Preparation is the key to success in any interview. In this post, we’ll explore crucial Child and Adolescent Counseling interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Child and Adolescent Counseling Interview
Q 1. Explain your approach to assessing the developmental stage of a child or adolescent client.
Assessing a child or adolescent’s developmental stage is crucial for tailoring effective interventions. My approach is multifaceted, combining standardized assessments with observational data and clinical judgment. I don’t rely on a single metric; instead, I integrate information from several sources to get a holistic picture.
- Standardized Assessments: I utilize age-appropriate tools like the Vineland Adaptive Behavior Scales or the Bayley Scales of Infant and Toddler Development (for younger children), and measures like the Child Behavior Checklist (CBCL) or the Adolescent Self-Report (ASR) for older clients. These provide quantitative data on developmental milestones across various domains (cognitive, social-emotional, adaptive functioning).
- Clinical Interview: A detailed interview with the child/adolescent and their parents/guardians is essential. I ask open-ended questions to understand their strengths, challenges, interests, and daily routines. This qualitative information provides context and depth to the quantitative data from assessments.
- Observation: Direct observation of the child/adolescent’s behavior during sessions is invaluable. This helps me assess their interaction style, emotional regulation, communication skills, and overall presentation, complementing information gathered through interviews and tests.
- Developmental History: A comprehensive developmental history from parents/guardians is crucial. Information on significant milestones, developmental delays, medical history, and family dynamics enriches the understanding of the client’s developmental trajectory.
For example, a teenager struggling with social anxiety might score high on anxiety scales, display avoidance behaviors during sessions, and report difficulty making friends in the interview. This combined information paints a clearer picture than any single assessment alone. This integrated approach allows me to accurately gauge their developmental stage and identify specific areas needing support.
Q 2. Describe your experience with evidence-based therapeutic interventions for anxiety disorders in children.
I have extensive experience using evidence-based interventions for childhood anxiety. My approach is often tailored to the specific anxiety disorder (e.g., generalized anxiety disorder, social anxiety disorder, separation anxiety disorder) and the child’s developmental level. Cognitive Behavioral Therapy (CBT) is a cornerstone of my practice.
- Cognitive Restructuring: This involves helping the child identify and challenge negative or catastrophic thoughts contributing to their anxiety. For example, a child fearing public speaking might think, “Everyone will laugh at me.” We’d explore the validity of this thought and develop more balanced perspectives.
- Exposure Therapy: This gradually exposes the child to feared situations or objects in a safe and controlled environment. This helps them learn that their feared outcomes are unlikely and build coping skills. For a child with a fear of dogs, this might involve starting with pictures of dogs, then videos, then observing dogs from a distance, gradually progressing closer.
- Relaxation Techniques: I teach children and adolescents various relaxation techniques, including deep breathing exercises, progressive muscle relaxation, and mindfulness practices, to manage anxiety symptoms in the moment.
- Parent Training: Involving parents is essential. I educate them about anxiety disorders and teach them how to support their child using consistent positive reinforcement and implementing strategies learned in therapy.
I also incorporate other evidence-based techniques such as Acceptance and Commitment Therapy (ACT) when appropriate, focusing on acceptance of difficult emotions and commitment to valued actions. The selection of techniques depends on the child’s age, the specific anxiety disorder, and their individual needs and preferences.
Q 3. How do you handle ethical dilemmas, such as confidentiality breaches, in child and adolescent counseling?
Ethical dilemmas are an unavoidable part of child and adolescent counseling. Confidentiality is paramount, but it’s not absolute. My approach to handling breaches or potential breaches adheres strictly to ethical guidelines and legal mandates.
- Duty to Warn/Protect: If a child discloses a serious threat of harm to themselves or others (e.g., suicidal ideation, plans to harm someone), I have a legal and ethical obligation to break confidentiality and take appropriate action. This might involve contacting the appropriate authorities (child protective services, law enforcement) or the child’s parents/guardians.
- Mandatory Reporting: In many jurisdictions, I am mandated to report suspected child abuse or neglect. This is a legal requirement, regardless of the child’s or family’s wishes.
- Informed Consent/Assent: I carefully explain the limits of confidentiality to both the child (age-appropriately) and their parents/guardians. I obtain informed consent from parents and assent from the child whenever possible, ensuring they understand the process and their rights.
- Supervision & Consultation: I regularly engage in supervision and consultation with experienced colleagues to discuss ethical dilemmas and ensure I’m making responsible and well-informed decisions.
Addressing ethical dilemmas requires careful consideration, thorough documentation, and a commitment to acting in the best interests of the child. Every situation is unique, and I approach each with a commitment to ethical decision-making.
Q 4. What are the key differences between treating children and adolescents?
Treating children and adolescents requires distinct approaches due to their differing developmental stages, cognitive abilities, and emotional maturity.
- Cognitive Development: Children have limited abstract thinking skills compared to adolescents. Therapeutic techniques need to be adapted accordingly. With younger children, play therapy might be more effective than verbal processing. Adolescents, with their enhanced abstract thinking, can engage in more complex cognitive-behavioral techniques.
- Emotional Regulation: Children’s emotional regulation skills are still developing. Therapists need patience and strategies for helping them manage intense emotions. Adolescents experience a wide range of emotions, sometimes struggling with identity formation and emotional volatility. The therapeutic approach must acknowledge these developmental realities.
- Communication Styles: Communication techniques must adapt to the child’s or adolescent’s developmental stage and communication preferences. Play, art, or other creative mediums can be useful with children. Adolescents often respond well to collaborative, peer-focused interventions.
- Parental Involvement: Parental involvement is usually crucial in working with children, while adolescent therapy often aims to increase autonomy and self-reliance, though parental collaboration is still vital in many cases. The therapist must navigate this balance carefully.
For example, a young child experiencing trauma might benefit from play therapy, where they can express their feelings through play, while an adolescent dealing with depression might engage in a collaborative discussion about their emotions and coping mechanisms.
Q 5. Describe your experience working with children from diverse cultural backgrounds.
Cultural competence is essential in my practice. I understand that cultural background significantly influences a child’s or adolescent’s behavior, beliefs, values, and family dynamics. My approach involves continuous learning and self-reflection.
- Cultural Humility: I recognize that I can’t fully understand another person’s culture; therefore, I approach each client with humility, seeking to learn about their unique experiences and perspectives.
- Cultural Awareness Training: I participate in ongoing professional development to expand my knowledge of diverse cultures and their impact on mental health.
- Culturally Adapted Interventions: I adapt my therapeutic techniques to be culturally sensitive and relevant. This might involve utilizing culturally appropriate assessment tools, adapting language, and understanding family structures and communication styles.
- Collaboration with Community Resources: I work closely with community resources and cultural leaders to ensure culturally appropriate services are provided.
For instance, working with a family from a collectivist culture, I would ensure that family members are actively involved in the therapeutic process, respecting their collective decision-making style. Understanding the cultural nuances is critical in building trust and achieving positive outcomes.
Q 6. How do you involve parents or guardians in the therapeutic process?
Parental or guardian involvement is crucial in most cases, particularly with younger children. However, the level of involvement needs to be tailored to the age and developmental stage of the child and the specific therapeutic goals. My approach emphasizes collaboration and shared responsibility.
- Collaborative Approach: I view parents/guardians as partners in the therapeutic process. I regularly communicate with them, providing updates on the child’s progress and collaboratively developing strategies for managing challenges at home.
- Psychoeducation: I provide psychoeducation to parents/guardians about the child’s diagnosis, treatment plan, and coping strategies. This empowers them to support their child effectively.
- Parent Training: I often incorporate parent training components into the treatment plan, teaching parents specific techniques to manage challenging behaviors or promote positive interactions.
- Age-Appropriate Involvement: With adolescents, I aim to empower them to take an active role in their treatment, while still maintaining open communication with parents/guardians, particularly regarding significant safety concerns.
The level of parental involvement is determined through open communication, respecting the adolescent’s privacy and autonomy while maintaining collaboration with parents to provide the most effective support.
Q 7. Explain your understanding of trauma-informed care and how you integrate it into your practice.
Trauma-informed care is a fundamental principle guiding my practice. It recognizes that many children and adolescents have experienced trauma and that this can significantly impact their mental health and behavior. My approach emphasizes safety, trustworthiness, choice, collaboration, and empowerment.
- Safety: Creating a safe and predictable therapeutic environment is paramount. This includes building rapport, establishing clear boundaries, and ensuring the child feels comfortable and secure.
- Trustworthiness and Transparency: I build trust by being consistent, reliable, and honest. I clearly explain procedures and provide choices whenever possible.
- Choice and Control: I empower children and adolescents by providing choices within the therapeutic process. This might involve selecting activities, setting goals, or determining the pace of treatment.
- Collaboration: I work collaboratively with the child, their parents/guardians, and other relevant professionals to develop a comprehensive treatment plan.
- Empowerment: I focus on building the child’s strengths and resilience, helping them develop coping mechanisms and skills to manage their trauma-related challenges.
For example, if a child has experienced abuse, I avoid pressuring them to disclose details prematurely. I focus on building trust and safety first, allowing them to share at their own pace. I also pay close attention to signs of retraumatization and adapt my approach accordingly. Trauma-informed care is not just a set of techniques, but a philosophy that permeates all aspects of my practice.
Q 8. What is your approach to crisis intervention with young clients?
My approach to crisis intervention with young clients is grounded in safety, empathy, and empowerment. It’s a collaborative process, not a directive one. First and foremost, I ensure the child’s immediate safety. This might involve contacting relevant authorities like Child Protective Services if abuse or neglect is suspected, or working with the family to create a safe home environment. Then, I use active listening to understand the child’s experience, validating their feelings without judgment. We collaboratively identify coping mechanisms they already possess or can develop, focusing on small, manageable steps rather than overwhelming them with long-term solutions. For example, if a child is experiencing an anxiety attack, we might focus on deep breathing techniques and grounding exercises before delving into the underlying cause. The goal is to help them regain a sense of control and develop self-soothing strategies.
A key aspect is involving caregivers when appropriate and building a strong therapeutic alliance. This includes educating them about the child’s experience and collaboratively developing strategies for support at home. Crisis intervention is not a standalone event; it’s a crucial first step toward ongoing support and therapy to address the underlying issues.
Q 9. How do you assess for suicidal ideation in adolescents, and what steps would you take if you identified it?
Assessing for suicidal ideation requires a sensitive and direct approach. I utilize a combination of methods, including open-ended questions like, “Have you ever thought about harming yourself?” or “Have you felt like life isn’t worth living?” I avoid leading questions and create a safe space where they feel comfortable sharing their thoughts and feelings. Nonverbal cues are equally important; I pay close attention to their body language, tone of voice, and overall demeanor. I also utilize standardized assessment tools, such as the Suicide Risk Assessment Scale, which helps to quantify the risk level.
If suicidal ideation is identified, my immediate priority is ensuring their safety. This involves creating a safety plan collaboratively with the client, their family, and other relevant professionals. The safety plan might include identifying trusted adults, removing access to lethal means, and establishing crisis contact information. If the risk is deemed high, hospitalization may be necessary. It’s crucial to remember that each situation is unique; the intervention strategies are always tailored to the specific circumstances and the client’s individual needs. Ongoing monitoring and therapy are crucial after an immediate crisis is resolved.
Q 10. Describe your experience with different therapeutic modalities, such as play therapy or cognitive behavioral therapy (CBT).
My therapeutic toolbox includes a range of modalities, tailored to the individual needs of the child. Play therapy is particularly effective with younger children who may not have the verbal skills to express their emotions. Through play, children can process trauma, explore feelings, and develop coping mechanisms. For example, using dolls to reenact a difficult situation allows a child to gain control and process feelings associated with the event in a safe environment.
Cognitive Behavioral Therapy (CBT) is valuable for older children and adolescents who can engage in more structured therapeutic work. CBT helps identify negative thought patterns and replace them with more positive and realistic ones. We might use journaling, cognitive restructuring exercises, or behavioral experiments to address anxieties or depression. I also integrate elements of other approaches, such as solution-focused therapy, focusing on strengths and identifying workable solutions, and narrative therapy which helps children to re-author their stories and find meaning in their experiences. The choice of modality is always dictated by the client’s age, developmental stage, and presenting issues.
Q 11. How do you adapt your therapeutic approach to address the unique needs of children with special needs?
Adapting my approach for children with special needs requires a deep understanding of their specific challenges and strengths. This often involves collaborating closely with other professionals, such as educators, therapists specializing in specific disabilities, and medical professionals. For example, when working with a child with autism, I would adapt my communication style to their sensory sensitivities and communication preferences, possibly incorporating visual aids or structured activities. For a child with ADHD, I might incorporate strategies to improve focus and attention, such as incorporating movement breaks or using visual timers. The key is to create a therapeutic environment that accommodates their unique needs, builds on their strengths, and promotes their overall well-being. Communication with the family is paramount to fully understand the child’s challenges and support them holistically.
Q 12. Explain your experience working with children who have experienced abuse or neglect.
Working with children who have experienced abuse or neglect requires a trauma-informed approach. This involves recognizing that trauma can significantly impact a child’s development, emotional regulation, and relationships. I prioritize creating a safe and trusting environment where the child feels empowered to share their experiences at their own pace. I avoid pressuring them to disclose details before they are ready. Trauma-focused therapy modalities like EMDR (Eye Movement Desensitization and Reprocessing) or narrative therapy can be particularly effective. I ensure that the child’s voice is centered, actively listening, validating their feelings, and helping them to regain a sense of control over their lives. Collaboration with caregivers and social work professionals is crucial to provide holistic support, which frequently includes providing safe housing, medical care, and creating a stable environment.
My approach always prioritizes the child’s safety and well-being. I follow mandatory reporting procedures if abuse is suspected, and work closely with Child Protective Services. It’s important to understand that healing from trauma is a long process, and I’m dedicated to supporting the child through each stage of their recovery.
Q 13. How do you build rapport and trust with young clients?
Building rapport and trust with young clients is foundational to effective therapy. It begins with creating a welcoming and safe environment, one where the child feels comfortable being themselves. I use age-appropriate language, making sure to explain things clearly and simply. I show genuine interest in their lives, paying attention to their interests and hobbies, using play and humor appropriately to establish a connection. I validate their feelings, letting them know that it’s okay to feel whatever they are feeling, even if those feelings are difficult.
Maintaining confidentiality is paramount – explaining how confidentiality works in a way they understand helps them trust me. Consistency and reliability are also crucial; showing up on time, being prepared for our sessions, and following through on what we agree upon demonstrates respect for their time and needs. Building this foundation of trust takes time and patience, but it’s the bedrock of any successful therapeutic relationship.
Q 14. How do you utilize assessment tools to inform your treatment plan?
Assessment tools are integral to informing my treatment plan. They provide a more structured and objective approach to understanding the client’s needs, and allow for tracking progress over time. The tools used depend heavily on the age, developmental stage, and presenting issues of the child. For younger children, observational measures and parent reports can be valuable, while for adolescents, self-report questionnaires can be utilized. Examples of common tools include standardized questionnaires assessing depression (e.g., Children’s Depression Inventory), anxiety (e.g., Screen for Child Anxiety Related Emotional Disorders), and trauma (e.g., Trauma Symptom Checklist for Children). Developmental assessments can provide insight into cognitive and social-emotional functioning.
The information gathered from these assessments, combined with clinical interviews and observations, helps me tailor a personalized treatment plan addressing their specific needs and challenges. Assessment isn’t a one-time event; it’s an ongoing process that informs treatment adjustments and monitors progress toward goals. Regular reviews of the assessment data ensure the interventions remain effective and relevant to the changing needs of the child.
Q 15. Describe your experience with documenting client progress and creating treatment plans.
Documenting client progress and developing treatment plans are fundamental aspects of effective child and adolescent counseling. It’s a process that requires meticulous record-keeping and a collaborative approach with the client and their family (when appropriate).
My approach begins with a comprehensive initial assessment, which includes gathering information from the client, parents/guardians, and potentially school records or other relevant sources. This assessment informs the development of a tailored treatment plan outlining specific, measurable, achievable, relevant, and time-bound (SMART) goals. For instance, a goal might be: “Reduce anxiety symptoms, as measured by the Spielberger State-Trait Anxiety Inventory (STAI), by 50% within 12 weeks.”
Progress is documented regularly, often after each session, using progress notes that detail the client’s mood, behavior, adherence to the treatment plan, and any significant events or challenges. I use a combination of qualitative observations (e.g., “Client demonstrated increased self-awareness during today’s session”) and quantitative data (e.g., “Client reported a decrease in their anxiety score on the STAI from 60 to 45”). This data is then used to modify the treatment plan as needed to ensure it remains effective and responsive to the client’s evolving needs. Regular reviews of the treatment plan with the client and their family ensure everyone is on the same page and allows for adjustments based on feedback and progress.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you ensure the safety and well-being of your clients?
Ensuring client safety and well-being is my paramount concern. This is a proactive and ongoing process, integrated into every aspect of my work. It starts with building a strong therapeutic alliance based on trust and respect. Open communication is crucial; I create a safe space where clients feel comfortable discussing anything, including potential safety concerns.
My approach involves several key strategies:
- Risk assessment: At the outset and throughout therapy, I conduct thorough risk assessments to identify any potential threats to the client’s safety (self-harm, suicidal ideation, harm to others). These assessments are documented meticulously.
- Safety planning: If risks are identified, we collaboratively develop safety plans with concrete steps the client can take in moments of crisis. This might involve identifying trusted adults, creating a list of coping mechanisms, or establishing contact information for emergency services.
- Mandated reporting: I adhere strictly to mandated reporting laws, reporting any suspicion of abuse or neglect to the appropriate authorities. This is a legal and ethical obligation, prioritizing the child’s safety.
- Supervision and consultation: I regularly consult with supervisors and colleagues to discuss complex cases and ensure I am taking appropriate safety measures.
Ultimately, ensuring client safety is not a checklist but a continuous, thoughtful process that requires vigilance, ethical awareness, and a commitment to putting the client’s best interests first.
Q 17. What are your strategies for managing challenging behaviors in children and adolescents?
Managing challenging behaviors in children and adolescents requires a multifaceted approach that takes into account the individual’s developmental stage, underlying causes of the behavior, and the specific context in which the behavior occurs. It’s crucial to avoid simplistic labeling and instead focus on understanding the function of the behavior.
My strategies often involve:
- Functional Behavioral Assessment (FBA): This involves systematically observing and analyzing the antecedents (events preceding the behavior), the behavior itself, and the consequences (events following the behavior) to understand the purpose of the behavior. For example, a child might be acting out to escape a disliked task or to gain attention.
- Positive Behavior Support (PBS): This focuses on teaching replacement behaviors and providing positive reinforcement for desired behaviors. Instead of solely punishing undesirable actions, PBS emphasizes teaching and rewarding appropriate alternatives.
- Cognitive Behavioral Therapy (CBT): CBT techniques can help children and adolescents identify and change negative thought patterns and beliefs that contribute to challenging behaviors. For example, if a child believes they are inherently bad, CBT can help them challenge that belief.
- Collaboration with parents/guardians and school: Consistent strategies across different environments (home, school) are crucial for effective behavior management. Collaboration helps ensure a unified approach.
It’s vital to remember that patience and consistency are key. Progress may be gradual, and setbacks are normal. Regular monitoring and adjustments to strategies are necessary to ensure the effectiveness of the intervention.
Q 18. How do you handle situations where a client’s parents disagree with your recommendations?
Disagreements between parents and my recommendations are not uncommon. Addressing these situations requires skillful communication, empathy, and a collaborative approach. The goal is not to impose my viewpoint but to facilitate a shared understanding and a treatment plan that respects everyone’s concerns.
My approach typically involves:
- Open and respectful dialogue: Creating a safe space for parents to express their concerns and perspectives is paramount. I listen actively, validate their feelings, and explain my rationale clearly and respectfully, avoiding jargon.
- Collaboration and compromise: I work collaboratively with parents to find common ground and develop a treatment plan that incorporates their input while upholding professional ethical standards. This might involve adjusting the pace of therapy, focusing on specific goals prioritized by the family, or involving other professionals (e.g., family therapist).
- Education and information: Often, disagreements stem from a lack of understanding of the client’s challenges or the therapeutic process. I provide clear explanations of the client’s diagnosis, treatment rationale, and potential outcomes. I might use analogies or examples to make complex information more accessible.
- Setting clear boundaries: While respecting parental input, it’s vital to maintain professional boundaries. If there are significant disagreements that compromise the client’s well-being or impede effective treatment, I might refer the family to another therapist whose approach aligns better with their preferences.
Ultimately, the focus is on finding a solution that best supports the child’s needs within the family context.
Q 19. Explain your understanding of the legal and ethical considerations related to mandated reporting.
Mandated reporting is a legal and ethical obligation for child and adolescent counselors. It requires reporting any suspicion of child abuse or neglect to the appropriate authorities, typically child protective services. The specific details of mandated reporting laws vary by jurisdiction, but the core principle remains the same: prioritizing the safety and well-being of the child.
My understanding of mandated reporting encompasses:
- Defining abuse and neglect: I am familiar with the legal definitions of different forms of abuse (physical, emotional, sexual) and neglect. The threshold for reporting is often suspicion rather than absolute certainty.
- Recognizing signs and symptoms: I am trained to identify signs of abuse and neglect, both physical and behavioral, in children and adolescents.
- Reporting procedures: I understand the procedures for making a report, including the required information and the appropriate authorities to contact.
- Documentation: I meticulously document any suspicions of abuse or neglect, including dates, times, and the basis for my concerns. This documentation is vital for legal protection and transparency.
- Ethical considerations: While mandated reporting is legally required, it also carries significant ethical implications. I carefully balance the client’s right to confidentiality with the responsibility to protect them from harm. In cases where there is ambiguity, I seek supervision and consultation to make informed decisions.
Failing to report suspected abuse or neglect can have serious legal and ethical repercussions. Prioritizing the safety of the child is always paramount.
Q 20. How do you collaborate with other professionals, such as teachers, doctors, or social workers?
Collaboration with other professionals is crucial for providing comprehensive care to children and adolescents. Effective collaboration requires clear communication, shared goals, and respect for each professional’s expertise.
My strategies for collaboration include:
- Parent/guardian involvement: I maintain open communication with parents/guardians, keeping them informed about the client’s progress and involving them in the treatment process where appropriate and consented.
- School liaison: I communicate regularly with teachers, school counselors, and other school personnel to gain insights into the child’s behavior and academic performance, and to coordinate interventions across settings. For example, discussing strategies for managing classroom behavior.
- Medical professionals: When necessary, I collaborate with pediatricians, psychiatrists, or other medical professionals to obtain relevant medical information and coordinate treatment, such as medication management.
- Social workers: I work with social workers to access resources and support services for families facing challenges, like housing instability or financial hardship.
- Formal referrals: When appropriate, I make formal referrals to other specialists, such as neuropsychologists or occupational therapists, providing necessary information for continuity of care.
Effective collaboration ensures a holistic approach to care, maximizing the chances of positive outcomes for the child or adolescent.
Q 21. How do you maintain your own well-being and prevent burnout as a child and adolescent counselor?
Maintaining my own well-being is not just a personal priority but an ethical responsibility as a child and adolescent counselor. Burnout is a real risk in this demanding profession, and it directly impacts my ability to provide effective and compassionate care to my clients.
My strategies for preventing burnout include:
- Self-care practices: I prioritize activities that promote physical and mental well-being, such as regular exercise, healthy eating, sufficient sleep, and engaging in hobbies that I enjoy.
- Stress management techniques: I utilize stress management techniques, including mindfulness practices, deep breathing exercises, and spending time in nature. This helps me manage the emotional toll of the work.
- Supervision and consultation: Regular supervision with experienced colleagues provides a space to process challenging cases, reflect on my practice, and receive support and guidance.
- Setting boundaries: I maintain healthy boundaries between my professional and personal life, avoiding overwork and prioritizing time off. I carefully manage my caseload to avoid feeling overwhelmed.
- Seeking support: I recognize the importance of seeking support from friends, family, or a therapist when needed. This helps maintain perspective and prevent isolation.
- Continuing education: Engaging in continuing education opportunities keeps me updated on best practices, enhances my skills, and reinforces my sense of professional competence and purpose.
By prioritizing my own well-being, I am better equipped to support the well-being of my clients.
Q 22. Describe a time you had to deal with a difficult or challenging client.
One particularly challenging client was a 15-year-old girl, Sarah, who exhibited severe self-harm behaviors and expressed intense feelings of worthlessness. Her initial sessions were marked by significant resistance and a refusal to engage meaningfully. I recognized that her resistance stemmed from a deep-seated fear of vulnerability and a lack of trust. My approach involved building rapport slowly, focusing on establishing a safe and non-judgmental therapeutic space. Instead of directly confronting her self-harm, I began by validating her feelings and acknowledging the immense pain she was experiencing. We started with activities like art therapy and journaling, which allowed her to express herself without the pressure of direct verbalization. Gradually, as trust developed, we delved into the underlying issues, including a history of trauma and family conflict. The process was lengthy and required patience, flexibility, and consistent support. We eventually incorporated Cognitive Behavioral Therapy (CBT) techniques to help her identify and challenge negative thought patterns and develop healthier coping mechanisms. While there were setbacks, consistent effort resulted in a significant reduction in her self-harm behaviors and a noticeable improvement in her overall mood and self-esteem.
Q 23. What are the common signs of depression and anxiety in children and adolescents?
Identifying depression and anxiety in children and adolescents can be complex, as symptoms often manifest differently than in adults. Common signs of depression include persistent sadness, loss of interest in activities once enjoyed, significant changes in appetite or sleep patterns, feelings of hopelessness or worthlessness, fatigue, and difficulty concentrating. In adolescents, irritability and social withdrawal are also common. Anxiety in children and adolescents can present as excessive worry, nervousness, difficulty sleeping, irritability, stomach aches or headaches, and avoidance behaviors. Younger children might exhibit separation anxiety or clinginess. Adolescents may experience social anxiety, panic attacks, or obsessive-compulsive behaviors. It’s important to remember that these symptoms can overlap, and a thorough assessment is crucial for accurate diagnosis. Observing changes in behavior and academic performance, alongside parental reports, are invaluable.
Q 24. What are your strategies for engaging reluctant clients?
Engaging reluctant clients often requires a collaborative and flexible approach. I begin by acknowledging their reluctance and validating their feelings. I avoid pressure and instead focus on building rapport by finding common ground. This might involve discussing their interests, hobbies, or even something as simple as the weather. The goal is to create a safe and non-threatening environment where they feel comfortable sharing their thoughts and feelings. I might suggest activities like games or creative arts therapies as an alternative to traditional talk therapy, especially with younger clients. Collaborative goal setting is crucial. Instead of imposing a treatment plan, I work with the client to identify their goals and tailor the therapy accordingly. Flexibility is key; I’m willing to adjust my approach based on the client’s responses and preferences.
Q 25. How do you address the issue of confidentiality with children?
Confidentiality is a crucial aspect of the therapeutic relationship, but with minors, it’s nuanced. I explain confidentiality in a way that a child or adolescent can understand, emphasizing that our conversations are private. However, I also clearly explain the limits of confidentiality. I explain that I am mandated to report situations involving immediate danger to themselves or others, including thoughts of suicide or self-harm, and instances of child abuse or neglect. I explain this in simple terms, using age-appropriate language and offering examples to illustrate these exceptions. This approach aims to balance the importance of privacy with the legal and ethical obligations I have to protect the child’s well-being.
Q 26. Explain your experience with diagnosing and treating ADHD in children.
Diagnosing ADHD requires a comprehensive assessment, combining behavioral observations, parent and teacher reports, and standardized testing. I utilize various assessment tools, including rating scales (like the Conners’ Rating Scales) and clinical interviews to gather information about the child’s symptoms, their impact on daily functioning, and their developmental history. A thorough assessment helps differentiate ADHD from other conditions with overlapping symptoms. Treatment typically involves a multi-faceted approach. Behavioral therapy, focusing on strategies to improve attention, impulse control, and organizational skills, plays a vital role. In many cases, medication may be recommended in consultation with a psychiatrist or physician, especially when symptoms significantly impair functioning. I work closely with parents and educators to create a consistent and supportive environment at home and school, involving them actively in the treatment plan. Regular monitoring and adjustments to the treatment plan are essential to ensure its effectiveness and address any emerging challenges.
Q 27. What are your strategies for working with families experiencing conflict?
Working with families experiencing conflict often involves employing family systems therapy principles. My approach focuses on understanding the family’s dynamics and communication patterns. I help family members identify recurring patterns of interaction that contribute to the conflict. I facilitate open communication, encouraging each member to express their feelings and perspectives in a safe and respectful environment. I teach active listening skills and conflict-resolution techniques, empowering them to communicate more effectively. I often utilize family sculpting or other visual techniques to help family members visualize their roles and relationships within the family system. The goal is to help the family develop healthier communication strategies, establish clear boundaries, and improve their overall functioning. Collaboration and a non-judgmental approach are key to fostering positive change.
Q 28. Describe a time you successfully helped a child or adolescent overcome a significant challenge.
One of the most rewarding experiences involved working with a young boy, Mark, who suffered from severe social anxiety. He was virtually isolated and struggled to interact with his peers. My approach focused on building his self-esteem and developing coping skills. We started with gradual exposure techniques, beginning with small interactions, like saying hello to a classmate. We progressively increased the complexity of the social situations, using role-playing and positive reinforcement. I also incorporated Cognitive Restructuring techniques to help him challenge his negative thoughts and beliefs about social situations. We celebrated small victories along the way, building his confidence. Over time, Mark’s social anxiety significantly reduced. He started making friends, participating in class activities, and even joined the school’s drama club. Witnessing his transformation from a withdrawn and anxious child to a confident and outgoing young man was incredibly fulfilling and highlighted the power of therapeutic intervention.
Key Topics to Learn for Child and Adolescent Counseling Interview
- Developmental Psychology: Understanding child and adolescent development across various stages, including cognitive, social, emotional, and physical milestones. Practical application: Analyzing a case study and identifying developmental delays or challenges.
- Therapeutic Modalities: Familiarity with various therapeutic approaches such as Cognitive Behavioral Therapy (CBT), Play Therapy, Family Systems Therapy, and Person-Centered Therapy. Practical application: Discussing the suitability of different therapies for specific age groups and presenting cases.
- Ethical and Legal Considerations: Understanding confidentiality, mandated reporting, and ethical dilemmas in working with children and adolescents. Practical application: Analyzing ethical scenarios and proposing solutions.
- Assessment and Diagnosis: Proficiency in utilizing assessment tools and diagnostic criteria (e.g., DSM-5) to evaluate mental health concerns. Practical application: Describing the process of conducting a comprehensive assessment.
- Trauma-Informed Care: Understanding the impact of trauma on children and adolescents and implementing trauma-sensitive approaches in therapy. Practical application: Explaining how to create a safe and supportive therapeutic environment.
- Crisis Intervention and Safety Planning: Skills in identifying and managing crises and developing safety plans for clients at risk. Practical application: Describing procedures for handling self-harm or suicidal ideation.
- Cultural Competence: Understanding the impact of culture and diversity on mental health and providing culturally sensitive care. Practical application: Discussing strategies to adapt therapeutic approaches to diverse populations.
- Collaboration and Teamwork: Understanding the importance of collaborating with parents, schools, and other professionals. Practical application: Describing effective communication strategies with various stakeholders.
Next Steps
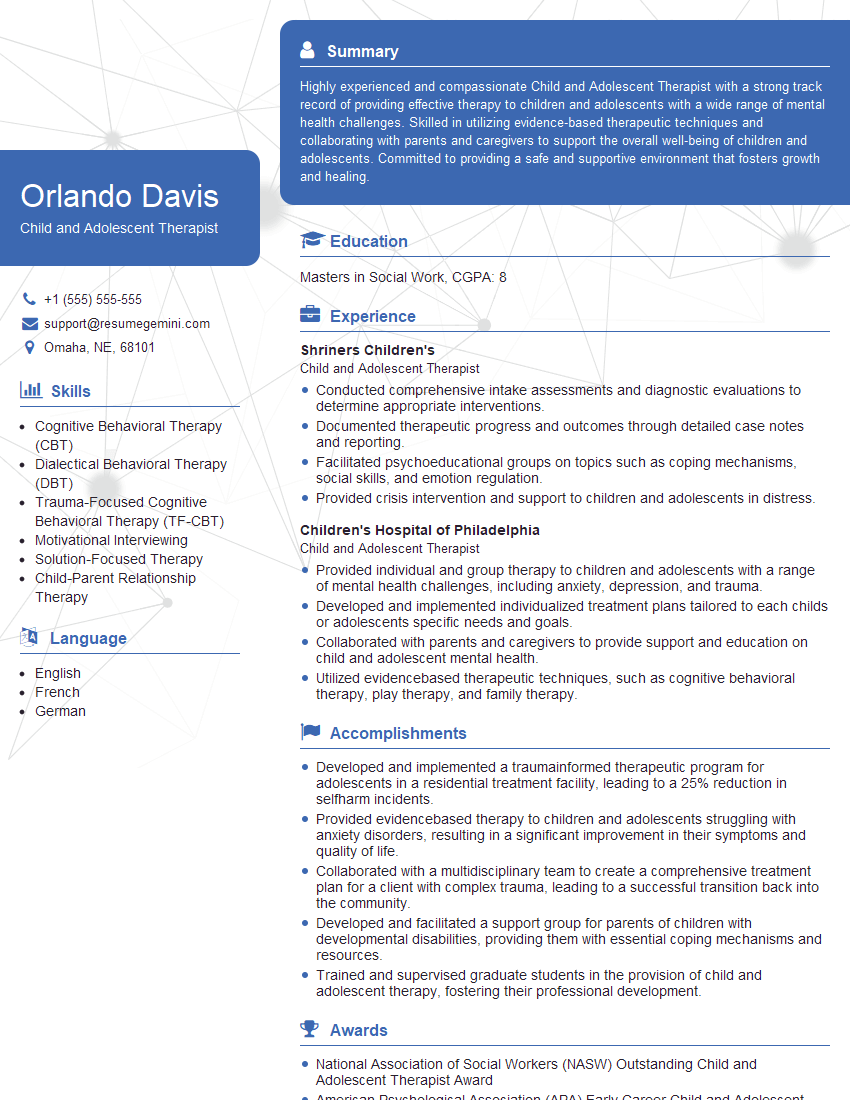
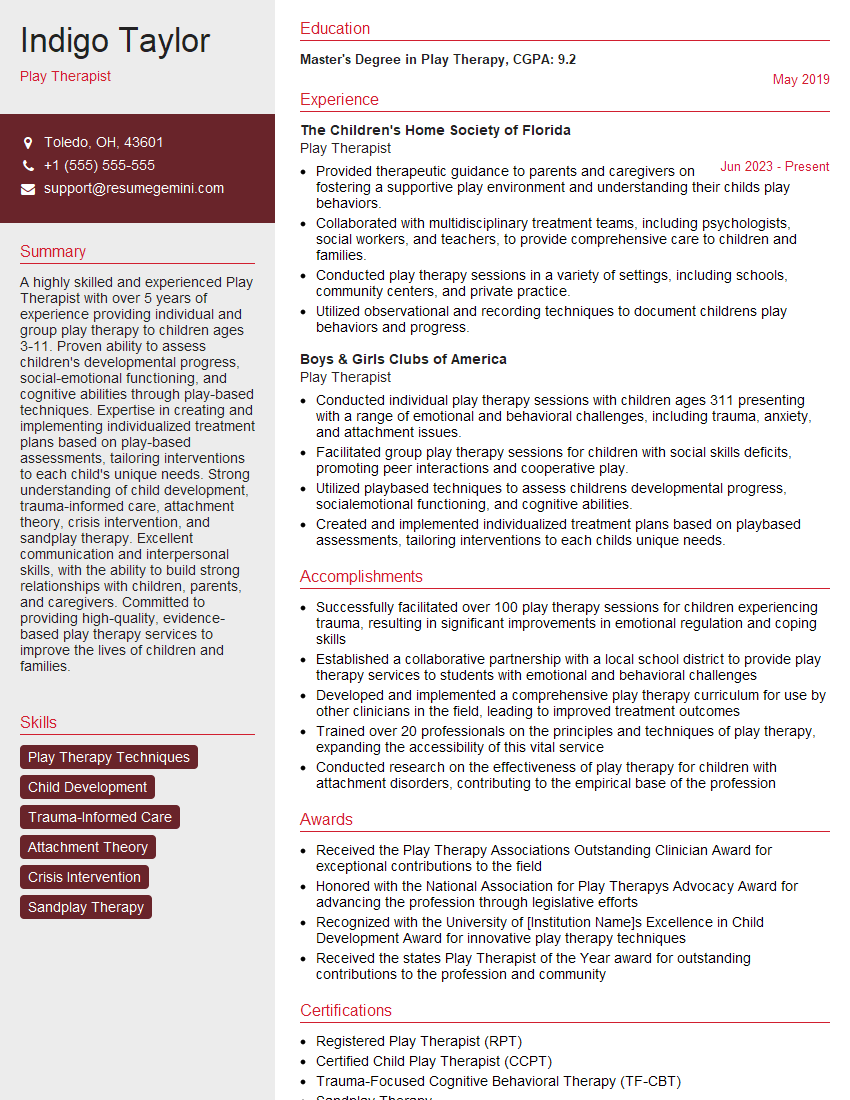
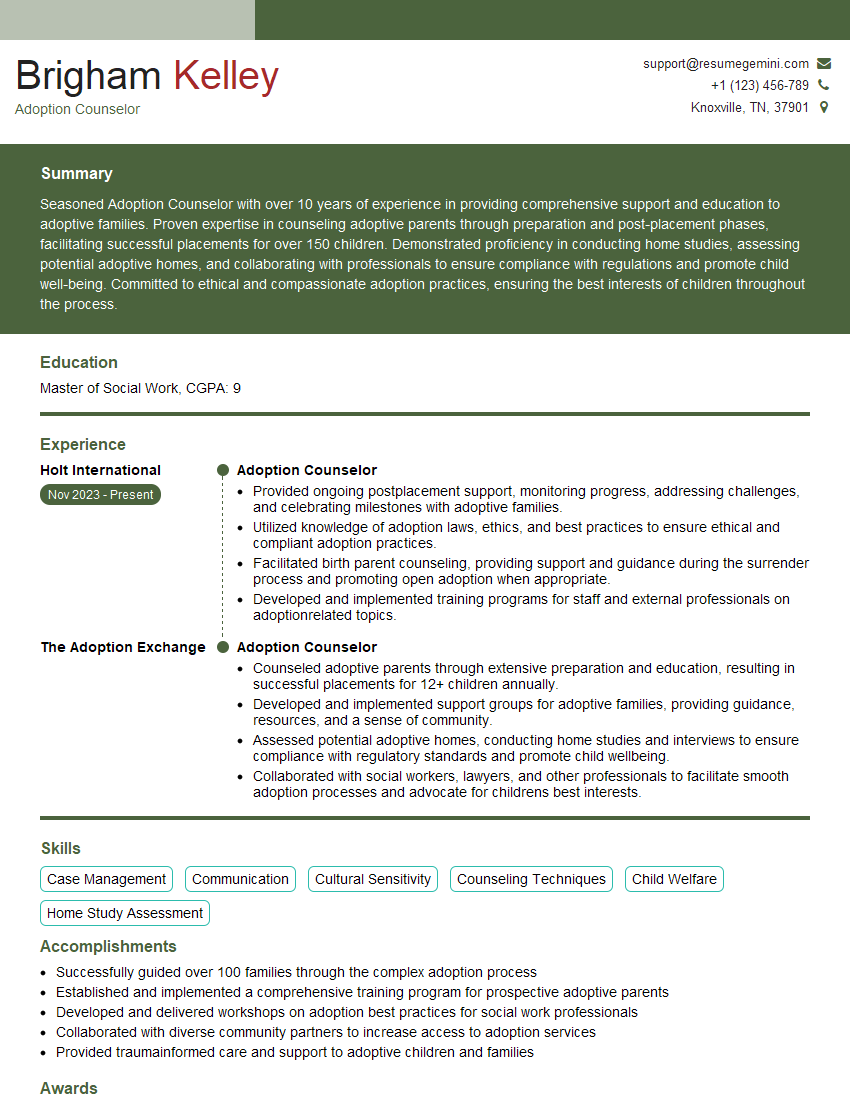
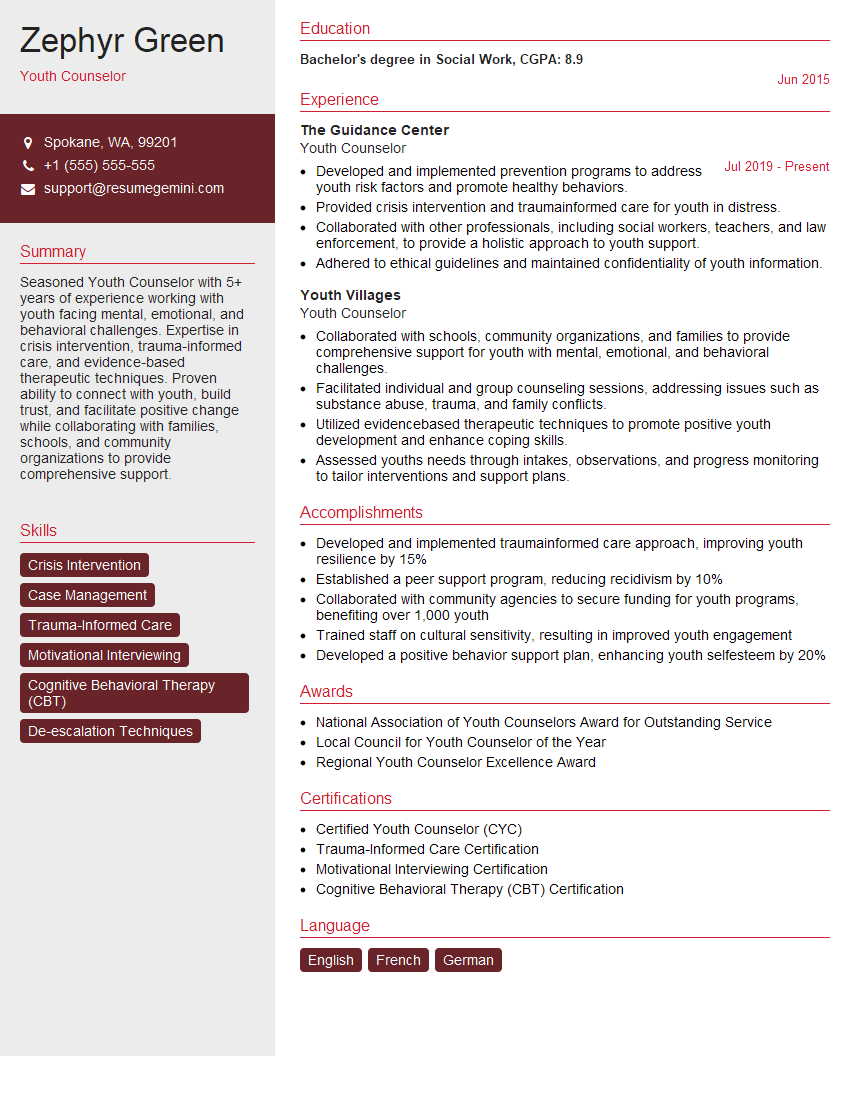
Mastering Child and Adolescent Counseling opens doors to a fulfilling and impactful career, allowing you to make a real difference in the lives of young people. To maximize your job prospects, creating a strong, ATS-friendly resume is crucial. ResumeGemini is a trusted resource that can help you build a professional and effective resume tailored to the specific demands of this field. We provide examples of resumes specifically designed for Child and Adolescent Counseling positions to help you showcase your skills and experience effectively. Take the next step towards your dream career today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO