Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Draw blood interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Draw blood Interview
Q 1. Describe the proper procedure for venipuncture.
Venipuncture, or drawing blood, is a common procedure requiring precision and adherence to safety protocols. It begins with proper patient identification and verification of the test request. Next, hand hygiene and donning appropriate personal protective equipment (PPE), including gloves, are crucial. Then, you select a suitable vein, typically in the antecubital fossa (the inner elbow area), observing for visible veins. Apply a tourniquet approximately 4-6 inches above the puncture site to distend the veins. After cleansing the area with an antiseptic, like isopropyl alcohol, allow it to air dry completely. Then, you anchor the vein, inserting the needle into the vein at a 15-30 degree angle, bevel up. Once you observe a flash of blood in the collection tube, you gently release the tourniquet and proceed with blood collection following the order of draw. After collection, remove the needle and apply pressure to the puncture site until bleeding stops, securing a bandage. Finally, properly dispose of all sharps and label the samples according to lab requirements.
Imagine threading a needle through a fabric – you need a steady hand and a clear view. Venipuncture requires similar precision and care to ensure accurate results and patient safety.
Q 2. What are the different types of blood collection tubes and their uses?
Different colored blood collection tubes contain various additives that preserve the blood sample for specific tests. For instance:
- Red top tubes (no additives) are used for serum tests.
- Lavender top tubes (EDTA) are used for complete blood counts (CBCs).
- Light blue top tubes (sodium citrate) are used for coagulation studies.
- Green top tubes (heparin) are used for plasma tests.
- Gray top tubes (sodium fluoride and potassium oxalate) are used for glucose testing.
The additives prevent clotting or maintain the integrity of certain blood components for analysis. Choosing the incorrect tube can compromise the reliability of test results, similar to using the wrong cooking utensil in a recipe.
Q 3. Explain the order of draw for blood collection tubes.
The order of draw is a critical step to avoid cross-contamination of additives between tubes. It ensures accurate and reliable lab results. The standard order is generally:
- Blood culture bottles
- Light blue (sodium citrate)
- Red (no additive) or Serum Separator Tubes (SST)
- Gold (SST)
- Green (heparin)
- Lavender (EDTA)
- Gray (sodium fluoride and potassium oxalate)
This sequence minimizes the risk of contamination, much like following a carefully planned baking recipe to avoid unintended flavors.
Q 4. How do you identify a patient correctly before drawing blood?
Patient identification is paramount to prevent medical errors. Before venipuncture, always check at least two identifiers, such as the patient’s full name and date of birth, and compare this with the requisition form. This verification process is non-negotiable to ensure the right patient receives the right test.
Imagine giving a medicine to the wrong person – the consequences could be disastrous. Patient identification in phlebotomy is equally critical for patient safety.
Q 5. What are the potential complications of venipuncture?
Potential complications of venipuncture include hematoma (bruising), vasovagal reaction (fainting), infection, nerve damage, and thrombophlebitis (inflammation of the vein). These complications are rare when the procedure is performed correctly but must be addressed if they occur.
Just like any medical procedure, potential risks are minimal with proper technique and precautions.
Q 6. How do you handle a difficult or challenging vein?
Difficult veins require patience and skill. Strategies include: using a smaller gauge needle, warming the area to dilate veins, applying a blood pressure cuff instead of a tourniquet, changing the patient’s position to encourage venous distension, and trying different venipuncture sites. If the vein is still inaccessible, it’s crucial to seek assistance from a colleague or supervisor rather than persisting and potentially causing harm.
Think of it like fishing – if you’re not getting a bite, you try a different lure, a different location, or even a different type of fish!
Q 7. What are the steps you take if you accidentally stick yourself with a needle?
Accidental needlesticks are a serious concern. Immediate action is crucial: remove gloves, wash the area thoroughly with soap and water for at least 30 seconds, report the incident immediately to a supervisor, and seek medical evaluation. Post-exposure prophylaxis (PEP) may be necessary depending on the circumstances.
Safety is always paramount in this profession and there are clear procedures in place for these types of incidents.
Q 8. How do you manage a patient who faints during a blood draw?
Patient fainting during a blood draw is a serious event requiring immediate action. The most important thing is to ensure patient safety. I would immediately remove the needle, apply pressure to the venipuncture site, and have the patient lie down, preferably with their legs elevated. This helps increase blood flow to the brain. I’d loosen any tight clothing around the neck and ensure the patient has adequate airflow.
Monitoring vital signs like pulse and respiration is crucial. I would continuously assess their condition and provide reassurance and comfort. Once the patient has recovered, I’d offer water and allow them ample time to rest before attempting another draw, if necessary. If the fainting is severe or prolonged, or if there are other concerning symptoms, I’d immediately call for medical assistance.
For instance, I once had a patient faint mid-draw. Following this protocol, the patient quickly recovered, and we were able to resume the procedure after a short delay. Always prioritize the patient’s safety and well-being; a second attempt can wait.
Q 9. Describe your experience with different venipuncture sites.
My experience encompasses a range of venipuncture sites. The most common is the antecubital fossa (the inner elbow area), specifically the median cubital vein, which is usually the easiest to access and has good vein size and stability. I also frequently utilize veins in the forearm (cephalic and basilic veins) as alternatives. Occasionally, I may use veins on the hand, especially in patients with difficult access in the arm, though these veins tend to be smaller and more prone to hematoma.
The selection of a venipuncture site depends on factors such as the patient’s vein condition, the required blood volume, and the patient’s overall comfort. I always assess the site before choosing, ensuring the vein is palpable, visible, and suitable for puncture. I also consider patient factors like age and previous venipunctures.
For example, in elderly patients with fragile veins, I would prioritize the forearm or antecubital fossa and avoid the hand veins to minimize the risk of complications.
Q 10. Explain the importance of proper antiseptic technique.
Proper antiseptic technique is paramount to prevent contamination and potential infection. It involves cleaning the venipuncture site with an appropriate antiseptic, such as isopropyl alcohol (70%), in a circular motion, starting from the center and moving outwards. The area should be allowed to air dry completely before inserting the needle; this is essential as alcohol can hemolyze (break down) red blood cells.
Using a sterile antiseptic and proper technique minimizes the risk of introducing pathogens into the bloodstream. Failure to do so could lead to localized infections or more severe bloodstream infections (bacteremia or septicemia). The Centers for Disease Control (CDC) provides detailed guidelines on proper antiseptic techniques, and adherence to these guidelines is non-negotiable.
In practice, this means paying meticulous attention to detail. I always ensure my hands are clean before starting the procedure, and I avoid touching the cleaned area after preparing it. Thorough antiseptic application is a habit I never compromise.
Q 11. How do you ensure the integrity of the collected blood sample?
Ensuring the integrity of the collected blood sample is crucial for accurate and reliable laboratory results. This starts with selecting the appropriate collection tubes based on the required tests. Each tube has specific additives (anticoagulants, clot activators) which must be mixed correctly after collection to prevent clotting or other alterations to the sample. Proper filling of the tubes is also critical, avoiding underfilling which can compromise test results or overfilling which may cause leakage or hemolysis.
Gentle inversion of tubes after collection helps to ensure proper mixing of additives. Samples should be transported and stored according to laboratory instructions, usually at a specific temperature to maintain stability. Proper labeling with patient identifiers (name, date of birth, date and time of collection) is essential to avoid mix-ups and ensure the patient’s safety.
For example, if a tube is underfilled, the ratio of blood to additive might be incorrect, which can lead to inaccurate results. Similarly, rough handling can lead to hemolysis, compromising many tests. Careful attention to these details guarantees sample integrity.
Q 12. What do you do if you have difficulty locating a vein?
Difficulty locating a vein can be frustrating for both the phlebotomist and the patient. My approach involves a systematic assessment. First, I would ensure the patient is properly hydrated and relaxed. Dehydration can make veins more difficult to palpate. I would then carefully palpate (feel for) the vein using my index and middle fingers, applying gentle pressure to see if it fills and then rolls under my fingers, indicating a healthy vein.
Applying a warm compress (heat) to the area can help dilate the veins, making them more visible and accessible. I may try different positions for the patient’s arm, such as lowering it or slightly elevating it. In some cases, using a tourniquet helps make the veins more prominent. If all of these fail, I would seek assistance from a colleague or refer the patient to a more experienced phlebotomist.
It’s important to avoid multiple attempts in the same area to prevent hematoma formation and patient discomfort. In some cases, ultrasound guidance may be necessary to locate a hidden vein.
Q 13. How do you handle a patient with fragile veins?
Patients with fragile veins require a delicate and careful approach. Smaller gauge needles (e.g., 23-gauge or even 25-gauge) are preferred to minimize trauma to the vein walls. Applying minimal pressure during the venipuncture procedure is important, as is avoiding repeated attempts in the same location. The tourniquet shouldn’t be too tight or left on for too long.
I would choose a vein that appears strong and well-supported and avoid rolling veins or those that feel very superficial or fragile. Gentle insertion of the needle, at a shallow angle, is crucial to prevent the vein from collapsing. Post-venipuncture, I would apply sustained pressure to the site for a longer duration to prevent hematoma formation.
In some cases, a smaller volume of blood may need to be collected to prevent further vein trauma. Patient communication and reassurance are key here to ease any anxiety they may have.
Q 14. Explain the proper disposal of used needles and other sharps.
Proper disposal of used needles and other sharps is a critical aspect of infection control and safety. Immediately after use, needles should never be recapped. They should be disposed of directly into a designated sharps container; these containers are puncture-resistant and designed to prevent accidental needle sticks. The sharps container should be clearly labeled and placed in a readily accessible location.
The container should be replaced when it’s approximately two-thirds full, according to facility policy. This prevents overfilling and accidental spills or needle sticks. Once full, the container should be disposed of according to local regulations, typically involving a designated medical waste disposal service.
Never attempt to reuse needles or improperly dispose of them in regular trash. This is a serious safety hazard for healthcare workers and anyone handling the waste. Adherence to these procedures is crucial for maintaining a safe working environment and preventing the spread of infectious diseases.
Q 15. What are the signs and symptoms of hematoma formation?
Hematoma formation, or the collection of blood outside blood vessels, after a venipuncture, presents with a range of signs and symptoms. Initially, you might see a small bump or swelling at the puncture site. This can be accompanied by localized pain, tenderness, and discoloration of the skin, ranging from a light bruise (red or purple) to a larger, darker bluish hue as the blood pools. In more severe cases, the hematoma can be quite large, causing significant discomfort and potentially restricting movement. The size and severity of the hematoma depend on factors like the size of the blood vessel injured, the patient’s coagulation status, and the amount of bleeding.
For example, a small, barely noticeable hematoma might resolve on its own within a few days. Conversely, a large hematoma could take weeks to heal completely and may even require medical intervention. It’s important to note that a small amount of bruising is often expected after venipuncture, but anything larger or causing significant pain should be documented and monitored.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you prevent hematoma formation during venipuncture?
Preventing hematoma formation is a crucial aspect of safe venipuncture. The key is to minimize trauma to the vessel and surrounding tissues. This starts with careful site selection – opting for veins that are easily accessible and robust enough to withstand needle insertion. Applying proper pressure to the puncture site immediately after needle removal is paramount. The pressure should be consistent and direct, preventing blood leakage from the puncture site for at least 5-10 minutes, or longer if needed. Using appropriate gauge needles also plays a significant role; smaller gauge needles (e.g., 21-23 gauge) generally cause less trauma.
Another vital step is to ensure the needle is inserted smoothly and at the correct angle, avoiding multiple punctures or deep insertion. If a patient has a bleeding disorder or is on anticoagulant medications, extra care is needed, potentially requiring longer compression or the use of a pressure bandage. Finally, avoiding bending the arm or the area immediately after the procedure helps minimize pressure on the site and the possibility of causing bleeding.
Q 17. What are the safety precautions you take during venipuncture?
Safety during venipuncture is paramount, encompassing several crucial precautions. First, always follow proper hand hygiene protocols, including thorough handwashing or the use of an alcohol-based hand rub. Next, ensuring proper patient identification is non-negotiable, preventing errors. This involves checking the patient’s identification band against the requisition form before proceeding. Selecting the appropriate equipment, including sterile needles and collection tubes, is also critical to minimize the risk of infection.
Throughout the procedure, maintaining aseptic technique is crucial. The use of alcohol swabs to disinfect the puncture site before venipuncture eliminates microorganisms and reduces the risk of infection. Proper disposal of sharps and used materials is also essential, complying with infection control guidelines. After venipuncture, appropriate disposal of needles and other potentially infectious materials into puncture resistant containers is crucial to preventing accidental needlesticks and ensuring environmental safety.
Q 18. How do you handle patient anxiety or fear during a blood draw?
Addressing patient anxiety and fear during a blood draw is essential for a positive patient experience and a successful procedure. First, I establish a calm and reassuring demeanor. A gentle and friendly approach can go a long way. I clearly explain the procedure in simple, easy-to-understand terms, answering any questions the patient may have. Distraction techniques, such as engaging the patient in casual conversation or offering them something to hold, can help alleviate anxiety. I might offer them a choice of positions to increase their comfort and provide reassurance throughout the process.
For example, some patients find it helpful to look away or have someone hold their hand during the procedure. If a patient is still exhibiting significant anxiety, I may consult with the nursing staff or physician, particularly if the patient has a history of vasovagal reactions. In such cases, alternative strategies such as lying down or pre-medicating the patient might be considered.
Q 19. Describe your experience with different blood collection devices.
My experience encompasses a wide range of blood collection devices. I’m proficient with various needle gauges, from smaller gauges for delicate veins to larger ones for blood draws requiring larger volumes. I’m familiar with different types of evacuated tube systems, including those used for various tests, such as serum, plasma, and whole blood collection. I’m also experienced in using winged infusion sets (butterfly needles) for difficult venipunctures, particularly on patients with fragile or superficial veins.
Furthermore, I’ve worked with various safety-engineered devices designed to minimize needlestick injuries, such as retractable needles and needle safety holders. My experience also extends to working with syringe-based systems, which are sometimes preferred for certain blood tests or for patients with specific needs. I am comfortable using different types of tourniquets, ensuring their appropriate placement to facilitate vein visualization without causing discomfort.
Q 20. What are the legal and ethical considerations of phlebotomy?
Phlebotomy carries significant legal and ethical considerations. Legally, we must adhere to all relevant regulations and maintain accurate documentation of all procedures. Patient consent is crucial; we must ensure patients understand the procedure and its risks before proceeding. Improper techniques or breaches in patient confidentiality can result in legal repercussions. Ethically, we must uphold patient autonomy, respecting their right to refuse treatment.
Maintaining patient dignity and confidentiality is paramount, alongside ensuring the safe and accurate collection of samples. We must avoid shortcuts that might compromise the integrity of the test results. A significant ethical dilemma could arise if a patient refuses consent but the requested tests are time-sensitive and potentially life-saving. In such situations, it’s crucial to understand the reasons for refusal and, if possible, work collaboratively to reach a solution. Maintaining accurate records, reporting any incidents immediately, and adhering to professional codes of conduct are all essential components of ethical phlebotomy.
Q 21. How do you maintain patient confidentiality?
Maintaining patient confidentiality is a cornerstone of my practice and a legal obligation. I never discuss a patient’s medical information with anyone other than authorized personnel directly involved in their care. I strictly adhere to HIPAA (Health Insurance Portability and Accountability Act) regulations and any local or institutional policies. Patient information, including test results and any other details associated with the blood draw, is only accessible to authorized personnel.
Any discussions relating to the patient’s condition or the purpose of their blood draw are only held in private settings or through secure communication channels to prevent unauthorized access. I ensure that all documentation and electronic records are handled securely, using password-protected systems and following established protocols for data storage and disposal. During the procedure itself, I avoid discussing the patient’s details with others, and I only disclose relevant information to the authorized personnel responsible for receiving the sample.
Q 22. How do you handle a situation where a patient refuses a blood draw?
Respecting patient autonomy is paramount. If a patient refuses a blood draw, my first step is to calmly and empathetically inquire about their concerns. I’d explain the procedure clearly, addressing any misconceptions or anxieties they might have. For example, if they’re afraid of needles, I might explain the various techniques to minimize discomfort, such as using smaller needles or applying numbing cream (if approved by a physician). I’d also explain the importance of the test and its potential impact on their health. If, after this discussion, the refusal persists, I meticulously document the refusal, including the reason provided by the patient, in their medical record. It’s crucial to ensure the patient understands their right to refuse treatment and that this refusal is respected without judgment. I then inform the appropriate medical personnel – the physician or nurse – about the situation so they can determine the next course of action.
Q 23. Describe your experience with blood culture collection.
Blood culture collection requires meticulous aseptic technique to prevent contamination. My experience involves collecting blood samples using a chlorhexidine or povidone-iodine skin antiseptic, following strict guidelines for site preparation. I use a vacutainer system with appropriate culture bottles, ensuring the order of collection is adhered to (aerobic bottle first, then anaerobic). It’s crucial to avoid touching the collection site after disinfection. During collection, I maintain careful observation for hemolysis and ensure proper blood volume is obtained in each bottle, avoiding under or overfilling. Post-collection, proper labeling and immediate transport to the lab are essential for accurate results. I’ve handled numerous blood cultures, and I meticulously follow all infection control protocols to ensure accuracy and prevent false-positive results. For example, I’ve encountered situations where a patient’s skin wasn’t properly cleansed, resulting in contamination – learning from those experiences underscores the importance of meticulous preparation and technique.
Q 24. Explain the process of labeling and handling blood samples.
Accurate labeling is critical to prevent errors. Immediately after drawing blood, I label each tube with the patient’s full name, unique medical record number (MRN), date, time of collection, and my initials. The label must be affixed directly to the tube, never relying on requisitions slips or separate labels. This is to prevent mixing up the sample and errors in identification. All information must be legible and permanent. Different tube types have different handling requirements, such as those for serum vs. plasma. Serum tubes are allowed to clot before centrifugation, while plasma tubes contain anticoagulants and are processed immediately after collection to prevent clotting. Tubes must be handled gently to avoid hemolysis, which can compromise test results. After labeling, tubes are transported to the lab promptly and stored appropriately according to lab protocols. For example, if a sample requires refrigeration, it’s immediately placed in a cool container to maintain its integrity.
Q 25. What are the quality control measures you follow in phlebotomy?
Quality control is at the heart of accurate phlebotomy. This begins with ensuring proper equipment is used; checking expiration dates on collection tubes and needles is mandatory. Before each venipuncture, I verify patient identification using two identifiers, such as name and date of birth, to prevent sample mix-ups. I regularly check the vacuum in the tubes to ensure they’re working correctly. If the tube doesn’t fill properly, I try an alternate tube or site. I also meticulously document any issues encountered during collection – for instance, if a patient experiences complications such as hematoma formation. I maintain proficiency through continuing education, ensuring my skills stay current and in line with best practices. Regular internal audits and external proficiency testing programs confirm the accuracy and reliability of our phlebotomy procedures. Think of it like a baker always checking their oven temperature – consistent quality control ensures accurate and reliable results.
Q 26. How do you troubleshoot common issues encountered during venipuncture?
Troubleshooting is a regular part of the job. If I can’t find a vein, I might try different sites, use a smaller needle, apply a warm compress, or use a vein finder device. If there is difficulty with blood flow, I can try a different angle with the needle, ensuring it’s fully inserted into the vein. If I encounter excessive bleeding after the draw, I apply pressure to the site for an adequate time. If a hematoma forms, I immediately document it and inform the appropriate medical personnel. Hemolysis, the breakdown of red blood cells, can be caused by forceful aspiration or using a small needle for a large volume collection. Therefore, I use the appropriate sized needle and gentle suction. Each complication requires a different approach – but careful observation, thorough documentation, and the ability to adapt to unexpected situations are crucial for resolving these issues.
Q 27. Describe your experience with point-of-care testing (POCT).
My experience with point-of-care testing (POCT) includes performing glucose monitoring using glucometers. I’ve received training on proper device calibration and quality control procedures to ensure the accuracy of these rapid tests. The process involves collecting a small blood sample using a lancet, applying the sample to the test strip, and interpreting the results displayed on the meter. I’m aware of the limitations of POCT—these tests offer rapid results, but they may not always be as precise as lab-based tests. This information is critical for interpreting and reporting the results and communicating them effectively to the medical team. Strict adherence to quality control measures is imperative for maintaining the reliability of POCT results in clinical decision-making.
Q 28. What are your strategies for continuous improvement in your phlebotomy skills?
Continuous improvement is a priority. I regularly participate in continuing education programs to stay updated on the latest phlebotomy techniques and best practices. I actively seek feedback from colleagues and supervisors and use this feedback to refine my skills and techniques. I also review my own performance regularly, identifying areas for improvement. I’m always looking for new technologies and methods to improve efficiency and patient comfort, such as the use of vein finders. In addition, I’m committed to adhering to all safety protocols and maintaining a clean and organized work environment. This systematic approach to self-improvement ensures that I’m constantly refining my skills and maintaining the highest standards of quality in my phlebotomy practice. Think of it as a musician always practicing to hone their skills – constant learning and refinement are key to mastery.
Key Topics to Learn for Blood Draw Interview
- Patient Interaction and Communication: Mastering effective communication techniques to build rapport with patients, addressing anxieties, and obtaining informed consent.
- Venipuncture Techniques: Developing proficiency in various venipuncture methods (e.g., vacuum tube, syringe), understanding vein selection, and proper needle insertion techniques.
- Anatomy and Physiology of the Circulatory System: A solid understanding of vein location, blood flow, and potential complications related to blood draws.
- Infection Control and Safety Procedures: Thorough knowledge of universal precautions, aseptic techniques, and proper disposal of sharps and biohazardous materials.
- Specimen Handling and Processing: Understanding proper labeling, handling, storage, and transportation of blood samples to ensure accurate test results.
- Troubleshooting and Problem-solving: Developing the ability to identify and address common issues encountered during blood draws, such as difficult veins or hematoma formation.
- Medical Terminology and Abbreviations: Familiarity with common medical terminology and abbreviations used in phlebotomy and laboratory settings.
- Legal and Ethical Considerations: Understanding patient confidentiality, HIPAA regulations, and professional conduct in a healthcare setting.
- Equipment Operation and Maintenance: Proficiency in using and maintaining phlebotomy equipment, including vacutainers, tourniquets, and safety needles.
- Quality Control and Assurance: Understanding the importance of accurate procedures and adherence to protocols to ensure reliable test results.
Next Steps
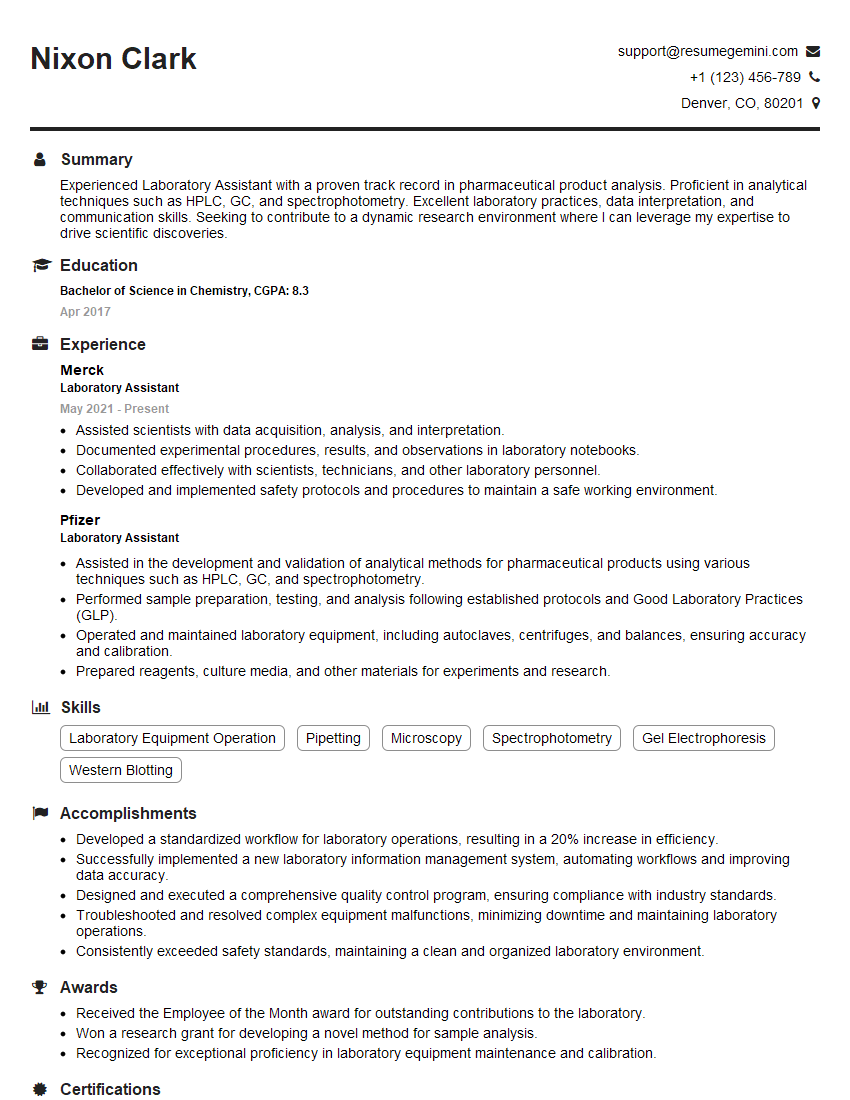
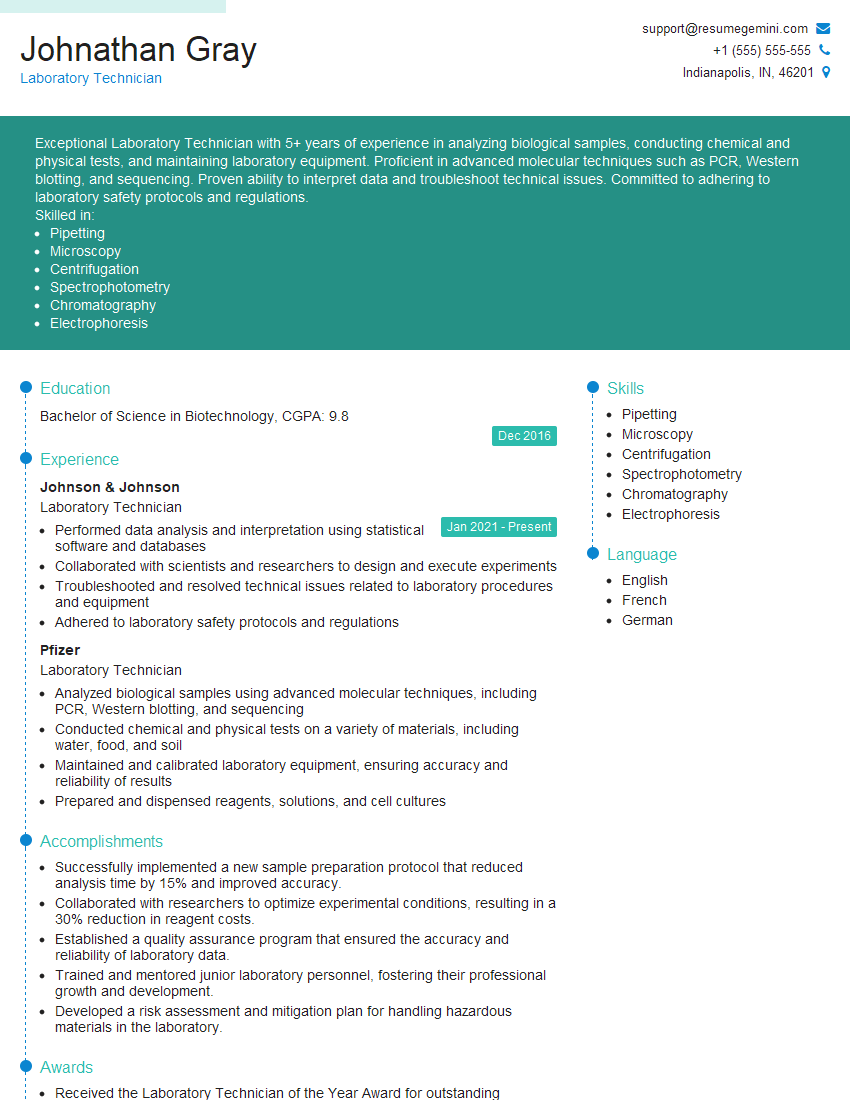
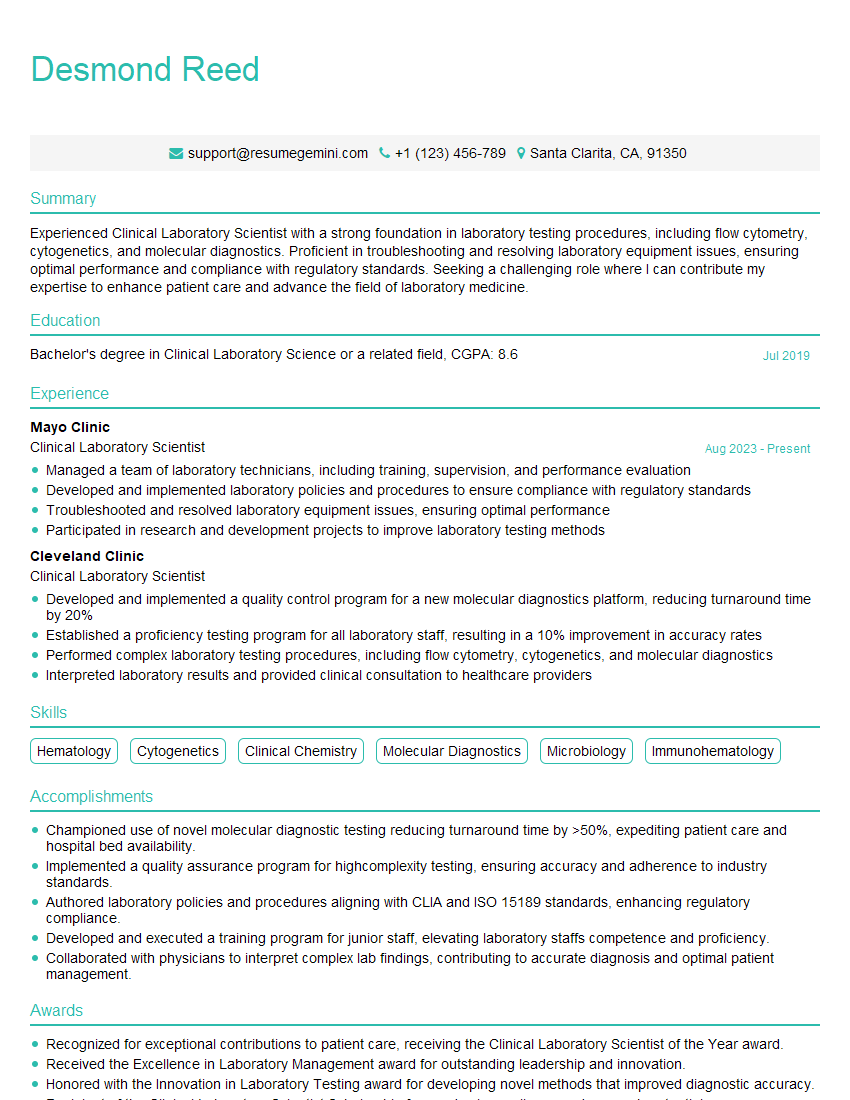
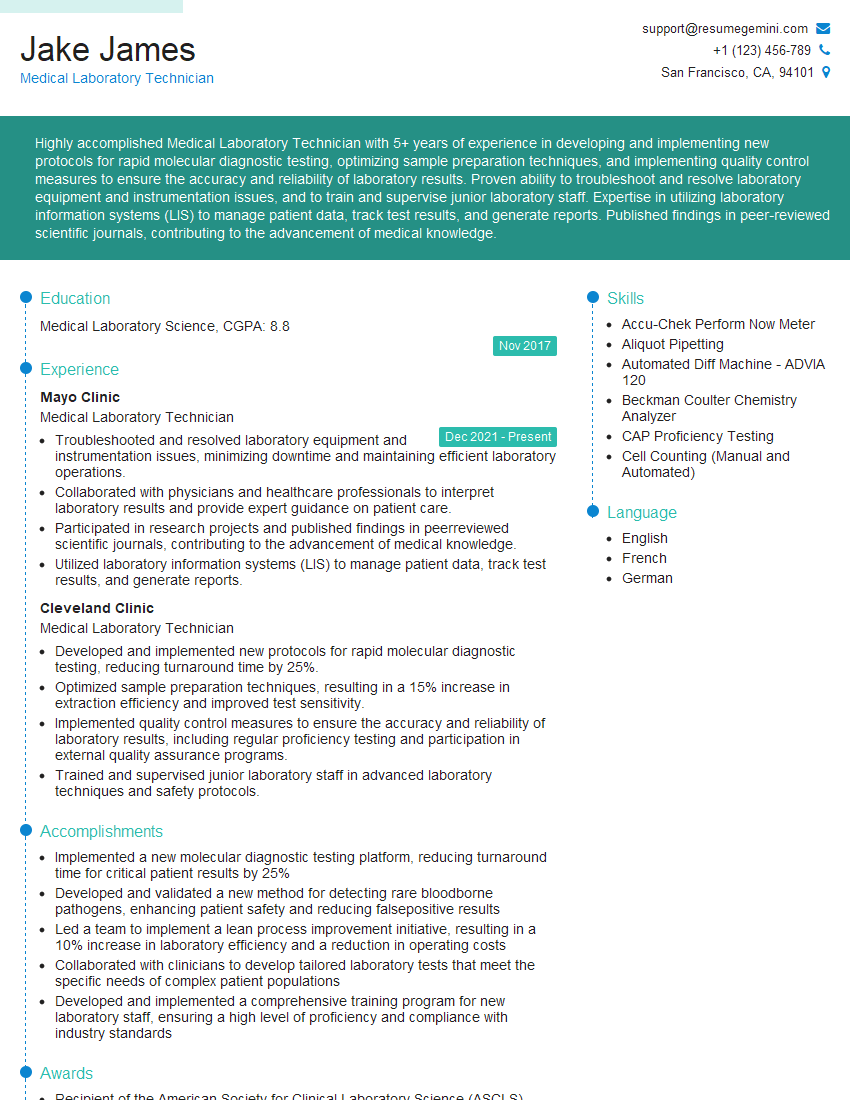
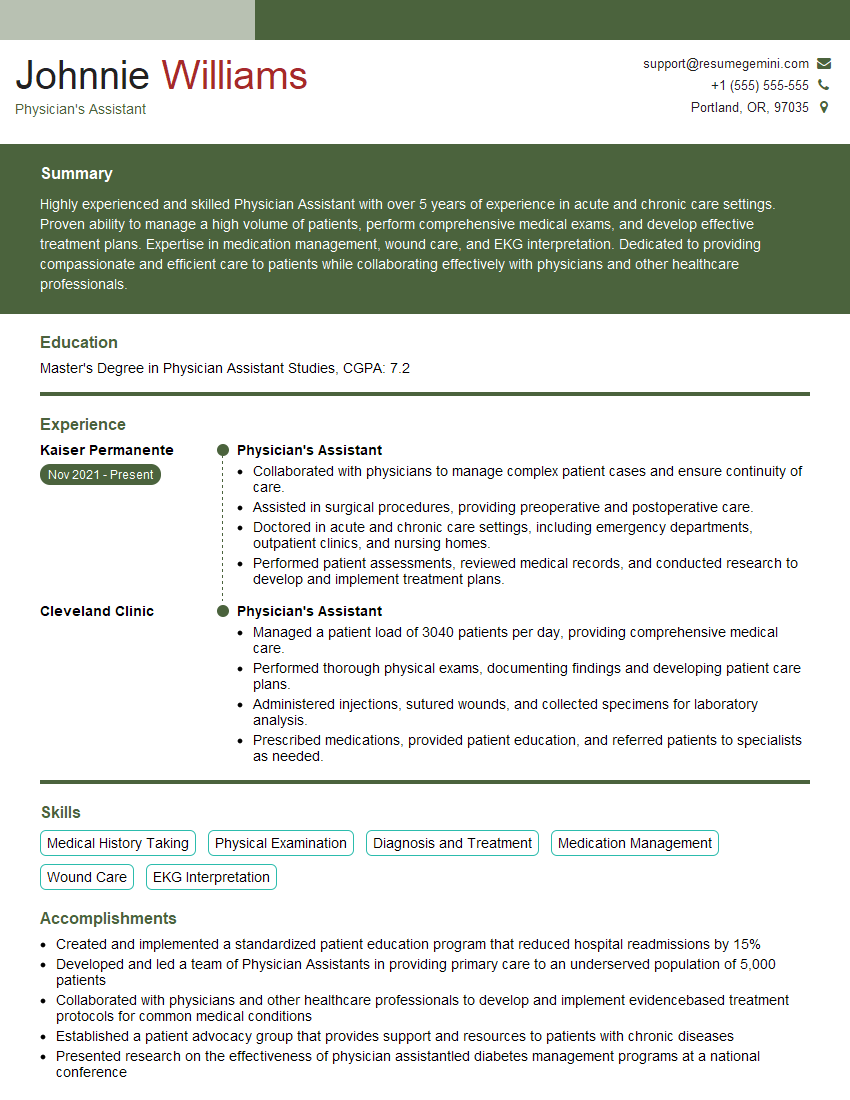
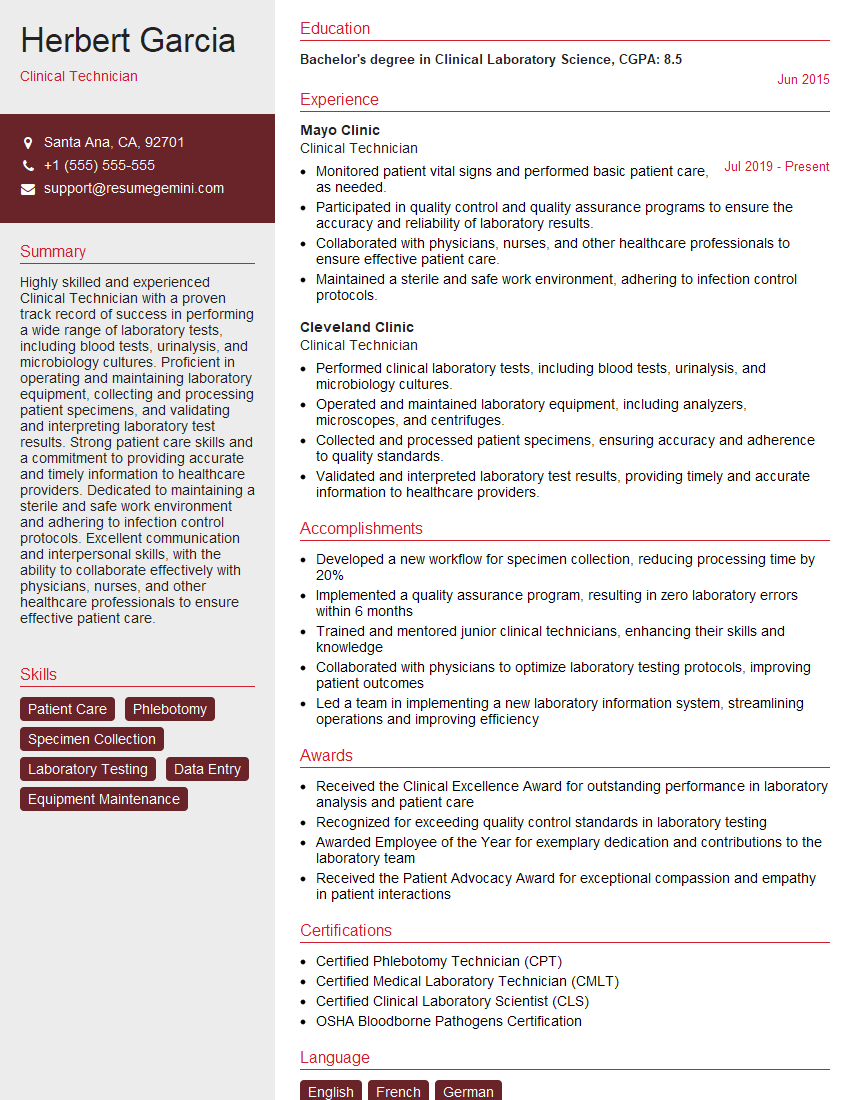
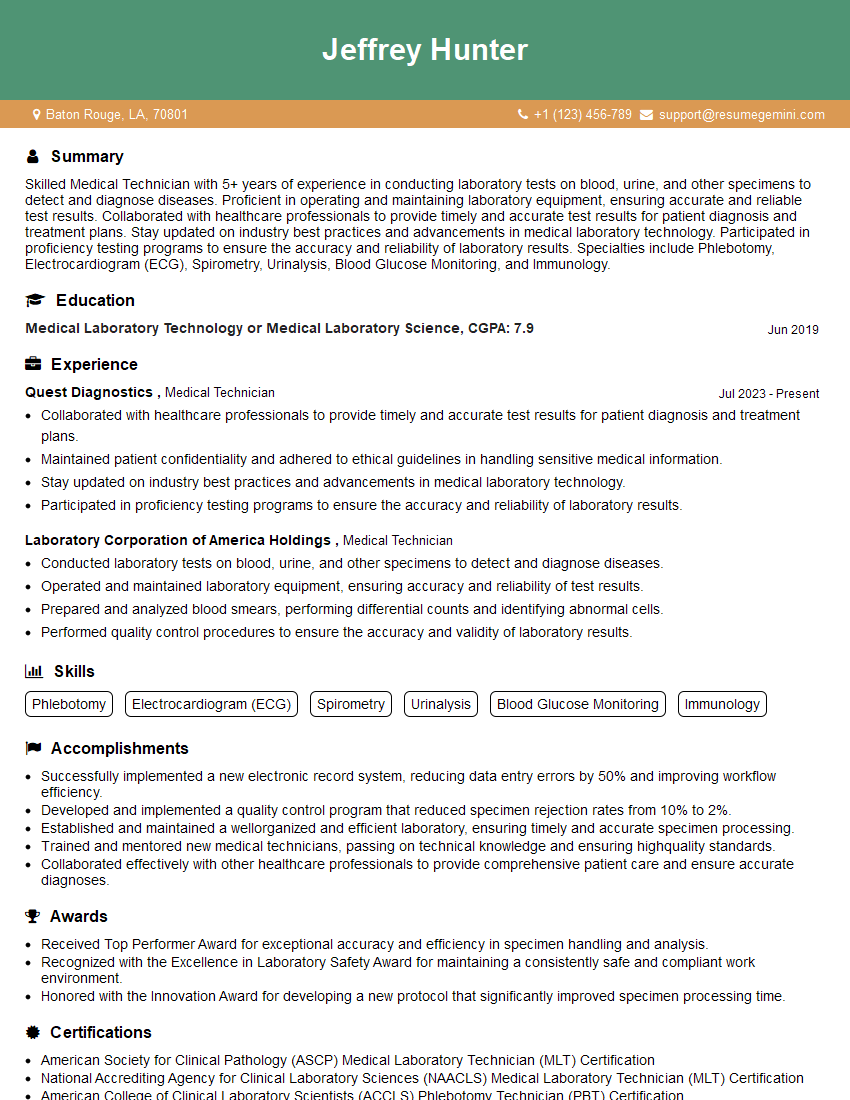
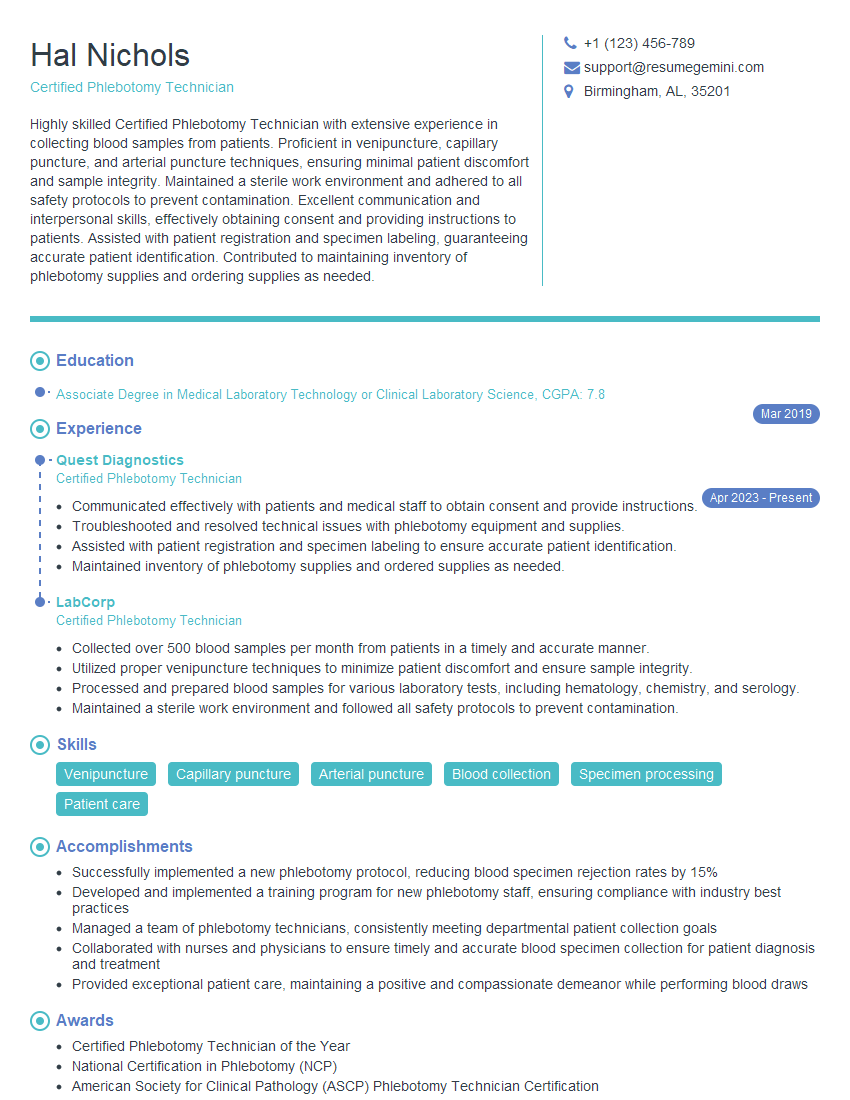
Mastering blood draw techniques is crucial for a successful career in healthcare, opening doors to diverse roles and advancement opportunities. A strong, ATS-friendly resume is essential to highlight your skills and experience to potential employers. To significantly improve your chances, leverage ResumeGemini to craft a compelling and effective resume. ResumeGemini provides tools and resources to create a professional document that showcases your qualifications. Examples of resumes tailored to blood draw positions are available to guide your creation process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO