essential Nutrients: Folic acid (B9) is crucial for preventing neural tube defects in developing embryos. Iron is vital for preventing anemia, particularly during pregnancy. Iodine is necessary for thyroid hormone production, which impacts fertility and fetal development. Zinc plays a role in sperm production, and antioxidants protect against oxidative stress that can damage reproductive cells.
Weight Management: Both obesity and underweight can negatively impact fertility. Obesity is associated with hormonal imbalances, reduced fertility, and increased risk of pregnancy complications. Underweight can disrupt menstrual cycles and lead to ovulation problems.
Dietary Recommendations: A diet rich in fruits, vegetables, whole grains, lean protein, and healthy fats is recommended. Limiting processed foods, sugary drinks, and unhealthy fats is important. Adequate hydration is also essential. It is recommended to meet with a registered dietitian for personalized dietary advice. They will take into consideration your individual nutritional needs, whether you are trying to conceive or are currently pregnant or breastfeeding.
Proper nutrition is a cornerstone of reproductive well-being, ensuring optimal functioning of the reproductive system throughout all stages of life.
Q 28. Describe a recent advance in reproductive technology and its significance.
Recent advances in reproductive technology include improvements in preimplantation genetic testing (PGT). Initially used to detect chromosomal abnormalities, PGT is now evolving to screen for a wider range of genetic disorders, including single-gene mutations and other genetic variations that may lead to debilitating diseases or conditions.
Significance: Advanced PGT techniques offer improved accuracy and efficiency in identifying embryos with genetic abnormalities. This significantly enhances the chances of successful implantation of healthy embryos and reduces the risk of having a child with a genetic disorder. The development of comprehensive genetic screening methods allows for more informed decisions regarding embryo selection. This also decreases the need for invasive diagnostic procedures during pregnancy, safeguarding fetal health.
The ongoing development and refinement of PGT techniques are revolutionizing assisted reproductive technologies, offering couples facing the risk of inheritable diseases more options for starting a family while minimizing risks to the child and family.
Key Topics to Learn for Your Reproductive Physiology Interview
- Gametogenesis: Understand the processes of spermatogenesis and oogenesis, including hormonal regulation and potential points of failure. Consider practical applications in fertility treatments.
- Hormonal Control of Reproduction: Master the intricate interplay of hypothalamic-pituitary-gonadal (HPG) axis hormones (GnRH, FSH, LH, estrogen, progesterone, testosterone) and their feedback mechanisms. Think about how disruptions in this axis manifest clinically.
- Menstrual Cycle: Thoroughly grasp the phases of the menstrual cycle, including endometrial changes, hormonal fluctuations, and their clinical significance. Be prepared to discuss diagnostic approaches related to menstrual irregularities.
- Fertilization and Implantation: Review the processes of fertilization, early embryonic development, and implantation. Understand the molecular and cellular mechanisms involved. Consider clinical implications like IVF and ectopic pregnancies.
- Pregnancy and Parturition: Explore the physiological changes during pregnancy, focusing on placental function, fetal development, and the initiation of labor. Be ready to discuss complications of pregnancy and delivery.
- Lactation: Understand the hormonal regulation and physiological processes involved in lactation. Consider the nutritional aspects and potential challenges.
- Contraception: Familiarize yourself with various contraceptive methods, their mechanisms of action, and their effectiveness. Consider the hormonal and non-hormonal options.
- Infertility: Understand the common causes of both male and female infertility, including diagnostic approaches and treatment strategies. Consider the ethical implications of assisted reproductive technologies (ART).
- Reproductive Endocrinology and Infertility: For more advanced interviews, delve deeper into specific endocrinological disorders affecting reproduction, such as PCOS, endometriosis, and hypogonadism.
- Problem-Solving: Practice applying your knowledge to hypothetical scenarios. Consider how you would approach a case study or troubleshoot a clinical problem related to reproductive physiology.
Next Steps
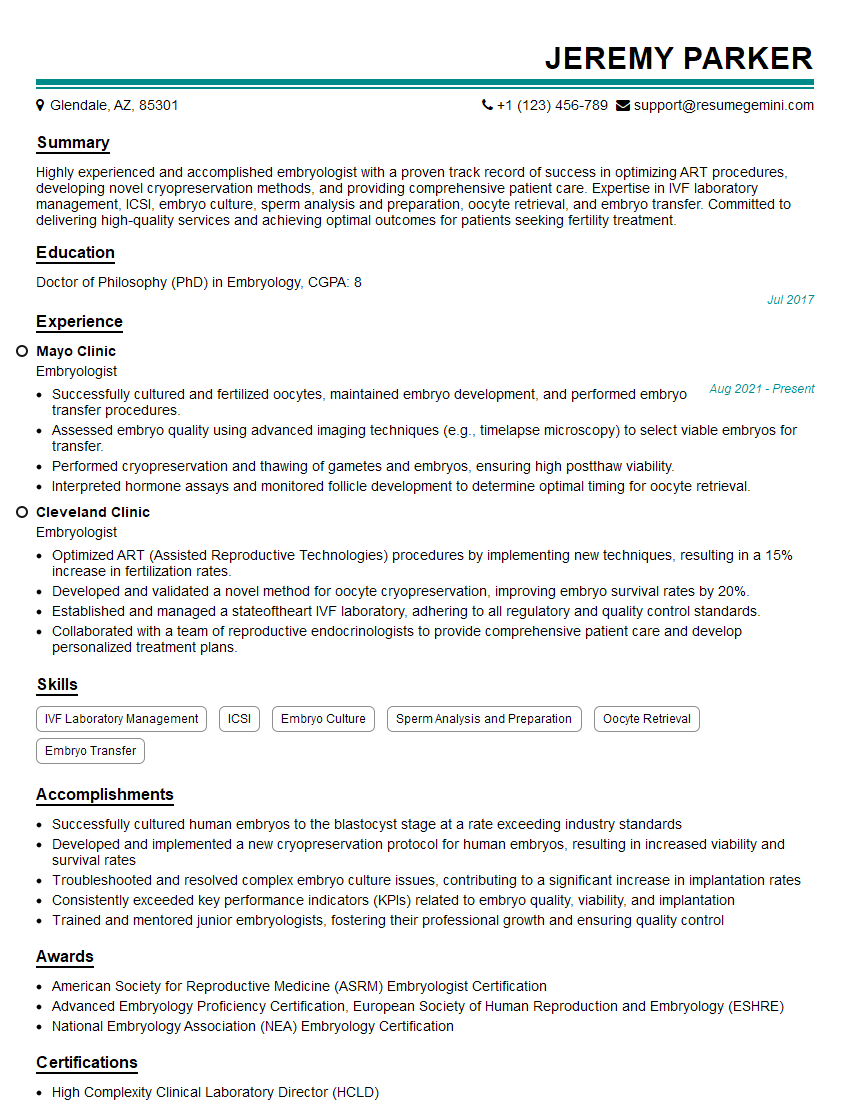
Mastering Reproductive Physiology is crucial for advancing your career in research, clinical practice, or related fields. A strong understanding of these complex processes is highly valued by employers. To maximize your job prospects, it’s essential to create an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource for building professional, impactful resumes tailored to your specific career goals. Examples of resumes tailored to Reproductive Physiology are available, providing you with a head start in crafting a compelling application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO