Are you ready to stand out in your next interview? Understanding and preparing for Clinical Supervision and Mentoring interview questions is a game-changer. In this blog, we’ve compiled key questions and expert advice to help you showcase your skills with confidence and precision. Let’s get started on your journey to acing the interview.
Questions Asked in Clinical Supervision and Mentoring Interview
Q 1. Describe your approach to providing constructive feedback during supervision.
My approach to providing constructive feedback centers around the principles of specificity, balance, and collaboration. I avoid generalizations and focus on observable behaviors and their impact. For instance, instead of saying ‘You need to be more assertive,’ I might say, ‘In the last session, when the client challenged your interpretation, you seemed hesitant to fully articulate your perspective. This may have left the client feeling unheard. Let’s explore ways to confidently express your clinical judgments while remaining empathetic.’ This approach combines a specific observation with suggestions for improvement, fostering a collaborative dialogue rather than a critical judgment. I always ensure that the feedback is balanced, acknowledging both strengths and areas for growth, and that it’s delivered in a timely and supportive manner, allowing for immediate reflection and discussion.
Q 2. How do you handle conflict between supervisees?
Handling conflict between supervisees requires a delicate balance of fairness, impartiality, and active listening. My first step is to meet with each supervisee individually to understand their perspectives, ensuring a safe space for open communication. I encourage them to express their concerns and feelings without interruption. Then, I facilitate a joint meeting if appropriate, acting as a neutral mediator. The goal is not to determine who is ‘right’ or ‘wrong,’ but to help them understand each other’s viewpoints and collaboratively find solutions. I may use conflict resolution strategies such as identifying common goals, clarifying misunderstandings, and generating mutually agreeable solutions. In situations involving serious ethical violations or interpersonal harm, clear boundaries and potential disciplinary actions must be addressed.
Q 3. Explain your process for evaluating supervisee performance.
My process for evaluating supervisee performance is multifaceted and aligns with professional standards. It combines multiple data points to create a holistic picture of their progress. This includes regular observation of their clinical work (e.g., through session recordings, case notes review, and live supervision), assessment of their self-reflection and professional development, and feedback from clients (with their consent, of course). I use a structured evaluation form that addresses key competencies such as clinical skills, ethical decision-making, self-awareness, and interpersonal effectiveness. This form allows for both quantitative (e.g., rating scales) and qualitative (e.g., written comments) data. The evaluation is discussed with the supervisee in a supportive and collaborative way, focusing on growth and improvement. This ensures the evaluation serves as a valuable tool for professional development, not just a judgment of performance.
Q 4. What are your preferred methods for assessing supervisee competence?
Assessing supervisee competence is a continuous process, employing several methods to ensure a comprehensive understanding. I observe their clinical skills through role-playing exercises, case presentations, and live supervision. I review their written work, such as treatment plans, session notes, and progress summaries, focusing on clarity, accuracy, and ethical considerations. I also assess their self-awareness through reflective practice, encouraging them to critically examine their own biases and limitations. Finally, client feedback, obtained with appropriate consent and anonymity, can provide valuable insights into the supervisee’s effectiveness. The combination of these methods creates a reliable and valid assessment of their competence, allowing for personalized feedback and support.
Q 5. How do you foster a supportive and collaborative supervisory relationship?
Fostering a supportive and collaborative supervisory relationship is paramount. This is achieved through creating a safe and confidential space where supervisees feel comfortable sharing their experiences, challenges, and successes without fear of judgment. I actively listen, show empathy, and offer support. I establish clear expectations and boundaries from the outset, while also prioritizing flexibility and adaptation as needed. Regular check-ins allow us to assess the supervisory process and make adjustments as required. I encourage open communication, using ‘I’ statements to share my observations and perspectives, and I consistently model respect and collaboration in my interactions. I view supervision as a partnership, where we jointly work toward the supervisee’s professional growth and well-being. This relationship is built on trust, mutual respect, and a shared commitment to excellence in clinical practice.
Q 6. Describe your experience with different supervision models (e.g., psychodynamic, cognitive-behavioral).
My experience encompasses various supervision models, including psychodynamic, cognitive-behavioral, and integrative approaches. In psychodynamic supervision, the focus is on the supervisee’s countertransference and the impact of their own personal experiences on their clinical work. We explore unconscious processes and how they influence the therapeutic relationship. In cognitive-behavioral supervision, we emphasize the application of specific techniques, focusing on the identification and modification of maladaptive thoughts and behaviors. We discuss case conceptualization, treatment planning, and the use of evidence-based interventions. My integrative approach draws on the strengths of different models, tailoring the supervision to the individual needs and preferences of each supervisee and the specific clinical challenges they encounter. I believe that flexibility and adaptability are crucial to effective supervision, and I choose the most appropriate theoretical framework depending on the situation.
Q 7. How do you address ethical dilemmas that arise during supervision?
Addressing ethical dilemmas is a critical aspect of supervision. When an ethical dilemma arises, my first step is to ensure the safety and well-being of the client. Then, I work collaboratively with the supervisee to thoroughly explore the situation, considering all relevant ethical principles and professional guidelines. We use ethical decision-making frameworks, such as the A-B-C-D-E method (Assess, Benefit, Consequences, Duty, Education) to analyze the situation systematically. This framework helps us identify potential courses of action and their associated implications. We also discuss relevant professional codes of ethics and relevant legal considerations. If necessary, we consult with other experienced professionals or seek guidance from an ethics committee. Transparency, documentation, and ongoing reflection are crucial in navigating complex ethical dilemmas, ensuring the protection of clients and upholding professional standards.
Q 8. How do you maintain your own professional development as a supervisor?
Maintaining my professional development as a supervisor is an ongoing commitment, crucial for providing effective and ethical guidance. It’s like a doctor staying current on medical advancements – stagnant knowledge leads to outdated practices.
Continuing Education: I regularly attend workshops, conferences, and webinars focused on the latest research in clinical supervision, therapeutic modalities, and ethical considerations. For instance, I recently completed a course on trauma-informed supervision, which significantly enhanced my ability to support supervisees working with trauma survivors.
Peer Supervision: I actively participate in peer supervision groups where I can discuss challenging cases, receive feedback on my own supervisory style, and learn from colleagues’ experiences. This creates a supportive network for continuous learning and growth.
Supervision of my own practice: I also seek supervision for my own clinical work to ensure I maintain a strong self-awareness and address any personal biases or countertransference issues that might impact my supervision.
Reading and Research: I dedicate time to reading professional journals, books, and articles related to supervision and relevant clinical areas. This allows me to stay updated on best practices and emerging trends.
Q 9. How do you ensure confidentiality within the supervisory relationship?
Confidentiality is paramount in the supervisory relationship. It forms the bedrock of trust and allows supervisees to openly explore challenging cases without fear of judgment or repercussions. I establish clear boundaries around confidentiality from the outset of the supervisory relationship.
Informed Consent: I provide supervisees with a written statement clearly outlining the limits of confidentiality. For example, I will explain situations where I might be legally obligated to break confidentiality, such as threats of harm to self or others.
Record Keeping: I maintain meticulous records, adhering to all relevant legal and ethical guidelines. My notes are stored securely and are only accessible to me, unless there is a legal requirement for disclosure.
Avoiding Casual Discussion: I never discuss supervisory cases in informal settings or with individuals who are not directly involved in the supervisory process. This includes refraining from casual conversations about clients in public places.
Data Security: I utilize secure electronic storage and comply with all relevant data protection regulations to ensure client information remains protected.
Q 10. How do you adapt your supervisory style to meet the diverse needs of supervisees?
Adapting my supervisory style to meet diverse needs is essential. A one-size-fits-all approach simply won’t work. I believe in tailoring my approach to each supervisee’s unique experience, personality, and learning style.
Developmental Level: I consider the supervisee’s experience level. A newly licensed therapist will require different support than a seasoned clinician.
Learning Preferences: Some supervisees prefer structured, directive supervision; others thrive in a more collaborative, reflective environment. I assess their preferences and adapt accordingly, possibly incorporating different approaches like role-playing, case presentations, or reflective practices.
Cultural Sensitivity: I am mindful of cultural differences and ensure that my supervision style is inclusive and respectful of diverse perspectives. I make sure to consider the impact of cultural factors on clinical practice and adjust my approach accordingly.
Feedback and Evaluation: I use a combination of methods for evaluating progress, including regular feedback sessions, performance reviews, and self-reflection exercises to cater to different needs and preferences.
Q 11. What are your strategies for supporting supervisees’ professional growth?
Supporting supervisees’ professional growth is a core component of effective supervision. I view my role as a facilitator of their development, helping them to achieve their professional goals.
Goal Setting: We collaboratively establish clear, measurable, achievable, relevant, and time-bound (SMART) goals for each supervision period. This provides a roadmap for their professional growth.
Skill Development: I identify areas where the supervisee needs further development and provide targeted training, resources, or opportunities for skill enhancement. This might include recommending specific workshops, providing feedback on specific techniques, or offering opportunities for observation of my own work.
Self-Reflection: I encourage self-reflection and critical analysis of their practice through journaling, case discussions, and other reflective exercises. This fosters a deeper understanding of their strengths and weaknesses.
Networking and Mentorship: I assist supervisees in building their professional networks by connecting them with other professionals, encouraging presentations at conferences, or linking them to relevant professional organizations.
Q 12. Describe your experience with mentoring junior colleagues.
My experience mentoring junior colleagues has been incredibly rewarding. I’ve found that a supportive and collaborative approach yields the best results. I’ve mentored several junior therapists, providing guidance on everything from clinical technique to navigating the complexities of the professional world.
Example: I mentored a new graduate struggling with case conceptualization. We worked together using a structured approach, breaking down complex cases into manageable parts, and practicing different therapeutic interventions. By providing regular feedback and encouragement, I helped her gain confidence and proficiency in this crucial skill.
Shared Learning: I believe mentorship is a two-way street, and I value the opportunity to learn from the perspectives and experiences of junior colleagues. Their fresh insights often challenge my assumptions and broaden my understanding.
Q 13. How do you identify and address potential burnout in supervisees?
Identifying and addressing potential burnout in supervisees is crucial. Burnout can severely impact their well-being and professional effectiveness. I actively look for signs, which can manifest in various ways.
Signs of Burnout: These include decreased job satisfaction, cynicism, emotional exhaustion, depersonalization, and physical symptoms such as fatigue, insomnia, and headaches.
Open Communication: I create a safe space for supervisees to discuss their experiences, both personal and professional. I encourage open communication about workload, stress levels, and any challenges they might be facing.
Self-Care Strategies: I help supervisees develop healthy coping mechanisms and self-care strategies, emphasizing the importance of maintaining a work-life balance. This might include recommending stress-reduction techniques, promoting mindfulness practices, or encouraging participation in activities outside of work.
Referral: If I suspect a supervisee is experiencing significant burnout, I strongly encourage them to seek professional help from a therapist or counselor.
Q 14. What resources do you utilize to support your supervision practice?
I utilize a variety of resources to enhance my supervision practice. It’s like a toolbox filled with various instruments, each suited for a different task.
Professional Organizations: I am a member of relevant professional organizations, such as the [Insert Relevant Professional Organization], which provides access to continuing education opportunities, ethical guidelines, and networking opportunities.
Supervision Texts and Journals: I regularly consult various texts and journals focused on clinical supervision and relevant therapeutic approaches.
Online Resources: I leverage various online resources, including databases of research articles and professional development webinars, to stay current with the latest trends and research findings.
Consultants and Experts: When faced with challenging cases or ethical dilemmas, I don’t hesitate to seek consultation from experienced colleagues or other experts in the field.
Q 15. How do you balance the needs of individual supervisees with the overall goals of the program?
Balancing individual supervisee needs with program goals requires a delicate approach. It’s like conducting an orchestra – each musician (supervisee) has unique strengths and needs, but the overall performance (program goals) must be harmonious and successful. I achieve this through careful planning and individualized supervision plans.
- Individualized Learning Plans: Each supervisee starts with a personalized plan outlining their specific professional development goals, aligned with the broader program objectives. This ensures individual growth contributes to the overall success. For example, a supervisee focused on improving trauma-informed care might tailor their goals to reflect this, while still contributing to the program’s overall goal of enhancing client outcomes.
- Regular Check-ins: Frequent one-on-one meetings allow for continuous monitoring of progress and adjustment of the plan based on individual needs. If a supervisee is struggling with a particular skill, we can adapt their plan and provide additional support, without compromising the larger program’s timeline.
- Group Supervision: Utilizing group supervision sessions allows for peer learning and support. Supervisees can learn from each other’s experiences and challenges, fostering a sense of community while still pursuing individual growth. This allows for a shared understanding of the overall program goals and how individual contributions fit into the bigger picture.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you facilitate self-reflection and professional growth in supervisees?
Facilitating self-reflection and professional growth involves creating a safe and supportive environment where supervisees can explore their practice critically and honestly. Think of it as helping them build their own professional compass. I use several techniques:
- Reflective Questioning: I use open-ended questions to encourage supervisees to analyze their clinical work, such as ‘What was your initial reaction to the client’s statement?’, ‘What other approaches could you have taken?’, and ‘What did you learn from this experience?’ This prompts deeper thinking and self-awareness.
- Case Conceptualization: We collaboratively work through challenging cases, exploring theoretical frameworks and different approaches to improve future practice. This forces the supervisee to analyze their interventions, identify strengths and weaknesses, and learn from mistakes.
- Feedback and Goal Setting: Providing constructive feedback, focusing both on strengths and areas for development, is crucial. We then collaboratively set specific, measurable, achievable, relevant, and time-bound (SMART) goals to guide their professional development.
- Supervision Logs: Encouraging supervisees to maintain logs of their sessions enhances self-reflection. Regular review of these logs, during supervision sessions, provides valuable insights into patterns and areas needing improvement.
Q 17. How do you utilize case studies in your supervisory sessions?
Case studies are invaluable tools in supervision. They provide a safe space to explore complex clinical situations without the immediate pressures of real-time practice. I utilize them in several ways:
- Illustrative Cases: I present de-identified cases to illustrate specific clinical concepts, techniques, or ethical dilemmas, sparking discussion and critical analysis. For example, discussing a case showcasing boundary issues can help supervisees identify potential pitfalls in their own practice.
- Supervisee-Presented Cases: Supervisees bring their own anonymized cases for discussion and analysis. This fosters ownership and enables a more in-depth exploration of their clinical decision-making process.
- Role-Playing: Using case studies as a basis, we engage in role-playing scenarios to practice specific techniques or address challenging situations. This provides a safe space for practicing communication skills and intervention strategies.
- Comparative Case Analysis: Presenting several related cases allows supervisees to compare and contrast approaches, highlighting the importance of individualization of care and contextual factors.
Q 18. How do you provide supervision to supervisees in diverse settings?
Supervising in diverse settings requires adaptability and cultural sensitivity. My approach centers around understanding and respecting the unique contexts in which supervisees operate.
- Contextual Understanding: I begin by thoroughly understanding the specific setting, including the organizational culture, client population, and any relevant policies or regulations. This allows me to tailor my supervision to the unique challenges and opportunities presented.
- Culturally Sensitive Supervision: I strive to create a culturally safe space where supervisees feel comfortable discussing their experiences and challenges in a non-judgmental environment. This includes acknowledging and addressing any potential power dynamics or biases that might exist.
- Collaboration and Consultation: I actively seek consultation with colleagues and supervisors experienced in working with diverse populations and settings to enhance my ability to provide effective and culturally competent supervision.
- Tailored Supervision Strategies: The methods I employ, including the frequency and format of supervision, are adapted to best fit the needs and circumstances of the setting and the supervisee. For instance, virtual supervision might be more practical for supervisees in remote settings.
Q 19. How do you address supervisees’ personal challenges that may impact their work?
Addressing supervisees’ personal challenges requires a nuanced approach, balancing professional boundaries with genuine care and support. It is crucial to remember that the well-being of the supervisee is interconnected with their professional competence.
- Confidentiality and Boundaries: I clearly define the limits of confidentiality and the scope of my role as a supervisor. While providing support, I emphasize the importance of seeking appropriate professional help for personal challenges impacting their work.
- Early Identification: Regular check-ins and open communication create opportunities to identify potential issues early on. Signs of burnout, stress, or personal difficulties might be visible in their clinical work or personal demeanor.
- Referral and Support: If a supervisee’s personal challenges significantly impact their ability to function professionally, I would recommend seeking assistance from appropriate mental health professionals or employee assistance programs.
- Self-Care Strategies: I encourage and support healthy coping mechanisms and self-care practices to mitigate the effects of stress and burnout in the profession. This might include mindfulness techniques, time management strategies, or seeking peer support.
Q 20. Describe your experience with conducting performance reviews for supervisees.
Performance reviews are an opportunity for both assessment and growth. I approach them as a collaborative process focused on both acknowledging achievements and identifying areas for development.
- Data-Driven Assessment: Reviews are based on observable behaviors and documented performance data, including case notes, client feedback, and peer observations. This approach is objective and avoids relying solely on subjective impressions.
- Constructive Feedback: I provide both positive and constructive feedback using the ‘sandwich method’—beginning with a strength, providing specific constructive feedback, and ending with another positive point. This helps make critical feedback less daunting.
- Goal Setting for Improvement: Following the review, we collaborate to set realistic and attainable goals for improvement. These goals are specific and tied to observable behaviors, with timelines for achieving them.
- Follow-Up and Support: The review isn’t a one-time event. We schedule follow-up meetings to discuss progress toward goals and offer additional support as needed. This ensures the supervisee feels supported throughout their professional growth journey.
Q 21. How do you manage difficult conversations with supervisees?
Difficult conversations are inevitable in supervision. My approach emphasizes empathy, clarity, and a focus on problem-solving.
- Preparation: Before the conversation, I carefully consider the issues to be addressed, outlining key points and potential solutions. I strive to maintain a calm and neutral demeanor.
- Active Listening: I actively listen to the supervisee’s perspective, showing empathy and understanding. This demonstrates respect and creates an environment for open dialogue.
- Clear Communication: I communicate my concerns directly but respectfully, using ‘I’ statements to avoid assigning blame. For example, instead of saying ‘You made a mistake,’ I might say ‘I noticed this approach presented some challenges in this case; let’s explore alternative options.’
- Collaborative Problem-Solving: We work together to identify solutions and develop an action plan. This shifts the focus from criticism to growth and empowerment.
- Follow-Up: After the conversation, I follow up to check on progress and provide any additional support needed. This reinforces the commitment to collaborative growth and shows continued care.
Q 22. What are your strategies for promoting diversity, equity, and inclusion in supervision?
Promoting diversity, equity, and inclusion (DEI) in supervision is crucial for creating a safe and supportive learning environment for supervisees from all backgrounds. My strategies involve proactively creating an inclusive space where diverse perspectives are valued and celebrated. This begins with self-reflection on my own biases and ensuring my approach is culturally sensitive and responsive to individual needs.
- Culturally Responsive Supervision: I actively learn about and incorporate the cultural backgrounds and experiences of my supervisees into the supervision process. This includes understanding how their cultural contexts may influence their practice and adjusting my approach accordingly.
- Inclusive Language and Communication: I use inclusive language, avoiding jargon or assumptions about my supervisees’ backgrounds or experiences. I actively listen to understand their perspectives and create a space where they feel comfortable expressing themselves honestly.
- Equitable Access to Resources and Opportunities: I ensure that all supervisees have equal access to resources and opportunities for professional development. This includes providing tailored support based on individual needs and advocating for equal opportunities within the organization.
- Addressing Microaggressions and Bias: I actively address microaggressions and any instances of bias that may arise during supervision. This includes open dialogue and education to foster a more inclusive environment.
- Diverse Supervision Models: I embrace diverse supervisory models, such as peer supervision, group supervision, or mentoring, to create a more inclusive and collaborative learning environment.
For example, I recently supervised a social worker from a refugee background. I made sure to be sensitive to the potential trauma she might have experienced and the cultural nuances influencing her client interactions, adapting my feedback and support accordingly.
Q 23. Describe a time you had to make a difficult decision regarding a supervisee.
One challenging situation involved a supervisee who was consistently violating client confidentiality. This was a difficult decision because it involved balancing my ethical obligations with my responsibility to support the supervisee’s professional growth. My first step was to document all instances of the breach, ensuring accurate records of dates, times, and specific details.
I then engaged in a series of carefully planned supervisory sessions with the supervisee, providing supportive feedback while clearly outlining the ethical violations and potential consequences. I explored the underlying reasons for their behavior, understanding that it could stem from stress, inexperience, or other factors. We collaboratively developed a plan of action to address the issue, which included additional training on ethical codes and strategies for maintaining confidentiality. This included role-playing scenarios and reflective exercises.
Despite the plan, the breaches continued. As a last resort, and after thoroughly documenting the situation and consulting with my supervisor and the relevant ethics board, I reported the repeated violations to the appropriate authorities. This was a difficult but necessary decision to protect client well-being and uphold professional ethics. While it was emotionally challenging, it ultimately affirmed the importance of upholding ethical standards, even when it means taking difficult actions.
Q 24. How do you ensure ongoing professional competence in your area of expertise?
Maintaining ongoing professional competence is a continuous process, not a one-time event. My approach involves a multi-faceted strategy to stay current with best practices, research, and ethical guidelines in clinical supervision and mentoring.
- Continuing Education: I actively participate in workshops, conferences, and training programs related to clinical supervision, mentoring, and relevant therapeutic modalities. I regularly review and engage with peer-reviewed research to stay updated on the latest findings and best practices.
- Professional Development: I actively seek out professional development opportunities, including attending workshops, conferences, and webinars on related topics such as trauma-informed care, cultural competency, and ethical decision-making in supervision.
- Supervision and Consultation: I regularly engage in my own supervision and consultation with experienced colleagues to gain feedback on my practice and enhance my skills. This provides a valuable opportunity to reflect on my own practice and identify areas for improvement.
- Networking and Collaboration: I actively engage in networking and collaboration with other supervisors and mentors to share best practices, discuss challenging cases, and participate in peer learning opportunities.
- Self-Reflection: I regularly engage in self-reflection to identify areas of strength and growth within my supervisory practice, and seek feedback on my effectiveness as a supervisor. Journaling and regular personal reflection helps solidify this.
For instance, I recently completed a specialized training program in trauma-informed supervision, equipping me with additional skills and knowledge to support supervisees working with trauma survivors.
Q 25. How do you document supervisory sessions?
Documentation is crucial for accountability, ethical practice, and effective supervision. My documentation process prioritizes clarity, accuracy, and confidentiality. I use a structured approach that balances thorough record-keeping with the need to maintain client confidentiality.
I typically utilize electronic health record (EHR) systems with secure access to store supervisory notes. These notes include the date, time, and attendees of the session. I focus on summarizing key discussion points, action plans agreed upon, any concerns raised, and the supervisee’s progress and challenges. I avoid recording verbatim conversations, instead, opting for concise summaries and key observations. I also document any relevant ethical considerations or decisions made during the session. All documentation is stored securely and adheres to relevant privacy regulations and organizational policies.
It is essential to maintain concise, objective notes focusing on observable behaviors and professional progress. This documentation serves as a vital resource for ongoing supervision, professional development, and potential legal or ethical review. This balance between thoroughness and brevity ensures effective documentation while preventing unnecessary lengthiness.
Q 26. Explain the importance of setting clear boundaries in a supervisory relationship.
Setting clear boundaries in a supervisory relationship is essential for maintaining a professional and ethical practice. These boundaries protect both the supervisor and the supervisee, fostering a healthy and productive working relationship. Clear boundaries create a safe space for honest and open communication, encourage professional growth, and prevent potential conflicts of interest.
- Time Boundaries: Clearly defining the start and end times of supervision sessions, as well as adhering to these set times, ensures a respectful use of each person’s time.
- Professional Role Boundaries: Maintaining a professional relationship that prioritizes the supervisee’s growth while avoiding dual relationships or personal disclosures beyond what is professionally necessary.
- Confidentiality Boundaries: Maintaining confidentiality of information shared during supervision, with exceptions as required by law or professional ethics.
- Communication Boundaries: Establishing clear guidelines for communication outside of supervision sessions, avoiding informal or personal contact unless appropriate.
- Physical Boundaries: Maintaining professional physical distance and appropriate demeanor.
For example, I clearly state at the beginning of each supervisory relationship my availability, the expected format and structure of sessions, and the limits of confidentiality. This fosters a trusting and productive professional relationship.
Q 27. How do you handle situations where a supervisee is resistant to feedback?
Resistance to feedback is common in supervisory relationships. My approach focuses on understanding the underlying reasons for the resistance and collaboratively working towards a more receptive environment. It is crucial to approach this with empathy and patience.
- Empathetic Inquiry: Instead of directly confronting the resistance, I start by exploring the supervisee’s perspective. Asking open-ended questions like, “I’ve noticed you seem hesitant about this feedback; can you tell me more about your perspective?” helps to understand their reaction.
- Reflective Practice: Encouraging self-reflection through prompting questions that allow the supervisee to consider their own practice and experience. This can foster insight into their resistance.
- Collaborative Problem-Solving: Shifting the focus from criticizing the supervisee to collaboratively problem-solving potential challenges. This collaborative approach transforms feedback into a joint process focused on growth.
- Reframing Feedback: Presenting feedback in a constructive and supportive manner, focusing on specific behaviors and their impact rather than making general or judgmental statements. Using “I” statements helps to avoid a confrontational tone.
- Adjusting Approach: If resistance persists, I might adjust my approach, perhaps using different methods of delivering feedback, or involving other professionals like a peer or mentor.
For example, if a supervisee consistently dismisses feedback on their communication style, I might provide specific examples of their communication and then engage them in a discussion about the impact of this style on client interactions and the therapeutic relationship. This allows them to see the feedback in action and understand the impact.
Key Topics to Learn for Clinical Supervision and Mentoring Interview
- Ethical Considerations in Supervision: Understanding boundaries, confidentiality, and duty of care within the supervisory relationship. Practical application: Role-playing scenarios involving ethical dilemmas.
- Models of Supervision: Familiarize yourself with various approaches (e.g., psychodynamic, cognitive-behavioral, integrative) and their strengths and limitations. Practical application: Comparing and contrasting different models and their suitability for diverse clinical situations.
- The Supervisory Process: Mastering the stages of supervision, from initial assessment to termination. Practical application: Developing a structured plan for a supervisory session, considering case conceptualization and goal setting.
- Feedback and Evaluation Techniques: Learning effective methods for providing constructive criticism and guidance, fostering self-reflection and professional growth in supervisees. Practical application: Practicing delivering feedback using the SBI (Situation, Behavior, Impact) model.
- Mentorship vs. Supervision: Understanding the key differences and how both contribute to professional development. Practical application: Identifying scenarios where mentorship would be more appropriate than supervision, and vice-versa.
- Legal and Regulatory Frameworks: Understanding relevant laws and regulations impacting clinical practice and supervision. Practical application: Analyzing case studies involving potential legal or ethical violations.
- Cultural Competence in Supervision: Recognizing and addressing the impact of culture and diversity on the supervisory relationship. Practical application: Developing culturally sensitive strategies for working with supervisees from diverse backgrounds.
- Burnout Prevention and Self-Care in Supervision: Recognizing the challenges of supervision and implementing strategies for maintaining well-being. Practical application: Identifying personal strategies for managing stress and preventing burnout in the supervisory role.
Next Steps
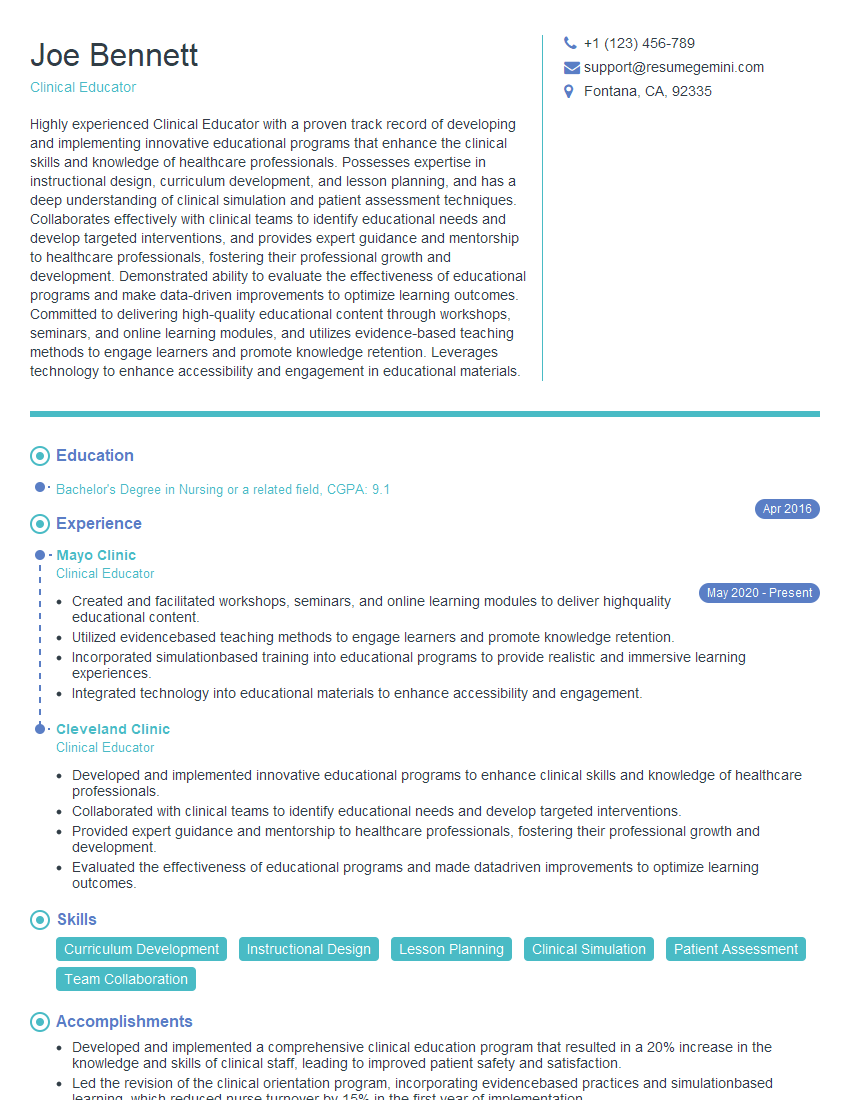
Mastering Clinical Supervision and Mentoring significantly enhances your career prospects, opening doors to leadership roles and advanced opportunities within your field. To maximize your chances of securing your dream position, a well-crafted, ATS-friendly resume is crucial. ResumeGemini is a trusted resource that can help you create a professional and impactful resume, tailored to highlight your skills and experience in Clinical Supervision and Mentoring. Examples of resumes tailored to this specialization are available to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO