Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Behavioural Health interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Behavioural Health Interview
Q 1. Explain the difference between anxiety and depression.
While anxiety and depression often coexist, they are distinct conditions. Anxiety is characterized by excessive worry, fear, and nervousness, often manifesting as physical symptoms like a racing heart, shortness of breath, and trembling. It’s about anticipating future threats. Think of it like a car constantly revving its engine, even when not moving. Depression, on the other hand, is marked by persistent sadness, loss of interest in activities, feelings of hopelessness and worthlessness, and changes in sleep and appetite. It’s a pervasive feeling of being stuck in the mud. Imagine a car that’s stalled and won’t start.
For example, someone with anxiety might constantly worry about a presentation at work, leading to physical symptoms days before. Someone with depression might withdraw from social events and lose pleasure in activities they once enjoyed, even experiencing feelings of intense sadness and despair.
Q 2. Describe the stages of grief and loss.
The Kübler-Ross model describes five stages of grief, but it’s crucial to understand that these stages aren’t linear; individuals may experience them in a different order, skip stages, or revisit them. These stages are:
- Denial: A refusal to accept the loss. This is a protective mechanism, allowing time to process the enormity of the situation.
- Anger: Frustration and resentment directed towards oneself, others, or even a higher power. This stage represents the struggle to accept the reality of the loss.
- Bargaining: Attempting to negotiate with a higher power or fate to change the outcome. This is often fueled by a desire to undo the loss.
- Depression: Overwhelming sadness, hopelessness, and despair. This reflects the true weight of the loss.
- Acceptance: Coming to terms with the loss and finding a way to move forward. This doesn’t mean happiness, but rather a sense of peace and resolution.
For instance, someone grieving the loss of a loved one might initially deny the reality of their death, then become angry at the unfairness of it all. They might bargain with God or fate, later falling into deep depression before finally accepting the loss and finding ways to remember their loved one.
Q 3. What are the common symptoms of PTSD?
Post-Traumatic Stress Disorder (PTSD) is triggered by experiencing or witnessing a traumatic event. Common symptoms can be categorized into four clusters:
- Intrusive Re-experiencing: Flashbacks, nightmares, intrusive thoughts, or intense distress when exposed to reminders of the trauma.
- Avoidance: Efforts to avoid memories, thoughts, feelings, or situations associated with the trauma.
- Negative Alterations in Cognition and Mood: Inability to remember aspects of the trauma, persistent negative beliefs about oneself or the world, distorted sense of blame, feeling detached from others, and persistent negative emotional state.
- Alterations in Arousal and Reactivity: Irritability, reckless or self-destructive behavior, hypervigilance, exaggerated startle response, difficulty sleeping, and concentration problems.
For example, a veteran might experience flashbacks of combat, avoid watching war movies, have difficulty sleeping, and be easily startled by loud noises. A survivor of a car accident might have nightmares about the accident, feel constantly on edge, and struggle to concentrate at work.
Q 4. What are some evidence-based treatments for substance abuse disorder?
Evidence-based treatments for Substance Use Disorder (SUD) typically involve a combination of approaches tailored to the individual’s needs. These include:
- Medication-Assisted Treatment (MAT): Medications like methadone, buprenorphine, or naltrexone can reduce cravings and withdrawal symptoms, making it easier to abstain.
- Cognitive Behavioral Therapy (CBT): Helps individuals identify and change negative thinking patterns and behaviors that contribute to substance use.
- Motivational Interviewing (MI): A collaborative approach that helps individuals explore their ambivalence about change and strengthen their intrinsic motivation to recover.
- Contingency Management (CM): Uses rewards and consequences to reinforce abstinence and encourage positive behavior changes.
- 12-Step Facilitation (TSF): Guides individuals through the 12 steps of Alcoholics Anonymous (AA) or Narcotics Anonymous (NA), emphasizing community support and spiritual growth.
For instance, a person struggling with opioid addiction might benefit from MAT with buprenorphine, combined with CBT to address underlying issues contributing to their substance use. This integrated approach offers the best chance of long-term recovery.
Q 5. Explain the principles of Cognitive Behavioral Therapy (CBT).
Cognitive Behavioral Therapy (CBT) is a structured, goal-oriented approach that focuses on the interplay between thoughts, feelings, and behaviors. The core principles are:
- Thoughts influence feelings and behaviors: Our thoughts are not necessarily facts, but they powerfully shape our emotional and behavioral responses.
- Identifying and challenging maladaptive thoughts: CBT helps individuals identify negative or unhelpful thought patterns (cognitive distortions) and challenge their validity.
- Developing coping skills: CBT equips individuals with strategies to manage difficult emotions and situations.
- Behavioral experiments: Testing out new behaviors and observing their impact on thoughts and feelings.
For example, someone with social anxiety might have the thought, “Everyone will judge me if I speak up in the meeting.” CBT would help them challenge this thought by examining the evidence for and against it, developing coping skills like deep breathing, and gradually practicing speaking up in less intimidating situations.
Q 6. How would you assess a client’s risk for suicide?
Assessing suicide risk requires a comprehensive and sensitive approach. It involves gathering information from multiple sources, including the client’s self-report, collateral information from family and friends, and clinical observation. Key factors to consider include:
- Suicidal Ideation: The presence and frequency of thoughts about suicide, including plans and intentions.
- Hopelessness: A pervasive feeling of despair and lack of control over one’s life.
- Impulsivity: A tendency to act on thoughts and feelings without considering the consequences.
- Access to lethal means: Availability of firearms, medications, or other methods that could be used for suicide.
- History of suicide attempts: Past attempts are significant risk factors.
- Major life stressors: Recent losses, relationship problems, financial difficulties, or other significant stressors.
- Mental health disorders: The presence of depression, anxiety, schizophrenia, or other mental illnesses significantly increases suicide risk.
A structured risk assessment tool, combined with clinical judgment, can help determine the level of risk and guide the development of a safety plan. The process is iterative and requires ongoing monitoring.
Q 7. What are the ethical considerations in maintaining client confidentiality?
Maintaining client confidentiality is paramount in behavioral health. Ethical considerations include:
- Duty to Warn/Protect: Exceptions to confidentiality exist when there’s a credible threat of harm to the client or others. This requires careful judgment and often involves consultation with supervisors or legal professionals.
- Informed Consent: Clients must be fully informed about the limits of confidentiality before treatment begins.
- Data Security: Protecting client information from unauthorized access, use, or disclosure through secure storage and transmission methods. This includes adherence to HIPAA regulations (in the US).
- Record Keeping: Maintaining accurate and complete records in accordance with professional and legal standards. Records must be stored securely and only accessed by authorized personnel.
- Professional Boundaries: Maintaining appropriate professional relationships with clients, avoiding dual relationships that could compromise confidentiality or objectivity.
For example, if a client reveals plans to harm someone, the therapist has a legal and ethical obligation to take appropriate steps, which may include notifying the intended victim and/or law enforcement. Furthermore, all client records must be kept secure, with access limited to authorized personnel only.
Q 8. Describe your experience with crisis intervention.
My experience with crisis intervention spans over ten years, encompassing work in both inpatient and outpatient settings. I’ve managed a wide range of crises, from suicidal ideation and self-harm to acute psychotic episodes and severe anxiety attacks. My approach is rooted in a rapid assessment of risk, followed by immediate stabilization and development of a safety plan. This involves actively listening to the individual, validating their feelings, and collaboratively creating strategies to manage the immediate crisis and prevent future occurrences. For instance, I once worked with a young man experiencing a severe panic attack. My first step was to create a safe and calming environment. I then used breathing techniques and grounding exercises to help him regain control. We discussed the triggers of his anxiety and collaboratively developed a plan involving coping strategies, medication management (in conjunction with his psychiatrist), and ongoing therapy. Ultimately, the focus is always on de-escalation, safety, and connecting the individual with appropriate ongoing support.
Q 9. How would you handle a client who is resistant to treatment?
Resistance to treatment is a common challenge in behavioral health. I approach it with empathy and understanding, recognizing that resistance often stems from underlying fears, mistrust, or previous negative experiences. My strategy involves building a strong therapeutic alliance based on trust and respect. I start by actively listening to the client’s concerns and validating their feelings. I avoid confrontation and instead aim to collaboratively explore the reasons for their resistance. This often involves motivational interviewing techniques, focusing on identifying the client’s own goals and values, and exploring how treatment can help them achieve those goals. For example, if a client expresses reluctance to participate in group therapy, I would explore their specific concerns. Perhaps it’s a fear of judgment or a preference for individual sessions. By addressing these concerns directly, we can collaboratively find an approach that works for them – perhaps starting with individual sessions and gradually incorporating group activities as they feel more comfortable.
Q 10. What is your approach to working with clients from diverse cultural backgrounds?
Working with clients from diverse cultural backgrounds requires cultural humility and sensitivity. This means acknowledging my own biases, actively seeking to understand the client’s cultural perspective, and adapting my approach accordingly. It’s crucial to avoid imposing my own cultural norms and instead collaborate with the client to develop a culturally sensitive treatment plan. This includes understanding the client’s beliefs about mental health, their preferred communication styles, and the role of family and community in their lives. For instance, when working with a client from a collectivist culture, family involvement might be vital for successful treatment. Similarly, understanding the client’s religious or spiritual beliefs can inform the therapeutic process and ensure that interventions are compatible with their values. In essence, it’s about tailoring the therapeutic relationship and intervention to the unique cultural context of the individual.
Q 11. Explain the diagnostic criteria for a specific mental health disorder (e.g., Major Depressive Disorder).
Major Depressive Disorder (MDD), according to the DSM-5, requires a persistent low mood or loss of interest or pleasure (anhedonia) for at least two weeks, accompanied by at least four additional symptoms. These symptoms can include significant weight loss or gain, insomnia or hypersomnia, fatigue or loss of energy, feelings of worthlessness or excessive guilt, diminished ability to think or concentrate, and recurrent thoughts of death or suicide. The symptoms must cause clinically significant distress or impairment in social, occupational, or other important areas of functioning and cannot be attributable to another medical condition or substance use. It’s important to note that the severity and presentation of MDD can vary greatly between individuals. A proper diagnosis requires a thorough clinical assessment by a qualified professional.
Q 12. How do you differentiate between different types of anxiety disorders?
Differentiating between anxiety disorders involves careful assessment of the specific symptoms, triggers, and the context in which they occur. For example, Generalized Anxiety Disorder (GAD) is characterized by persistent and excessive worry about various events and activities, while Panic Disorder involves recurrent unexpected panic attacks – discrete periods of intense fear or discomfort. Social Anxiety Disorder (SAD) centers around intense fear of social situations and scrutiny, whereas Specific Phobias involve an irrational fear of specific objects or situations. Obsessive-Compulsive Disorder (OCD) is defined by recurrent obsessions (intrusive thoughts) and compulsions (repetitive behaviors) aimed at reducing anxiety. A proper diagnosis requires a comprehensive evaluation that considers the duration, frequency, intensity, and impact of the symptoms on the individual’s life. The key is to understand the specific pattern of symptoms, triggers, and their impact on daily functioning to accurately differentiate between these conditions.
Q 13. Describe your experience utilizing different therapeutic modalities.
My experience encompasses a range of therapeutic modalities, including Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and psychodynamic therapy. CBT is particularly effective in addressing thought patterns and behaviors contributing to mental health challenges. For instance, I use CBT techniques to help clients identify and challenge negative automatic thoughts and develop more adaptive coping mechanisms. DBT, on the other hand, is excellent for managing intense emotions and improving interpersonal relationships, often beneficial for clients with borderline personality disorder. Psychodynamic therapy helps clients explore unconscious patterns and past experiences affecting their current functioning. The choice of modality is tailored to the individual client’s needs and preferences, often integrating elements from different approaches for a more holistic and effective treatment plan.
Q 14. How would you collaborate with a multidisciplinary treatment team?
Collaboration with a multidisciplinary team is crucial for providing comprehensive care. My approach involves regular communication and coordination with psychiatrists, nurses, case managers, and other relevant professionals. This collaboration ensures that the client receives a cohesive and integrated approach to their treatment. I actively participate in team meetings, contribute my clinical expertise, and ensure that the client’s treatment plan is consistent across different settings. Open communication channels are essential, allowing for seamless exchange of information and a shared understanding of the client’s progress. Regular updates on the client’s status, treatment response, and any emerging concerns are fundamental to effective teamwork. This integrated approach optimizes client outcomes and fosters a supportive environment for both the client and the treatment team.
Q 15. What is your experience with documentation and record-keeping?
Accurate and meticulous documentation is the cornerstone of ethical and effective behavioral health practice. My experience encompasses comprehensive charting within Electronic Health Records (EHRs), adhering to HIPAA regulations and all relevant professional standards. This includes detailed progress notes reflecting sessions with clients, incorporating assessments, treatment plans, and measurable outcomes. I’m proficient in using various coding systems (e.g., ICD-10, CPT) to ensure accurate billing and data analysis for tracking treatment efficacy. For instance, in my previous role, I implemented a new documentation system which improved efficiency by 15% and reduced audit errors to zero.
Beyond the EHR, I’m skilled in maintaining client files, both physical and digital, securely and confidentially. This involves proper disposal of sensitive information and adhering to all relevant data privacy laws. I regularly participate in continuing education to stay abreast of the latest best practices in documentation and record-keeping.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you maintain your own mental health and wellbeing as a behavioral health professional?
Self-care is not just a buzzword; it’s a non-negotiable for behavioral health professionals. The demanding nature of our work requires intentional strategies to maintain mental and emotional wellbeing. My approach is multifaceted. Firstly, I prioritize setting healthy boundaries: I maintain a strict work-life balance, making time for hobbies outside work to avoid burnout. For example, I enjoy hiking and meditation, activities that help clear my mind and alleviate stress.
Secondly, I prioritize my physical health: regular exercise, a balanced diet, and sufficient sleep are essential. I also actively engage in peer supervision and consultation, discussing challenging cases and processing my experiences with trusted colleagues. This provides a valuable support network and helps prevent compassion fatigue. Finally, I practice self-compassion; I acknowledge that even as a professional, I’m human and will face challenges. This involves being kind to myself when things are difficult and seeking professional support when needed.
Q 17. Describe a challenging case and how you approached it.
One particularly challenging case involved a young adult struggling with severe anxiety and depression, complicated by a history of childhood trauma. Initial sessions were marked by significant resistance and difficulty establishing trust. The client demonstrated significant emotional dysregulation and expressed feelings of hopelessness and worthlessness.
My approach was rooted in building a strong therapeutic alliance. I prioritized active listening and validation, focusing on creating a safe and non-judgmental space. We gradually explored the client’s trauma history using a trauma-informed approach, focusing on empowerment and self-agency rather than retraumatization. I incorporated evidence-based techniques such as Cognitive Behavioral Therapy (CBT) and mindfulness practices to manage anxiety symptoms. We also utilized a collaborative treatment plan, regularly reviewing and adjusting strategies based on the client’s progress and feedback.
The process was lengthy, requiring patience and flexibility. However, over time, the client began to demonstrate increased self-awareness, improved coping mechanisms, and a significant reduction in their symptoms. The success of this case highlighted the importance of tailored therapeutic interventions, a collaborative approach, and prioritizing the therapeutic relationship.
Q 18. How do you handle conflict resolution within a therapeutic setting?
Conflict resolution within the therapeutic setting requires a delicate balance of maintaining boundaries while fostering a safe and collaborative space. My approach focuses on early identification and proactive management of potential conflicts. This may involve setting clear expectations at the outset of therapy regarding communication styles and treatment goals.
If conflicts arise, I utilize a structured approach: I begin by actively listening to all parties involved, aiming to understand each perspective without judgment. I then work to facilitate open communication, helping clients articulate their needs and concerns constructively. The goal is not to ‘solve’ the conflict for the client, but to empower them to develop their own conflict resolution skills. If the conflict significantly impacts the therapeutic process, or if it involves ethical or legal concerns, I may consult with supervisors or seek additional consultation.
For example, if two clients in a group therapy setting have a disagreement, I would guide them to use ‘I’ statements, actively listen to each other, and brainstorm solutions together. This emphasizes collaboration and mutual respect, while reinforcing the importance of healthy communication within the therapeutic environment.
Q 19. What is your understanding of the DSM-5?
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), is a widely used classification system for mental disorders. It provides a standardized framework for clinicians to diagnose and understand a wide range of conditions, aiding in treatment planning and research. The DSM-5 uses a descriptive approach, detailing criteria for each diagnosis to ensure reliability and consistency across different settings and practitioners.
My understanding of the DSM-5 goes beyond mere diagnosis. I recognize its limitations, such as the potential for over-diagnosis or misdiagnosis, the impact of cultural factors on presentation, and the inherent complexity of human behavior. Therefore, I use the DSM-5 as a guide within a holistic assessment process. This involves considering the client’s individual history, cultural background, and presenting symptoms to arrive at a comprehensive understanding of their experience rather than relying solely on diagnostic labels. This ensures person-centered care.
Q 20. Explain the concept of trauma-informed care.
Trauma-informed care is a philosophical approach that recognizes the pervasive impact of trauma on individuals and communities. It shifts the focus from a ‘what’s wrong with you’ perspective to a ‘what happened to you’ perspective. This means understanding that past experiences of trauma, abuse, or neglect can significantly shape an individual’s current behaviors, emotions, and relationships.
A trauma-informed approach emphasizes safety, trustworthiness, choice, collaboration, and empowerment. In practice, this involves creating a safe and supportive environment where clients feel heard, respected, and validated. It involves avoiding potentially triggering language or behaviors, providing choices whenever possible, and empowering clients to take control of their own recovery journey. It also considers the potential for retraumatization in therapeutic interactions and actively works to prevent it. For example, avoiding coercive or controlling language and providing clear explanations are key aspects.
Q 21. How do you assess a client’s strengths and resources?
Assessing a client’s strengths and resources is crucial for developing an effective treatment plan and fostering resilience. It involves moving beyond identifying problems and focusing on what the client brings to the therapeutic process. My approach is multifaceted and involves several strategies.
Firstly, I use a strengths-based perspective in all assessments. This includes actively listening for signs of resilience, coping mechanisms, and positive relationships. I may use structured assessments, such as questionnaires or inventories, to gather objective data on strengths and resources. I also actively explore the client’s social support network, identifying family, friends, or community resources that can provide assistance.
Secondly, I collaborate with the client to identify their own strengths and resources. I may use open-ended questions, such as ‘What are some things you’re proud of?’ or ‘What are some skills or talents you have?’ This collaborative approach empowers the client and emphasizes their active role in their recovery. For instance, a client might initially focus on their weaknesses, but through exploration, reveal hidden talents or previous successes that can be leveraged in the treatment process.
Q 22. Describe your experience with medication management (if applicable).
While I don’t personally prescribe medication, my experience in behavioral health involves extensive collaboration with prescribing psychiatrists and primary care physicians. This collaboration is crucial for holistic patient care. My role focuses on assessing a client’s symptoms, providing detailed information regarding their mental health status, and working closely with the medical team to monitor medication effectiveness and address any side effects. For example, I might observe a client experiencing increased anxiety after starting a new medication. I would then communicate this observation to the prescribing physician, who could adjust the dosage or consider alternative treatment options. This collaborative approach ensures the medication regimen aligns with the client’s therapeutic goals and overall well-being. I am also adept at educating clients about their medication, including its purpose, potential side effects, and the importance of adherence to the prescribed regimen.
Q 23. What is your understanding of the legal and regulatory aspects of behavioral health?
Understanding the legal and regulatory aspects of behavioral health is paramount. This includes HIPAA (Health Insurance Portability and Accountability Act) regulations regarding client confidentiality, which are fundamental to building trust and ensuring ethical practice. I am well-versed in mandated reporting laws, understanding my obligations to report suspected child abuse, elder abuse, or situations where a client poses a danger to themselves or others. I also stay current on state and federal laws governing the practice of behavioral health, including licensure requirements and professional boundaries. For instance, I am familiar with the nuances of informed consent procedures, ensuring clients understand their rights and the implications of treatment before beginning therapy. This includes explaining the limits of confidentiality and any potential risks associated with the therapeutic process.
Q 24. What are your strategies for managing your caseload effectively?
Effective caseload management requires a structured and organized approach. I use a combination of electronic health records (EHRs) to track client progress, appointments, and documentation. I prioritize tasks based on urgency and client need, focusing on those requiring immediate attention. Time blocking within my schedule ensures allocated time for specific tasks, such as client sessions, administrative work, and continuing education. Regular review of my caseload allows me to identify potential scheduling conflicts or clients who might require additional support. Furthermore, I proactively communicate with clients regarding scheduling and any potential delays, maintaining transparency and fostering a strong therapeutic alliance. Delegating tasks when appropriate and setting realistic goals prevents burnout and allows for efficient and effective case management.
Q 25. How do you incorporate evidence-based practices into your therapeutic approach?
My therapeutic approach is grounded in evidence-based practices. For example, when working with clients struggling with depression, I utilize Cognitive Behavioral Therapy (CBT) techniques to identify and challenge negative thought patterns and develop more adaptive coping mechanisms. For clients with anxiety, I might employ Exposure and Response Prevention (ERP) techniques, a cornerstone of treatment for obsessive-compulsive disorder (OCD). I regularly consult research literature and attend professional development workshops to stay abreast of the latest evidence-based interventions. I tailor my approach to the individual needs of each client, considering their unique circumstances, cultural background, and preferences. This ensures that treatment is not only effective but also respectful and culturally sensitive.
Q 26. How do you build rapport with clients?
Building rapport with clients is essential for successful therapy. I begin by creating a safe and welcoming environment where clients feel comfortable sharing their experiences. Active listening is paramount; I pay close attention to both verbal and nonverbal cues, reflecting back what I hear to ensure understanding. Empathy and genuine interest in the client’s well-being are crucial; I strive to understand their perspective and validate their feelings. I also demonstrate respect for their autonomy and make sure they feel empowered in the therapeutic process. For example, I start sessions by asking open-ended questions like, “What’s been on your mind lately?” This encourages them to take the lead and share what is most important to them.
Q 27. Describe your approach to providing culturally competent care.
Providing culturally competent care involves recognizing and respecting the diverse cultural backgrounds, beliefs, and values of my clients. I acknowledge that cultural factors significantly influence mental health experiences and treatment preferences. I actively seek to understand the cultural context of a client’s challenges and avoid imposing my own cultural biases onto the therapeutic process. This includes being mindful of language barriers and utilizing interpreters when necessary. I also stay informed about cultural differences in communication styles, family dynamics, and expressions of emotion. For instance, I adapt my therapeutic approach to resonate with a client’s specific cultural background, ensuring that my interventions are relevant and culturally sensitive. This may involve incorporating culturally appropriate metaphors, collaborating with community leaders, or simply demonstrating cultural awareness throughout sessions.
Q 28. Explain your understanding of motivational interviewing.
Motivational Interviewing (MI) is a client-centered, directive counseling approach designed to elicit and strengthen motivation for change. It’s built on the principles of collaboration, evocation, and autonomy. Rather than directly advising or imposing solutions, MI helps clients explore and resolve their ambivalence towards change. The core skills of MI include open-ended questions, affirming the client’s strengths, reflective listening, and summarizing to ensure understanding. For example, a client struggling with substance abuse might express both a desire to quit and a fear of the challenges involved. Using MI, I would explore these conflicting feelings, highlighting their strengths and resources while guiding them to discover their own reasons for change. This collaborative process empowers the client to take ownership of their journey and increases their commitment to achieving their goals.
Key Topics to Learn for Your Behavioural Health Interview
- Diagnostic and Statistical Manual of Mental Disorders (DSM-5): Understand the diagnostic criteria for common mental health disorders and their implications for treatment planning.
- Therapeutic Approaches: Familiarize yourself with various therapeutic modalities such as Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and psychodynamic therapy. Be prepared to discuss their strengths, weaknesses, and appropriate applications.
- Crisis Intervention and Risk Assessment: Master the skills needed to effectively assess and manage individuals in crisis situations, including suicide risk assessment and intervention strategies.
- Ethical and Legal Considerations: Develop a strong understanding of ethical principles in behavioural health, including confidentiality, informed consent, and mandated reporting.
- Case Management and Treatment Planning: Practice developing comprehensive treatment plans tailored to individual needs, considering biopsychosocial factors and coordinating care with other professionals.
- Cultural Competence and Diversity: Demonstrate awareness of cultural influences on mental health and the importance of providing culturally sensitive and appropriate care.
- Evidence-Based Practices: Understand the importance of using empirically supported treatments and interventions, and be able to discuss relevant research findings.
- Trauma-Informed Care: Learn about the impact of trauma on mental health and how to apply trauma-informed principles in your practice.
- Substance Use Disorders: Understand the assessment and treatment of co-occurring mental health and substance use disorders.
- Communication and Interpersonal Skills: Develop your skills in establishing rapport, active listening, empathy, and clear communication with clients, families, and colleagues.
Next Steps
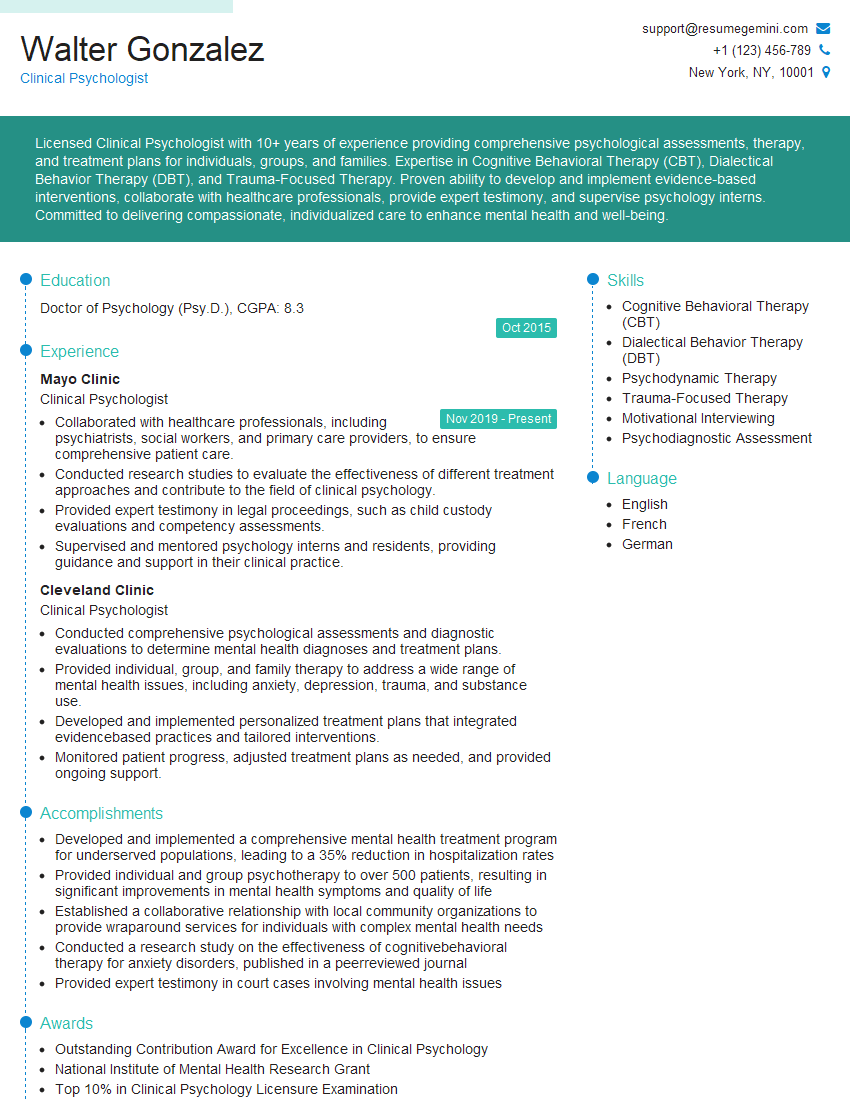
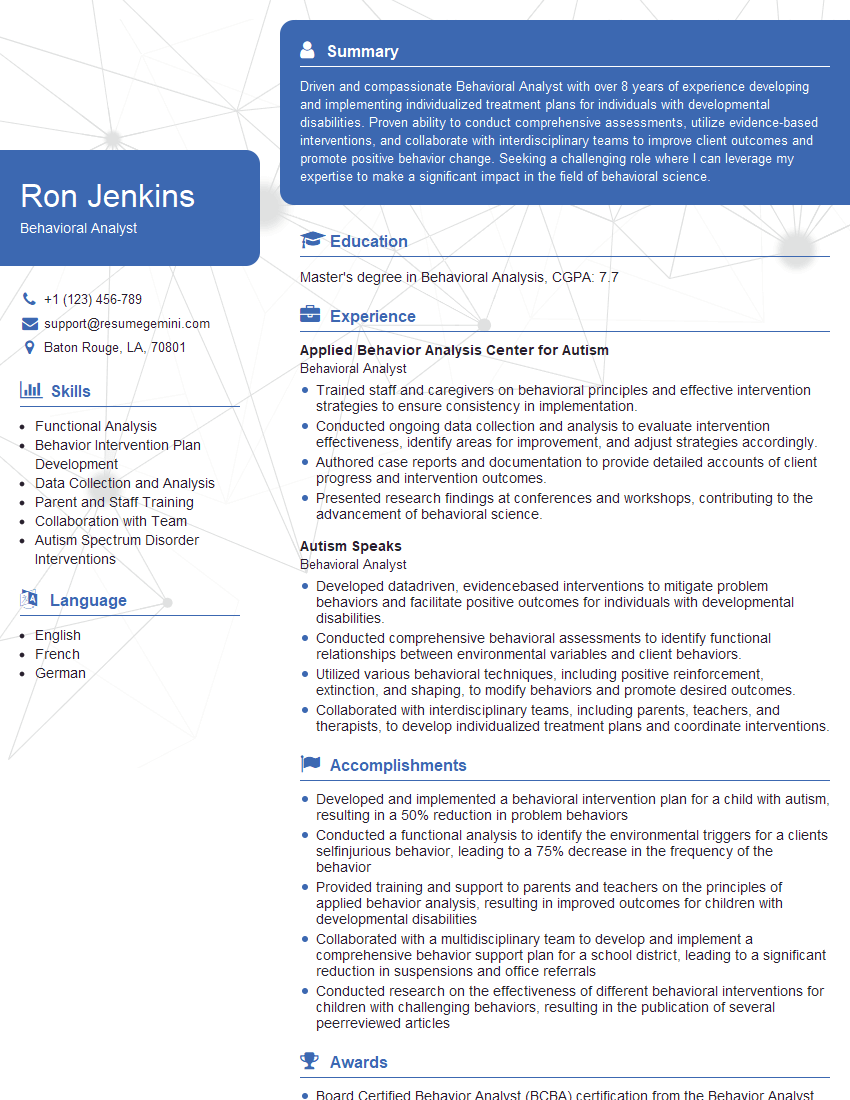
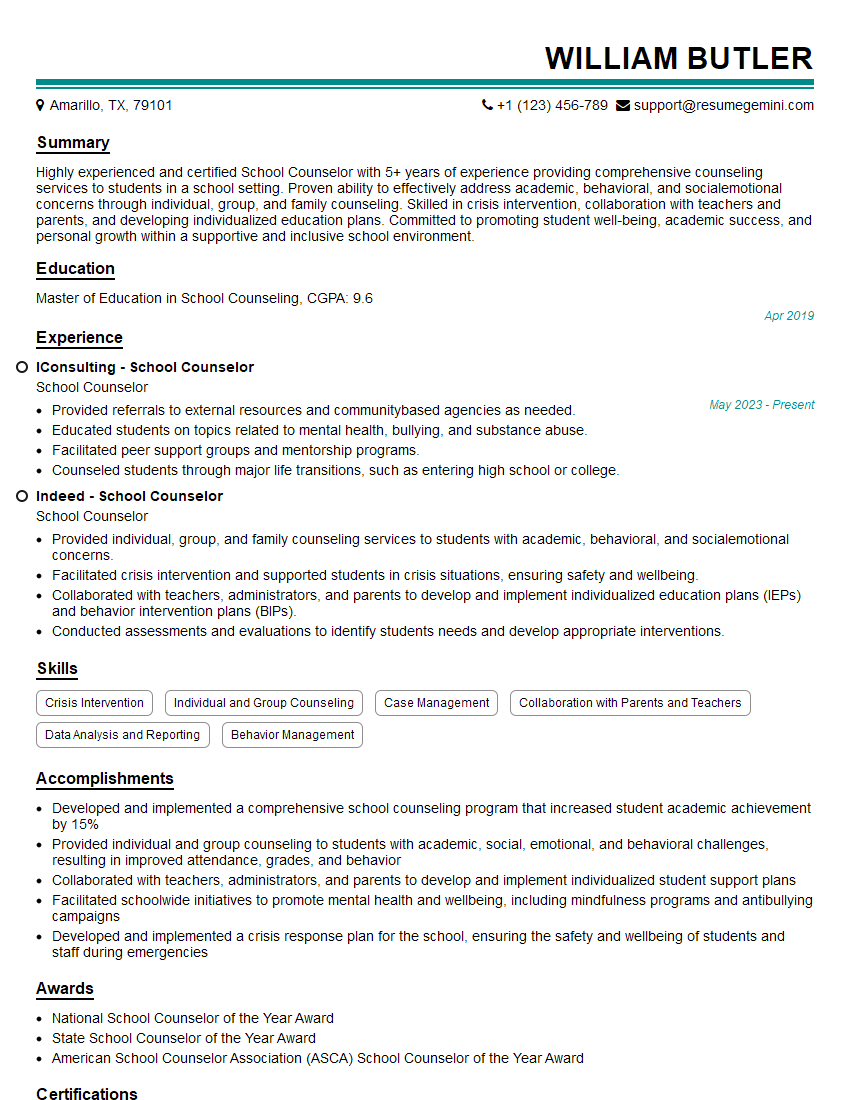
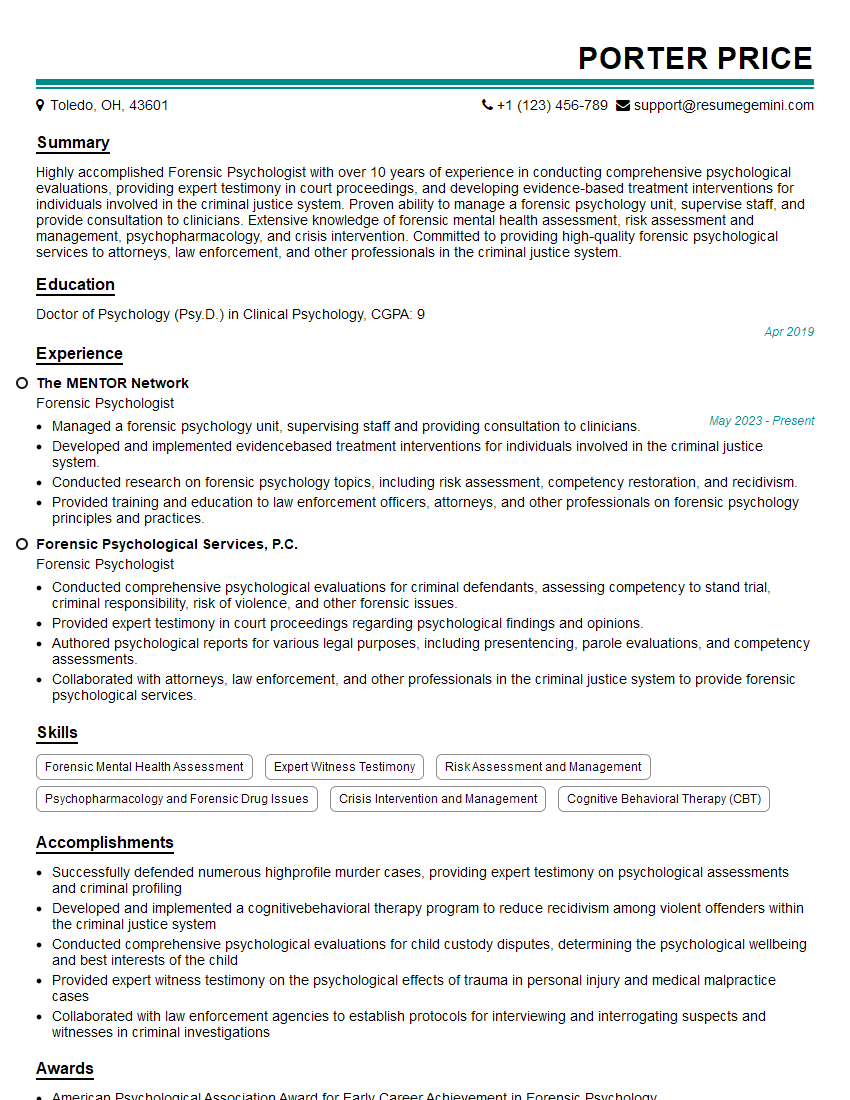
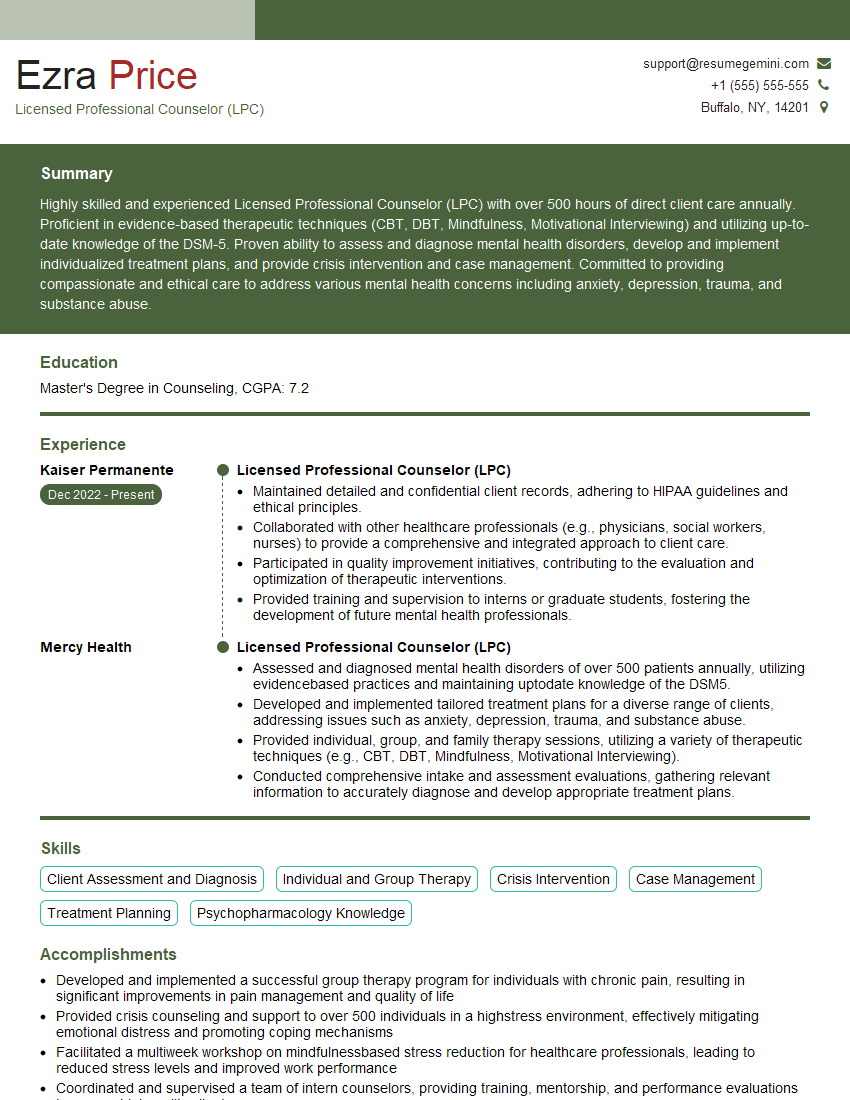
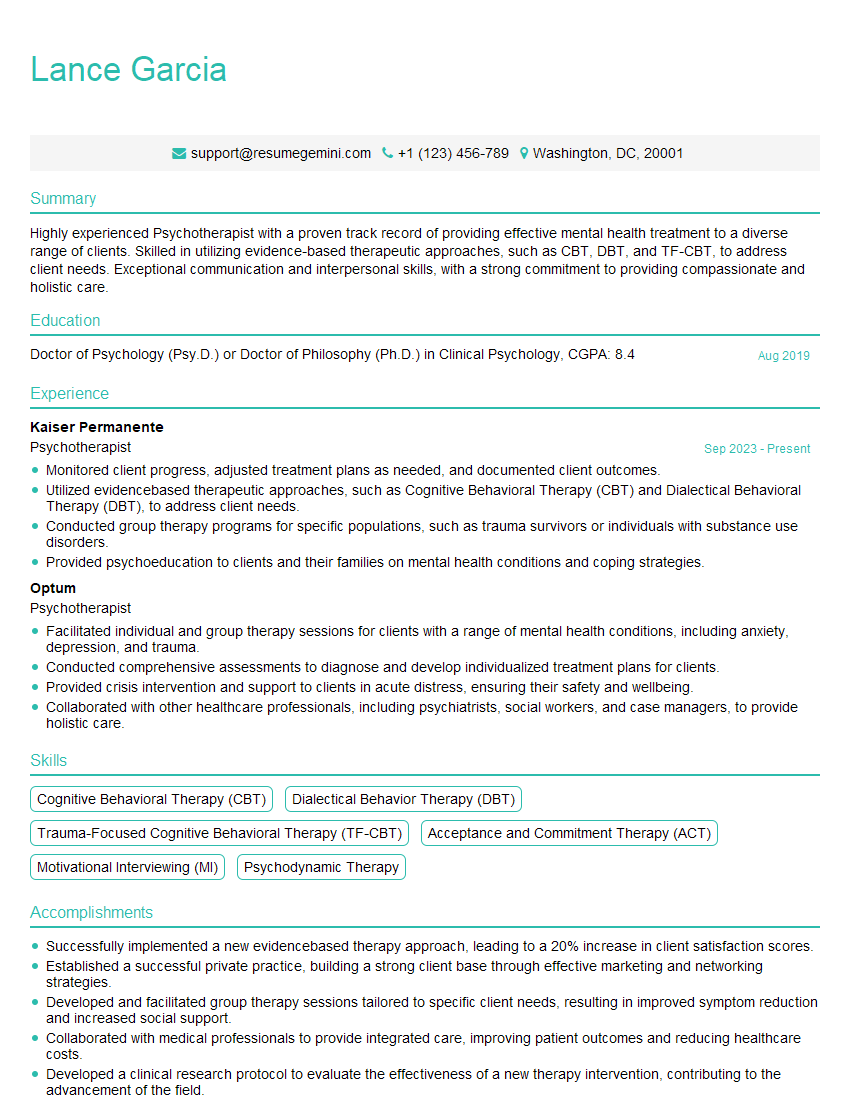
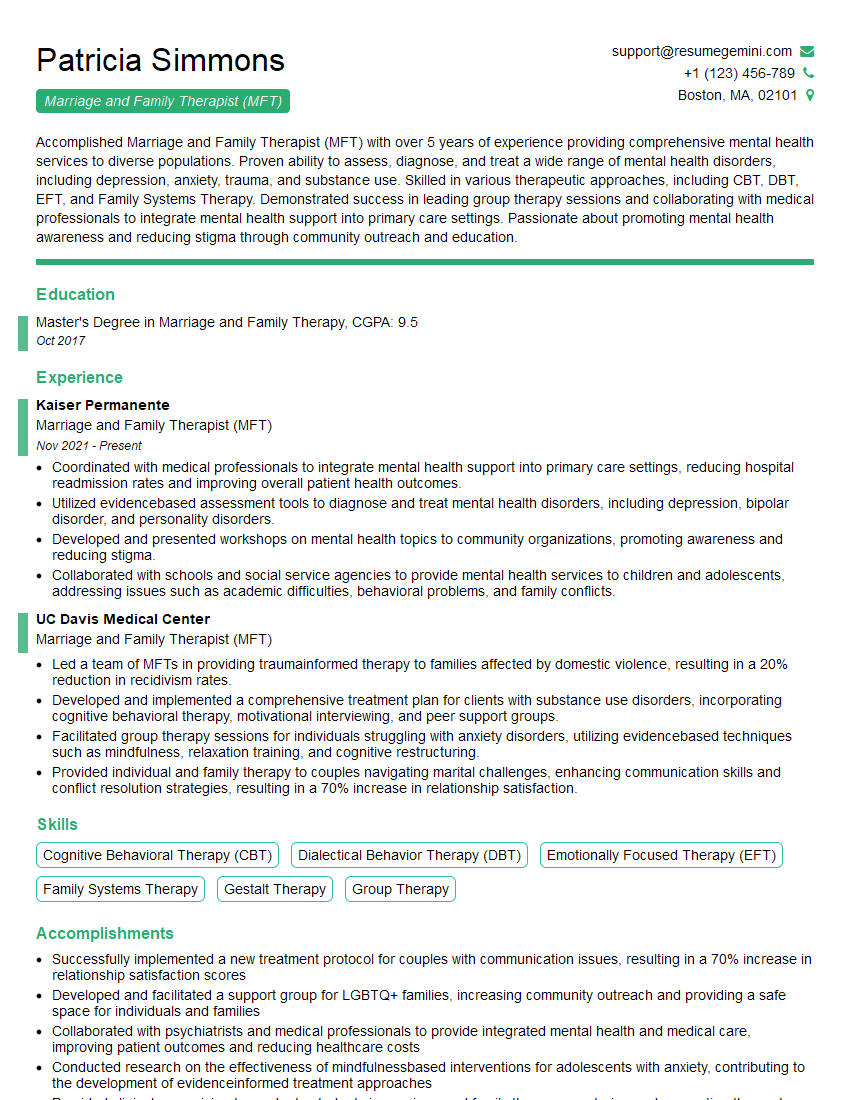
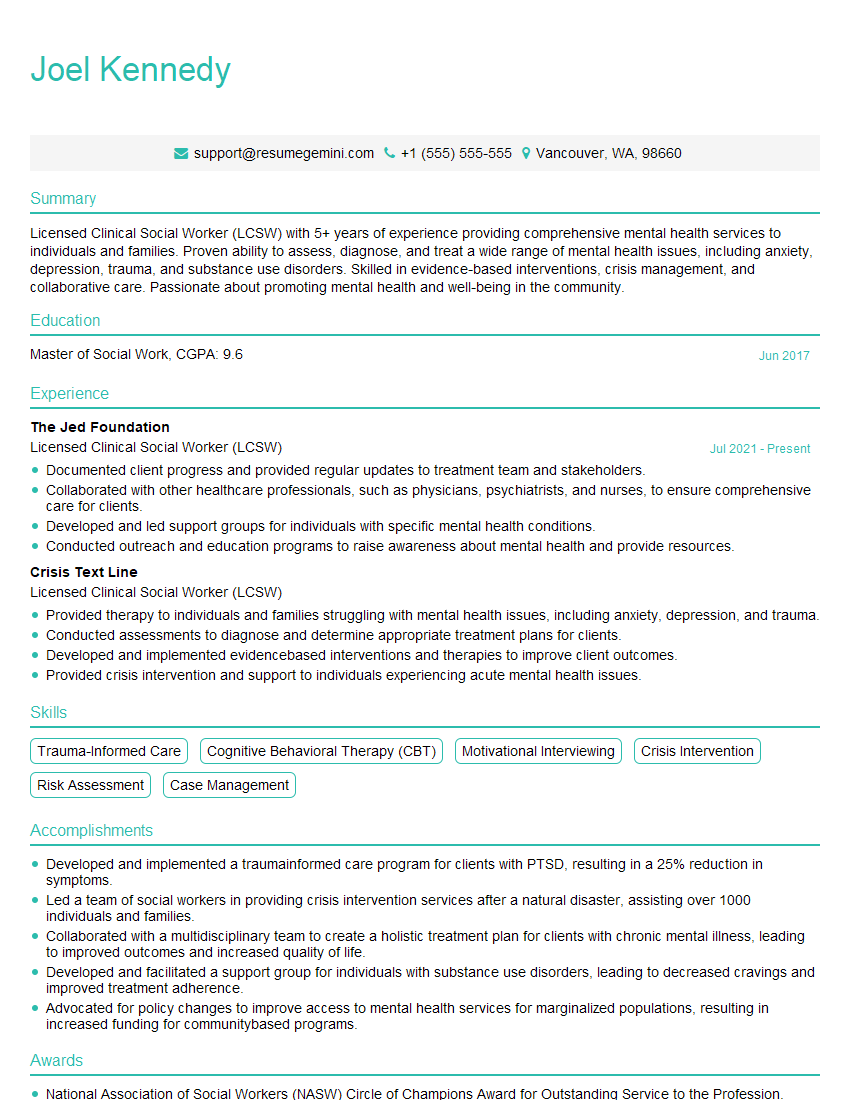
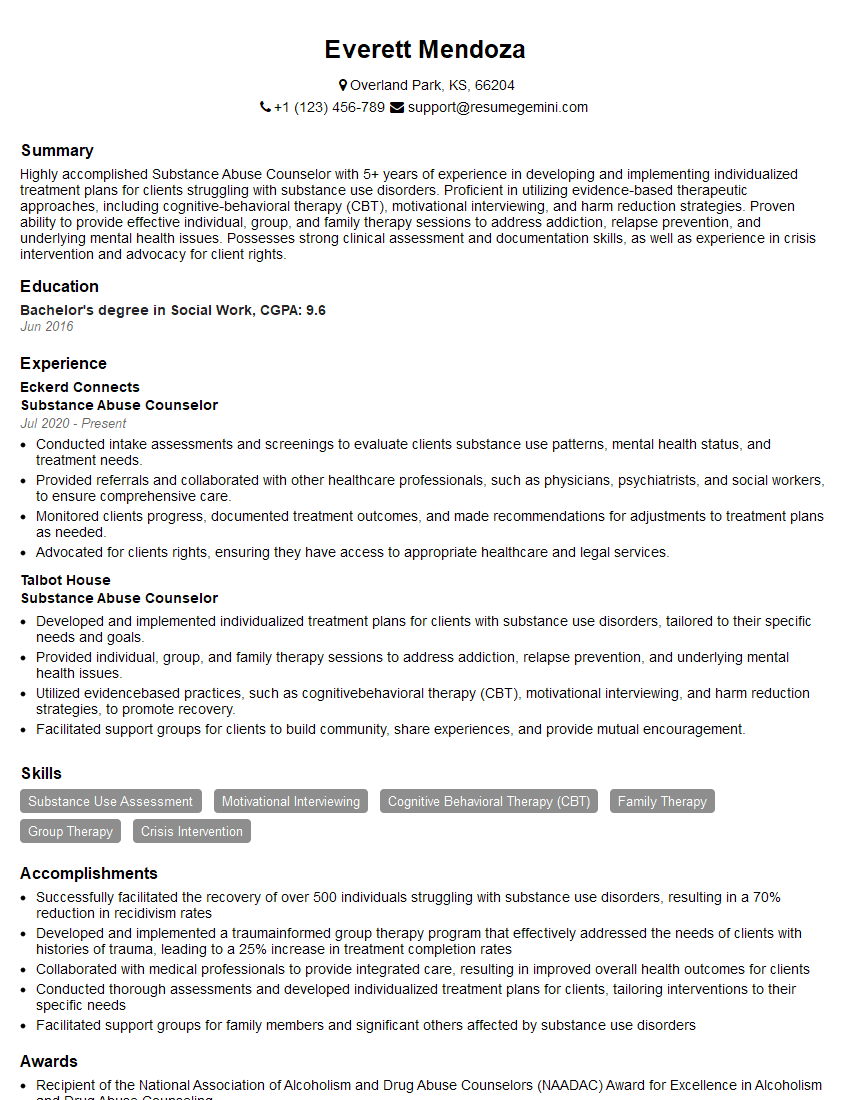
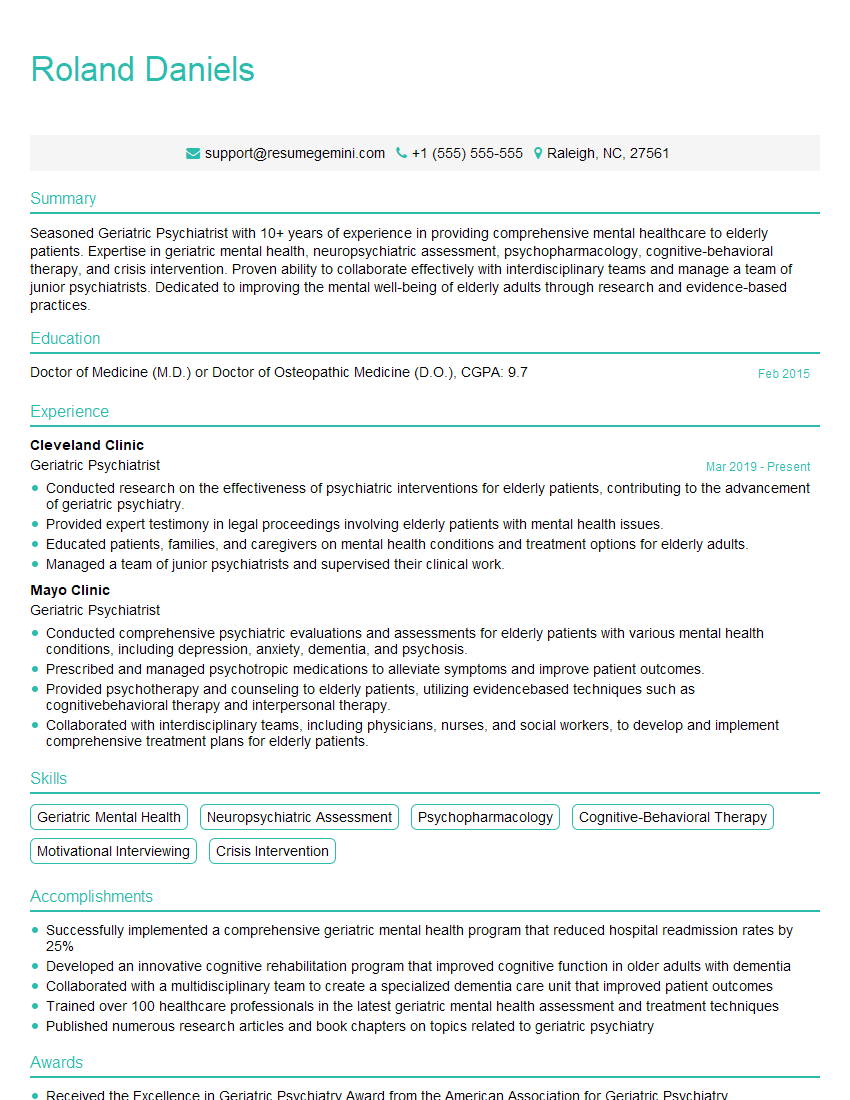
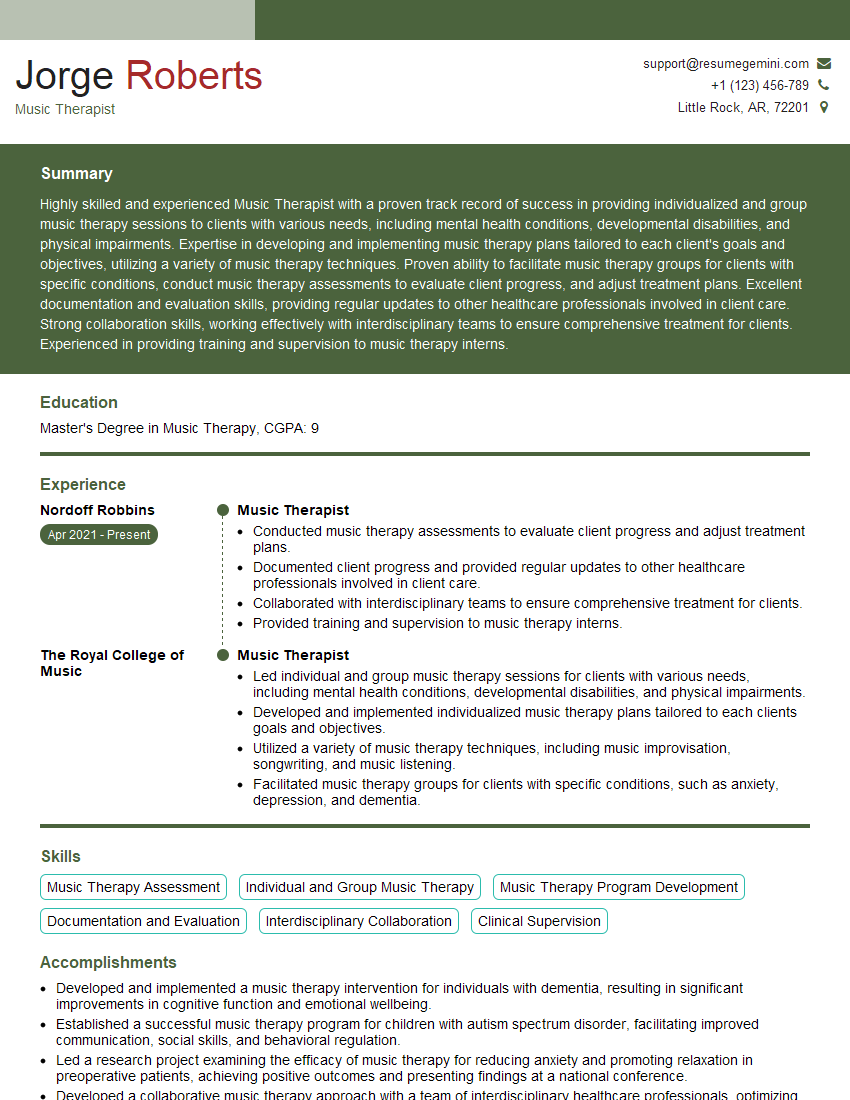
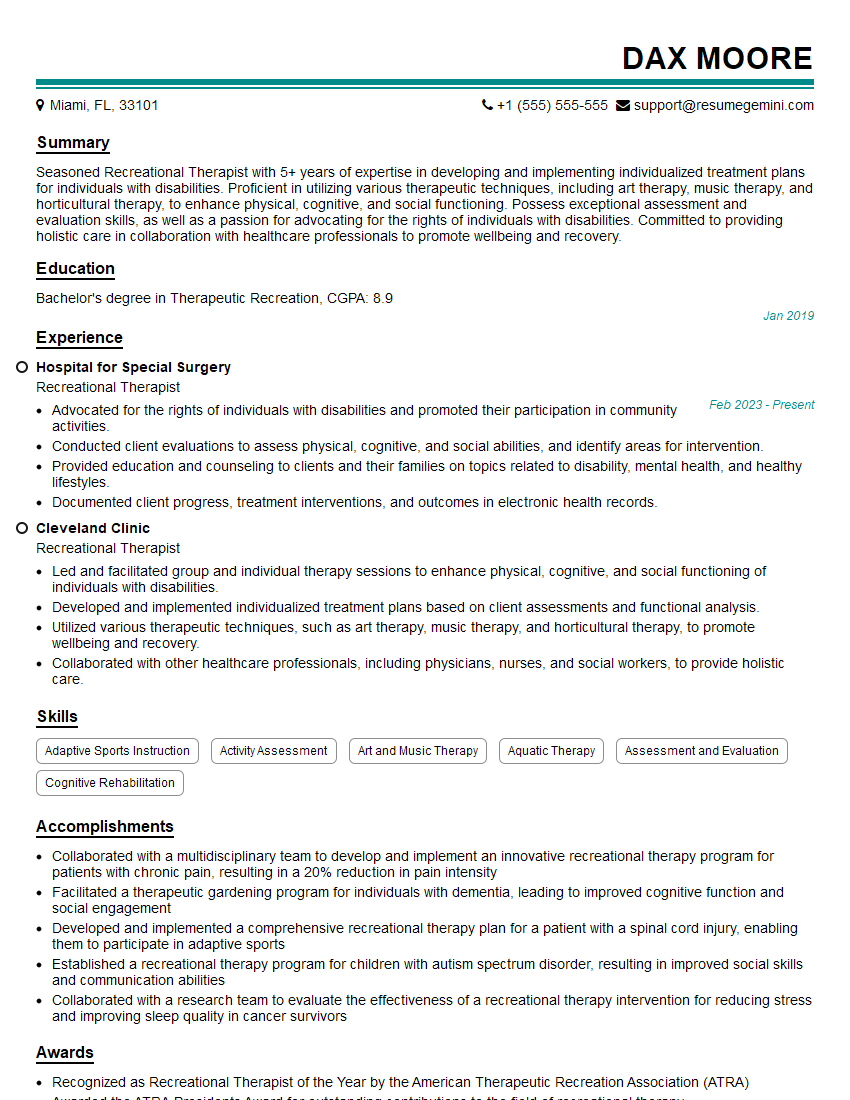
Mastering these key areas of Behavioural Health will significantly enhance your career prospects and open doors to fulfilling and impactful roles. A strong resume is crucial in showcasing your skills and experience to potential employers. Creating an ATS-friendly resume is vital to ensuring your application gets noticed. To help you build a compelling and effective resume, we recommend using ResumeGemini. ResumeGemini offers a user-friendly platform and provides examples of resumes tailored specifically to the Behavioural Health field. Invest the time to craft a professional resume that accurately reflects your qualifications and aspirations – it’s a vital step in securing your dream job.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO