Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Emergency First Aid (for pets) interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Emergency First Aid (for pets) Interview
Q 1. Describe the steps you would take if you encountered a pet experiencing severe bleeding.
Severe bleeding in pets is a life-threatening emergency requiring immediate action. The priority is to control the bleeding, preventing shock. Think of it like plugging a leak in a water pipe – you need to stop the flow.
- Assess the Situation: Ensure your own safety first. Is the environment safe for you and the pet? What type of wound is causing the bleeding? Is it arterial (bright red, spurting), venous (dark red, steady flow), or capillary (oozing)?
- Control the Bleeding: Apply direct pressure to the wound using a clean cloth or bandage. Don’t remove any embedded objects; instead, bandage around them. Elevate the injured limb if possible, to help reduce blood flow.
- Seek Veterinary Care: Transport the pet to the nearest veterinary clinic or emergency animal hospital immediately. Keep the pressure on the wound during transport, but be aware of the possibility of needing to check circulation if the limb is very distal or if you need to remove the bandage to clean it.
- Monitor Vital Signs: While waiting for veterinary care, check your pet’s heart rate and breathing. Signs of shock (pale gums, weak pulse, rapid breathing) require prompt attention.
Example: Imagine your dog is bleeding profusely from a leg wound after a fight. Applying direct pressure with a clean towel while calling for immediate veterinary help is paramount.
Q 2. How would you treat a pet suffering from heatstroke?
Heatstroke in pets is a serious condition caused by overheating. It’s like leaving a chocolate bar in the sun – it melts and can be ruined. Quick action is critical.
- Move to a Cool Place: Immediately move your pet to a shaded, cool area, such as air conditioning or under a fan.
- Cool the Pet Down: Apply cool (not ice cold) water to their paws, ears, and body. Avoid submerging them in cold water. You can use wet towels or a damp cloth. A fan can aid cooling.
- Monitor Breathing and Heart Rate: Check your pet’s breathing and pulse regularly.
- Offer Cool Water: If your pet is conscious and able to drink, offer small amounts of cool water. Don’t force it.
- Seek Veterinary Care: Heatstroke is a medical emergency. Get your pet to a vet as quickly as possible.
Example: Leaving a dog in a parked car on a hot day, even for a short time, can lead to heatstroke. Recognizing the symptoms (panting, lethargy, collapse) and acting quickly are vital.
Q 3. What are the signs of shock in a pet, and what first aid measures would you implement?
Shock is a life-threatening condition where the body isn’t getting enough blood flow. Think of it as a plumbing system with low water pressure – organs aren’t getting what they need.
Signs of Shock:
- Pale or bluish gums
- Rapid, weak pulse
- Rapid, shallow breathing
- Weakness or collapse
- Lethargy or unconsciousness
- Cold extremities
First Aid Measures:
- Keep the Pet Warm: If the pet is cold, gently wrap them in a blanket to help maintain body temperature.
- Keep the Head Low: This can help improve blood flow to the brain.
- Administer Oxygen (if trained): If you’re trained and equipped, administering supplemental oxygen can be beneficial.
- Control Bleeding: If bleeding is present, address it immediately.
- Transport Immediately: Shock is a critical condition requiring urgent veterinary care.
Example: A dog hit by a car may go into shock due to internal bleeding and trauma. Immediate treatment to control bleeding, keep the animal warm, and transport it are crucial.
Q 4. Explain the procedure for administering CPR to a small dog.
CPR (Cardiopulmonary Resuscitation) in small dogs is similar to human CPR but requires adjustments for size. Think of it as delicately restarting a tiny engine.
- Check for Breathing and Pulse: Check for breathing and a heartbeat for no more than 10 seconds.
- Mouth-to-Snout Rescue Breaths: Cover the dog’s nose and mouth with your mouth and gently give two rescue breaths. Each breath should last about a second.
- Chest Compressions: Place the heel of one hand over the widest part of the dog’s chest (typically just behind the front legs) and the other hand on top. Press down firmly, compressing the chest about ⅓ to ½ inch, and repeat 30 times.
- Repeat Cycles: Continue two breaths and 30 compressions cycles until the dog begins to breathe on its own or professional help arrives.
- Seek Veterinary Care: CPR is a temporary measure; veterinary care is necessary for proper diagnosis and treatment.
Important Note: Improper CPR can cause further injury. Consider taking a pet CPR course for proper training.
Q 5. How would you handle a pet that has ingested poison?
Ingestion of poison is a serious emergency. Think of it like a computer virus – it can wreak havoc on the system. Immediate action is critical.
- Identify the Poison: If possible, identify the type and amount of poison ingested. This information is crucial for the vet.
- Contact a Vet or Poison Control: Immediately contact your veterinarian or the ASPCA Animal Poison Control Center (APCC). They can provide specific guidance based on the poison ingested.
- Follow Instructions: Carefully follow any instructions given by the veterinarian or APCC. This might involve inducing vomiting (only if instructed to do so), administering activated charcoal, or other interventions.
- Do Not Induce Vomiting Without Guidance: Never induce vomiting without specific instructions from a vet or APCC. Some poisons can cause more harm if vomited.
- Transport to the Vet: Transport your pet to the veterinary clinic or emergency animal hospital for monitoring and treatment.
Example: If your dog eats rat poison, immediate contact with the APCC and a vet is crucial. They will guide you on the appropriate next steps, which might include administering specific antidotes.
Q 6. What are the signs of a pet experiencing an allergic reaction, and how would you respond?
Allergic reactions in pets can range from mild to severe and life-threatening, like a sudden, intense food sensitivity.
Signs of Allergic Reaction:
- Hives or welts
- Swelling of the face, lips, or tongue
- Difficulty breathing
- Vomiting or diarrhea
- Itching or scratching
- Weakness or collapse
Response:
- Identify the Allergen: If possible, identify the allergen that triggered the reaction.
- Remove the Allergen: If the allergen is still present (e.g., a bee sting), remove it carefully.
- Administer Antihistamine (if trained): If you have a veterinarian-prescribed antihistamine for your pet and are trained to administer it, give the appropriate dose.
- Monitor Breathing: Closely monitor your pet’s breathing. Difficulty breathing is a critical sign requiring immediate veterinary attention.
- Seek Veterinary Care: Allergic reactions can rapidly worsen. Immediate veterinary attention is crucial.
Example: A dog stung by a bee may experience swelling, hives, and difficulty breathing. Immediate removal of the stinger, administration of an antihistamine (if trained and instructed by a veterinarian), and prompt veterinary care are necessary.
Q 7. How would you stabilize a pet with a suspected broken bone?
Suspected broken bones require careful handling to prevent further injury. Think of it like supporting a broken branch – you need to immobilize it to prevent further damage.
- Minimize Movement: Keep the pet calm and minimize movement of the injured limb.
- Immobilize the Limb (Splinting): If possible, create a splint using readily available materials (cardboard, sticks, towels) to support the injured limb. Pad the splint with soft material to prevent pressure sores. The goal is to immobilize the joint above and below the suspected fracture.
- Transport Carefully: Use a stretcher or sturdy board to transport the pet to the veterinary clinic, ensuring minimal movement of the injured area.
- Monitor Vital Signs: Observe your pet for signs of pain, swelling, or changes in vital signs.
- Seek Veterinary Care: Veterinary attention is necessary to diagnose the fracture and provide appropriate treatment (e.g., X-rays, setting the bone, casting).
Example: A cat with a suspected broken leg after falling from a height needs its leg immobilized with a splint before transportation to the vet. This will minimize pain and prevent further damage.
Q 8. Describe your experience with bandaging a pet’s wound.
Bandaging a pet’s wound requires careful technique to prevent infection and promote healing. First, you must assess the wound – its depth, length, and the presence of any foreign bodies. Never attempt to clean a severely deep or actively bleeding wound yourself; immediate veterinary attention is crucial. For minor wounds, gentle cleaning with mild soap and water is necessary, followed by thorough rinsing. The bandage itself should be clean and sterile. I prefer using non-stick gauze to prevent the bandage from adhering to the wound. The bandage should be snug but not constricting; you should be able to easily slip a finger underneath. Too tight a bandage can restrict blood flow, while a loose one will be ineffective. The bandage should cover the entire wound and extend slightly beyond its edges. It’s essential to secure the bandage with tape that won’t irritate the pet’s skin. Finally, monitor the wound and bandage regularly for signs of infection, such as swelling, redness, or discharge. If you notice any of these, seek veterinary care promptly.
For example, I once helped a dog with a small cut on its paw. After cleaning the wound, I applied a thin layer of antibiotic ointment, covered it with non-stick gauze, and secured it with vet wrap. I checked the bandage regularly and removed it after a few days once the wound had started to heal. Remember, always consult a vet for guidance on more severe wounds.
Q 9. How would you handle a pet suffering from a seizure?
Seizures in pets can be terrifying, but a calm and controlled response is crucial. First, ensure your pet’s safety by moving them away from any potential hazards. Time the seizure; this information is vital for the vet. Do not try to restrain your pet during a seizure; instead, gently cushion their head to prevent injury. After the seizure subsides, keep your pet warm and quiet, allowing them to recover slowly. Do not offer food or water until they are fully alert. Contact your veterinarian immediately following a seizure, providing details such as the duration and severity. They may want to run tests to identify the underlying cause, which could be anything from epilepsy to a brain tumor.
Remember, while you can provide basic care during the seizure, veterinary intervention is essential for diagnosis and treatment.
Q 10. What are the different types of pet carriers and their suitability in emergencies?
Pet carriers come in various forms, each with its own advantages and disadvantages in emergency situations. Hard-sided carriers offer the best protection in a car accident, preventing your pet from being thrown around. Soft-sided carriers are more portable but offer less protection. The choice depends on the situation and your pet’s size and temperament. A smaller, easily carried carrier is ideal for quick evacuations, while a larger, more robust one is best for longer transports. Always ensure the carrier is well-ventilated and allows your pet to stand comfortably. In an emergency, your goal is to secure your pet safely and transport them to the vet quickly and efficiently.
For example, a hard-sided carrier is preferred when transporting a cat during a hurricane. However, a smaller, soft-sided carrier might be better for a quick vet trip with a small dog in a normal setting.
Q 11. What steps would you take to assess a pet’s airway?
Assessing a pet’s airway involves looking for obstructions and evaluating breathing. First, check for any visible signs of obstruction, like vomit, blood, or a foreign object. Gently open the pet’s mouth and check the airway, removing any visible obstructions if possible (but only if it’s easily accessible and you can do it safely). Observe the chest for the rise and fall of the rib cage, indicating breathing. Feel for the presence of a heartbeat. If breathing is absent or labored, you may need to administer CPR. Remember, pet CPR techniques differ from human CPR, so specialized training is highly recommended.
For example, a dog choking on a ball would require carefully removing the ball from its mouth. However, a dog that’s unconscious and not breathing needs immediate CPR and veterinary assistance.
Q 12. Explain the importance of maintaining a calm demeanor while providing first aid to a pet.
Maintaining a calm demeanor while providing first aid is crucial because pets are very sensitive to their owner’s emotional state. A stressed or anxious owner will likely increase the pet’s anxiety, making it more difficult to provide effective care. A calm and reassuring presence helps keep the pet calm and cooperative. This is especially important when dealing with injured or frightened animals. Think of it like this: a calm approach helps to reduce the pet’s fear response, making the assessment and treatment process safer and more effective for both you and your pet.
I have found that speaking softly and using a gentle touch is always more effective when dealing with an injured pet.
Q 13. How would you deal with an aggressive pet requiring first aid?
Dealing with an aggressive pet requiring first aid necessitates caution and safety. Never approach an aggressive animal without proper protection. If possible, use a muzzle to prevent bites. If a muzzle isn’t available and you can do so safely, use a towel to control the animal’s head. Enlist the help of another person, if possible. Try to assess the injuries while keeping a safe distance. Remember to prioritize your safety; it’s impossible to help a pet if you are injured yourself. Veterinary assistance may be necessary both for managing the aggression and treating the pet’s injuries. In some cases, sedation by a veterinarian might be required before safe treatment is possible. Professional help should always be sought in such scenarios.
For instance, I’ve seen cases where a vet needed to sedate a very aggressive cat before treatment of a wound could safely begin.
Q 14. Discuss the limitations of pet first aid and when veterinary intervention is crucial.
Pet first aid is designed to stabilize a pet until professional veterinary care can be obtained. It’s not a replacement for veterinary treatment. Pet first aid’s limitations include the inability to perform complex diagnostic tests or administer certain medications. While you can clean minor wounds, control bleeding, and provide basic support, severe injuries like broken bones, internal bleeding, or major trauma require immediate veterinary attention. Any condition that doesn’t improve quickly or shows signs of worsening necessitates a vet visit. Delayed treatment for serious injuries can have dire consequences. The rule of thumb is: when in doubt, seek veterinary assistance.
For example, while you can bandage a small cut, a deep puncture wound that requires stitching needs a vet. Similarly, while you might initially stabilize a pet after a car accident, it still needs immediate vet care for potential internal injuries.
Q 15. What are the common signs of dehydration in pets, and how would you address them?
Dehydration in pets is a serious condition, often indicated by sunken eyes, dry gums, and lethargy. Assessing skin turgor (the speed at which skin returns to its normal position after being pinched) is crucial; slow return indicates dehydration. Other signs include decreased urination, loss of appetite, and increased heart rate. Addressing dehydration involves gentle rehydration, ideally under veterinary supervision. For mild dehydration, offering small amounts of water or electrolyte solutions (specifically formulated for pets) frequently is beneficial. However, never force fluids. Severe dehydration requires immediate veterinary attention as intravenous fluids may be necessary to prevent organ damage. Think of it like this: just as we need to rehydrate after a strenuous workout, pets need help recovering fluid loss from illness or heatstroke.
- Mild Dehydration: Offer small amounts of water frequently.
- Moderate to Severe Dehydration: Immediate veterinary care is required.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How would you handle a pet with a suspected eye injury?
Suspected eye injuries in pets require immediate and cautious handling. Never attempt to remove embedded objects yourself. Instead, gently cover the affected eye with a clean, damp cloth or sterile eye pad to protect it. Avoid applying any pressure. Transport the pet to a veterinary clinic immediately. While en route, keep the pet calm and minimize head movement to prevent further damage. Imagine you’ve gotten something in your eye – you’d want someone to protect it and get you to the doctor quickly, right? The same principle applies to our furry friends.
- DO: Cover the eye gently and transport to a vet.
- DON’T: Try to remove foreign objects or apply pressure.
Q 17. What is your experience using a pet oxygen mask?
I have extensive experience using pet oxygen masks, both in a veterinary setting and during emergency response situations. Proper mask fit is critical. It needs to create a seal around the pet’s nose and mouth to deliver oxygen effectively. Different sizes of masks are available to fit various breeds and sizes. The flow rate of oxygen is adjusted based on the pet’s size and respiratory distress level. Monitoring the pet’s respiratory rate and effort during oxygen administration is essential, and I always ensure proper training and supervision before using an oxygen mask on a pet.
I’ve used oxygen masks to assist pets suffering from respiratory distress, smoke inhalation, and cardiac arrest. It’s vital to remain calm and efficient during administration. In a life-threatening situation, every second counts, and using an oxygen mask can be the difference between life and death.
Q 18. Explain your understanding of different wound types and appropriate dressing techniques.
Wound types vary significantly. We have lacerations (cuts), abrasions (scrapes), punctures (deep wounds from pointed objects), avulsions (tissue torn away), and burns. Dressing techniques are also different for each type. For lacerations, cleaning with saline solution and applying a sterile dressing is usually sufficient. Puncture wounds may require veterinary attention to assess for infection and potential internal damage. Avulsions need to be covered with a sterile dressing, and the lost tissue should be wrapped in a damp sterile gauze and transported with the patient. Burns require immediate cooling with cool (not cold) water and a sterile dressing. Always try to keep the wound clean, prevent further infection, and stabilize the injured area. Imagine building a protective barrier for a wound; the dressing is that barrier, preventing infection and promoting healing.
- Lacerations: Clean, sterile dressing.
- Puncture Wounds: Veterinary attention.
- Avulsions: Sterile dressing, transport lost tissue.
- Burns: Cool water, sterile dressing.
Q 19. How would you assist a pet struggling to breathe?
Assisting a pet struggling to breathe is a high-priority situation. Initial assessment involves checking for airway obstruction (foreign bodies, swelling). If an obstruction is present, attempt gentle removal (only if visible and easily accessible). If the pet is not breathing, CPR may be necessary. This includes chest compressions and rescue breaths (mouth-to-nose or using a pet resuscitation mask). Positioning the pet to improve breathing (e.g., elevating the head in certain cases) can be beneficial. Transport to a veterinary clinic is crucial – the pet requires immediate veterinary care, including oxygen therapy, and potentially advanced life support.
Remember, prompt action is vital. Every second counts. It’s essential to stay calm and work efficiently while seeking professional help.
Q 20. What safety measures do you take when providing first aid to a potentially infectious animal?
Safety is paramount when dealing with potentially infectious animals. Always wear appropriate personal protective equipment (PPE), including gloves, eye protection, and potentially a mask, gown, or even a face shield, depending on the suspected infection. Avoid direct contact with body fluids. After providing first aid, thoroughly wash your hands and any exposed skin with soap and water. Proper disposal of contaminated materials is essential. In cases involving bites, seek medical attention promptly to assess for infection. These precautions not only protect me but also prevent the spread of potential zoonotic diseases (diseases that can be transmitted from animals to humans).
Q 21. How familiar are you with different types of pet medications used in emergency situations?
I’m familiar with a range of pet medications used in emergency situations. This includes medications for pain relief (e.g., analgesics), control of seizures (e.g., diazepam), treatment of shock (e.g., fluids), and management of respiratory distress. Knowledge of dosage and administration routes is crucial. However, I always emphasize that administering any medication to a pet without explicit veterinary instructions is risky and may lead to unintended consequences. It’s always best to contact a veterinarian or animal emergency service for guidance.
My knowledge is complemented by a deep understanding of the potential side effects and contraindications associated with each medication. This is essential for ensuring the safe and effective treatment of pets during emergencies.
Q 22. Describe a time you had to improvise first aid equipment for a pet.
Improvisation is key in emergency pet first aid, especially when you’re away from a well-stocked kit. One instance involved a dog with a severe leg laceration bleeding profusely. I didn’t have a proper pressure bandage, so I used a clean, thick kitchen towel, rolled it tightly, and applied firm pressure directly to the wound. I then secured it using strips of an old bedsheet torn into strips, creating a makeshift bandage. This controlled the bleeding until we reached the veterinary clinic. The key is to use clean, absorbent materials that can create pressure and secure the wound.
Another example involves using a plastic bottle filled with warm water wrapped in a towel as a makeshift hot water bottle to gently warm a hypothermic kitten. Thinking creatively about what you have available is vital. The principle is to address the immediate need with available resources, ensuring the material is clean and safe to avoid further injury or infection.
Q 23. Explain your knowledge of the proper disposal of medical waste after providing pet first aid.
Safe disposal of medical waste after pet first aid is crucial to prevent the spread of zoonotic diseases – illnesses transmittable from animals to humans. Items like soiled bandages, gauze pads saturated with blood or other bodily fluids, and any material that came into direct contact with the pet’s wound should be treated as biohazardous waste.
Ideally, these materials should be placed in a leak-proof, sealed plastic bag. Double-bagging is even better. The bag should be clearly labeled as ‘biohazardous waste’ and disposed of according to your local regulations. Many areas require specific waste disposal services for biohazardous materials. Never put this type of waste in regular household garbage. In some cases, incineration is the most appropriate method of disposal.
Q 24. How would you handle a situation where multiple pets require simultaneous first aid?
Simultaneous first aid for multiple pets requires a systematic approach prioritizing the most critical cases first. Think of it like triage in human emergency medicine. A quick assessment of each pet’s condition—ABCs (Airway, Breathing, Circulation)— is essential. You’d identify the pet with the most life-threatening condition (e.g., severe bleeding, respiratory distress) and focus on that one first. Then, you would move to the next most critical animal. If possible, enlist help to assist in providing concurrent care.
Imagine a scenario where one cat is choking and another has a broken leg. The choking cat needs immediate attention to clear its airway. While someone attends to the choking cat, another person can prepare to immobilize the broken leg of the second cat. This approach helps make the best use of available time and resources.
Q 25. What are the common causes of pet trauma, and what are the initial steps in managing each?
Common causes of pet trauma include road traffic accidents (RTAs), falls, animal attacks, and poisoning. The initial steps for management vary depending on the specific injury but always involve assessing the scene for safety before approaching the animal.
- RTAs: Check for breathing, bleeding, and fractures. Control bleeding, immobilize suspected fractures, and maintain airway patency.
- Falls: Assess for spinal injuries, head trauma, and fractures. Maintain airway and immobilize the spine and any affected limbs.
- Animal Attacks: Control bleeding, clean and dress wounds, assess for shock, and seek veterinary attention promptly. Pay attention for signs of infection.
- Poisoning: Identify the poison if possible. Induce vomiting or administer activated charcoal as directed by a veterinary professional. Monitor breathing and heart rate closely. Contact emergency veterinary services immediately.
Remember to always prioritize your own safety before approaching a potentially aggressive or injured animal.
Q 26. Describe your knowledge of pet anatomy and physiology.
Understanding pet anatomy and physiology is fundamental to effective first aid. This knowledge allows for accurate assessment of injuries and appropriate interventions. For example, knowing the location of major blood vessels helps in controlling bleeding, while understanding respiratory mechanics guides airway management. Familiarity with the skeletal structure helps in recognizing and stabilizing fractures.
Specific knowledge varies by species and breed but includes understanding heart and lung placement, the locations of major organs, and the basic physiological responses to injury, such as shock. A good understanding of canine and feline anatomy is vital. For instance, I need to know where to palpate for a pulse on different breeds, which varies depending on the size and fur.
Q 27. How would you assess the level of consciousness of an unresponsive pet?
Assessing the level of consciousness in an unresponsive pet involves a systematic approach. First, assess responsiveness to stimuli. Gently call the pet’s name and observe for any reaction. If there is no response, try a light touch or a gentle pinch to a paw. Look for any signs of pain response.
Next, check the pet’s breathing and pulse rate. Is the breathing regular and adequate? Is there a palpable pulse? Absence of breathing or a weak pulse indicates a critical situation. Assess pupil response to light. Dilated pupils can indicate shock, trauma, or head injury.
A pet that doesn’t respond to stimuli, exhibits abnormal breathing, or lacks a palpable pulse is in a critical state and requires immediate veterinary attention.
Q 28. What resources would you use to find up-to-date information about pet first aid techniques?
Keeping up-to-date with pet first aid techniques is essential. I utilize several resources including veterinary professional organizations such as the American Veterinary Medical Association (AVMA), the American Animal Hospital Association (AAHA), and veterinary journals. Reputable veterinary colleges and universities often provide online resources and continuing education materials. It is crucial to be discerning about the information you use. Look for sources that cite research and are written by qualified veterinary professionals.
Additionally, certified pet first aid and CPR courses are invaluable. These courses provide hands-on training and updated information delivered by experts, building confidence and competence. Regular participation in continuing education enhances knowledge and skills ensuring I can provide the best possible care.
Key Topics to Learn for Emergency First Aid (for Pets) Interview
- Assessment of the Situation: Understanding the immediate environment and the pet’s condition before acting. This includes recognizing signs of shock, assessing for injuries, and ensuring your own safety.
- Cardiopulmonary Resuscitation (CPR): Knowing the techniques for performing CPR on different sizes and breeds of animals, including chest compressions and rescue breaths. Practical application involves practicing on a mannequin or through simulation exercises.
- Bleeding Control: Mastering techniques for controlling various types of bleeding, including applying direct pressure, elevation, and tourniquets (where appropriate). Understanding when to seek immediate veterinary attention is crucial.
- Wound Care: Learning how to clean and dress wounds to prevent infection. This includes understanding different types of wounds and the appropriate cleaning solutions and bandages.
- Shock Management: Recognizing the signs of shock and implementing appropriate first aid measures, such as keeping the pet warm and minimizing stress. Understanding the underlying causes of shock is also important.
- Fracture Management: Understanding how to immobilize suspected fractures using readily available materials while waiting for veterinary care. This involves proper splinting techniques.
- Poisoning and Toxin Exposure: Recognizing common household toxins dangerous to pets and knowing the initial steps to take before seeking veterinary help. This includes understanding when to induce vomiting and when not to.
- Seizure Management: Knowing how to safely manage a pet experiencing a seizure, protecting the animal from injury, and timing the event for veterinary reporting.
- Heat Stroke and Hypothermia: Understanding the signs, prevention, and treatment of both heat stroke and hypothermia in pets. This includes knowing when and how to cool down or warm up an animal appropriately.
- Transportation to Veterinary Care: Knowing safe and efficient methods for transporting an injured or ill pet to a veterinary clinic, including the use of appropriate carriers and restraints.
Next Steps
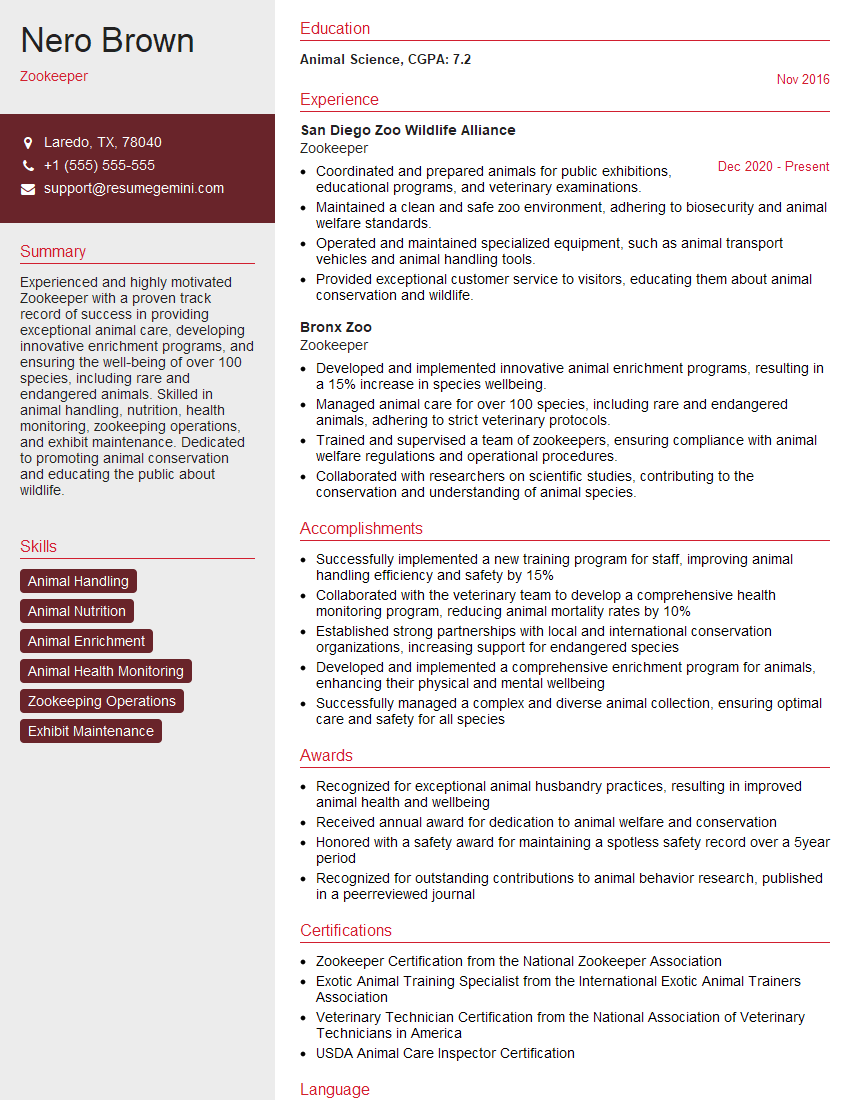
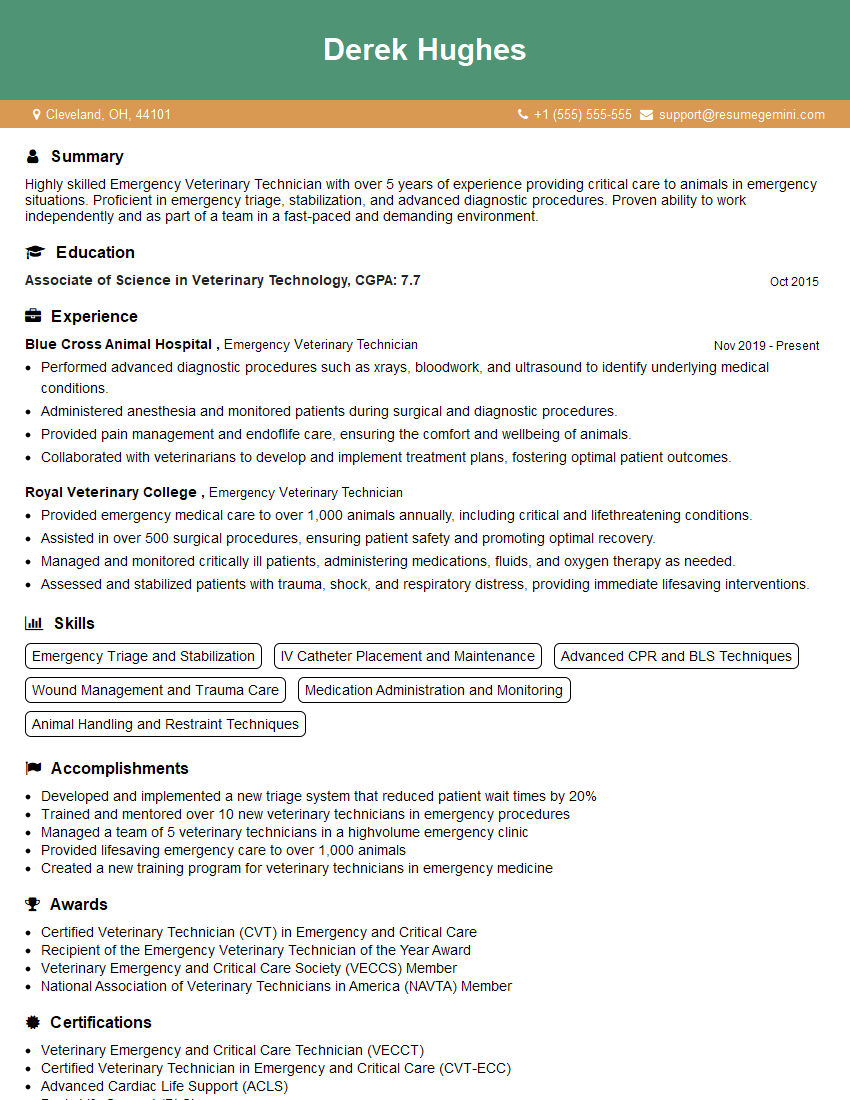
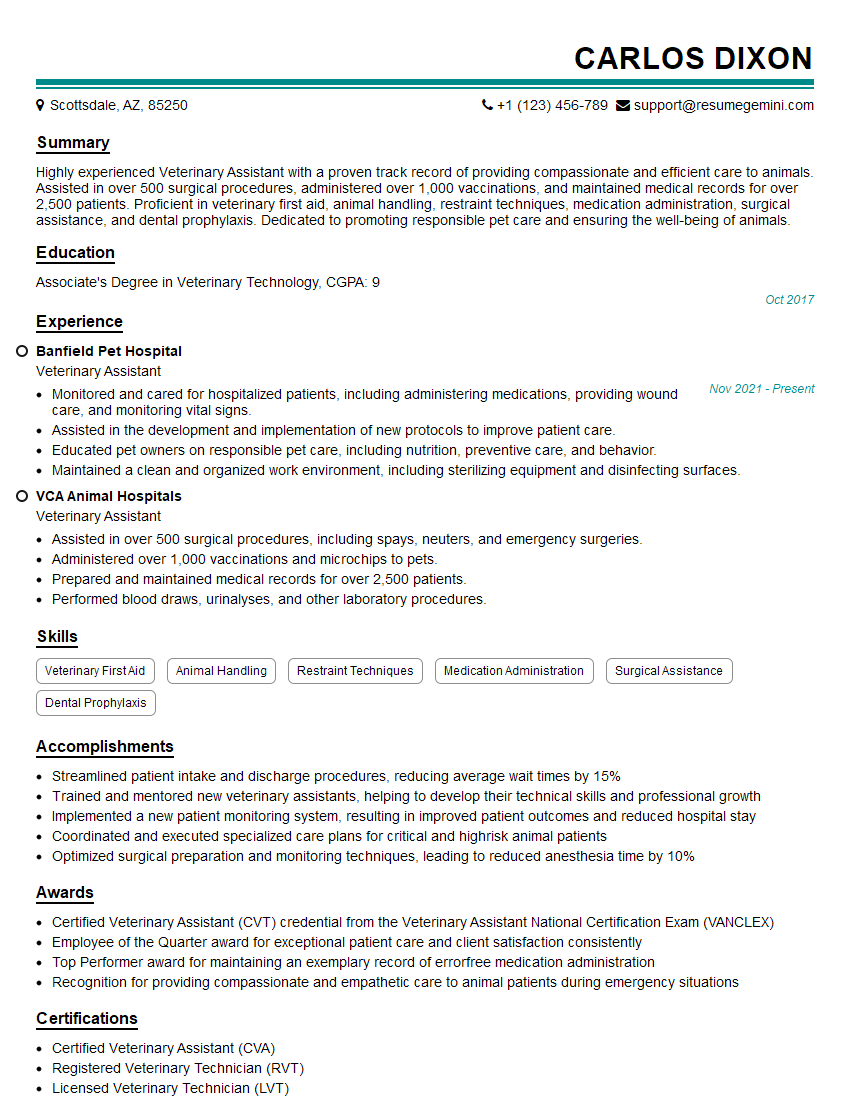
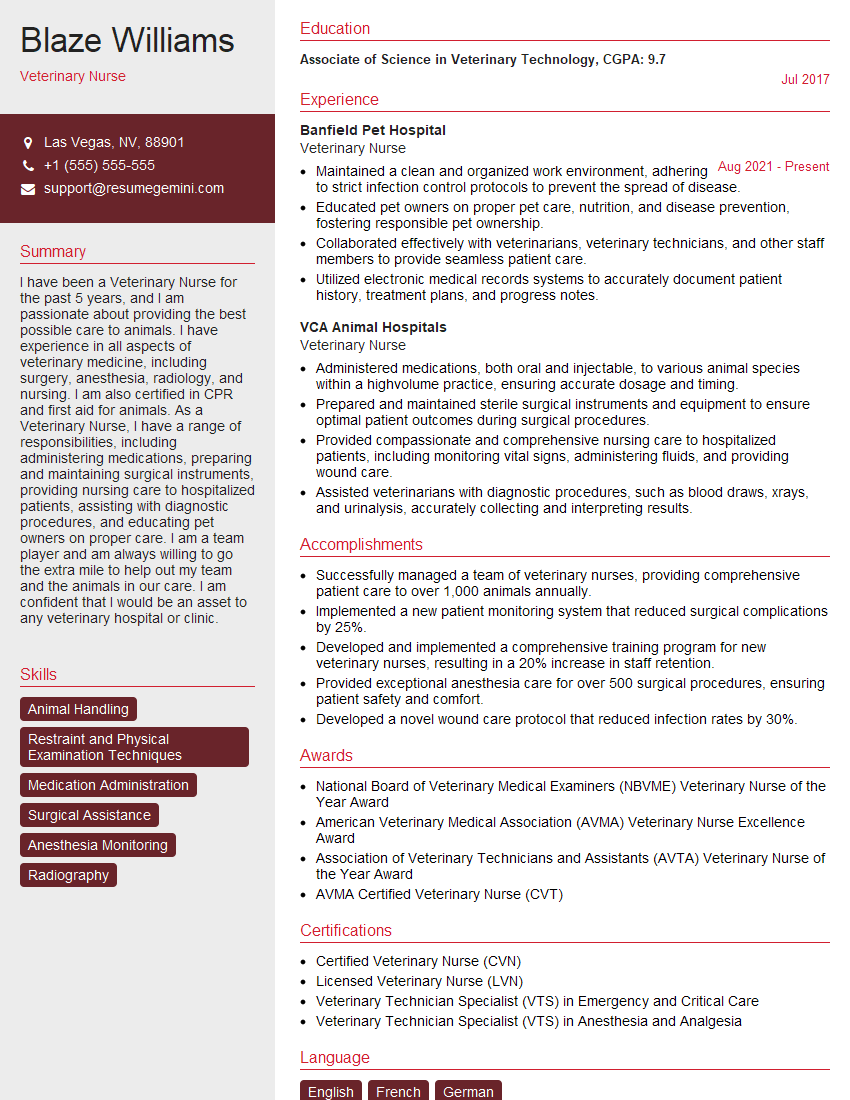
Mastering Emergency First Aid for pets significantly enhances your value as a candidate and opens doors to a fulfilling career in animal care. To stand out, you need a resume that showcases your skills effectively. Creating an ATS-friendly resume is crucial for getting your application noticed. ResumeGemini is a trusted resource to help you build a professional and impactful resume that will highlight your expertise in Emergency First Aid for pets. Examples of resumes tailored to this specific field are available through ResumeGemini, ensuring your application makes a strong first impression. Take the next step in your career journey today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO