Interviews are more than just a Q&A session—they’re a chance to prove your worth. This blog dives into essential Good Clinical Practice interview questions and expert tips to help you align your answers with what hiring managers are looking for. Start preparing to shine!
Questions Asked in Good Clinical Practice Interview
Q 1. Explain the principles of Good Clinical Practice (GCP).
Good Clinical Practice (GCP) is an international ethical and scientific quality standard for designing, conducting, recording, and reporting clinical trials that involve the participation of human subjects. It’s all about ensuring the rights, safety, and well-being of trial participants are protected, while also guaranteeing the credibility and reliability of the data generated. Think of it as a set of rules and guidelines that ensure clinical trials are conducted ethically and scientifically sound.
- Protection of Participants: GCP emphasizes informed consent, ensuring participants understand the study’s purpose, procedures, risks, and benefits before agreeing to participate. It also prioritizes participant safety throughout the trial, including regular monitoring and reporting of adverse events.
- Data Integrity: GCP ensures the accuracy, completeness, and reliability of data generated in clinical trials. This involves meticulous record-keeping, data validation, and audit trails to ensure the data’s authenticity.
- Ethical Conduct: GCP is underpinned by ethical principles, such as honesty, integrity, and transparency. This includes adhering to relevant regulations and guidelines, such as those from the ICH (International Council for Harmonisation).
- Scientific Validity: GCP guides the design and conduct of clinical trials to ensure they are scientifically sound and robust. This includes appropriate study design, statistical analysis, and data interpretation.
Q 2. Describe the ICH-GCP guidelines and their importance.
The ICH-GCP guidelines are a set of internationally harmonized guidelines that provide a unified standard for GCP across various regulatory authorities worldwide. They are crucial for ensuring consistency in the conduct of clinical trials, regardless of their geographic location. This harmonization simplifies the process of submitting clinical trial data to multiple regulatory agencies, saving time and resources. Imagine trying to navigate different traffic laws in each country you drive through; ICH-GCP acts as a universal set of ‘traffic rules’ for clinical trials.
The importance of ICH-GCP lies in:
- Global Acceptance: Acceptance by most regulatory agencies globally, making it easier for multinational trials.
- Patient Safety: Prioritizing the safety and well-being of participants through clear guidelines.
- Data Integrity: Ensuring the reliability and credibility of clinical trial data through standardized procedures.
- Regulatory Compliance: Facilitating compliance with regulations and avoiding potential delays or setbacks.
Q 3. What are the key responsibilities of a CRA?
A Clinical Research Associate (CRA) plays a pivotal role in ensuring the quality and integrity of clinical trials. They act as the eyes and ears of the sponsor at the trial site, verifying that the trial is being conducted according to the protocol and GCP guidelines. Think of them as the quality control officers for a clinical trial.
Key responsibilities include:
- Monitoring: Regularly visiting trial sites to review trial conduct, documentation, and source data verification.
- Protocol Compliance: Ensuring investigators adhere to the study protocol and GCP guidelines.
- Data Verification: Checking the accuracy and completeness of data collected by the investigators. This includes examining case report forms (CRFs) and other trial documentation.
- Adverse Event Reporting: Monitoring and tracking adverse events reported during the trial.
- Regulatory Compliance: Ensuring the trial complies with all relevant regulatory requirements.
- Communication: Maintaining communication between the sponsor, investigators, and other study personnel.
- Training: Providing training to investigators and study staff on GCP and study-specific procedures.
Q 4. How do you ensure patient safety in a clinical trial?
Patient safety is paramount in clinical trials. It’s not just a guideline, it’s a moral imperative. Several strategies ensure patient safety:
- Thorough Protocol Development: The study protocol must meticulously detail the study procedures, inclusion/exclusion criteria, potential risks, and safety monitoring plans.
- Informed Consent Process: Participants must provide informed consent, fully understanding the study’s purpose, procedures, and potential risks and benefits.
- Adverse Event Reporting: A robust system for reporting, investigating, and managing adverse events (AEs) and serious adverse events (SAEs) is crucial. This often involves detailed documentation and reporting to regulatory agencies.
- Regular Monitoring: CRAs conduct regular site visits to monitor participant safety and data quality. This includes reviewing medical records, laboratory data, and other relevant documentation.
- Independent Data Safety Monitoring Board (DSMB): In larger trials, an independent DSMB may be established to periodically review safety data and make recommendations to ensure participant safety.
- Ethics Committee Oversight: Ethics committees/IRBs review the study protocol and provide ongoing oversight to protect participant rights and well-being.
For example, if a participant experiences a serious adverse event, the CRA will immediately report it to the sponsor and potentially to regulatory authorities, and steps will be taken to mitigate further risk.
Q 5. Explain the process of informed consent.
Informed consent is a fundamental ethical principle in clinical research. It’s the process by which a potential participant is provided with all the necessary information to make a voluntary and informed decision about whether or not to participate in a clinical trial. This is not just about signing a form; it’s about genuine understanding and voluntary agreement.
The process typically involves:
- Pre-Consent Discussion: The investigator explains the study’s purpose, procedures, potential risks and benefits, compensation (if any), and the participant’s rights in clear, understandable language.
- Consent Form Review: The participant receives a written consent form that details all aspects of the study, and the investigator clarifies any questions.
- Question and Answer Session: The participant is encouraged to ask questions and ensure they fully understand the study.
- Voluntary Participation: The participant is free to withdraw from the study at any time without penalty.
- Consent Documentation: The signed informed consent form serves as legal documentation of the participant’s voluntary agreement to participate in the trial.
For example, in a study involving a new medication, the informed consent document would explain the medication’s purpose, how it’s administered, potential side effects, and alternative treatment options.
Q 6. What are the essential components of a case report form (CRF)?
A Case Report Form (CRF) is a standardized document used to collect and record data for each individual participant in a clinical trial. It’s like a structured questionnaire that ensures consistent data collection across all participants. Think of it as the central repository for all participant-specific information.
Essential components of a CRF include:
- Participant Demographics: Age, gender, race, ethnicity, etc.
- Inclusion/Exclusion Criteria: Confirmation that the participant met the criteria to participate.
- Medical History: Pre-existing conditions, allergies, medications.
- Treatment Information: Details of the treatment regimen, including dosage and administration.
- Adverse Events: Reporting of any adverse events or side effects experienced by the participant.
- Laboratory Data: Results of blood tests, urine tests, etc.
- Assessments: Results of any assessments conducted, such as physical exams or questionnaires.
- Study Endpoint Data: Data relevant to the study’s primary and secondary endpoints.
- Date and Signature: To ensure accurate documentation and traceability of the data.
Q 7. Describe your experience with data management in clinical trials.
My experience in clinical trial data management encompasses all aspects of data handling, from database setup and data entry to data cleaning, validation, and reporting. I am proficient in using various data management systems (e.g., EDC systems) and statistical software packages. I have been involved in several projects that involve the creation and management of electronic data capture (EDC) databases, the development of data validation rules, and the implementation of data quality control procedures.
In one project, I was responsible for developing and implementing data validation rules for a large, multi-center clinical trial. These rules ensured data consistency and accuracy, identifying and resolving errors before they could impact the study’s results. For instance, I developed a rule to flag any inconsistencies between reported adverse events and the corresponding medical records. This rigorous approach ensured data integrity and contributed to the successful completion of the trial.
I am adept at using various data management systems and statistical packages like SAS and R to process, analyze and present data. Data management is a critical part of ensuring the credibility and success of any clinical trial, and I’m passionate about ensuring this process is as robust and reliable as possible.
Q 8. How do you handle deviations and discrepancies in clinical trial data?
Handling deviations and discrepancies in clinical trial data is crucial for maintaining data integrity and ensuring the reliability of trial results. It involves a systematic process of detection, documentation, investigation, and resolution. Think of it like a detective story – we need to find the discrepancy, understand its cause, and then make sure it doesn’t affect the overall conclusion.
Detection: Regular data quality checks, including data validation, range checks, and consistency checks, are essential. We use software to flag potential issues, and manual review is also important, especially for complex data.
Documentation: Every deviation or discrepancy needs meticulous documentation. This includes the date, time, nature of the issue, the individuals involved, the investigation steps taken, and the resolution.
Investigation: A thorough investigation is vital to understand the root cause. This might involve reviewing source documents, interviewing involved personnel, and analyzing the data’s context. For example, a discrepancy might be due to a data entry error, a protocol deviation, or a problem with the equipment used.
Resolution: Corrective actions are implemented to prevent recurrence. This could involve retraining staff, improving data entry procedures, or modifying equipment. A clear record of the resolution is maintained.
Reporting: Significant deviations are escalated to the appropriate regulatory authorities and the sponsor.
For example, if we find a discrepancy in a patient’s weight recorded on different days, we’d investigate whether it’s a genuine fluctuation or a data entry error. If it’s an error, we correct it, document the correction, and consider implementing measures to prevent similar errors in the future, such as double-data entry or improved data validation rules.
Q 9. What is the role of an independent ethics committee (IEC) or Institutional Review Board (IRB)?
The Independent Ethics Committee (IEC), also known as the Institutional Review Board (IRB), plays a vital role in protecting the rights and welfare of human participants in clinical trials. They act as independent guardians, ensuring that the research is ethically sound and conducted in accordance with ethical principles and applicable regulations.
Review of Protocols: The IEC/IRB meticulously reviews the study protocol, including the research question, methodology, risks and benefits to participants, informed consent process, and data handling procedures. They ensure the study is scientifically sound and ethically justifiable.
Informed Consent: They scrutinize the informed consent process to confirm that participants are fully informed about the study’s purpose, procedures, potential risks and benefits, and their rights. They make sure participants understand they can withdraw at any time without penalty.
Monitoring Safety: The IEC/IRB reviews safety data throughout the trial, particularly reports of adverse events. They assess whether the risks are acceptable and whether the study should continue, be modified, or terminated.
Compliance Oversight: They ensure the study adheres to all relevant ethical guidelines, regulations, and laws.
Think of them as an independent oversight body, making sure the trial is conducted with the utmost respect for participants’ well-being. Their approval is necessary to legally conduct a clinical trial involving human subjects.
Q 10. Explain the process of adverse event (AE) reporting.
Adverse event (AE) reporting is a critical aspect of clinical trial safety monitoring. An AE is any untoward medical occurrence in a patient or clinical trial participant administered a pharmaceutical product and which does not necessarily have a causal relationship with this treatment. Reporting involves a structured process to ensure that any potential safety signals are promptly identified and investigated.
Detection: AEs are identified through various sources, including patient self-reporting, investigator observations, and review of medical records.
Documentation: Each AE is meticulously documented, including the date, nature of the event, severity, relationship to the investigational product, actions taken, and outcome.
Reporting: AEs are reported to the sponsor and regulatory authorities according to predefined timelines and seriousness criteria. Serious AEs (SAEs), which are defined as those that result in death, are life-threatening, require hospitalization or prolongation of existing hospitalization, result in persistent or significant disability/incapacity, or are a congenital anomaly/birth defect, are reported immediately.
Assessment: The sponsor assesses the causality of AEs, determining whether they are related to the investigational product. This assessment is often based on medical expertise and established criteria.
Follow-up: Appropriate follow-up actions are taken, such as modifying the treatment plan, conducting further investigations, or alerting healthcare providers.
Imagine a scenario where a patient experiences a sudden drop in blood pressure after receiving the investigational drug. This would be reported as an AE, and the seriousness and potential relationship to the drug would be carefully evaluated.
Q 11. How do you ensure the quality and integrity of clinical trial data?
Ensuring the quality and integrity of clinical trial data is paramount. It’s like building a skyscraper – if the foundation is weak, the entire structure is compromised. This involves a multifaceted approach that spans the entire trial lifecycle.
Data Management Plan: A comprehensive data management plan should be in place from the outset, outlining procedures for data collection, handling, storage, and validation.
Data Validation: Robust data validation checks are essential to detect and correct errors early. This includes range checks, consistency checks, and plausibility checks. For example, a patient’s age cannot be negative.
Data Monitoring: Regular data monitoring and review help identify potential anomalies and inconsistencies. We use statistical techniques to detect unexpected patterns.
Auditing: Regular audits (internal and external) are conducted to ensure compliance with GCP guidelines and data quality standards.
Training: Comprehensive training for study personnel is crucial to ensure that data is collected, recorded, and handled according to the highest standards.
Electronic Data Capture (EDC): Utilizing EDC systems enhances data quality by minimizing manual errors and improving data consistency.
By implementing these measures, we can ensure that the data generated is reliable, accurate, and fit for its intended purpose – supporting regulatory submissions and informing healthcare decisions.
Q 12. Describe your experience with clinical trial audits.
I have extensive experience with clinical trial audits, both as an auditor and an auditee. Audits are a systematic and independent examination of the trial’s conduct and data to verify compliance with GCP guidelines and regulatory requirements. They are crucial for ensuring the reliability and integrity of the data.
Internal Audits: These are conducted by the sponsor or CRO to proactively identify and correct deficiencies before external audits.
External Audits: These are performed by regulatory authorities or independent auditors to verify compliance and data integrity. These audits are far more rigorous and can have significant consequences if non-compliance is found.
Audit Process: The audit process typically involves reviewing study documents, interviewing personnel, and examining data to verify compliance with the protocol, GCP guidelines, and regulatory requirements. Any deviations or discrepancies are documented and reported.
Corrective Actions: Any findings from an audit require the implementation of corrective and preventive actions (CAPAs) to address the deficiencies and prevent recurrence.
I’ve been involved in numerous audits, both leading and participating in them, gaining valuable experience in identifying potential issues, conducting thorough investigations, and implementing effective corrective actions. I’ve successfully led teams to resolve audit findings and improve processes to ensure ongoing compliance and data quality. For instance, in one instance, an audit revealed inconsistencies in source data verification; I developed and implemented a new training program to remedy this issue, ultimately improving the quality of the data and increasing the overall compliance.
Q 13. What are your strategies for managing risks in a clinical trial?
Risk management in clinical trials is essential for ensuring the safety of participants, the integrity of the data, and the success of the trial itself. It’s about proactively identifying, assessing, and mitigating potential problems.
Risk Identification: This involves systematically identifying potential risks throughout the trial lifecycle. This can be done through brainstorming sessions, reviewing past trial experiences, and considering potential protocol deviations and site-specific challenges.
Risk Assessment: This involves evaluating the likelihood and potential impact of each identified risk. This will often involve using a risk matrix to categorize risks based on severity and probability.
Risk Mitigation: This involves implementing strategies to reduce the likelihood or impact of risks. Examples include improving communication, providing additional training, implementing quality control measures, and developing contingency plans.
Risk Monitoring: Ongoing monitoring is essential to track the effectiveness of risk mitigation strategies and to identify new or emerging risks.
Documentation: All aspects of risk management should be meticulously documented, including the identified risks, assessment results, mitigation strategies, and monitoring activities.
For example, if a trial involves a new technology or procedure, there’s a risk of equipment failure. We might mitigate this by having backup equipment, providing additional training, and developing a detailed contingency plan to handle equipment malfunctions.
Q 14. How do you handle conflicts of interest in clinical research?
Conflicts of interest (COIs) in clinical research can compromise the integrity and objectivity of the trial. It’s about transparency and ensuring that personal interests don’t influence the research process. Think of it as maintaining an unbiased playing field.
Disclosure: All individuals involved in the trial (investigators, study staff, monitors) must disclose any potential COIs, including financial interests, personal relationships, or other factors that could create a bias. This often involves completing conflict of interest questionnaires.
Management: Once a COI is identified, it needs to be managed appropriately. This might involve modifying the individual’s role, implementing oversight measures, or even excluding the individual from the trial if the COI is too significant.
Independent Review: An independent body (often the IEC/IRB) should review COI disclosures to ensure they are thorough and that appropriate management strategies are in place.
Documentation: All COI disclosures and management strategies must be meticulously documented.
For instance, if an investigator has a financial stake in the company sponsoring the trial, this would be a significant COI that needs to be disclosed and managed appropriately. This could involve having another investigator oversee certain aspects of the trial or implementing rigorous oversight measures to ensure the data’s independence.
Q 15. Explain your understanding of blinding and randomization in clinical trials.
Blinding and randomization are crucial techniques in clinical trials designed to minimize bias and enhance the reliability of results. Randomization is the process of assigning participants to different treatment groups (e.g., placebo, drug A, drug B) completely by chance. This ensures that the groups are comparable at the start of the trial, reducing the risk of confounding factors influencing the outcome. Think of it like flipping a coin – each participant has an equal chance of landing in any group. A proper randomization method, like stratified randomization or block randomization, is used to ensure balance across different subgroups.
Blinding, also known as masking, prevents participants and/or investigators from knowing which treatment a participant is receiving. This prevents conscious or unconscious bias from influencing the assessment of treatment effects. There are different levels of blinding: single-blind (participants are unaware of their treatment assignment), double-blind (both participants and investigators are unaware), and triple-blind (participants, investigators, and data analysts are unaware). For instance, in a double-blind study of a new pain medication, neither the patient nor the doctor administering the drug would know if the pill is the actual medication or a placebo.
The combination of randomization and blinding significantly strengthens the internal validity of a clinical trial, allowing for a more accurate assessment of the treatment’s true effect.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the key regulatory requirements for conducting clinical trials?
Key regulatory requirements for conducting clinical trials vary slightly depending on the region (e.g., FDA in the US, EMA in Europe), but some common overarching principles include adherence to Good Clinical Practice (GCP) guidelines, which provide a standard for the design, conduct, performance, monitoring, auditing, recording, analyses, archiving and reporting of clinical trials that produce credible and reliable results. These guidelines are essential for protecting the rights, safety and well-being of trial participants and maintaining the integrity of the data.
- Ethical Review Board (IRB) or Institutional Review Board (IEC) approval: All trials require ethical review and approval to ensure the study is ethically sound and protects participants’ rights.
- Informed consent: Participants must provide informed consent, meaning they understand the study’s purpose, procedures, risks, and benefits before participating.
- Data integrity and quality: Accurate and reliable data collection and management are paramount. This involves using standardized procedures, proper documentation, and regular data monitoring.
- Regulatory compliance: All aspects of the trial must comply with relevant regulations, including those related to safety reporting, adverse event management, and data privacy.
- Investigator qualification and training: Investigators must be appropriately qualified and trained to conduct the trial according to GCP standards.
- Protocol adherence: The trial must be conducted strictly according to the approved protocol.
Non-compliance with these regulations can lead to serious consequences, including study termination, regulatory sanctions, and reputational damage. A thorough understanding of the applicable regulations is essential for successfully conducting a clinical trial.
Q 17. How familiar are you with electronic data capture (EDC) systems?
I am highly familiar with electronic data capture (EDC) systems. My experience spans several leading EDC platforms, including [mention specific platforms e.g., Medidata Rave, Oracle InForm, etc.]. I understand the benefits of EDC, such as improved data quality, reduced data entry errors, faster data analysis, and enhanced compliance with regulatory requirements. I’m proficient in designing case report forms (CRFs) within these systems, managing user access and permissions, conducting data queries, and generating reports. I also have experience with EDC system validation and data migration processes.
In a previous study, we successfully migrated data from a paper-based system to an EDC system, minimizing data loss and ensuring data integrity throughout the process. This transition significantly streamlined our data management processes and improved the efficiency of the trial.
Q 18. Describe your experience with data cleaning and validation.
Data cleaning and validation are critical steps in ensuring the quality and reliability of clinical trial data. My approach involves a multi-step process:
- Data review and query generation: Thorough review of the data for inconsistencies, outliers, and missing values. Queries are generated to clarify any questionable data points.
- Query resolution: Working with site personnel to resolve queries, obtaining clarifications, and correcting any errors.
- Data validation: Applying programmed edits and checks within the EDC system to identify further inconsistencies and errors.
- Data cleaning: Correcting errors and inconsistencies identified during the review and validation processes.
- Data reconciliation: Verifying that the cleaned data is consistent across different data sources.
- Documentation: Meticulously documenting all data cleaning and validation activities, including the queries, resolutions, and corrections made.
For example, in one study, we identified a significant discrepancy in the age reported for a subset of participants. By systematically reviewing the source documents and contacting the sites, we were able to correct the error, preventing misleading conclusions from being drawn from the data analysis.
Q 19. What is your approach to problem-solving in a clinical trial setting?
My approach to problem-solving in a clinical trial setting is methodical and data-driven. I typically follow these steps:
- Problem definition: Clearly define the problem, including the context, impact, and stakeholders involved.
- Data analysis: Gather and analyze relevant data to understand the root cause of the problem.
- Solution brainstorming: Generate multiple potential solutions, considering their feasibility, cost, and potential impact.
- Solution evaluation: Evaluate the potential solutions based on predefined criteria, such as effectiveness, efficiency, and risk.
- Solution implementation: Implement the chosen solution, ensuring proper communication and collaboration with stakeholders.
- Monitoring and evaluation: Monitor the effectiveness of the implemented solution and make adjustments as needed.
For example, if we encountered unexpected delays in patient recruitment, I would analyze the recruitment data to pinpoint the bottlenecks (e.g., site activation issues, low patient referral rates). Then, I would collaborate with the study team to develop and implement strategies to address these issues, such as improving communication with referral sources or providing additional training to site staff.
Q 20. How do you manage timelines and budgets in clinical trials?
Managing timelines and budgets in clinical trials requires careful planning, meticulous tracking, and proactive risk management. I utilize project management tools and techniques, such as Gantt charts and critical path analysis, to visualize timelines and identify potential delays. Regular monitoring of progress against the budget is crucial, using tools like earned value management to track performance and identify variances. Proactive communication with stakeholders is essential to ensure everyone is informed of any issues and potential solutions.
A key strategy I use is to develop contingency plans to address potential delays or budget overruns. This might involve identifying alternative solutions, negotiating with vendors, or adjusting the study protocol if necessary. Regular meetings with the study team and sponsors are crucial for reviewing progress, managing risks, and ensuring everyone is aligned on the project’s goals.
Q 21. Explain your experience with different clinical trial phases.
I have experience across all phases of clinical trials. My understanding of each phase includes:
- Phase I: Focuses on safety and tolerability of the investigational product in a small group of healthy volunteers. This phase helps to determine the appropriate dose range for further studies.
- Phase II: Evaluates the efficacy and safety of the investigational product in a larger group of patients with the target disease. This phase helps to refine dosing and identify potential side effects.
- Phase III: Large-scale trials designed to confirm the efficacy and safety of the investigational product in a large patient population. This phase provides the data needed for regulatory approval.
- Phase IV: Post-market surveillance to monitor the long-term effects and safety of the approved product in a wider patient population.
In my previous roles, I have been involved in all phases, from designing case report forms for Phase I studies to managing large datasets in Phase III trials and contributing to post-market surveillance in Phase IV. This broad experience has provided me with a comprehensive understanding of the nuances of each phase and the interdependencies between them.
Q 22. Describe your experience working with cross-functional teams.
Throughout my career, I’ve consistently thrived in cross-functional team environments. I believe the success of a clinical trial hinges on seamless collaboration between various specialists – from medical monitors and data managers to regulatory affairs and biostatisticians. For instance, in a recent Phase III oncology trial, I was instrumental in bridging the communication gap between the data management team and the medical monitoring team. The data management team had identified some inconsistencies in the data entry, while the medical monitors were concerned about the potential impact on safety reporting. By facilitating regular meetings and fostering open communication, we were able to efficiently resolve the issues, ensuring data accuracy and timely safety reporting. My approach focuses on active listening, clear communication of expectations, and leveraging each team member’s unique expertise to achieve a shared objective. I believe in promoting a collaborative culture where everyone feels empowered to contribute and voice concerns.
- Facilitating effective meetings: Setting clear agendas, ensuring all relevant stakeholders attend, and effectively summarizing action items.
- Utilizing project management tools: Leveraging tools like Asana or Jira to streamline workflow, track progress, and enhance transparency.
- Conflict resolution: Addressing disagreements constructively through mediation and finding mutually acceptable solutions.
Q 23. How do you communicate effectively with investigators and sponsors?
Effective communication with investigators and sponsors is paramount to the successful execution of a clinical trial. With investigators, I prioritize building strong, trusting relationships built on mutual respect and transparency. This involves regular communication updates, proactive problem-solving, and a willingness to address their questions and concerns promptly. For example, if an investigator raises concerns about a protocol amendment, I would ensure I thoroughly explain the rationale and answer their questions completely. With sponsors, I maintain open and transparent communication regarding study progress, budget, timelines, and any potential risks or challenges. Regular status reports, both written and verbal, are essential. I often use data visualization tools to present complex information clearly and concisely. For instance, presenting safety data with clear graphs and tables rather than lengthy textual reports would improve their comprehension. My communication style is always tailored to the audience; I ensure that technical details are explained clearly and simply, avoiding jargon where possible.
Q 24. How do you stay current with GCP guidelines and regulatory changes?
Staying current with GCP guidelines and regulatory changes is an ongoing process that I take very seriously. I regularly review updates from regulatory bodies like the FDA and EMA, subscribe to relevant journals and newsletters (e.g., the DIA’s publications), and actively participate in professional development activities, including webinars and conferences. I’m also a member of professional organizations such as the Society for Clinical Research Associates (SOCRA), which keeps me informed about the latest advancements and best practices in GCP. Furthermore, I consistently review and update my knowledge of the International Council for Harmonisation (ICH) guidelines, paying close attention to any changes or clarifications. This proactive approach ensures that my work is always compliant and adheres to the highest ethical and scientific standards. I see this as an essential element of my responsibilities, as staying abreast of the latest regulations is crucial for ensuring data integrity and patient safety.
Q 25. Describe your experience with clinical trial reporting.
I have extensive experience in all aspects of clinical trial reporting, from preparing case report forms (CRFs) and data listings to generating clinical study reports (CSRs) and integrated summaries of safety (ISS). I am proficient in using various software applications, including SAS and R, to analyze data and prepare reports. For example, in a recent study, I was responsible for generating the CSR, which required careful analysis of the data, interpretation of the results, and presentation of the findings in a clear and concise manner. I also have experience in preparing regulatory submissions, including preparing documents for regulatory agencies like the FDA and EMA. My focus is always on accuracy, completeness, and adherence to regulatory guidelines and industry best practices. I understand the importance of meticulous documentation and ensuring that all reports are properly validated and signed off by the relevant personnel. I work to make sure the reports meet the regulatory requirements and are easily understandable to the intended audience.
Q 26. What are your strengths and weaknesses in a clinical research setting?
My strengths lie in my meticulous attention to detail, my strong analytical and problem-solving skills, and my ability to build strong working relationships. I’m adept at managing complex projects, handling multiple priorities simultaneously, and meeting tight deadlines. I’m also a highly effective communicator and collaborator. A weakness I am actively working on is delegating tasks. I sometimes tend to take on too much responsibility, leading to potential burnout. I’ve implemented strategies to address this, such as proactively identifying team members with the appropriate skills to handle specific tasks, and trusting in their capabilities to complete the work effectively. I’ve found that regularly reviewing progress and providing constructive feedback helps to ensure the success of the delegated tasks and fosters a sense of shared responsibility within the team.
Q 27. Why are you interested in this specific role in Good Clinical Practice?
I’m keenly interested in this specific role because it aligns perfectly with my passion for ensuring the integrity and ethical conduct of clinical research. I believe in the critical role clinical trials play in advancing medical knowledge and improving patient health. This role offers the opportunity to contribute directly to this process, ensuring that clinical trials are conducted in accordance with GCP, protecting participant rights and well-being, and delivering high-quality, reliable data to support the development of safe and effective therapies. The opportunity to work within a team dedicated to excellence in clinical research and contribute to improving patient outcomes strongly appeals to me. The specific responsibilities outlined in the job description further resonate with my skills and experience, making this a particularly exciting prospect.
Key Topics to Learn for Good Clinical Practice Interview
- Ethical Considerations in GCP: Understand the principles of informed consent, patient safety, and data integrity. Consider how these principles guide decision-making in real-world clinical trial scenarios.
- Regulatory Compliance (ICH-GCP Guidelines): Familiarize yourself with the key components of ICH-GCP guidelines and their practical implications for conducting clinical trials. Be prepared to discuss specific aspects, such as documentation requirements and audit trails.
- Case Report Form (CRF) Design and Data Management: Learn about the importance of well-designed CRFs for efficient data collection and analysis. Explore methods for ensuring data quality and managing inconsistencies.
- Monitoring and Auditing in GCP: Understand the roles and responsibilities of monitors and auditors in ensuring compliance with GCP guidelines. Be ready to discuss various monitoring strategies and the importance of timely issue resolution.
- Risk Management in Clinical Trials: Explore how risk mitigation strategies are implemented to protect patient safety and data integrity. Consider examples of potential risks and how they are addressed throughout a trial’s lifecycle.
- Data Integrity and Verification: Master the concepts of data integrity and the techniques used to verify its accuracy and reliability. Be prepared to discuss practical examples and potential challenges in maintaining data integrity.
- Investigator Site Selection and Management: Understand the criteria for selecting appropriate clinical trial sites and the processes involved in managing investigator relationships and performance.
- Pharmacovigilance and Safety Reporting: Understand the importance of pharmacovigilance in detecting and reporting adverse events. Be prepared to discuss the process of adverse event reporting and safety data management.
Next Steps
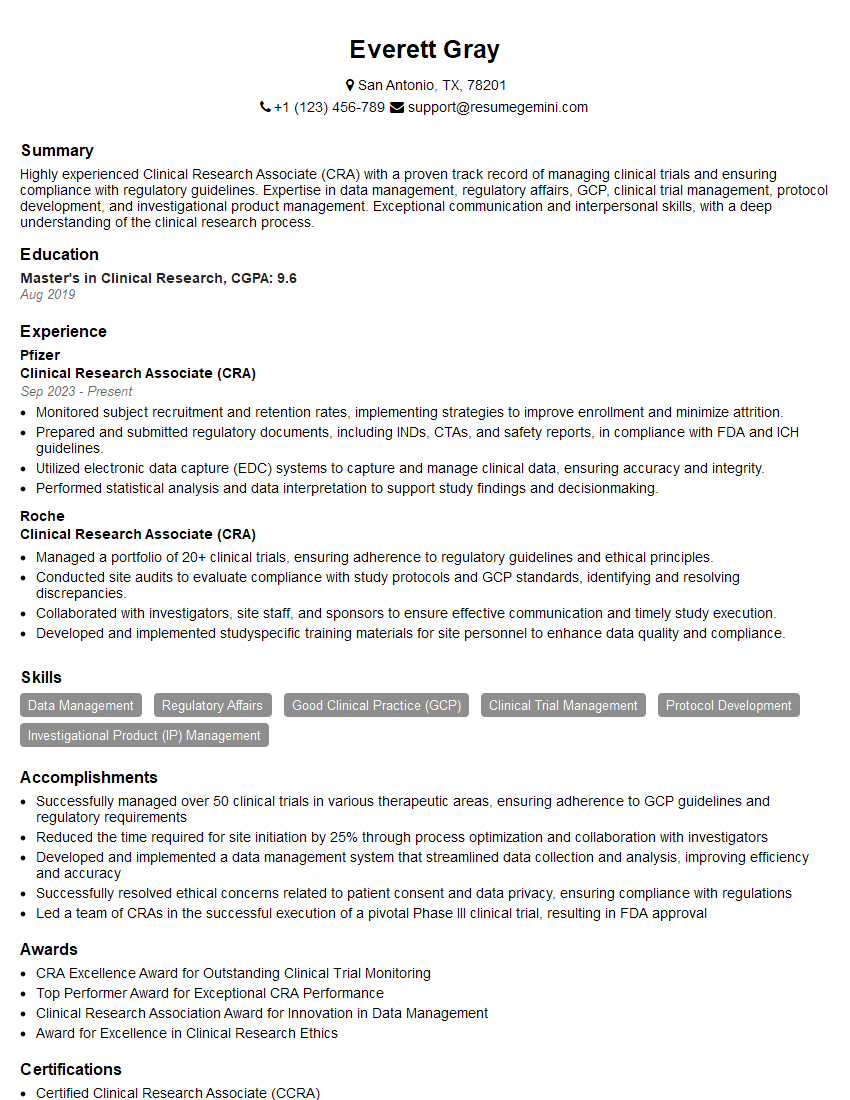
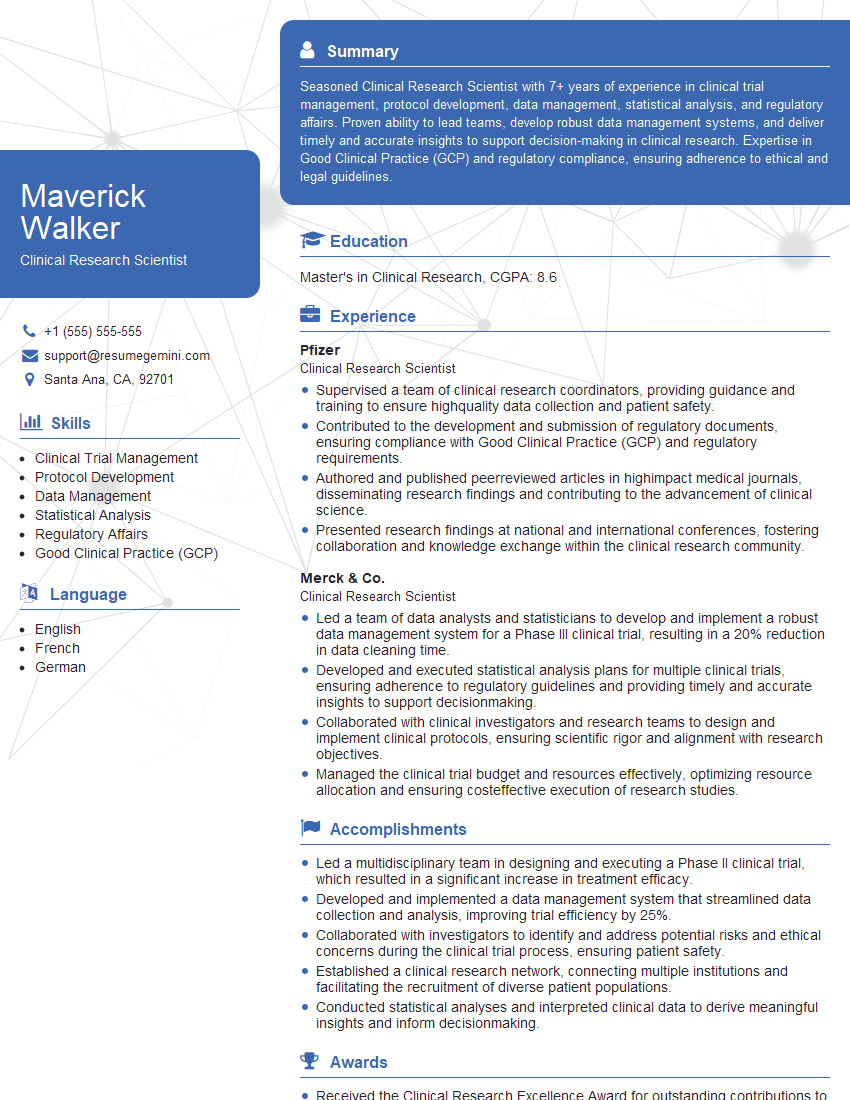
Mastering Good Clinical Practice is crucial for career advancement in the pharmaceutical and healthcare industries, opening doors to leadership roles and specialized expertise. An ATS-friendly resume is essential for maximizing your job prospects. To build a compelling and effective resume that highlights your GCP knowledge and experience, we strongly encourage you to utilize ResumeGemini. ResumeGemini offers a streamlined process for creating professional resumes, and we provide examples of resumes tailored to Good Clinical Practice to help you get started.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO