Interviews are more than just a Q&A session—they’re a chance to prove your worth. This blog dives into essential First Aid and Medical Care interview questions and expert tips to help you align your answers with what hiring managers are looking for. Start preparing to shine!
Questions Asked in First Aid and Medical Care Interview
Q 1. Describe the steps involved in performing CPR on an adult.
Performing CPR (Cardiopulmonary Resuscitation) on an adult is a life-saving technique used when someone stops breathing or their heart stops beating. It involves chest compressions and rescue breaths to circulate blood and oxygen.
- Check for responsiveness: Gently shake the person and shout, “Are you okay?” If there’s no response, call for emergency medical services (EMS).
- Call for help: Dial your local emergency number (e.g., 911 in the US).
- Check for breathing: Look, listen, and feel for normal breathing for no more than 10 seconds. If there’s no normal breathing or only gasping breaths, begin CPR.
- Chest compressions: Position yourself with your hands interlocked in the center of the chest, just below the nipple line. Push hard and fast, at a rate of 100-120 compressions per minute, allowing the chest to fully recoil after each compression. The depth of compressions should be at least 2 inches.
- Rescue breaths (optional, if trained): After 30 compressions, give two rescue breaths, each lasting about one second. Ensure a good seal around the mouth.
- Continue CPR: Repeat cycles of 30 compressions and two breaths until EMS arrives or the person shows signs of recovery.
Important Note: Hands-only CPR (chest compressions only) is also effective and can be performed if you are not trained in rescue breaths. However, if trained in both chest compressions and rescue breaths, it’s vital to perform both.
Q 2. How do you assess a patient’s airway, breathing, and circulation (ABCs)?
Assessing a patient’s Airway, Breathing, and Circulation (ABCs) is the first step in any emergency situation. It helps determine the severity of the problem and guides your immediate actions.
- Airway: Check if the airway is open and clear. Look for obstructions like vomit, blood, or a foreign object. If necessary, gently tilt the head back and lift the chin (head-tilt-chin-lift maneuver) to open the airway. If a neck injury is suspected, use the jaw-thrust maneuver instead.
- Breathing: Look for chest rise and fall, listen for breath sounds, and feel for breath on your cheek. Check for the presence and quality of breathing (rate, depth, and ease of breathing). If breathing is absent or inadequate, begin rescue breathing or CPR.
- Circulation: Assess the pulse, usually at the carotid artery (neck) or femoral artery (groin). Check for skin color (pale, blue, or flushed) and temperature (cold, clammy). If there’s no pulse, begin CPR immediately.
Remember: The order of ABCs can be adapted in some situations. For instance, severe bleeding might take priority (C-A-B).
Q 3. Explain the difference between stable and unstable side lying positions.
The side-lying recovery position is used to help maintain an open airway and prevent choking in an unconscious but breathing person. The difference between stable and unstable side-lying positions lies in the level of support and the patient’s condition.
Stable Side-Lying Position: This is used for a patient who is unconscious but breathing normally and without any immediate life-threatening injuries. The patient is carefully rolled onto their side, supporting their head and neck to prevent the tongue from obstructing the airway. A pillow or rolled-up clothing can be used for extra support.
Unstable Side-Lying Position: This is generally avoided. It might be used temporarily if a patient is unstable, with severe injuries or compromised breathing, while awaiting advanced medical attention. However, maintaining an open airway is the priority. This position will only be used until definitive care can be provided.
Q 4. What are the signs and symptoms of a stroke?
A stroke occurs when blood supply to the brain is interrupted, causing brain cells to die. Recognizing the signs and symptoms is crucial for timely intervention.
- Facial drooping: Ask the person to smile. Does one side of the face droop?
- Arm weakness: Ask the person to raise both arms. Does one arm drift downward?
- Speech difficulty: Ask the person to repeat a simple sentence. Is their speech slurred or strange?
- Sudden severe headache: A sudden, intense headache with no known cause can be a sign of stroke.
- Confusion: Difficulty understanding or speaking clearly.
- Loss of balance or coordination: Difficulty walking or maintaining balance.
- Vision changes: Blurred vision or sudden loss of vision in one or both eyes.
If you suspect a stroke, call emergency services immediately. Time is brain; the faster treatment is received, the better the chances of recovery.
Q 5. How would you manage a patient experiencing a severe allergic reaction (anaphylaxis)?
Anaphylaxis is a severe, life-threatening allergic reaction. Immediate action is crucial.
- Call emergency services immediately: This is the most important step.
- Administer epinephrine (adrenaline) if the person has an EpiPen or similar auto-injector: Follow the instructions on the auto-injector carefully. Inject into the outer thigh.
- Maintain an open airway: If the person’s airway is compromised, start rescue breathing or CPR as needed.
- Monitor vital signs: Check breathing, pulse, and level of consciousness.
- Position the person comfortably: Help the person lie down and elevate their legs if possible.
- Remove any triggers: If known, remove the allergen from contact with the skin or the environment.
- Stay with the person until medical help arrives: Monitor for worsening symptoms and provide reassurance.
Anaphylaxis requires immediate medical attention. Epinephrine is a crucial treatment and delays can be life-threatening. After administering epinephrine, continued monitoring is crucial.
Q 6. Describe the proper procedure for controlling external bleeding.
Controlling external bleeding involves several steps to minimize blood loss and prevent infection.
- Direct pressure: Apply firm, direct pressure to the wound using a clean cloth. Elevate the injured limb above the heart if possible.
- Do not remove any objects embedded in the wound: This could cause further bleeding and damage.
- Maintain pressure for at least 15-20 minutes: Even if the bleeding stops, maintain pressure for at least this amount of time to help ensure clotting.
- If bleeding continues, consider additional measures: You might need to apply a tourniquet as a last resort, but only if direct pressure fails and the bleeding is severe and life-threatening.
- Seek medical attention: External bleeding, especially if profuse, warrants immediate medical care.
Proper wound care is essential after the bleeding stops. The wound should be cleaned and covered with a sterile dressing to prevent infection. Seek professional medical care for deep wounds, wounds involving significant bleeding, or wounds that show signs of infection.
Q 7. What are the steps in treating a suspected fracture?
Suspected fractures require careful handling to prevent further injury. The primary goals are to immobilize the injured area, control pain, and prevent shock.
- Assess the scene: Ensure the scene is safe before approaching the injured person.
- Check the ABCs: Assess the airway, breathing, and circulation.
- Immobilize the injured area: Use splints, slings, or other materials to keep the injured area from moving. Improvised splints can be made from readily available materials like rolled-up towels, blankets, or even cardboard. Do not attempt to realign the broken bone.
- Control pain and prevent shock: Keep the person warm, elevate the injured limb if appropriate, and offer comfort and reassurance.
- Seek medical attention: Transport the person to a hospital for proper evaluation and treatment.
Improper handling of a fracture can lead to nerve and blood vessel damage, increased pain, and delayed healing. Professional medical care is essential for proper diagnosis and treatment.
Q 8. How would you handle a patient with a suspected spinal injury?
Suspected spinal injuries are extremely serious and require immediate, careful attention. The primary goal is to prevent further damage to the spinal cord. This means minimizing movement of the neck and spine.
- Assessment: First, check for responsiveness and airway, breathing, and circulation (ABCs). Look for any obvious deformities, and gently assess for pain or tenderness along the spine.
- Stabilization: Do NOT move the patient unless absolutely necessary. If possible, keep the patient still in the position found. If the patient is not breathing, start rescue breathing, but avoid any neck or head movement. If possible, use a cervical collar and a long spine board to immobilize the spine before any movement.
- Manual Stabilization: While waiting for emergency medical services (EMS), manually stabilize the head and neck to prevent movement. This involves carefully supporting the head with your hands, keeping the neck in a neutral position. Avoid any sudden jerks or twists.
- Monitoring: Continuously monitor the patient’s ABCs, level of consciousness, and for any changes in their condition. Maintain the patient’s body temperature.
- Emergency Services: Call for EMS immediately. Provide clear and concise information about the injury and the patient’s condition to the dispatcher.
Example: Imagine you find a person unconscious after a car accident. Even if they appear to be breathing, you should assume a spinal injury until proven otherwise. You would call 911 immediately, maintain manual stabilization of the head and neck, and wait for professional help to arrive and safely move the patient.
Q 9. Explain the proper technique for splinting a limb.
Splinting a limb aims to immobilize it to prevent further injury and pain. Proper splinting technique involves several crucial steps. It’s important to remember to always check for circulation (feeling, warmth, and color) before and after splinting.
- Assessment: Before splinting, gently assess the injured area for open wounds, deformities, and the presence of pulses. Note the position of the injured limb.
- Padding: Place soft padding (such as rolled-up towels or blankets) around the injured area before applying the splint. This helps to prevent pressure sores and improve comfort.
- Splint Application: Secure the splint to the injured limb, ensuring it extends above and below the injury site. The splint should be snug but not constricting. If using a rigid splint, it should be carefully aligned along the length of the limb to avoid any awkward angles. For a flexible splint, such as a triangular bandage, gently wrap it around and firmly secure it to immobilize the joint.
- Securing the Splint: Use bandages, straps, or other securing materials to hold the splint in place. Ensure that the straps are applied snugly but not so tight that they cut off circulation. You should be able to fit a finger under each strap.
- Reassessment: After splinting, reassess the limb’s circulation, movement, and sensation (CMS) to ensure proper blood flow is maintained. If you notice any problems, loosen the straps slightly.
Example: Imagine someone has a fractured forearm. You would pad the area, apply a splint that extends from the elbow to the wrist, and secure it using bandages. You would then check the fingers for feeling, warmth, and color to ensure circulation is not compromised.
Q 10. Describe the different types of burns and their treatment.
Burns are classified by depth (how deep they penetrate the skin) and surface area (how much of the body is affected).
- First-degree burns (superficial): These affect only the epidermis (outer skin layer). They cause redness, pain, and mild swelling. Treatment involves cooling the burn under cool (not ice-cold) running water for 10-20 minutes and applying a sterile bandage. Over-the-counter pain relievers can help with discomfort. Examples are mild sunburns.
- Second-degree burns (partial-thickness): These extend into the dermis (second skin layer). They cause blisters, intense pain, swelling, and redness. Treatment involves cooling the burn, removing any jewelry or clothing not stuck to the skin, covering the burn with a clean, sterile dressing. Seek medical attention for larger burns.
- Third-degree burns (full-thickness): These destroy all layers of skin and often underlying tissues. The skin may appear charred, white, or leathery. There may be little to no pain because the nerve endings are destroyed. These require immediate medical attention as they frequently lead to complications. Treatment involves immediate emergency medical care and specialized wound management.
Treatment Principles for All Burns: Always cool the burn, avoid applying ice directly, remove any restrictive clothing or jewelry (unless stuck to the wound), cover with a clean, sterile dressing, and seek medical attention for moderate to severe burns.
Q 11. How would you treat a patient experiencing hypothermia?
Hypothermia is a dangerously low body temperature. The body loses heat faster than it can produce it. Treatment focuses on gently rewarming the body.
- Gentle Rewarming: Move the victim to a warm place. Remove any wet clothing and replace it with dry clothing or blankets.
- Insulation: Wrap the person in warm blankets, focusing on the core body temperature (chest and abdomen). Use external warming devices such as heat packs (avoid placing directly on skin) to prevent hypothermia and frostbite.
- Warm Drinks: Offer warm, non-alcoholic beverages (avoid caffeine and alcohol, which can worsen hypothermia). If conscious, provide warm sugar-sweetened drinks (sugar provides an energy source).
- Avoid Vigorous Activity: Avoid rubbing the extremities or engaging in vigorous activity. This can shock the system.
- Monitor and Seek Medical Attention: Monitor vital signs and call for medical assistance. Rewarming needs to be done slowly to prevent cardiac complications.
Example: A hiker gets lost in a blizzard and is found unconscious and shivering uncontrollably. You would carefully move the person to a warmer environment, remove wet clothing, wrap them in blankets, and seek immediate medical attention.
Q 12. How would you treat a patient experiencing heatstroke?
Heatstroke is a life-threatening condition resulting from the body’s inability to regulate its temperature. It’s a medical emergency requiring immediate intervention.
- Cool the Body: This is the most crucial step. Immerse the patient in cool water (if available), apply cool compresses to the neck, groin, and armpits, or fan the patient while spraying them with cool water.
- Remove Excess Clothing: Remove any unnecessary clothing to aid in cooling.
- Hydration: If conscious and able to swallow, offer sips of cool water. Avoid giving anything else by mouth.
- Monitor Vital Signs: Monitor the patient’s breathing and heart rate.
- Immediate Medical Attention: Heatstroke is a medical emergency. Call for immediate medical attention; transport the patient to the hospital as quickly as possible.
Example: An athlete collapses during a strenuous sporting event. They are flushed, sweaty and unresponsive. You would immediately start cooling them down by any available method and call 911.
Q 13. What are the signs and symptoms of diabetic shock?
Diabetic shock (hypoglycemic shock or insulin shock) occurs when blood sugar levels drop dangerously low.
- Symptoms: Signs include sudden weakness, sweating, confusion, shakiness, rapid heartbeat, anxiety, hunger, dizziness, and even loss of consciousness. Severe cases may lead to seizures or coma.
- Treatment: If the patient is conscious and can swallow, give them 15-20 grams of fast-acting carbohydrates, such as glucose tablets, hard candies, or sugary drinks (like juice or regular soda). Check their blood sugar levels again after 15 minutes. If the symptoms are not improving or if the person is unconscious, call emergency medical services immediately.
Important Note: Never give anything by mouth to an unconscious person. It’s important to always carry a quick-acting sugar source such as glucose tablets or juice, and know how to treat it.
Q 14. How would you manage a patient experiencing a seizure?
A seizure is a sudden surge of electrical activity in the brain. The treatment focuses on protecting the individual from harm and ensuring their safety.
- Safety: Protect the person from injury. Move any nearby objects that could cause harm. If the person is standing or sitting, gently guide them to the floor and protect their head. Do not restrain them.
- Positioning: Turn the person gently onto their side to help them breathe more easily and prevent choking. Keep their airway open.
- Monitoring: Time the seizure. Note the type of movements, if any.
- Post-Seizure Care: After the seizure stops, check their breathing and pulse. Monitor for any injuries. Once they regain consciousness, keep them lying down and provide comfort and support. Offer water or juice when able.
- Medical Attention: Call for emergency medical services if the seizure lasts longer than 5 minutes, if it’s the person’s first seizure, or if injuries occur during the seizure. They may require further assessment and medication.
Example: If someone starts having a seizure, your primary action would be to make sure the immediate environment is safe. Then, help them gently to the ground, protecting their head. Afterwards, you’d carefully monitor their breathing and call for emergency medical services if necessary.
Q 15. Describe your experience with wound care.
Wound care is a crucial aspect of first aid and encompasses a wide range of procedures, from cleaning minor abrasions to managing complex lacerations. My experience includes assessing wound depth, size, and contamination; selecting appropriate cleaning solutions, such as sterile saline or water; debriding (removing) any foreign bodies or dead tissue; and applying the correct dressings and bandages to promote healing and prevent infection. I’m proficient in techniques for managing different wound types, including puncture wounds, lacerations, avulsions, and burns. I’ve worked extensively with both simple and complex wound management, including suturing (although I’d only perform this within my scope of practice and when appropriate training and certification allow) and the application of advanced dressings like hydrocolloids and alginates. For example, I once treated a deep laceration sustained during a hiking accident, requiring meticulous cleaning, debridement, and the application of a pressure dressing to control bleeding before transport to a hospital.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the key considerations when providing first aid in a remote location?
Providing first aid in a remote location necessitates careful consideration of several factors. Firstly, limited resources are a major constraint. This means prioritizing available supplies and adapting techniques to work with whatever is at hand. Secondly, evacuation time plays a significant role in determining the treatment strategy. Life-threatening conditions require immediate attention and may involve improvising solutions before more advanced care becomes available. Thirdly, environmental hazards (e.g., extreme weather, wildlife) can complicate both assessment and treatment. Finally, communication limitations can hinder access to emergency services. This requires meticulous documentation and clear communication with any rescuers. For example, in a remote wilderness setting, I would prioritize immediate stabilization of any life-threatening injuries (like controlling severe bleeding or airway obstruction) before focusing on less urgent wounds, utilizing any available materials for splints or dressings.
Q 17. Explain your knowledge of different types of bandages and dressings.
Bandages and dressings serve distinct purposes in wound care. Dressings are placed directly on the wound to absorb exudate (fluid), protect the wound from further contamination, and promote healing. Different dressings cater to varying wound types and exudate levels. For instance, gauze pads are versatile and absorbent, while hydrocolloid dressings provide a moist environment for healing and are suitable for minor wounds. Alginates are highly absorbent and useful for heavily draining wounds. Bandages secure dressings in place, provide compression to control bleeding, and offer support to the injured area. Examples include elastic bandages (for compression), roller bandages (for securing dressings), and triangular bandages (for slings and pressure points). Choosing the correct combination of dressing and bandage is vital for optimal wound management. Think of it like this: the dressing is the protective layer directly on the wound, and the bandage is the support structure holding everything in place.
Q 18. What is your approach to patient assessment and triage?
Patient assessment and triage follow a systematic approach. I use the ABCDE method: Airway (ensure the airway is clear and open), Breathing (assess respiratory rate and effort), Circulation (check pulse, blood pressure, and capillary refill), Disability (assess neurological status), and Exposure (assess the patient’s entire body for injuries). This initial assessment helps identify life-threatening conditions. Triage prioritizes patients based on the severity of their injuries and their likelihood of survival with immediate intervention. I use a simple system: Immediate (requiring immediate life-saving interventions), Delayed (requiring treatment but not immediately life-threatening), Minimal (minor injuries), and Expectant (unlikely to survive even with treatment).
Q 19. How do you prioritize multiple patients in a mass casualty incident?
In a mass casualty incident (MCI), efficient triage is paramount. I utilize the START (Simple Triage and Rapid Treatment) method or a similar system. This involves rapidly assessing patients based on respiration, perfusion (capillary refill), and mental status. Patients are categorized into four groups: Immediate, Delayed, Minimal, and Expectant, as described previously. The goal is to quickly identify and prioritize those needing immediate life-saving interventions. The process involves moving through a designated area, tagging patients with appropriate indicators, and delegating tasks to other first responders based on the identified needs. Resources are allocated strategically to maximize the number of lives saved. For example, in a building collapse, I’d focus first on rescuing those who are critically injured but still salvageable, then progress to those with less severe injuries.
Q 20. How do you maintain proper infection control protocols?
Maintaining proper infection control is essential to prevent the spread of infectious diseases. This involves several key steps: Hand hygiene is the cornerstone, using soap and water or alcohol-based hand sanitizer before and after contact with patients. Use of personal protective equipment (PPE) such as gloves, masks, eye protection, and gowns, is crucial, especially when dealing with wounds or bodily fluids. Proper disposal of contaminated materials, including sharps, dressings, and other waste, follows strict protocols. Environmental cleaning and disinfection of surfaces and equipment are also necessary to maintain a safe environment. Each step is vital to minimizing the risk of cross-contamination between patients and healthcare workers. A failure to follow these procedures can lead to serious infections and outbreaks.
Q 21. Describe your experience using an AED (Automated External Defibrillator).
I am proficient in using an AED (Automated External Defibrillator). I have completed numerous training courses and have practical experience in deploying it in emergency situations. The process is straightforward: Turn on the AED, attach the pads to the patient’s chest, and follow the voice prompts. The device analyzes the heart rhythm and advises whether a shock is necessary. If indicated, the AED delivers the shock. CPR (cardiopulmonary resuscitation) is performed before and after the shock, as per current guidelines. Proper placement of the pads is critical to ensure effective delivery of the shock. It is essential to note that AED use is part of a broader chain of survival, which includes early recognition of cardiac arrest, immediate CPR, rapid defibrillation, and post-resuscitation care. I’ve had several successful uses of an AED in the past, and each experience has reinforced the importance of maintaining up-to-date training and knowledge of best practices.
Q 22. What are your limitations as a first aider?
As a first aider, my limitations are clearly defined by my training and scope of practice. I am not a medical professional; I cannot diagnose illnesses or injuries, prescribe medications, or perform procedures beyond my certified skill set. For instance, I can provide basic wound care, but I cannot surgically repair a deep laceration. I can administer basic life support (BLS), but I cannot intubate a patient or administer advanced cardiac life support (ACLS). My role is to stabilize the patient until professional medical help arrives, providing immediate care to address life-threatening situations. Any actions I take are aimed at preventing further harm and preserving life, not at definitive treatment. Recognizing my limitations is crucial to providing safe and effective first aid.
Think of it like this: I’m a skilled mechanic who can change a tire and jumpstart a car, but I can’t rebuild an engine. I know when to call for a tow truck (paramedics) – a specialized professional – for issues beyond my abilities.
Q 23. How do you stay updated on the latest first aid and medical care guidelines?
Staying current in first aid and medical care is paramount. I achieve this through a multi-pronged approach. Firstly, I regularly participate in continuing education courses and workshops offered by reputable organizations such as the American Red Cross or the American Heart Association. These courses cover updates to guidelines, new techniques, and advancements in emergency medical care. Secondly, I subscribe to professional journals and newsletters that publish the latest research and best practices in emergency medicine. This keeps me informed about evolving standards and any changes in recommended procedures. Finally, I actively participate in professional networks and online communities where first aiders and medical professionals share knowledge and discuss recent developments. This combination of formal training and continuous self-learning ensures I am always operating with the most up-to-date and evidence-based practices.
Q 24. Describe a time you had to make a quick, critical decision in a first aid scenario.
During a local marathon, I encountered a runner experiencing severe chest pain and shortness of breath, possibly a heart attack. Immediate action was critical. While waiting for paramedics, I assessed the situation, noting his pale complexion and rapid, weak pulse. I knew administering oxygen was vital, but also realized that putting him in a supine position could worsen his condition if he was indeed suffering a heart attack. I made the quick decision to keep him seated and slightly elevated, provided oxygen, and continuously monitored his vital signs, reassuring him and remaining calm until professional help arrived. This scenario highlighted the importance of rapidly assessing the situation, prioritizing life-threatening issues, and adapting my approach based on the patient’s specific needs.
Q 25. How would you handle a difficult or uncooperative patient?
Handling a difficult or uncooperative patient requires patience, empathy, and strong communication skills. I begin by calmly and respectfully attempting to understand the patient’s concerns. I would actively listen, ensuring they feel heard and respected, even if their behavior is challenging. If the patient is combative or disoriented, my priority shifts to safety – both mine and theirs. I would maintain a safe distance and seek assistance from law enforcement or other qualified personnel if necessary. My goal is always to provide the best possible care within the boundaries of safety and respecting their autonomy, even when that autonomy may seem to be hindering their care.
For instance, if a patient refuses treatment, I would clearly explain the potential risks and benefits of accepting or refusing care and then document their decision. I ensure to maintain a respectful and non-judgmental demeanor throughout the interaction.
Q 26. What safety measures do you take to protect yourself and the patient?
Patient and personal safety are top priorities. I always follow universal precautions, treating all bodily fluids as potentially infectious. This includes wearing appropriate personal protective equipment (PPE) such as gloves, eye protection, and a mask, as needed. Before any contact, I would assess the scene for hazards, ensuring the area is safe for both the patient and myself. If the environment is unsafe (e.g., traffic accident, active fire), I would prioritize moving the patient to a safer location before initiating treatment only if it doesn’t compromise their well-being. After providing care, proper disposal of contaminated materials is crucial to prevent the spread of infection. This includes the safe disposal of used PPE and any contaminated materials.
Q 27. How do you document a first aid incident?
Accurate documentation of a first aid incident is essential for legal and medical reasons. My documentation would include the date, time, and location of the incident, a detailed description of the injury or illness, actions taken to provide first aid, the patient’s response to treatment, and any significant observations made. I would also record the time emergency medical services (EMS) were contacted and any pertinent information relayed to them. The patient’s consent for treatment, if obtained, would also be documented. This record should be clear, concise, and objective, avoiding subjective interpretations. It’s crucial to use factual language and avoid making assumptions. Finally, I maintain a record of any training certifications or updated knowledge.
Q 28. Describe your understanding of legal and ethical responsibilities in first aid and medical care.
My understanding of legal and ethical responsibilities in first aid involves adhering to a strict code of conduct. Legally, I am obligated to act within the scope of my training and certification. Providing care beyond my competency could lead to legal repercussions. Ethically, I am bound by the principles of beneficence (acting in the best interest of the patient), non-maleficence (avoiding harm), autonomy (respecting the patient’s right to make decisions about their care), and justice (providing fair and equitable care). Maintaining confidentiality is also vital. I would only share patient information with authorized personnel, such as emergency medical services or other healthcare providers involved in their care. My actions are always guided by these legal and ethical frameworks to ensure responsible and ethical care is delivered.
Key Topics to Learn for Your First Aid and Medical Care Interview
Ace your interview by mastering these crucial areas of First Aid and Medical Care. Remember to focus on both the theoretical understanding and practical application of these concepts.
- Primary Assessment: Understanding and applying the ABCDE approach (Airway, Breathing, Circulation, Disability, Exposure) in various emergency scenarios. Practice explaining your decision-making process in prioritizing patient care.
- Trauma Management: Learn about managing different types of injuries, including bleeding control (direct pressure, tourniquets), fracture management (immobilization), and spinal injury assessment. Be ready to discuss practical techniques and the importance of scene safety.
- Medical Emergencies: Gain a solid understanding of responding to conditions like heart attacks, strokes, seizures, and diabetic emergencies. Focus on recognizing symptoms, initiating appropriate interventions (e.g., CPR, recovery position), and explaining the rationale behind your actions.
- Wound Care: Master the principles of wound cleaning, dressing, and bandaging. Be prepared to discuss different types of wounds and appropriate treatment methods. Understand infection prevention and control measures.
- Pediatric and Geriatric First Aid: Familiarize yourself with the unique challenges and considerations when providing first aid to children and older adults. This includes age-specific assessment and treatment techniques.
- Legal and Ethical Considerations: Understand the legal implications of providing first aid, including consent, confidentiality, and reporting requirements. Be prepared to discuss ethical dilemmas you might encounter.
- Teamwork and Communication: Highlight your ability to work effectively within a team, communicate clearly and concisely under pressure, and follow established protocols.
Next Steps: Launch Your First Aid and Medical Care Career
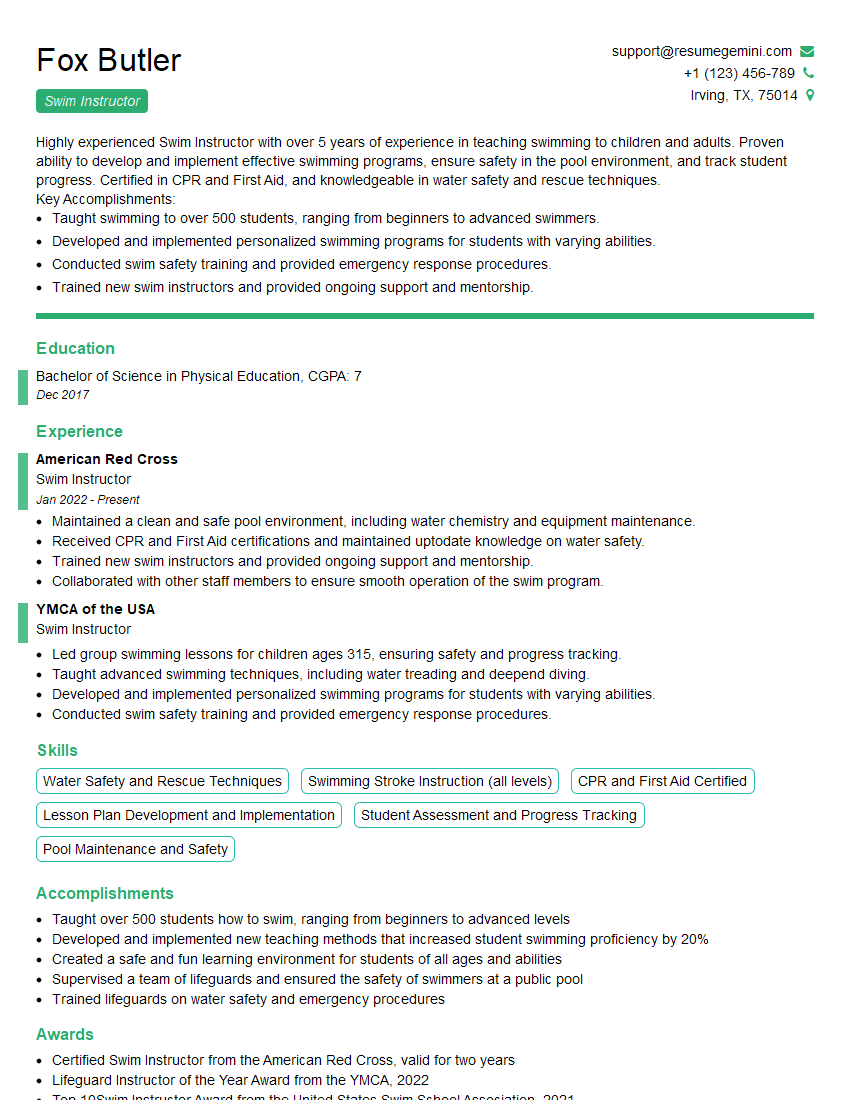
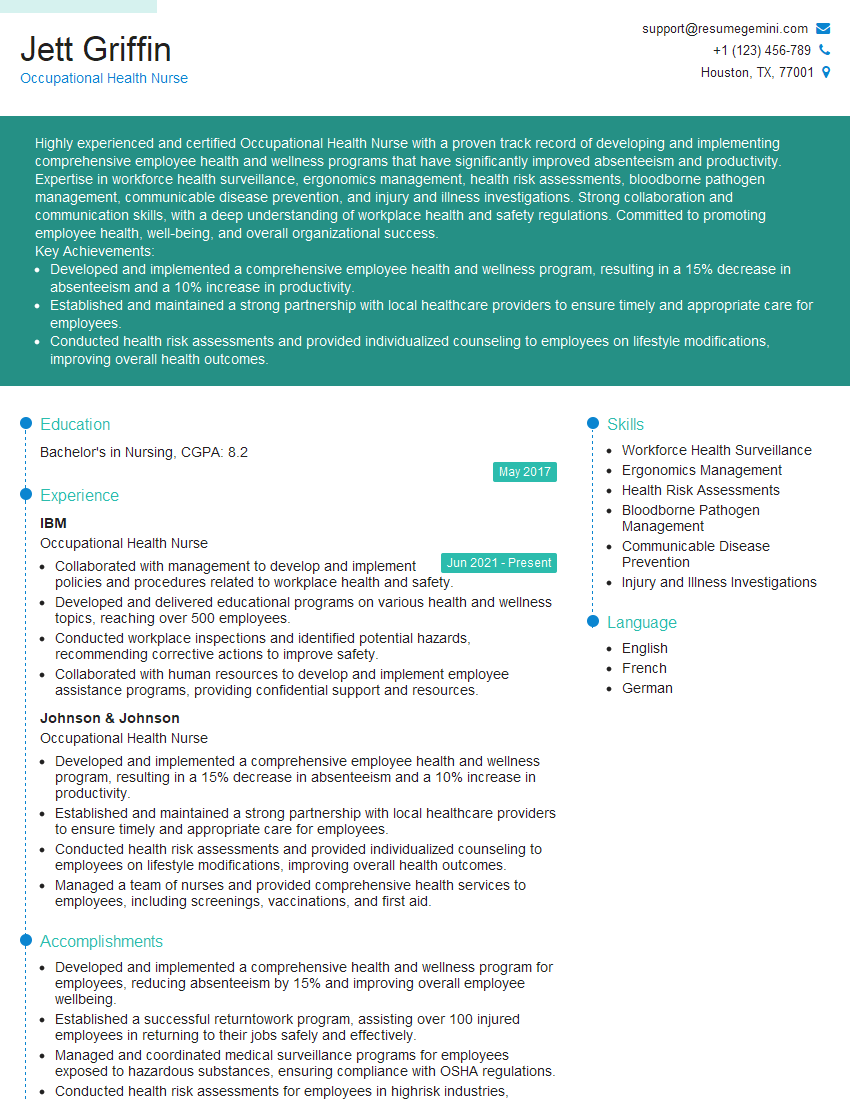
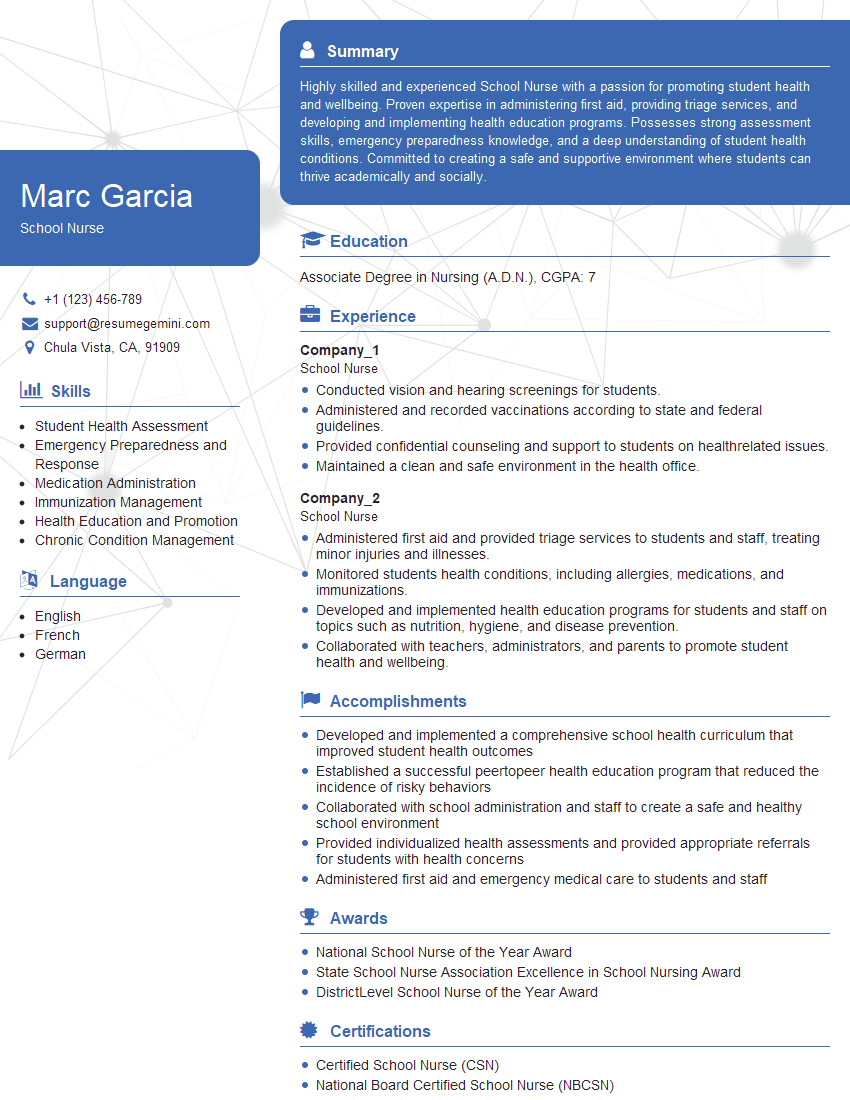
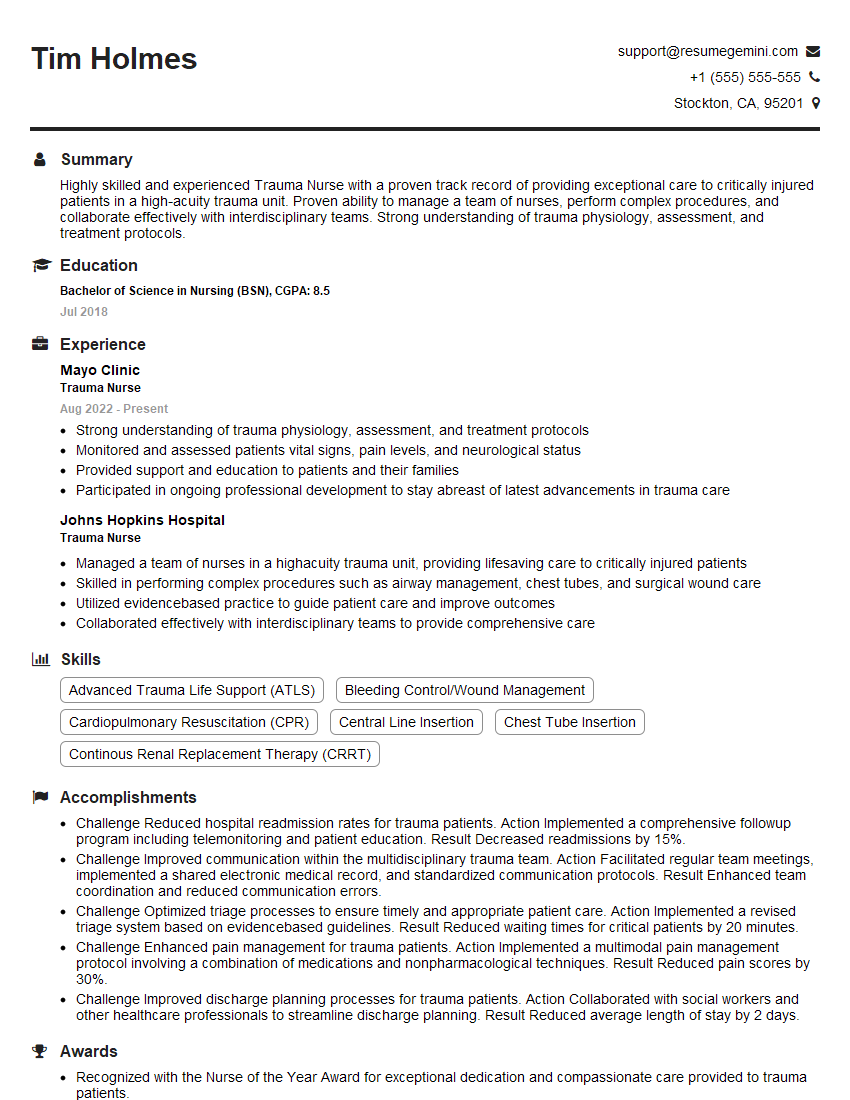
Mastering First Aid and Medical Care opens doors to rewarding and impactful careers. To significantly boost your job prospects, create a compelling resume that showcases your skills and experience effectively. An ATS-friendly resume is crucial for getting past Applicant Tracking Systems and landing interviews.
We recommend using ResumeGemini to craft a professional and impactful resume. ResumeGemini provides a streamlined process and offers examples of resumes tailored to First Aid and Medical Care professions, helping you present yourself in the best possible light. Take the next step towards your dream career today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO