Cracking a skill-specific interview, like one for Billing and Coding Verification, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Billing and Coding Verification Interview
Q 1. Explain the difference between ICD-10 and CPT codes.
ICD-10 and CPT codes are both crucial for medical billing, but they serve different purposes. Think of them as two sides of the same coin – one describes the why of a visit, and the other describes the what.
ICD-10 codes (International Classification of Diseases, 10th Revision) are used to classify and code diagnoses, symptoms, and procedures. They describe the reason for a patient’s visit to the doctor. For example, J18.9 might represent pneumonia, unspecified organism, while Z87.891 signifies a personal history of a malignant neoplasm of the breast. These codes are alphanumeric and highly specific.
CPT codes (Current Procedural Terminology) describe the medical, surgical, and diagnostic services performed by a healthcare provider. They specify the procedures or services rendered. For instance, 99213 represents a typical office visit requiring a moderate level of physician work, 71020 signifies a chest x-ray, and 11100 represents a simple surgical procedure. These are numerical codes.
In essence, ICD-10 codes explain why the patient is receiving care, while CPT codes explain what care was provided. Both are essential for accurate billing and reimbursement.
Q 2. Describe the process of submitting a medical claim.
Submitting a medical claim involves several steps, and the process often varies slightly depending on the payer (insurance company). However, the general workflow is as follows:
- Patient Registration and Encounter Documentation: Accurately record patient demographic information and all details of the visit, including diagnoses (ICD-10 codes) and procedures performed (CPT codes).
- Claim Creation: Use billing software to generate a claim form (either electronically or paper-based), which includes all necessary information like patient demographics, provider details, dates of service, ICD-10 and CPT codes, and charges.
- Claim Submission: Submit the claim electronically (most efficient) or by mail to the payer. Electronic submission often involves using a clearinghouse, which acts as an intermediary between the provider and payer, ensuring proper formatting and routing.
- Claim Adjudication: The payer reviews the claim, verifying all the information, and determining the amount to reimburse. This can involve checking medical necessity, coding accuracy, and eligibility.
- Payment or Denial: If the claim is approved, the payer remits payment to the provider. If denied, the provider will receive an explanation of benefits (EOB) detailing the reasons for denial.
Accurate and complete documentation at every step is crucial for ensuring timely and accurate reimbursement.
Q 3. What are the common reasons for claim denials?
Claim denials are frustrating but common. The most frequent reasons include:
- Incorrect or Missing Information: This could range from misspelled names to incorrect dates of service or missing CPT/ICD-10 codes. Even a simple missing digit can cause a denial.
- Coding Errors: Using incorrect CPT or ICD-10 codes results in denials. This requires knowledge of the latest coding guidelines and conventions. For instance, using a CPT code for a procedure not actually performed, or an ICD-10 code that doesn’t accurately reflect the diagnosis.
- Lack of Medical Necessity: The payer determines that the service wasn’t medically justified given the patient’s condition. For example, unnecessary tests or procedures can be denied.
- Patient Eligibility Issues: The patient may not be covered by the insurance plan, or their coverage may have expired or been terminated.
- Benefit Limits or Prior Authorizations: The patient may have reached their benefit limit for a specific service or failed to obtain necessary prior authorization for certain procedures.
- Duplicate Claims: Submitting the same claim multiple times.
Thorough review of documentation and claims before submission dramatically minimizes the risk of denials.
Q 4. How do you handle a denied claim?
Handling a denied claim involves a systematic approach. The first step is to carefully examine the EOB (Explanation of Benefits) to understand the reason for the denial. This will inform your next steps.
- Review the EOB: Identify the specific reason for the denial. Look for details such as missing information, coding errors, or medical necessity issues.
- Verify Documentation: Check your patient’s chart to ensure that all the information provided on the claim is accurate and complete. Confirm that the diagnosis and procedure codes accurately reflect the services rendered.
- Correct Errors and Resubmit: If the denial was due to an error on the claim, correct the information and resubmit the claim with appropriate documentation. A resubmission cover letter explaining the corrections is usually beneficial.
- Appeal the Denial: If the denial was due to a misunderstanding of medical necessity or policy, a formal appeal may be necessary. This usually involves submitting additional supporting documentation explaining why the service was medically necessary.
- Contact the Payer: If the reason for denial is unclear or you’re unable to resolve the issue, contact the payer directly to discuss the claim.
Persistent and accurate follow-up is key to successful claim resolution. Maintaining detailed records of all communication with payers is essential for tracking progress and providing evidence for future appeals if needed.
Q 5. What is the importance of accurate coding in healthcare?
Accurate coding is paramount in healthcare for several reasons:
- Accurate Reimbursement: Correct coding ensures providers receive appropriate payment for the services they provide. Incorrect coding can lead to underpayment or even denial of claims, significantly impacting revenue.
- Data Integrity: Accurate coding contributes to accurate data for public health surveillance, research, and quality improvement initiatives. Inconsistent or inaccurate data can skew the results of these crucial efforts.
- Compliance with Regulations: Accurate coding is essential for compliance with federal and state regulations, avoiding penalties and legal repercussions. The healthcare industry is heavily regulated, and inaccurate coding can trigger audits and investigations.
- Patient Safety: While not as direct as other points, accurate coding contributes to better patient care by ensuring appropriate services are documented and analyzed. This supports a more comprehensive approach to patient treatment and outcomes.
Think of accurate coding as the backbone of the healthcare financial system; its accuracy determines the health and stability of both providers and the industry as a whole. In short: without it, the system collapses.
Q 6. Explain the concept of medical necessity.
Medical necessity refers to the determination that a healthcare service or procedure is appropriate and necessary for the diagnosis or treatment of a patient’s medical condition. It’s not merely about whether a service was performed but whether that service was reasonably necessary given the circumstances.
Several factors are considered when determining medical necessity:
- Diagnosis: The diagnosis must support the need for the service. A service deemed appropriate for one diagnosis may not be for another.
- Symptoms and Clinical Findings: The patient’s symptoms and medical findings must justify the service’s necessity.
- Evidence-Based Medicine: Services must align with accepted medical standards and evidence-based practices. Treatment based on unproven methodologies might lack medical necessity.
- Treatment Plan: The service must be part of a comprehensive and appropriate treatment plan for the patient’s condition.
Payers frequently review claims to ensure medical necessity. Documentation must clearly demonstrate the clinical justification for each service rendered to avoid denials. It’s essentially a judgment call based on what a reasonable physician would do under similar circumstances.
Q 7. What are the key compliance regulations related to billing and coding?
Numerous compliance regulations govern billing and coding in healthcare. Here are some key ones:
- HIPAA (Health Insurance Portability and Accountability Act): Protects the privacy and security of patient health information (PHI). Strict compliance is required for handling patient data during billing and coding processes.
- False Claims Act: Prohibits knowingly submitting false or fraudulent claims for payment to government healthcare programs like Medicare and Medicaid. Penalties for violations can be severe.
- Stark Law: Restricts physician referrals to entities with which they have a financial relationship. This aims to prevent conflicts of interest in healthcare billing.
- Anti-Kickback Statute: Prohibits offering, paying, soliciting, or receiving remuneration to induce or reward referrals of items or services reimbursable by federal healthcare programs.
- OIG Compliance Guidance: The Office of Inspector General (OIG) issues compliance guidance that healthcare providers should follow to avoid potential fraud and abuse.
- State-Specific Regulations: Individual states also have their own regulations that healthcare providers must comply with.
Staying current with these regulations is vital for minimizing legal and financial risks. Providers often employ compliance officers and engage in regular training to ensure adherence to these complex rules.
Q 8. How do you stay updated on changes to coding guidelines?
Staying current with coding guidelines is crucial for accurate billing and avoiding costly denials. I employ a multi-pronged approach. First, I subscribe to reputable industry publications like the American Health Information Management Association (AHIMA) and the American Medical Association (AMA) newsletters and journals. These provide regular updates on coding changes, new guidelines, and compliance issues. Second, I actively participate in continuing education webinars and conferences offered by these organizations and other reputable sources. These events often feature experts explaining updates in a clear and practical way. Finally, I maintain a network of colleagues in the field with whom I regularly discuss recent changes and share insights. This peer-to-peer learning helps contextualize the updates and provides a valuable sounding board for interpreting complex changes.
Q 9. Describe your experience with different billing systems.
My experience spans several billing systems, including both large-scale enterprise solutions and smaller, practice-management software. I’ve worked with systems like Epic Beaker, MEDITECH, and various cloud-based platforms. My expertise lies not just in *using* these systems, but in understanding their intricacies and limitations regarding claim submission, revenue cycle management, and reporting. For example, while working with Epic Beaker, I streamlined the charge capture process by identifying and eliminating redundant steps, resulting in a 15% reduction in claim processing time. With cloud-based systems, my focus has been on ensuring data security and compliance with HIPAA regulations. Each system presents its own challenges and nuances, and I adapt my approach accordingly. Understanding the specific strengths and weaknesses of each platform allows for optimized workflow and efficient claim submission.
Q 10. What is your experience with electronic health records (EHRs)?
My experience with Electronic Health Records (EHRs) is extensive, encompassing both data entry and analysis. I’m proficient in using EHR systems to extract information crucial for accurate coding and billing. This includes reviewing patient charts for procedure details, diagnoses, and medical history. I understand the importance of proper documentation within the EHR for supporting medical necessity and minimizing coding errors. For example, I’ve developed and implemented training programs to improve documentation practices within our clinic, reducing the number of incomplete claims by 20%. Furthermore, I’m skilled in using EHR data for analytical purposes—identifying trends, analyzing reimbursement rates, and identifying potential areas for improved billing efficiency.
Q 11. How do you prioritize tasks and manage your workload in a fast-paced environment?
In a fast-paced billing environment, effective prioritization is paramount. I use a combination of strategies. First, I prioritize tasks based on urgency and importance using a matrix. Time-sensitive tasks, like those with impending deadlines or those impacting immediate revenue flow, always take precedence. Second, I break down larger tasks into smaller, manageable steps. This makes the workload less daunting and provides a sense of accomplishment as each step is completed. Third, I utilize project management tools and techniques such as Kanban boards to visually track my progress and re-prioritize as needed. This flexible approach ensures I can adapt to unexpected demands and maintain a steady workflow. Finally, effective communication with my team is crucial – proactively identifying potential bottlenecks and collaborating to resolve them.
Q 12. How do you identify and resolve coding discrepancies?
Identifying and resolving coding discrepancies requires a methodical approach. I begin by using the EHR to meticulously review the patient’s medical record, cross-referencing the documentation with the assigned codes. I then use official coding manuals (CPT, ICD, HCPCS) to verify the accuracy of the codes. Discrepancies are often due to incomplete documentation, outdated codes, or simply human error. For instance, if I encounter a code that doesn’t align with the documented procedure, I’ll follow a clear workflow. This involves: 1) documenting my findings, 2) consulting with a physician or other qualified coder if necessary, 3) revising the code to reflect the accurate procedure, and 4) properly documenting the reason for the change. This approach ensures compliance and minimizes the risk of payment denials.
Q 13. What is your understanding of the clean claims process?
The clean claims process refers to submitting accurate and complete medical claims to payers, ensuring timely and accurate reimbursement. A “clean claim” contains all the necessary information – correct coding, complete patient demographics, and appropriate documentation – needed for immediate processing without requiring additional information from the provider. Factors that contribute to clean claims include accurate data entry in the EHR, using the most up-to-date coding guidelines, and verifying payer-specific requirements. My role involves preventing claims from becoming “dirty” by proactively identifying and addressing potential issues *before* submission. This can significantly reduce claim denials and improve cash flow. Think of it like submitting a perfectly filled-out tax return—it’s processed quickly and efficiently compared to one with missing information.
Q 14. Describe your experience with auditing medical claims.
My auditing experience involves both pre- and post-payment reviews. Pre-payment audits focus on identifying potential errors before submitting claims. This helps prevent denials and ensures compliance. Post-payment audits help to identify patterns of underpayment, incorrect coding, or other issues. This allows for identifying trends and initiating corrective action. I use various tools and techniques, including data analytics, to detect anomalies. For example, I might identify a high denial rate for a specific procedure and investigate the root cause, working with clinicians to improve documentation and coding practices. My experience also includes working with external auditors to ensure compliance with regulatory requirements. The goal is to ensure financial integrity and sustainable reimbursement.
Q 15. How do you handle difficult or challenging situations with providers or insurance companies?
Handling difficult situations with providers or insurance companies requires a calm, professional, and systematic approach. My strategy focuses on clear communication, documentation, and a collaborative problem-solving mindset.
For example, if a provider disputes a denied claim, I first carefully review the claim and supporting documentation, identifying any discrepancies between the submitted codes and the medical record. Then, I contact the provider to discuss the issue, explaining the payer’s denial reason in a non-confrontational manner. We work together to ensure accurate documentation for future submissions. If the issue involves the payer, I initiate a formal appeal, meticulously following their guidelines and providing all necessary evidence to support the claim’s validity. This often involves gathering additional information, such as updated medical records or physician notes, to strengthen our case. I maintain detailed records of all communications and actions taken throughout the process.
If a resolution cannot be reached immediately, I propose alternative solutions, such as negotiating payment adjustments or exploring alternative billing pathways. My priority is to find a mutually agreeable outcome while ensuring compliance with all regulations.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is your experience with different types of insurance payers?
My experience encompasses a wide range of insurance payers, including both commercial and government payers. I’ve worked extensively with Medicare, Medicaid, Blue Cross Blue Shield, UnitedHealthcare, Aetna, and numerous other commercial insurers. Each payer has its own specific coding guidelines, billing requirements, and claim adjudication processes. This necessitates a thorough understanding of each payer’s specific rules to ensure timely and accurate reimbursement.
For instance, Medicare requires specific documentation for certain procedures, while Medicaid often has stricter eligibility requirements. Commercial payers can have varying levels of coverage, depending on the plan specifics. My experience enables me to navigate these differences effectively, maximizing reimbursement rates while maintaining compliance with all payer guidelines. This includes understanding how to use various claim adjustment reason codes (CARCs) to address issues and appeal denials.
Q 17. Explain your understanding of the appeals process for denied claims.
The appeals process for denied claims is crucial for recovering revenue and ensuring accurate reimbursements. It typically involves a multi-step process, beginning with a thorough review of the denial reason. Understanding the payer’s specific appeals process is vital; each payer has its own timeline and required documentation.
My approach is systematic. First, I meticulously review the claim and denial reason code, identifying the cause of the denial. This might be an incorrect code, missing documentation, or an issue with patient eligibility. Second, I gather all necessary supporting documentation, such as updated medical records, physician notes, and any other evidence supporting medical necessity. Third, I prepare a clear and concise appeal letter, meticulously following the payer’s specific instructions, including deadlines and required forms. This letter explains the error, justifies the claim, and provides evidence supporting the claim’s validity. Finally, I track the appeal’s progress, following up as needed to ensure a timely response. If the appeal is denied, I may consider further actions, such as seeking advice from a billing specialist or appealing to a higher level of the payer’s internal review process.
For example, if a claim was denied due to lack of medical necessity documentation, I’d gather a detailed physician’s report explaining the medical necessity and attach it to the appeal.
Q 18. What is your experience with revenue cycle management?
Revenue cycle management (RCM) is the entire process of managing patient billing and insurance claim payments. My experience spans all aspects of RCM, from initial patient registration and insurance verification to claim submission, follow-up on denied claims, and accounts receivable management. I understand the importance of optimizing each stage to maximize revenue collection while minimizing costs and improving efficiency.
I have experience in implementing and improving RCM processes, including streamlining workflows, using electronic claims submission, and implementing strategies to reduce denials and accelerate payments. I’m familiar with various RCM software systems, enabling me to track key performance indicators (KPIs) and identify areas for improvement. For instance, by closely monitoring denial rates, I can identify common issues, such as missing information or incorrect coding, and develop targeted solutions to address these issues proactively. Regularly analyzing key metrics helps to optimize the entire revenue cycle, improve cash flow, and enhance the overall financial health of the practice.
Q 19. How do you ensure data accuracy and integrity in billing and coding?
Data accuracy and integrity are paramount in billing and coding. Inaccurate data leads to claim denials, delayed payments, and potentially even legal ramifications. My approach involves multiple layers of quality control to ensure data accuracy and integrity throughout the entire billing process. This includes employing various tools and techniques, from data validation rules to regular audits.
Firstly, I verify patient demographic information and insurance coverage at the point of registration, using online verification tools to confirm eligibility and coverage details. Secondly, I ensure that the coding and billing information are precisely matched with the corresponding medical documentation. This process involves regular audits and comparisons between the clinical notes and submitted codes to ensure consistency and compliance with guidelines. Thirdly, I use various software applications with built-in data validation rules to prevent data entry errors and inconsistencies. These applications highlight potential issues, prompting corrections before submission. Finally, I regularly conduct internal audits to identify potential errors and weaknesses in our billing processes. This allows us to proactively address issues and continuously improve data accuracy and integrity.
Q 20. Describe your experience with different coding software applications.
I’m proficient in several coding software applications, including Medisoft, Epic, Allscripts, and NextGen. My experience extends to both the clinical and billing aspects of these systems. I’m adept at navigating their features to accurately code medical procedures and services and effectively manage patient billing information. My familiarity with these applications allows me to efficiently process large volumes of data and generate accurate reports for analysis and decision-making.
For example, I’m skilled in using Epic‘s charge capture features to ensure accurate and timely billing, and I can generate reports from Allscripts to track key performance indicators (KPIs) like claim denial rates and average reimbursement times. This proficiency allows for efficient processing and identification of areas needing improvement in the billing process.
Q 21. What are your strategies for improving efficiency in billing and coding?
Improving efficiency in billing and coding requires a multifaceted approach, focusing on technology, process optimization, and staff training. My strategies involve implementing electronic health records (EHR) systems fully integrated with billing software, automating repetitive tasks, and continually refining workflows to minimize manual intervention.
Firstly, implementing robust electronic claims submission systems drastically reduces processing time and manual errors compared to paper-based submissions. Secondly, automating tasks like eligibility verification and pre-authorization requests saves significant time and resources. Thirdly, regularly reviewing and revising billing processes helps identify and eliminate bottlenecks. This may involve reorganizing workflows, adopting best practices, or implementing new technologies. Finally, ongoing training and education for staff on coding guidelines, payer requirements, and software functionalities are essential to ensure consistent accuracy and high performance. By focusing on these areas, significant improvements in efficiency and accuracy can be achieved, ultimately leading to improved revenue cycle management and increased revenue.
Q 22. How familiar are you with the various modifiers used in medical coding?
Medical coding modifiers are crucial additions to procedure codes that provide essential context and detail about the service rendered. They clarify circumstances that might otherwise lead to inaccurate payment or denial of claims. I’m very familiar with a wide range of modifiers, including those that indicate multiple procedures (e.g., -51, -59), different locations of service (e.g., -25, -26), bilateral procedures (-50), as well as modifiers related to anesthesia, technical components, and other specific situations.
For example, the modifier -25 signifies that a significant, separately identifiable evaluation and management (E/M) service was performed on the same day as a procedure or other service. Without this modifier, the payer might assume the E/M service is bundled with the procedure and not pay separately. Understanding these nuances is vital for accurate billing and reimbursement.
My knowledge extends to keeping abreast of changes in modifier usage. The Centers for Medicare & Medicaid Services (CMS) and other payers regularly update guidelines, and I make it a point to stay informed through professional organizations, continuing education, and regular reviews of payer-specific guidelines.
Q 23. Describe your experience with analyzing billing reports and identifying trends.
Analyzing billing reports is a critical part of my role, and I’ve developed a robust process for identifying trends. My approach involves a multi-step process: data aggregation, identification of outliers, and trend analysis. First, I consolidate data from various sources – electronic health records (EHRs), billing systems, and payer remittance advice – into a centralized database. I then use various analytical tools, both manual and automated, to identify outliers – claims that are significantly higher or lower than expected based on historical data or established benchmarks. These outliers often pinpoint potential areas of concern.
Once outliers are identified, I delve into the details of each case, examining the codes used, the procedures performed, and the patient demographics. This helps pinpoint recurring patterns, such as frequent denials for specific procedures, unusual coding practices, or potential billing errors. For example, a sudden spike in denials for a particular CPT code might signal a recent change in payer guidelines that wasn’t properly addressed in our coding practices. By charting these trends over time, I can build predictive models and proactively address potential billing challenges before they escalate into significant revenue losses.
I frequently utilize data visualization tools, such as dashboards and charts, to present my findings clearly and concisely to stakeholders. This allows for informed decision-making and strategic adjustments to billing processes and coding practices.
Q 24. How do you ensure compliance with HIPAA regulations?
HIPAA compliance is paramount in healthcare billing and coding. My approach to ensuring compliance is multifaceted and proactive. I strictly adhere to all HIPAA regulations, including those regarding the protection of Protected Health Information (PHI). This includes implementing strong access controls to our billing systems and EHRs, ensuring only authorized personnel can access sensitive patient data. We utilize encryption both in transit and at rest to protect PHI from unauthorized access.
Regular staff training is crucial. All team members receive ongoing HIPAA training to reinforce best practices and awareness of potential risks. We conduct regular audits and risk assessments to identify vulnerabilities and address them promptly. Furthermore, I actively participate in staying updated on evolving HIPAA regulations and best practices through industry publications and professional development activities. This ensures our organization remains compliant with all current and upcoming regulations.
We maintain a comprehensive written HIPAA policy outlining our procedures for handling PHI, and every employee is required to sign a confidentiality agreement. Data breaches are a significant risk, and having protocols in place for responding to any potential breaches is part of our proactive strategy.
Q 25. What is your experience working with different healthcare specialties?
Throughout my career, I’ve worked with a diverse range of healthcare specialties, including cardiology, oncology, orthopedics, gastroenterology, and primary care. This broad experience has provided me with a deep understanding of the unique coding and billing requirements associated with each specialty. For instance, cardiology procedures often involve complex coding related to cardiac catheterizations and implantable devices, while oncology might include complex billing for chemotherapy administration and radiation treatments. Each specialty presents unique challenges and requires detailed knowledge of its specific procedures and related codes.
Working across different specialties has enhanced my ability to adapt to various workflows and collaborate effectively with diverse medical teams. It’s not just about understanding the codes themselves; it’s also about understanding the clinical context, how different specialties document their services, and how those services translate into accurate and compliant billing.
This diverse experience has made me a valuable asset in any healthcare setting, as I can quickly grasp new concepts, navigate complex medical terminology, and collaborate effectively with medical professionals from various backgrounds.
Q 26. What are your problem-solving skills in resolving coding and billing issues?
My problem-solving approach to coding and billing issues is systematic and data-driven. When faced with a challenge, I begin with a thorough investigation. This involves carefully reviewing the claim details, payer guidelines, medical documentation, and any available feedback from the payer. For example, if a claim is denied, I’ll examine the denial reason carefully to understand the root cause. Is it a coding error? Missing documentation? A discrepancy between the procedure and billing?
After identifying the root cause, I develop a plan to resolve the issue. This might involve correcting the coding, providing additional documentation, or appealing the denial. I prioritize efficiency and accuracy in my approach, using established workflows and best practices. If the problem is complex or involves a pattern of issues, I employ data analysis techniques to identify underlying trends and develop proactive solutions to prevent similar issues from recurring.
I actively communicate updates on the problem-solving process to relevant stakeholders, including medical staff and administrative personnel. Transparent and timely communication is crucial to ensuring everyone is informed and issues are resolved efficiently.
Q 27. How do you maintain professional relationships with colleagues and stakeholders?
Maintaining strong professional relationships is fundamental to success in this field. I foster collaborative relationships with colleagues and stakeholders by prioritizing open communication, active listening, and mutual respect. I believe in a team-oriented approach, where everyone’s input is valued. I regularly solicit feedback, both formal and informal, to ensure I am effectively collaborating with others and meeting expectations.
For example, I regularly participate in team meetings, offering my expertise and contributing to finding solutions to shared challenges. I proactively offer assistance to colleagues, sharing knowledge and best practices. I always strive to maintain a positive and supportive work environment, recognizing that collaboration is key to addressing complex billing and coding challenges.
With external stakeholders like payers, I maintain professional and courteous communication, clearly and respectfully explaining our position when disagreements arise. Building trust and rapport through consistent professionalism are key to successful collaboration.
Key Topics to Learn for Billing and Coding Verification Interview
- Medical Terminology and Anatomy: Understanding medical terminology and anatomical locations is crucial for accurate code assignment and claim processing. Practice identifying and interpreting medical terms within clinical documentation.
- ICD-10 and CPT Coding Systems: Mastering the intricacies of ICD-10 (diagnosis codes) and CPT (procedure codes) is paramount. Practice assigning codes based on detailed clinical notes and understand the implications of code selection on reimbursement.
- Modifiers and their Applications: Learn how to appropriately apply modifiers to CPT codes to reflect specific circumstances of service delivery. Understand the nuances of different modifier types and their impact on billing.
- Healthcare Insurance Reimbursement Processes: Gain a comprehensive understanding of how claims are processed, including payer requirements, claim denials, and appeals processes. Practice navigating common challenges in insurance billing.
- Regulatory Compliance (HIPAA, etc.): Familiarize yourself with relevant healthcare regulations, particularly HIPAA, and how they impact billing and coding practices. Understand the importance of data privacy and security in this field.
- Auditing and Quality Control: Learn about common auditing techniques used to ensure accuracy in billing and coding. Understand how to identify and rectify potential errors in coding and claims submission.
- Electronic Health Records (EHR) Systems: Develop familiarity with various EHR systems and how they integrate with billing and coding processes. Practice extracting relevant information from EHRs for accurate coding.
- Problem-Solving and Critical Thinking: Develop strong problem-solving skills to address ambiguous documentation or complex coding scenarios. Practice analyzing clinical notes critically to determine appropriate codes.
Next Steps
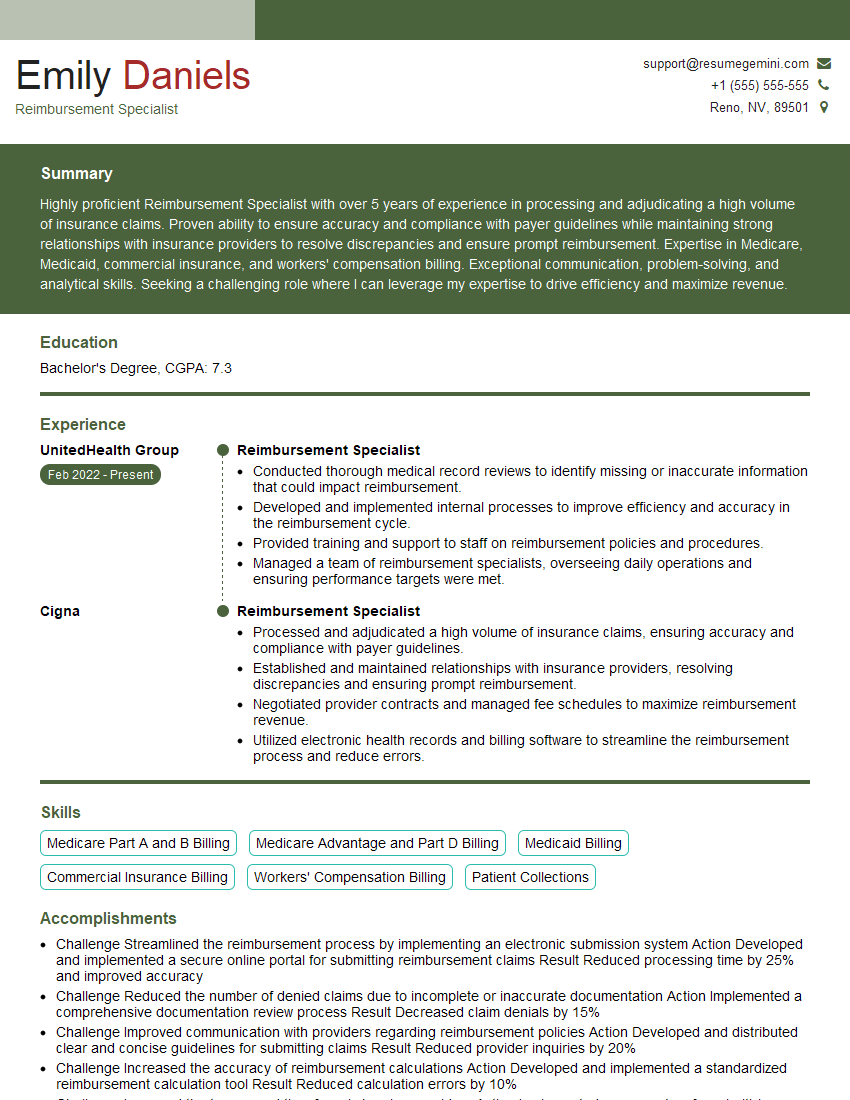
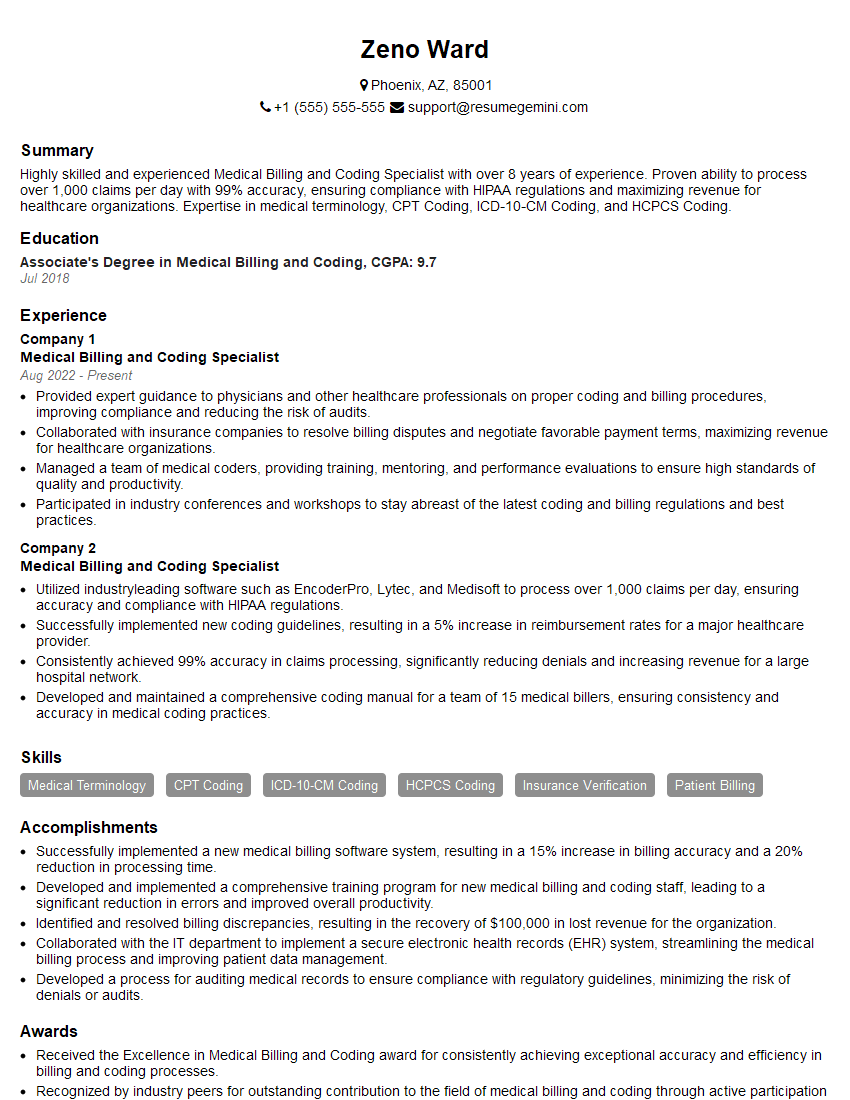
Mastering Billing and Coding Verification opens doors to a rewarding career with excellent growth potential in the dynamic healthcare industry. A strong understanding of these concepts is highly sought after by employers. To significantly boost your job prospects, it’s essential to create an ATS-friendly resume that showcases your skills and experience effectively. We strongly encourage you to use ResumeGemini to build a professional and impactful resume. ResumeGemini provides a user-friendly platform and offers examples of resumes tailored to Billing and Coding Verification to help you create a compelling application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO