Interviews are more than just a Q&A session—they’re a chance to prove your worth. This blog dives into essential Use of Specialized Diagnostic Equipment interview questions and expert tips to help you align your answers with what hiring managers are looking for. Start preparing to shine!
Questions Asked in Use of Specialized Diagnostic Equipment Interview
Q 1. Describe your experience with different types of diagnostic imaging equipment.
My experience encompasses a wide range of diagnostic imaging equipment, including X-ray systems (conventional and digital), computed tomography (CT) scanners, magnetic resonance imaging (MRI) systems, ultrasound machines, and fluoroscopy units. I’m proficient in operating and maintaining these systems, ensuring optimal image quality and patient safety. For instance, I’ve extensively used both conventional film-based X-ray machines and the latest digital radiography (DR) systems, understanding the advantages of each—DR’s superior image quality and digital manipulation capabilities compared to the older film systems. My experience also includes working with various ultrasound transducers, selecting the appropriate one depending on the anatomical region and the specific diagnostic task. I’m comfortable with different modalities and understand their respective strengths and weaknesses in various clinical settings.
- X-ray: Experienced with various types including mobile, fixed, and specialized units for dental or mammography.
- CT: Proficient in multislice CT and various reconstruction techniques.
- MRI: Experienced with various MRI sequences and coil technologies.
- Ultrasound: Experienced with various transducer types and applications, including Doppler and elastography.
- Fluoroscopy: Experienced in performing and monitoring fluoroscopic procedures.
Q 2. Explain the principles of operation for an MRI machine.
MRI, or Magnetic Resonance Imaging, leverages powerful magnets and radio waves to create detailed images of the body’s internal structures. It doesn’t use ionizing radiation, unlike X-rays or CT scans, making it a relatively safer option. The process begins by placing the patient within a strong magnetic field produced by large superconducting magnets. This field aligns the hydrogen atoms’ protons within the body. Then, radiofrequency pulses are emitted, temporarily disrupting this alignment. As the protons realign, they release energy, which is detected by the MRI machine’s receiver coils. This energy is then processed by sophisticated computer algorithms to create detailed cross-sectional images. Different tissue types have varying relaxation times (T1 and T2), allowing us to distinguish between them. For example, T1-weighted images are excellent for visualizing fat, appearing bright, while T2-weighted images are better for showing water, which also appears bright.
Think of it like this: the magnet aligns the protons like tiny compasses. The radio waves are like a temporary gust of wind that disrupts their alignment. As they settle back, they send out signals that reveal their environment – giving us highly detailed images.
Q 3. How do you ensure the safety of patients during diagnostic procedures?
Patient safety is paramount. My approach involves meticulous adherence to safety protocols, which vary based on the equipment used. For MRI, this includes screening for metallic implants (pacemakers, aneurysm clips) and claustrophobia. We carefully explain the procedure, addressing any concerns. For X-ray, we minimize radiation exposure using ALARA principles (As Low As Reasonably Achievable) by employing appropriate shielding and reducing exposure time. Patient monitoring throughout procedures is crucial, particularly during longer examinations like MRI or CT scans. We constantly monitor vital signs and look out for any adverse reactions. In the case of contrast agents used in CT or MRI, we carefully assess for allergies and monitor for potential allergic responses post-injection. Each procedure involves a thorough review of the patient’s medical history, and documentation of all safety precautions taken.
For example, before an MRI scan, I always verify the patient doesn’t have any metallic implants or devices that could be affected by the strong magnetic field, preventing a potential severe complication. Following these detailed protocols ensures the safety and well-being of all patients.
Q 4. What quality control measures do you employ for diagnostic equipment?
Quality control (QC) for diagnostic equipment is crucial for consistent image quality and accurate diagnoses. We employ a multi-faceted approach, including regular preventative maintenance, rigorous quality assurance tests (QA), and image quality checks. Preventive maintenance, scheduled regularly by the manufacturer’s recommendations, ensures the optimal functioning of the equipment. This involves regular inspections of various components, checking for wear and tear and calibration verification. QA tests are performed using phantoms—objects designed to mimic human anatomy—allowing us to assess image quality, spatial resolution, and other performance parameters. We maintain meticulous logs documenting all QC and QA procedures and results. We also use standardized image quality tests to assess the performance of the entire imaging chain, from the source to the displayed image.
For instance, we regularly perform phantom tests on our CT scanner to verify its slice thickness accuracy, spatial resolution, and low contrast detectability. These objective measures ensure consistent image quality and enable us to address any degradation promptly.
Q 5. Describe your troubleshooting skills when dealing with malfunctioning equipment.
Troubleshooting malfunctioning equipment requires a systematic and logical approach. I begin by identifying the nature of the malfunction – is it a software issue, hardware problem, or a problem with the workflow? I then consult the equipment’s error logs, technical manuals, and troubleshooting guides. If the issue isn’t readily apparent, I systematically check different components, using diagnostic tools provided by the manufacturer. When necessary, I escalate the problem to the biomedical engineering team for expert intervention. Effective communication with the engineering team, providing clear descriptions of the issue and relevant data, is crucial for timely resolution. I also document all troubleshooting steps taken and the outcome, ensuring a record for future reference. This methodical approach is crucial for efficient problem-solving and minimizing downtime.
For example, if an MRI machine displays an error message related to its gradient coils, I would first check the coil temperature and then systematically investigate the gradient amplifier and power supply, documenting each step before escalating to the biomed team.
Q 6. How do you interpret diagnostic images and reports?
Interpreting diagnostic images and reports requires extensive training and experience. It involves a thorough analysis of the images, correlating findings with the patient’s clinical history and other relevant information. I start by identifying key anatomical structures and looking for any abnormalities or deviations from the norm. This might include changes in tissue density, shape, size, or signal intensity (for MRI). The interpretation is not done in isolation; it’s crucial to consider the clinical context – why the image was ordered, and what the clinician is seeking to understand. The final report should be clear, concise, and accurate, clearly communicating findings to the referring physician. Using standardized reporting terminology is essential for consistent communication. It’s essential to maintain a high standard of accuracy as the images directly impact patient care and treatment decisions.
For example, in an X-ray of a chest, the interpretation would involve analyzing for lung opacities suggesting pneumonia, fluid collections, or masses. My report will clearly describe these findings and their potential significance. A lack of attention to detail could lead to a missed diagnosis with serious consequences.
Q 7. Explain the differences between CT and MRI scans.
CT (Computed Tomography) and MRI (Magnetic Resonance Imaging) are both powerful imaging modalities, but they differ significantly in their principles of operation and the type of information they provide. CT uses X-rays to generate cross-sectional images, providing excellent bone detail and visualizing soft tissues to a lesser degree. It’s faster than MRI, making it suitable for patients who can’t remain still for extended periods. MRI, on the other hand, uses strong magnetic fields and radio waves to produce high-resolution images of soft tissues, making it superior for evaluating the brain, spinal cord, and other soft tissue structures. It doesn’t use ionizing radiation. CT excels in detecting bone fractures, hemorrhages, and acute injuries, while MRI is better at visualizing subtle abnormalities in soft tissues, such as tumors and ligaments.
Think of it like this: CT is like a detailed blueprint of the building’s structure (bones), while MRI is like a detailed map of the building’s interior (soft tissues) with superior resolution. The choice depends heavily on the clinical question.
Q 8. What are the limitations of ultrasound imaging?
Ultrasound, while a valuable non-ionizing imaging modality, has inherent limitations. Its effectiveness is heavily dependent on the acoustic properties of the tissues being imaged. For instance, air and bone significantly attenuate ultrasound waves, leading to poor image quality or complete signal loss in areas like the lungs or behind dense bone structures.
- Limited penetration depth: Ultrasound struggles to penetrate deeper tissues effectively, making it less suitable for imaging structures deep within the body, like the retroperitoneum.
- Operator dependence: Image quality is significantly influenced by the skill and experience of the sonographer. Proper transducer placement, selection, and adjustment of parameters are crucial for optimal results.
- Difficulties with gas-filled structures: As mentioned, air creates significant artifacts and shadowing, hindering visualization of structures behind gas pockets in the gastrointestinal tract or lungs.
- Inability to image bone effectively: Bone reflects most of the ultrasound waves, resulting in poor visualization of underlying structures.
- Difficulty differentiating between similar tissue densities: Ultrasound may struggle to distinguish between tissues with similar acoustic impedance, such as certain types of soft tissue masses.
For example, while ultrasound excels in visualizing the gallbladder and liver, it’s not ideal for assessing the spine or brain. Understanding these limitations is key to selecting the appropriate imaging modality for each clinical scenario.
Q 9. How do you maintain patient confidentiality when handling medical images?
Maintaining patient confidentiality when handling medical images is paramount. It’s a cornerstone of ethical medical practice and is governed by stringent regulations like HIPAA (in the US) and similar legislation in other countries. My approach involves several key strategies:
- Strict adherence to access control protocols: PACS systems (Picture Archiving and Communication Systems) and other image storage systems should be configured to restrict access to authorized personnel only. Passwords should be strong and regularly updated, and access logs should be meticulously maintained.
- Secure image storage and transmission: Images are stored on secure servers with encryption protocols in place to prevent unauthorized access and data breaches during transmission and storage. We use dedicated networks and secure file transfer methods.
- Data anonymization when appropriate: When images are used for teaching or research purposes, identifiable information is removed to protect patient privacy, following appropriate IRB protocols. This often involves removing patient names, medical record numbers, and other identifying features.
- Education and training: All staff are rigorously trained on HIPAA regulations and our institution’s policies regarding patient data confidentiality. This includes the responsible handling, storage, and transmission of medical images.
- Regular audits and compliance checks: We regularly audit our systems and processes to ensure they are compliant with all relevant regulations and best practices for data security.
For example, if I need to share images with a consulting specialist, I’d use secure email or a HIPAA-compliant file transfer service rather than relying on standard email or insecure cloud storage.
Q 10. What is your experience with PACS systems?
I have extensive experience with PACS systems, having worked with several different vendors and implementations over the past 10 years. My experience encompasses all aspects of PACS operation, from image acquisition and storage to retrieval, viewing, and distribution. I’m proficient in using various PACS interfaces to access and manage medical images. I’m familiar with the workflow involved, including quality control measures, image annotation, and integrating PACS with other hospital information systems (HIS) and radiology information systems (RIS).
In my previous role, I played a key role in migrating our department to a new PACS system, a complex process that involved meticulous planning, data migration, user training, and ongoing system maintenance and troubleshooting. This included optimizing image quality settings, ensuring seamless integration with our HIS, and creating efficient workflows to improve diagnostic turnaround times.
My familiarity extends to troubleshooting common PACS issues, such as image display problems, network connectivity issues, and system performance bottlenecks. I’m comfortable working with various vendors for support and resolving technical difficulties promptly.
Q 11. Describe your knowledge of radiation safety protocols.
Radiation safety protocols are crucial to minimize exposure to ionizing radiation for both patients and healthcare workers. My knowledge includes:
- ALARA principle: This principle, which stands for “As Low As Reasonably Achievable,” guides all decisions regarding radiation exposure, emphasizing minimizing radiation dose while maintaining diagnostic image quality.
- Radiation protection measures: These include proper shielding techniques (using lead aprons and other protective gear), optimization of imaging parameters (minimizing exposure time and adjusting kVp and mAs appropriately), and the use of collimators to restrict the radiation field to the area of interest.
- Quality assurance and quality control: Regular testing and calibration of imaging equipment are vital to ensure that it functions correctly and delivers the appropriate radiation dose.
- Personnel monitoring: Radiation dosimeters are worn by personnel regularly exposed to ionizing radiation, allowing for accurate tracking of cumulative exposure.
- Regulatory compliance: I’m familiar with relevant regulations and guidelines, including those set by the FDA and the NRC (in the US) or equivalent international regulatory bodies, ensuring adherence to all safety standards and reporting requirements.
For example, I regularly review images before releasing them to ensure optimal image quality is achieved using the lowest possible radiation dose. I’m adept at performing quality control checks on imaging equipment to ensure it operates correctly, and I meticulously follow all safety precautions to protect myself and my colleagues from unnecessary radiation exposure.
Q 12. Explain the ALARA principle in the context of diagnostic imaging.
The ALARA principle, “As Low As Reasonably Achievable,” is fundamental to radiation safety in diagnostic imaging. It’s not about eliminating all radiation, which would render diagnostic imaging impossible, but about constantly striving to reduce radiation exposure to the lowest level possible while still obtaining diagnostic quality images. This involves a balance between the need for diagnostic information and the potential harm of radiation exposure.
In practice, ALARA is implemented through several strategies: optimizing imaging parameters (kVp, mAs, time), using appropriate shielding, employing image post-processing techniques to improve image quality without retaking images, and utilizing advanced imaging techniques that reduce radiation exposure, such as iterative reconstruction in CT scans. Regular quality assurance measures for equipment also contribute significantly to ALARA compliance.
For example, choosing a lower mA setting while still maintaining diagnostic quality, employing collimation to reduce the irradiated field, using the appropriate imaging protocol for the patient’s size and age, and repeating an image only when absolutely necessary are all core applications of the ALARA principle.
Q 13. How do you handle emergency situations involving diagnostic equipment?
Handling emergency situations involving diagnostic equipment requires a calm and systematic approach. My experience involves a range of scenarios, from equipment malfunctions to patient emergencies requiring immediate imaging. My response involves:
- Prioritizing patient safety: This is the paramount consideration. If a patient’s condition requires immediate intervention, the equipment malfunction might need to be addressed after stabilizing the patient.
- Assessing the situation: Identifying the nature of the problem (equipment malfunction, power outage, software glitch, etc.) is the first step to effective response.
- Implementing contingency plans: We have established protocols for various scenarios, including backup equipment and alternative imaging modalities. This ensures minimal disruption in patient care.
- Contacting appropriate support staff: Depending on the issue, contacting the equipment vendor’s technical support, biomedical engineering, or the radiology department supervisor is vital.
- Documenting the event thoroughly: Accurate records are crucial for quality assurance, identifying trends, and improving future responses to similar situations.
For instance, during a power outage, we would immediately switch to backup power supplies and utilize portable equipment as needed to minimize delays in providing critical patient care. Post-event documentation and analysis would ensure we learn from the incident and develop strategies to prevent similar situations in the future.
Q 14. What is your experience with image archiving and retrieval systems?
My experience with image archiving and retrieval systems is extensive. I’m proficient in using various systems, including PACS and other image management solutions. My expertise encompasses:
- Data management: I’m familiar with the processes involved in organizing, storing, and retrieving medical images, ensuring efficient access by authorized users.
- Data security and compliance: I understand the importance of data security and regulatory compliance (like HIPAA) in managing medical images, safeguarding patient privacy.
- System maintenance and troubleshooting: I have experience in troubleshooting common issues in image archiving systems, ensuring system integrity and efficient operation.
- Image compression and storage optimization: I’m familiar with different image compression techniques to optimize storage space and bandwidth usage while maintaining image quality.
- Integration with other systems: I have experience integrating image archiving systems with other hospital information systems (HIS) and radiology information systems (RIS).
In one instance, I streamlined our image archiving processes by implementing a new image compression algorithm, which reduced storage costs by 30% while preserving image quality and minimizing retrieval times. My work ensures that the department has smooth and compliant storage and retrieval of all medical images.
Q 15. Describe your understanding of different contrast agents used in imaging.
Contrast agents are substances used to enhance the visibility of internal structures during medical imaging. They work by altering the signal that the imaging modality detects, making specific tissues or organs stand out more clearly. Different imaging modalities utilize different types of contrast agents.
X-ray and CT: Iodine-based contrast agents are most common. These agents are injected intravenously, swallowed, or administered rectally, depending on the area being imaged. They increase the tissue’s radiodensity, making it appear whiter on the image. For example, a patient undergoing a CT scan of the abdomen might receive intravenous iodinated contrast to better visualize the blood vessels and organs.
MRI: Gadolinium-based contrast agents are frequently used. These agents affect the magnetic properties of tissues, increasing the signal intensity and making certain structures more visible. Gadolinium is often used to highlight areas of inflammation or tumors in brain MRI scans.
Ultrasound: Ultrasound contrast agents, also known as microbubbles, are typically gas-filled microspheres. They enhance the echogenicity of blood flow or specific tissues, improving image quality and visualization of blood vessels and tumors. This is particularly useful in cardiac ultrasound to assess blood flow and perfusion.
The choice of contrast agent depends on the specific imaging modality and the clinical question being addressed. It’s crucial to assess a patient’s history for allergies or contraindications before administering any contrast agent.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you communicate effectively with patients and healthcare professionals?
Effective communication is paramount in my role. With patients, I prioritize clear and concise explanations of the procedure, addressing any concerns or anxieties they may have. I use plain language, avoiding medical jargon unless absolutely necessary, and I always ensure they understand the purpose of the examination and what to expect. I actively listen to their questions and concerns, creating a comfortable and trusting environment.
Communication with healthcare professionals involves accurate and timely reporting of findings and collaborating on the appropriate interpretation of images. This involves clear and concise dictation or reporting, utilizing standardized terminology and referencing specific image findings accurately. I actively participate in multidisciplinary team meetings, contributing to case discussions and sharing my expertise to ensure optimal patient care. For instance, I might present findings from a chest X-ray to a pulmonologist to support their diagnosis of pneumonia.
Q 17. Explain your experience with different types of transducers in ultrasound.
Transducers are the heart of ultrasound imaging; they convert electrical energy into mechanical energy (sound waves) and vice versa. Different transducers are designed for specific applications and anatomical locations due to their varying frequency and shape.
Linear array transducers: High frequency, providing excellent image resolution for superficial structures like skin, breast, and thyroid. They produce a rectangular image.
Curvilinear array transducers: Lower frequency, offering deeper penetration for imaging abdominal and pelvic organs. The image is sector shaped.
Phased array transducers: Used for cardiac imaging, allowing for real-time visualization of the heart. The image is sector-shaped and offers excellent temporal resolution.
Endocavity transducers: Small, specialized transducers used for transvaginal or transrectal examinations, providing high-resolution images of pelvic organs.
My experience encompasses using all these transducer types routinely, selecting the appropriate transducer based on the clinical indication and the patient’s anatomy. For example, I would choose a curvilinear transducer for an abdominal ultrasound but a linear transducer for a thyroid ultrasound.
Q 18. How do you perform quality assurance checks on diagnostic images?
Quality assurance (QA) of diagnostic images is crucial for accurate diagnosis and patient safety. QA involves regular checks of the equipment and the images themselves to ensure optimal performance and image quality.
Equipment QA: This involves daily and periodic checks of the equipment’s functionality, including calibrations, testing of image quality using phantoms (test objects with known characteristics), and assessment of the equipment’s overall performance. This ensures the equipment is functioning within acceptable parameters.
Image QA: This includes reviewing images for technical quality, ensuring proper patient identification, appropriate image labeling, and checking for artifacts that could affect interpretation. A systematic approach is used, employing checklists and protocols to ensure consistent quality control.
For example, a daily quality control check on an X-ray machine might involve verifying the exposure levels and reviewing test images from a quality control phantom. For ultrasound, phantom images are used to assess the spatial resolution, penetration depth, and grayscale performance of the system.
Q 19. What are the safety precautions for operating X-ray equipment?
Operating X-ray equipment requires strict adherence to safety protocols to minimize radiation exposure to both patients and staff. Key precautions include:
ALARA principle: As Low As Reasonably Achievable. This principle guides all radiation safety practices, emphasizing minimizing radiation exposure while maintaining diagnostic image quality.
Shielding: Lead aprons and thyroid shields are mandatory for personnel during X-ray procedures, providing protection from scattered radiation. Patients may also receive shielding where appropriate.
Distance: Maintaining a safe distance from the X-ray beam during exposure significantly reduces radiation exposure.
Time: Minimizing the duration of X-ray exposure is critical. Using appropriate technique factors (kVp, mAs) helps reduce exposure time.
Collimation: Restricting the X-ray beam to the area of interest reduces unnecessary radiation to surrounding tissues.
Regular radiation safety training and adherence to established protocols are essential to prevent radiation-related injuries. Failure to follow these protocols can result in unnecessary radiation exposure, posing long-term health risks.
Q 20. Describe your experience with image processing software.
My experience with image processing software spans various platforms and applications. These tools are essential for enhancing image quality, improving visualization, and performing quantitative measurements.
PACS (Picture Archiving and Communication System): I am proficient in using PACS systems for image storage, retrieval, and distribution. This involves navigating the system, accessing patient records, and managing image files efficiently. This is fundamental to everyday workflow.
Image processing software: I use specialized software for advanced image manipulation, such as windowing and leveling (adjusting brightness and contrast), image fusion, and 3D reconstructions. This allows for optimal visualization of anatomical details and subtle findings.
For example, I routinely use image processing software to adjust the windowing levels of a CT scan to better visualize bone structures or soft tissues depending on the clinical question. In certain scenarios, 3D reconstruction software is utilized to create three-dimensional models for better understanding of complex anatomical structures.
Q 21. How do you identify and address artifacts in diagnostic images?
Artifacts in diagnostic images are any features that don’t correspond to actual anatomical structures. They can be caused by various factors, including equipment malfunctions, patient movement, or limitations of the imaging technique. Identifying and understanding these artifacts is crucial for accurate image interpretation.
Motion artifacts: Blurring or streaking caused by patient movement during image acquisition. For example, in ultrasound, patient movement can lead to blurry images. In X-ray, motion can create streaks.
Metal artifacts: Caused by metallic objects within the field of view, producing bright streaks or shadows. Dental fillings are a common example.
Scatter radiation artifacts: In X-ray imaging, scatter radiation can degrade image quality and create a hazy appearance.
Ring artifacts (CT): Appear as circular artifacts, often due to detector malfunctions in CT scanners.
Addressing artifacts involves understanding their cause. For motion artifacts, instructing patients on proper positioning and breath-holding techniques is crucial. For metal artifacts, adjusting imaging parameters or utilizing specialized techniques might be necessary. Careful review and understanding of the imaging technique’s limitations are vital in minimizing the impact of artifacts on diagnosis. Whenever in doubt, it’s appropriate to consult with colleagues or radiologists to discuss any potential impact of artifacts on the interpretation of the results.
Q 22. What is your understanding of the different types of ionizing radiation?
Ionizing radiation is a type of energy that can remove electrons from atoms, creating ions. This process can damage living cells and DNA, making it crucial to handle it with utmost care in diagnostic imaging. There are several types, primarily categorized by their origin and properties:
- X-rays: Produced by bombarding a metal target with high-speed electrons. Widely used in medical imaging (radiography, CT scans) due to their ability to penetrate tissues to varying degrees depending on energy level.
- Gamma rays: High-energy electromagnetic radiation emitted from radioactive nuclei during nuclear decay. Used in nuclear medicine (e.g., PET scans) for imaging and therapy.
- Alpha particles: Relatively heavy, positively charged particles emitted during radioactive decay. They have low penetrating power, posing less external radiation hazard, but significant internal hazard if ingested or inhaled.
- Beta particles: High-speed electrons or positrons emitted during radioactive decay. They have moderate penetrating power, and their use in diagnostics is less common than X-rays and gamma rays.
Understanding these differences is critical for selecting appropriate equipment, optimizing imaging protocols, and implementing effective radiation safety measures. For example, lead shielding is more effective against X-rays than beta particles. The choice of radiation type depends heavily on the application; high-resolution imaging often requires X-rays, while metabolic processes might be better visualized with gamma-emitting radiotracers in PET scans.
Q 23. How do you maintain and calibrate specialized diagnostic equipment?
Maintaining and calibrating specialized diagnostic equipment is a multi-faceted process crucial for ensuring accurate and reliable results. It involves a combination of preventative maintenance, regular calibration checks, and adherence to strict quality control protocols.
- Preventative Maintenance: This includes regular cleaning, inspection for wear and tear, and lubrication of moving parts. For instance, daily checks on ultrasound probes for damage, and annual servicing of X-ray tubes are vital.
- Calibration: Calibration involves verifying the accuracy of the equipment against known standards. This requires specialized tools and trained personnel. For example, in CT scanning, calibration ensures that the Hounsfield units (HU) accurately reflect tissue density. Similar rigorous calibration procedures exist for ECG machines (voltage, time), endoscopes (optical clarity, light intensity), and other diagnostic instruments.
- Quality Control: This encompasses performing quality assurance tests regularly to assess the equipment’s performance. For example, using phantoms (objects mimicking human tissue) to test the consistency and accuracy of imaging techniques in CT or ultrasound. Detailed records of all maintenance and calibration activities must be meticulously kept.
Failure to maintain and calibrate equipment can lead to inaccurate diagnoses, compromised patient safety, and even legal ramifications. Regular upkeep is not just a technical requirement but an ethical responsibility.
Q 24. Explain your knowledge of different types of ECG leads and their placement.
Electrocardiograms (ECGs) use leads to record the electrical activity of the heart. Different lead configurations provide different perspectives on this activity. The standard 12-lead ECG utilizes:
- Limb Leads (I, II, III, aVR, aVL, aVF): These six leads utilize electrodes placed on the limbs (right arm, left arm, and left leg). They provide a view of the heart’s electrical activity in the frontal plane.
- Chest Leads (V1-V6): These six leads utilize electrodes placed on the chest wall at specific locations. They provide a view of the heart’s electrical activity in the horizontal plane.
Lead Placement: Precise placement of these electrodes is crucial. Limb lead placement is standardized: right arm (RA), left arm (LA), and left leg (LL). Chest leads (V1-V6) are placed in a specific sequence across the chest, with V1 typically placed on the right side of the sternum (breastbone) and V6 on the mid-axillary line.
Incorrect lead placement can significantly alter the ECG tracing, leading to misinterpretation and inaccurate diagnoses. For example, a misplaced V1 lead could misrepresent the amplitude and direction of the QRS complex, potentially masking underlying heart conditions. Proper training and adherence to established protocols are vital to ensure accurate lead placement.
Q 25. Describe your experience working with various types of endoscopes.
My experience encompasses a variety of endoscopes, each designed for specific applications within the body. These include:
- Rigid Endoscopes: These provide a clear, unobstructed view but are limited in terms of flexibility. They are commonly used for procedures requiring a straight line of sight, such as bronchoscopy (examining the airways) or rigid cystoscopy (examining the bladder).
- Flexible Endoscopes: These offer increased maneuverability, allowing exploration of complex anatomical structures. Examples include colonoscopes (for examining the large intestine), gastroscopes (for examining the stomach and esophagus), and laparoscopes (for minimally invasive surgery).
- Specialized Endoscopes: These are designed for particular tasks, such as video endoscopes (providing high-resolution images), therapeutic endoscopes (allowing for tissue biopsies or treatment), and capsule endoscopes (small, swallowable devices providing images of the small intestine).
Working with these devices involves a thorough understanding of their operation, sterilization protocols, and potential complications. For example, meticulous cleaning and disinfection are crucial to prevent infection transmission, and proper handling ensures the integrity of the delicate optical components. Each type demands specific expertise in operation and image interpretation; a colonoscopy requires different skills and knowledge compared to a bronchoscopy.
Q 26. How do you manage data security related to patient diagnostic information?
Data security related to patient diagnostic information is paramount. It involves adherence to strict regulations (e.g., HIPAA in the US) and the implementation of robust security measures. These include:
- Access Control: Restricting access to patient data based on the principle of least privilege. Only authorized personnel with a legitimate need should have access to specific information.
- Data Encryption: Encrypting patient data both in transit (during transmission) and at rest (when stored). This prevents unauthorized access even if a breach occurs.
- Secure Storage: Using secure storage systems, both physical (e.g., locked cabinets) and digital (e.g., encrypted servers and databases), to protect sensitive information.
- Regular Audits and Security Assessments: Conducting regular audits to identify vulnerabilities and ensure compliance with security policies. Penetration testing can help identify weaknesses in the system.
- Employee Training: Educating staff on proper data handling procedures, including password management, recognizing phishing attempts, and reporting security incidents.
Any breach of patient data can have serious consequences, from reputational damage to legal penalties. A proactive approach to data security is essential to protect both patients and the organization.
Q 27. What is your experience with remote diagnostics and telehealth applications?
Remote diagnostics and telehealth applications are transforming healthcare, allowing for the delivery of diagnostic services remotely. My experience includes:
- Remote Image Interpretation: Reviewing diagnostic images (X-rays, CT scans, etc.) transmitted electronically from remote locations, offering interpretations and reports to referring physicians.
- Tele-ECG Interpretation: Analyzing ECGs transmitted electronically, providing interpretations and recommendations for patient management.
- Remote Monitoring: Utilizing remote monitoring devices to collect patient data (e.g., vital signs) and transmit it to healthcare professionals for monitoring and intervention.
These technologies are particularly valuable in areas with limited access to specialized healthcare professionals. However, it’s crucial to address challenges such as ensuring image quality, maintaining data security, and addressing the limitations of remote physical examination. For example, image compression can affect diagnostic accuracy, hence appropriate standards and protocols are vital. Moreover, ensuring reliable communication and network connectivity is also crucial for successful remote diagnostics.
Q 28. Describe a time you had to adapt to new diagnostic equipment or technology.
A significant adaptation involved the transition from traditional film-based radiography to digital radiography (DR). Initially, there was a learning curve in understanding the new workflow, image acquisition techniques, and post-processing capabilities of DR systems.
The initial challenge was learning the new software and hardware. Film-based radiography involved a relatively straightforward process – exposure, processing, and interpretation. DR introduced various settings and parameters that needed to be adjusted to optimize image quality for various patient types and body parts. I overcame this by participating in intensive training provided by the manufacturer and seeking mentorship from experienced colleagues.
Furthermore, adapting to the digital image management system required understanding new protocols for archiving, retrieving, and transmitting images securely. The transition also involved understanding the subtle differences in image characteristics between film and digital modalities to ensure accurate interpretation. Ultimately, this transition significantly improved image quality, workflow efficiency, and the ability to share images with colleagues instantly, illustrating the value of embracing new technologies in improving healthcare delivery.
Key Topics to Learn for Use of Specialized Diagnostic Equipment Interview
- Equipment Operation & Maintenance: Understanding the operational principles of various diagnostic tools (e.g., X-ray machines, ultrasound devices, MRI scanners), including safety protocols and routine maintenance procedures.
- Image Acquisition & Processing: Mastering techniques for obtaining high-quality diagnostic images, utilizing image processing software for enhancement and analysis, and understanding image artifacts and their implications.
- Quality Assurance & Control: Implementing quality control measures to ensure accuracy and reliability of diagnostic results, understanding relevant regulations and standards, and troubleshooting equipment malfunctions.
- Radiation Safety & Protection: Adhering to radiation safety protocols, minimizing patient exposure, and understanding the biological effects of radiation.
- Data Interpretation & Analysis: Accurately interpreting diagnostic images, identifying key findings, and documenting observations effectively. This includes understanding the limitations of each modality.
- Patient Interaction & Communication: Effectively communicating with patients, explaining procedures, and addressing concerns. Maintaining professionalism and empathy throughout the diagnostic process.
- Troubleshooting & Problem Solving: Diagnosing equipment malfunctions, performing basic repairs, or escalating issues to appropriate personnel. Developing systematic approaches to resolving technical challenges.
- Emerging Technologies & Trends: Staying updated on advancements in diagnostic imaging technology, including new modalities and techniques.
Next Steps
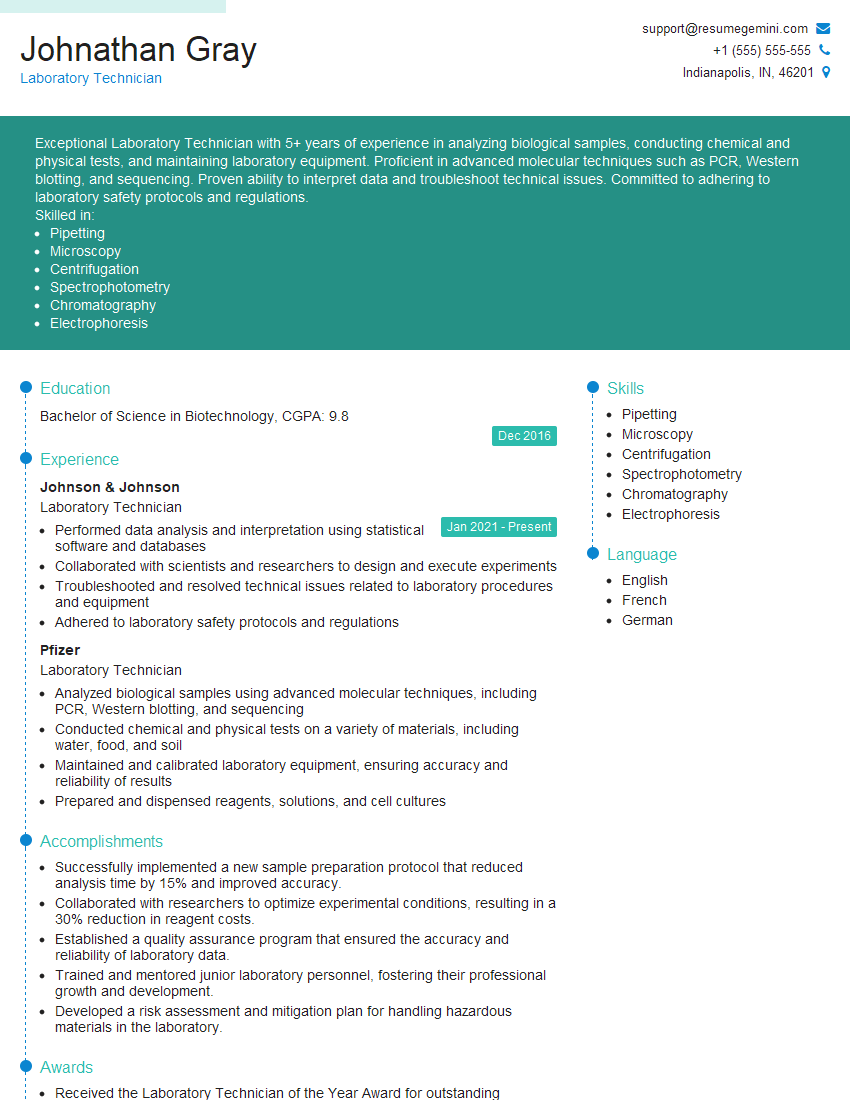
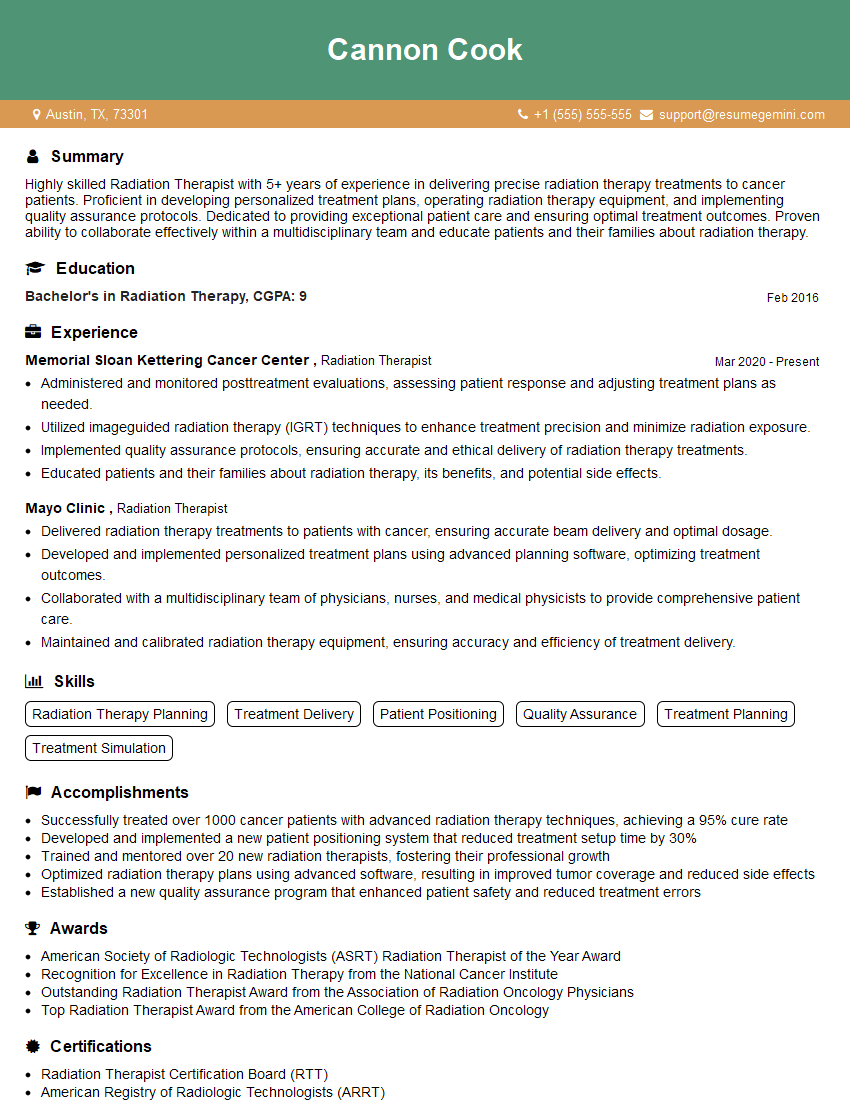
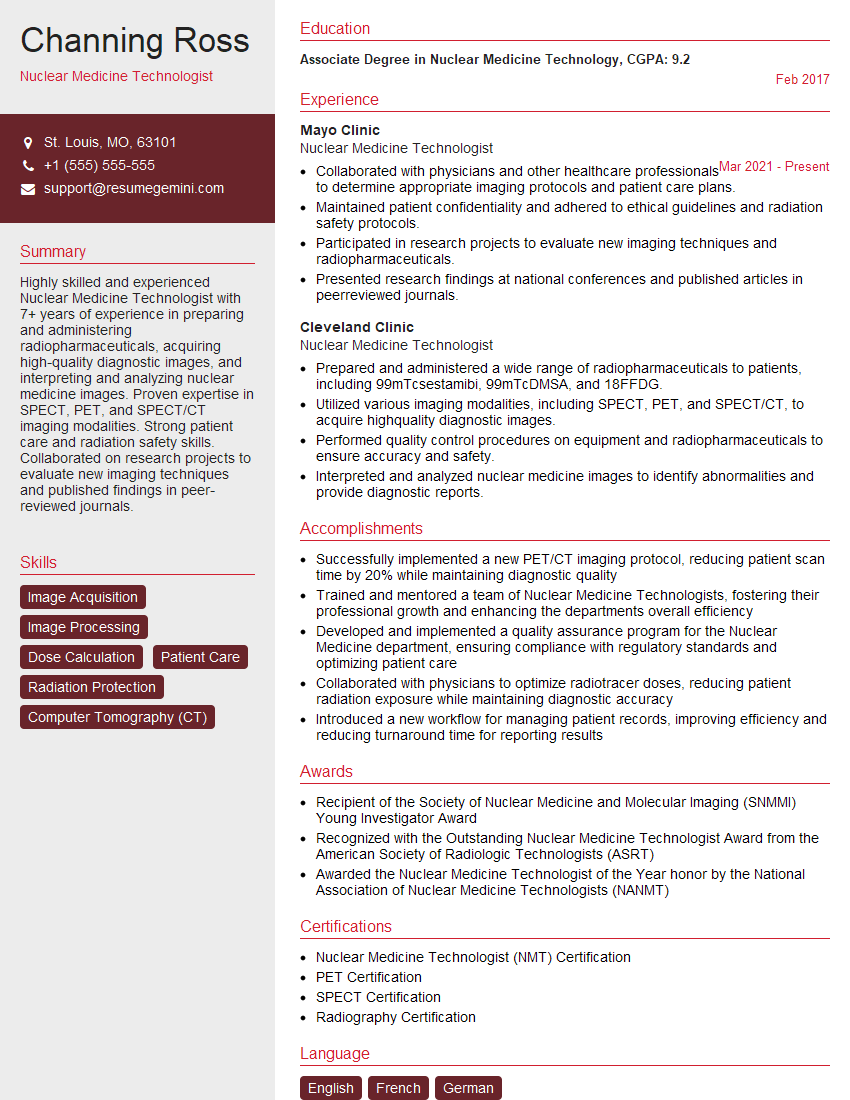
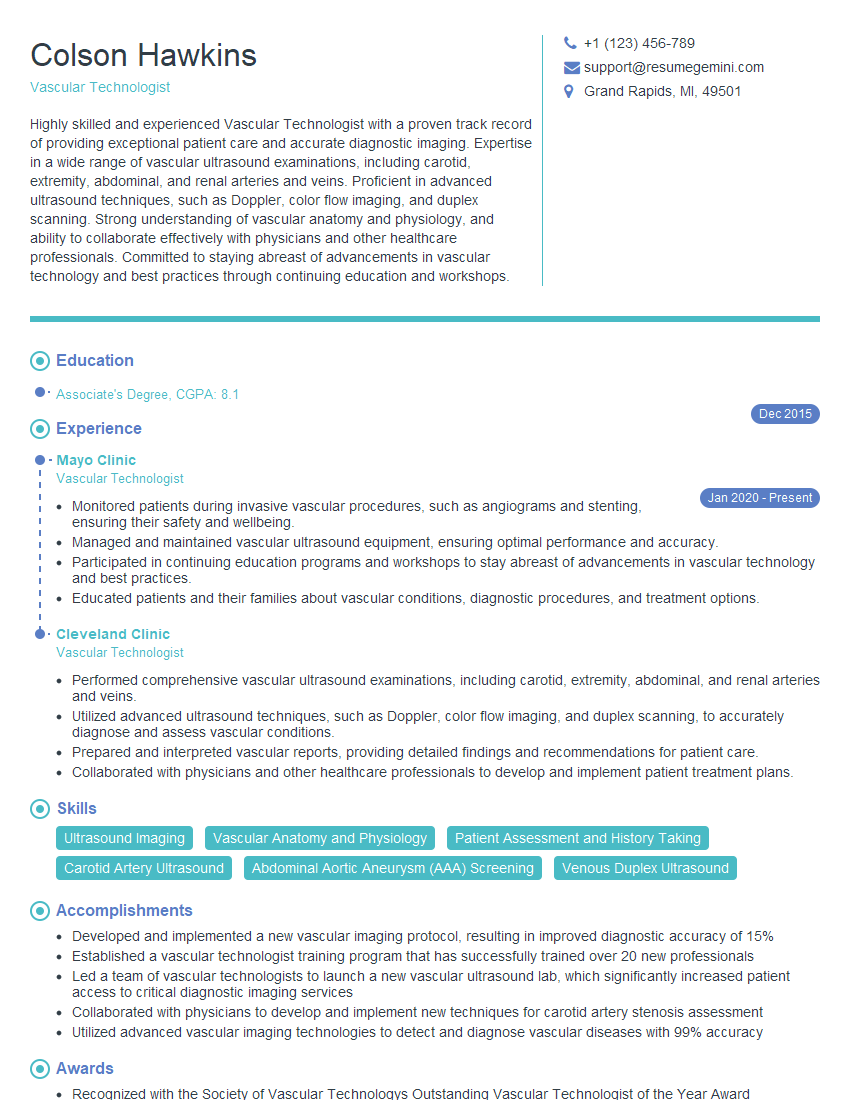
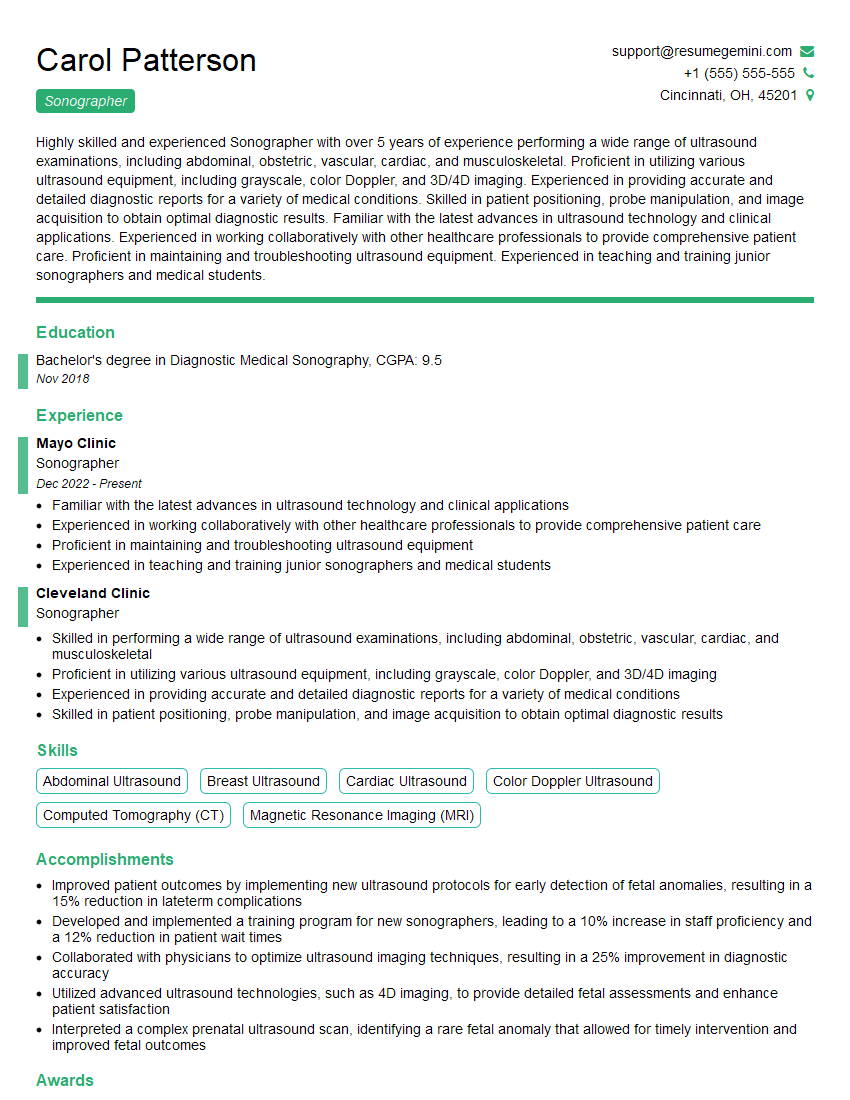
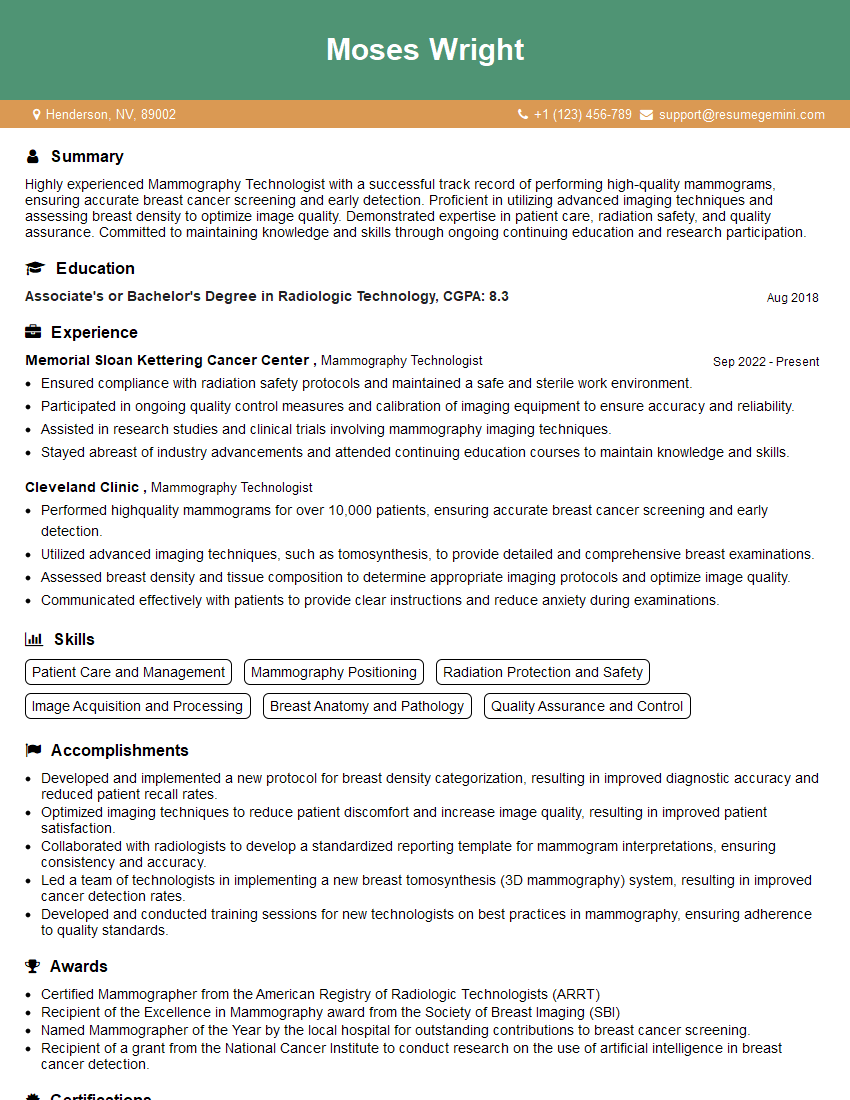
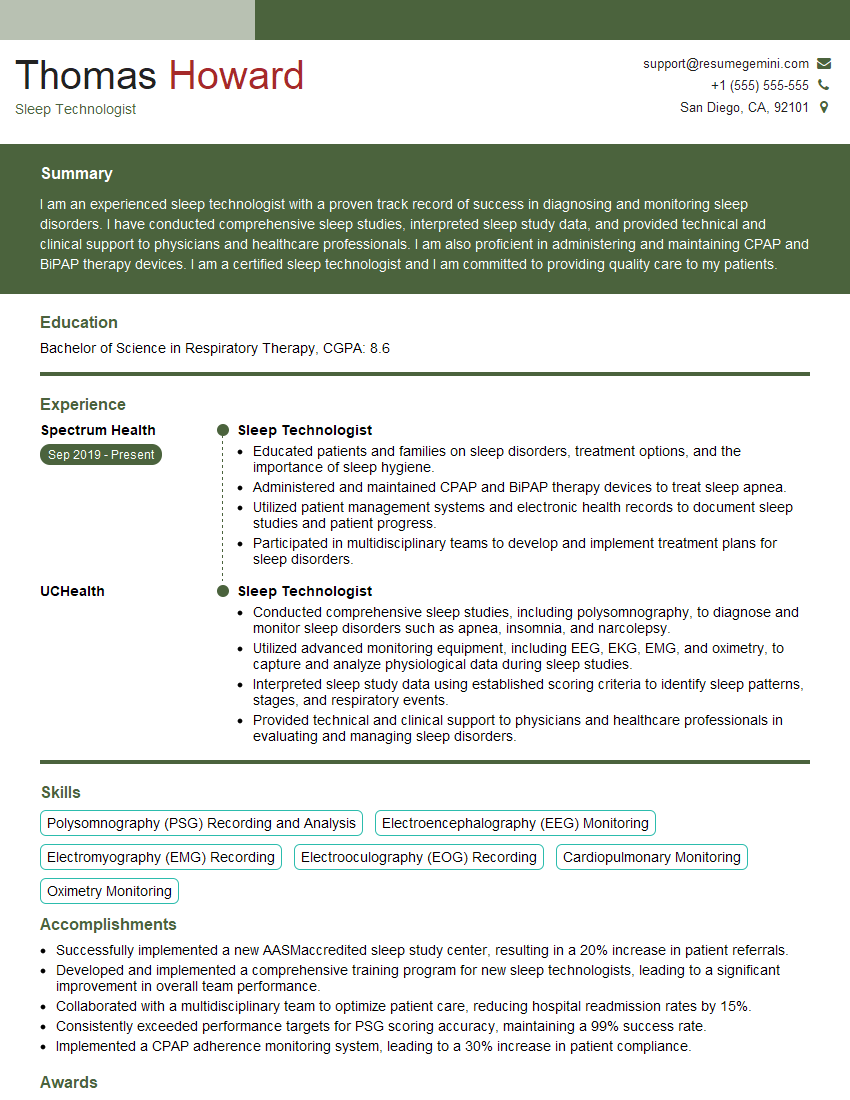
Mastering the use of specialized diagnostic equipment is crucial for career advancement in the healthcare field, opening doors to specialized roles and increased earning potential. A strong resume is your key to unlocking these opportunities. Crafting an ATS-friendly resume that highlights your skills and experience is essential. ResumeGemini can help you build a professional, impactful resume tailored to the demands of the job market. ResumeGemini provides examples of resumes specifically designed for professionals in Use of Specialized Diagnostic Equipment, offering valuable templates and guidance to help you stand out from the competition.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO