Cracking a skill-specific interview, like one for HIPAA Training, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in HIPAA Training Interview
Q 1. Explain the key components of the HIPAA Privacy Rule.
The HIPAA Privacy Rule establishes national standards to protect individuals’ medical records and other health information. Think of it as a strong lock on your medical information, preventing unauthorized access and ensuring your privacy.
Protected Health Information (PHI): This is the core of the rule. PHI includes any information, whether electronic, paper, or oral, that can be linked to a specific person and relates to their past, present, or future physical or mental health, provision of healthcare, or payment for healthcare. Examples include names, addresses, medical record numbers, diagnoses, and treatment details.
Individual Rights: The rule grants individuals significant rights regarding their PHI, including the right to access their records, request amendments, receive an accounting of disclosures, and request restrictions on certain uses or disclosures. Imagine being able to see your medical records and know who has accessed them.
Permitted Uses and Disclosures: HIPAA outlines specific circumstances where PHI can be used or disclosed without an individual’s authorization, such as for treatment, payment, or healthcare operations. For example, your doctor can share your information with the lab to run tests, or your insurer can use it to process a claim.
Minimum Necessary Standard: Only the minimum amount of PHI necessary to accomplish a particular purpose should be used or disclosed. This prevents unnecessary exposure of sensitive data. Think of it as only providing the essential details, not the whole medical file, to a researcher.
Privacy Officer: Covered entities must designate a Privacy Officer responsible for the development and implementation of privacy policies and procedures. This ensures someone is accountable for protecting patient privacy.
Q 2. Describe the HIPAA Security Rule and its safeguards.
The HIPAA Security Rule specifies safeguards to protect the confidentiality, integrity, and availability of electronic Protected Health Information (ePHI). It’s like a multi-layered security system protecting digital medical records.
Administrative Safeguards: These are policies, procedures, and processes designed to manage security risks. This includes risk analysis, security awareness training, and incident response plans.
Physical Safeguards: These protect ePHI from unauthorized physical access. Examples include access controls to computer rooms, security cameras, and protection of computer equipment.
Technical Safeguards: These use technology to control access to and protect ePHI. Examples include access controls (usernames and passwords), audit controls (tracking who accessed what), and encryption (scrambling the data to make it unreadable without a key). Think of these as electronic locks and alarms for your medical data.
Consider a hospital’s electronic health record (EHR) system. The administrative safeguards ensure staff receive proper training on data security, the physical safeguards secure server rooms, and the technical safeguards protect the data itself from unauthorized access through encryption and strong passwords.
Q 3. What are the differences between PHI and PII?
While both PHI and PII deal with identifying information, they differ in scope. PHI is a subset of PII specifically related to health information.
Protected Health Information (PHI): This is any information about an individual’s past, present, or future physical or mental health or condition, the provision of healthcare to an individual, or the past, present, or future payment for the provision of healthcare to an individual; and that identifies the individual or with respect to which there is a reasonable basis to believe it can be used to identify the individual.
Personally Identifiable Information (PII): This is any information that can be used to identify an individual. This is a broader term and includes information such as name, address, social security number, email address, and date of birth. PHI is a specific type of PII.
For example, a patient’s name and address are PII. If that information is combined with their diagnosis and treatment details, it becomes PHI.
Q 4. Explain the HIPAA Breach Notification Rule.
The HIPAA Breach Notification Rule requires covered entities and business associates to provide notification following a breach of unsecured protected health information (PHI). Imagine this as a mandatory alert system in case someone gains unauthorized access to your medical data.
If a breach occurs, the covered entity must notify affected individuals, the Secretary of Health and Human Services, and, in some cases, the media. The notification must include information about the breach, what information was involved, what steps are being taken to mitigate further harm, and what steps individuals can take to protect themselves.
The timing of notifications is crucial. Notification to individuals must occur without unreasonable delay, and in any case, no later than 60 days following the discovery of the breach. Reporting to HHS follows a similar timeframe.
Q 5. What is the role of a designated HIPAA Privacy Officer?
The HIPAA Privacy Officer is a key figure within a covered entity, responsible for overseeing all aspects of HIPAA compliance related to privacy. Think of them as the chief guardian of patient privacy within the organization.
Developing and Implementing Privacy Policies: They create and maintain the organization’s privacy policies and procedures, ensuring they align with HIPAA regulations.
Training and Education: They conduct HIPAA privacy training for staff, ensuring everyone understands their responsibilities.
Responding to Privacy Inquiries: They handle inquiries and complaints related to patient privacy.
Managing Privacy-Related Issues: They oversee investigations into potential privacy breaches and implement corrective actions.
The Privacy Officer ensures the organization protects patient information and complies with all applicable regulations. Their role is crucial in maintaining trust and upholding patient rights.
Q 6. Describe the process for obtaining authorization for the use or disclosure of PHI.
Obtaining authorization for the use or disclosure of PHI outside of permitted uses requires a specific process. This is essentially getting explicit permission from the patient beyond the standard uses allowed by HIPAA.
The authorization must be:
- In writing (or another form the individual agrees to).
- Contain specific information, including the purposes for the disclosure, the permitted disclosures, the individuals or organizations authorized to receive the information, and an expiration date for the authorization.
- Be signed and dated by the individual or their authorized representative.
Before obtaining authorization, the covered entity should fully inform the individual about the use or disclosure of PHI. They should also obtain any necessary consent from the individual. The process ensures transparency and protects the patient’s rights. A common scenario would be researchers needing authorization to use patient data for research purposes beyond the permitted uses of HIPAA.
Q 7. Explain the concept of Minimum Necessary.
The Minimum Necessary standard requires covered entities to only use, disclose, request, or receive the minimum amount of protected health information (PHI) needed to accomplish a specific purpose. Think of it as applying a ‘need-to-know’ principle to patient information.
For example, if a doctor needs to refer a patient to a specialist, they would only share the information directly relevant to the referral, not the entire medical record. This reduces the risk of unauthorized access and protects patient privacy. Failure to comply with the Minimum Necessary standard can result in a HIPAA violation.
Q 8. What are the penalties for HIPAA violations?
HIPAA violations can result in a wide range of penalties, depending on the severity and nature of the breach, as well as the covered entity’s knowledge and actions. These penalties can be substantial and include civil monetary penalties (CMPs), criminal penalties, and corrective action requirements.
- Civil Monetary Penalties (CMPs): These are tiered based on the level of culpability (knowing, willful neglect, etc.). A single violation can range from thousands to tens of thousands of dollars per violation, with higher penalties for repeat offenders or those demonstrating willful neglect. For example, a hospital might face substantial CMPs for failing to implement reasonable safeguards to protect ePHI, leading to a data breach.
- Criminal Penalties: In cases involving intentional violations or the knowing and wrongful disclosure of PHI for personal gain, criminal charges can be filed. These can lead to significant fines and even imprisonment. Imagine a healthcare worker who illegally sells patient data; they would face serious criminal consequences.
- Corrective Action Plans: Even without significant fines, a HIPAA violation can trigger the need for a comprehensive corrective action plan. This involves identifying the root cause of the violation, implementing changes to prevent future occurrences, and demonstrating compliance with HIPAA regulations. A clinic that experiences a data breach due to a lack of employee training would be required to develop a robust training program as part of its corrective action.
The Office for Civil Rights (OCR) within the Department of Health and Human Services (HHS) is responsible for enforcing HIPAA, investigating complaints, and imposing penalties.
Q 9. How does HIPAA apply to electronic protected health information (ePHI)?
HIPAA’s Privacy and Security Rules explicitly cover electronic protected health information (ePHI). This means that all the rules and regulations regarding the use, disclosure, and protection of PHI apply equally, whether the information is in paper form or electronic format. In fact, ePHI often presents greater security challenges due to its accessibility and potential for wider dissemination.
The Security Rule, in particular, outlines specific administrative, physical, and technical safeguards that covered entities must implement to protect ePHI. These safeguards address everything from access controls and encryption to data backup and disaster recovery planning. Failure to implement these safeguards can result in significant penalties, as previously explained.
Think of it this way: if you have a patient’s medical record on paper, you’d lock it in a secure cabinet. With ePHI, the equivalent is implementing robust access controls, encryption, and strong passwords to ensure that only authorized individuals can access the information.
Q 10. What are the requirements for HIPAA compliant email communication?
HIPAA-compliant email communication requires implementing several measures to protect the confidentiality, integrity, and availability of ePHI. Simply put, you can’t just send PHI via standard email.
- Encryption: Email messages containing ePHI must be encrypted using a HIPAA-compliant encryption method. This ensures that even if the email is intercepted, the content remains unreadable without the decryption key.
- Authentication: Implement measures to verify the sender and recipient’s identities. This could involve using digital certificates or other secure authentication methods to prevent unauthorized access.
- Access Controls: Limit access to ePHI to only authorized individuals. This includes controlling who can send, receive, and view PHI-containing emails.
- Secure Email Platforms: Consider using HIPAA-compliant email platforms that offer built-in security features like encryption, audit trails, and access controls.
- Data Loss Prevention (DLP) tools: Using DLP tools can help prevent accidental or malicious disclosure of ePHI via email.
- Training and Policies: Staff must be trained on proper procedures for sending and receiving ePHI via email.
For example, instead of sending a patient’s lab results directly through standard email, a HIPAA-compliant practice would use a secure email system with end-to-end encryption and ensure that only the patient and authorized personnel have access to the information.
Q 11. Describe the safeguards under the HIPAA Security Rule: Administrative, Physical, and Technical.
The HIPAA Security Rule mandates the implementation of three categories of safeguards to protect ePHI: Administrative, Physical, and Technical.
- Administrative Safeguards: These involve policies, procedures, and processes related to security. Examples include risk analysis, security awareness training for employees, policies on acceptable use of systems, and incident response plans. Imagine a hospital creating a comprehensive policy outlining proper procedures for handling data breaches, including who to contact and what steps to take.
- Physical Safeguards: These relate to the physical security of the environment where ePHI is stored and processed. This includes measures like access controls to facilities and equipment, the use of surveillance systems, and environmental controls to prevent damage to data. This could involve using keycard access to server rooms or ensuring that laptops containing ePHI are secured when not in use.
- Technical Safeguards: These are technical measures used to protect ePHI. Key examples include access control (usernames and passwords, multi-factor authentication), audit controls (tracking access to ePHI), integrity controls (preventing unauthorized changes to data), and encryption (protecting data at rest and in transit). A clinic might use strong encryption to protect patient data stored on its servers and employ multi-factor authentication to prevent unauthorized logins.
These three categories work together to create a comprehensive security framework. A weakness in one area can compromise the entire system. Therefore, robust implementation across all three is critical.
Q 12. How do you conduct a HIPAA risk assessment?
A HIPAA risk assessment is a systematic process to identify potential threats and vulnerabilities to the confidentiality, integrity, and availability of ePHI. It’s not a one-time event; it should be a regular, ongoing process.
Here’s a step-by-step approach:
- Identify Assets: List all systems, devices, and processes that store, process, or transmit ePHI. This includes servers, workstations, mobile devices, email systems, and databases.
- Identify Threats: Determine potential threats to ePHI. These could include malware, hacking attempts, insider threats, natural disasters, and loss or theft of devices.
- Identify Vulnerabilities: Evaluate potential weaknesses in your systems and processes that could be exploited by threats. This might include weak passwords, lack of encryption, outdated software, or inadequate physical security.
- Assess Risks: Determine the likelihood and impact of each identified threat and vulnerability. This will help you prioritize risks.
- Develop Mitigation Strategies: Create plans to address the identified risks. This might involve implementing stronger security controls, improving employee training, or investing in new security technologies.
- Implement and Monitor: Implement the mitigation strategies and regularly monitor their effectiveness. The assessment should be an ongoing iterative process, adapting to changing threats and vulnerabilities.
Imagine a clinic conducting a risk assessment and discovering that their network lacks adequate firewall protection. This would be identified as a vulnerability, and a mitigation strategy would be to install and configure a robust firewall.
Q 13. What is a Business Associate Agreement (BAA) and why is it important?
A Business Associate Agreement (BAA) is a contract between a covered entity (like a hospital or doctor’s office) and a business associate (a third-party vendor who handles PHI on behalf of the covered entity). It’s crucial because it ensures the business associate complies with HIPAA’s requirements for protecting PHI.
Importance of a BAA:
- Legal Compliance: A BAA legally binds the business associate to comply with HIPAA’s requirements for safeguarding PHI. Without it, the covered entity is legally responsible for the business associate’s actions related to PHI.
- Data Security: A properly drafted BAA outlines the specific security measures that the business associate must implement to protect PHI, ensuring a consistent level of protection across the entire system.
- Liability: It clarifies the responsibilities and liabilities of both parties in case of a data breach or other HIPAA violation.
- Transparency: It establishes a clear framework for communication and cooperation between the covered entity and the business associate concerning PHI.
For example, if a hospital uses a cloud-based service to store patient records, it needs a BAA with the cloud provider to ensure that the provider complies with HIPAA regulations concerning the storage and protection of that data.
Q 14. Explain the concept of de-identification of PHI.
De-identification of PHI is the process of removing or altering identifying information from PHI so that it no longer identifies or can be reasonably linked to an individual. This allows for the use of data for research, public health purposes, or other activities while protecting individual privacy.
The HIPAA Privacy Rule outlines specific methods for de-identification, focusing on the removal of 18 identifiers, such as name, address, all elements of dates (except year), telephone numbers, fax numbers, email addresses, social security numbers, medical record numbers, health plan beneficiary numbers, account numbers, certificate/license numbers, vehicle identifiers and serial numbers, device identifiers and serial numbers, web universal resource locators (URLs), internet protocol (IP) address numbers, biometric identifiers, full-face photographic images and any comparable images, and any other unique identifying number, characteristic, or code.
There are two main approaches to de-identification:
- Removal of Identifiers: Directly removing all 18 identifiers from the data set.
- Safe Harbor Method: This method ensures that the remaining data cannot be reasonably linked to an individual by applying specific statistical safeguards to the data.
However, even after de-identification, careful consideration must be given to the potential for re-identification, especially with the use of sophisticated data analysis techniques. A dataset might appear de-identified but still be vulnerable if combined with other datasets, creating a risk of re-identification.
Q 15. What are the requirements for HIPAA compliant data storage and disposal?
HIPAA compliant data storage and disposal requires a multi-faceted approach ensuring the confidentiality, integrity, and availability of protected health information (PHI). This begins with choosing secure storage methods. For electronic PHI, this means encryption both in transit (during transmission) and at rest (when stored). Think of it like using a locked safe for your most valuable documents – only authorized individuals with the correct key (access credentials) can open it.
- Data Storage: This includes using encrypted hard drives, cloud storage with robust security measures (including business associate agreements with the cloud provider), and access control lists that limit access to only authorized personnel. Regular audits and vulnerability scans are critical to identify and mitigate potential risks.
- Data Disposal: When disposing of PHI, whether electronic or paper-based, secure destruction is paramount. This prevents unauthorized access. For electronic data, this involves secure deletion methods, data sanitization, or physical destruction of storage media. For paper records, this means shredding to comply with industry standards. Always follow your organization’s documented policies and procedures.
For example, imagine a clinic transitioning to a new electronic health record system. They must ensure that all PHI on the old system is securely erased or transferred using encrypted methods before decommissioning the system. Similarly, any printed documents containing PHI should be shredded before disposal.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you handle a potential HIPAA breach?
Handling a potential HIPAA breach involves a swift and organized response. Speed is crucial; the longer you wait, the more extensive the damage could be. A documented incident response plan is essential. The first step involves identifying the breach – understanding what happened, what data was compromised, and how it happened. Then, contain the breach to prevent further damage.
Next, notify affected individuals and the OCR as required. This notification process has specific timelines dictated by HIPAA. After notification, we launch a thorough investigation. We document everything: timeline of events, involved parties, and corrective actions taken. We then implement measures to prevent future occurrences. This might include retraining staff, improving security protocols, or updating technology. Finally, we conduct a thorough review of our incident response plan to identify areas for improvement.
Imagine a laptop containing patient data is stolen from a doctor’s car. The immediate response includes disabling remote access to the laptop, reporting the theft to the authorities, and initiating a breach investigation. This scenario highlights the importance of robust security measures and incident reporting protocols.
Q 17. What are the key elements of a HIPAA compliant incident response plan?
A HIPAA-compliant incident response plan is a detailed roadmap for handling data breaches. It’s not just a document, but a living plan that’s regularly reviewed and updated. Key elements include:
- Risk Assessment: Identifying vulnerabilities and potential threats.
- Incident Response Team: Defining roles and responsibilities for each member.
- Incident Reporting Procedures: Clear steps on how to report suspected or confirmed breaches, including internal and external notification processes.
- Data Breach Investigation Procedures: A detailed method for identifying the scope, cause, and impact of the breach.
- Remediation and Recovery Plan: Steps to take to correct the problem, recover data, and prevent future breaches.
- Notification Procedures: Guidelines for notifying individuals whose PHI was compromised and the OCR.
- Post-Incident Review: Analyzing what happened, identifying areas for improvement in our security measures and protocols.
The plan should be regularly tested through tabletop exercises or simulations to ensure its effectiveness and to identify weaknesses.
Q 18. Explain the role of the Office for Civil Rights (OCR) in enforcing HIPAA.
The Office for Civil Rights (OCR) is the enforcement arm of HIPAA. They investigate complaints of HIPAA violations, conduct audits, and impose penalties on organizations that fail to comply. Their role ensures accountability and helps maintain the privacy and security of PHI. They have the authority to investigate and enforce compliance across various sectors, such as healthcare providers, health plans, and business associates. This includes initiating investigations based on complaints received or through their own audits.
If a violation is found, the OCR may take action such as issuing corrective action plans, issuing monetary penalties, or even pursuing civil action. The OCR plays a critical role in maintaining trust in the healthcare system by fostering compliance with HIPAA’s standards.
Q 19. How do you train staff on HIPAA compliance?
HIPAA training must be comprehensive, engaging, and regularly updated. It shouldn’t be a one-time event but an ongoing process. Methods include interactive online modules, in-person workshops, and scenario-based training that allows staff to practice applying their knowledge. The training should cover all aspects of HIPAA, including the Privacy Rule, the Security Rule, and the Breach Notification Rule. It needs to be tailored to the specific roles and responsibilities of each employee. For example, a receptionist’s training will differ from a physician’s.
Crucially, training should be assessed to ensure comprehension, using quizzes, tests, or performance evaluations. Documentation is key; we maintain records of all training completed by each staff member. Regular refreshers and updates are necessary to keep up with changes in regulations and best practices.
Imagine using a gamified online training platform, where staff can work through interactive modules and earn badges for completing training modules. This makes the learning process engaging and ensures active participation.
Q 20. What are some common HIPAA violations and how to avoid them?
Common HIPAA violations often stem from negligence or lack of awareness. Some examples include:
- Improper disposal of PHI: Failing to securely shred or destroy paper documents or properly sanitize electronic media.
- Unauthorized access to PHI: Allowing unauthorized personnel to access PHI, such as leaving computers unlocked or failing to implement strong password policies.
- Lack of employee training: Failing to provide adequate HIPAA training to employees.
- Failure to implement security measures: Not implementing appropriate security measures such as firewalls and intrusion detection systems.
- Improper use of mobile devices: Using unsecured mobile devices to access or transmit PHI.
To avoid these violations, organizations must develop and implement robust policies and procedures, provide comprehensive training, and regularly monitor compliance. Think of it like building a strong house; you need a solid foundation, secure walls, and reliable locks to protect the valuable contents inside. The same principles apply to protecting PHI.
Q 21. Explain the differences between permitted disclosures and required disclosures under HIPAA.
HIPAA distinguishes between permitted and required disclosures of PHI. Permitted disclosures allow the release of PHI under specific circumstances, such as when an individual authorizes the release or when it’s needed for treatment, payment, or healthcare operations (TPO). Required disclosures mandate the release of PHI under specific circumstances, such as in response to a valid court order or to report certain types of abuse or neglect.
Permitted Disclosures: These are generally authorized by the individual or fall under the TPO exception. For example, a patient can authorize their physician to share their records with another healthcare provider. Sharing PHI for treatment (e.g., consulting a specialist), payment (e.g., billing insurance), or healthcare operations (e.g., quality assurance) is also permitted under HIPAA.
Required Disclosures: These are mandated by law, regardless of patient authorization. This includes situations like responding to a subpoena, reporting suspected child abuse, or complying with public health reporting requirements. The key distinction lies in the legal obligation. Permitted disclosures are allowed but not required, while required disclosures are mandatory due to legal or public health obligations.
Q 22. What are your strategies for maintaining ongoing HIPAA compliance?
Maintaining ongoing HIPAA compliance is a continuous process, not a one-time event. Think of it like regularly servicing your car – you don’t just do it once and forget. My strategy involves several key components:
Regular Training and Education: Annual HIPAA training is a must, but it shouldn’t be a check-the-box exercise. I incorporate regular refresher courses, interactive modules, and scenario-based training to keep the information fresh and relevant. I also tailor training to specific roles and responsibilities, ensuring that staff understand their unique HIPAA obligations. For instance, a billing clerk’s training will differ from that of a physician.
Policy and Procedure Updates: HIPAA regulations evolve. I regularly review and update our organization’s policies and procedures to reflect these changes. This includes reviewing access controls, data encryption methods, and breach notification plans. It’s crucial to document these updates and ensure everyone is aware of the modifications.
Risk Assessments and Audits: Regular risk assessments help identify vulnerabilities in our systems and processes. I conduct these assessments at least annually, focusing on areas like data storage, access controls, and employee practices. Internal audits, performed by trained personnel or external experts, provide an objective view of our compliance status and highlight areas for improvement.
Incident Response Plan: A well-defined incident response plan is critical. This plan outlines the steps to take in the event of a HIPAA violation or security breach. This isn’t just a document; it requires regular testing and training to ensure everyone knows their roles and responsibilities in a real-world emergency. Think of it as a fire drill for data security.
Vendor Management: We carefully vet and monitor our vendors who handle protected health information (PHI). This includes ensuring they have their own robust HIPAA compliance programs in place and that our contracts include strong data protection clauses.
Q 23. Describe your experience with HIPAA audits and investigations.
I have extensive experience with HIPAA audits and investigations, both from the perspective of preparing for them and responding to them. I’ve been involved in several internal audits and have worked closely with external auditors. My approach always focuses on proactive compliance. Preparation is key!
During an audit or investigation, my focus is on transparency and collaboration. This includes:
Documenting Policies and Procedures: Maintaining meticulous documentation of our HIPAA compliance program is crucial. This includes policies, procedures, training records, risk assessments, and audit results. Think of this as your ‘evidence file’ showing your commitment to compliance.
Data Access Controls: Demonstrating robust data access controls is essential. This involves showing how we limit access to PHI based on the principle of least privilege – only those who need access have it, and their access is regularly reviewed.
Incident Response: If a breach or violation has occurred, a detailed, documented response is vital, clearly outlining the steps taken to contain the situation and mitigate any harm. We detail how we investigated the incident, notified affected individuals and the government as needed (if applicable), and what corrective actions have been implemented.
My experience has taught me the importance of thorough documentation, proactive risk management, and a culture of compliance. A successful audit isn’t just about passing; it’s about demonstrating a commitment to protecting patient information.
Q 24. How do you stay updated on HIPAA regulations and changes?
Staying updated on HIPAA regulations and changes is paramount. It’s a dynamic landscape. My approach is multifaceted:
Subscription to Regulatory Updates: I subscribe to reputable sources like the HHS website and newsletters from compliance experts. This ensures I receive timely notifications of rule changes and guidance updates.
Professional Organizations: Active participation in professional organizations dedicated to healthcare compliance and privacy keeps me abreast of industry best practices and emerging trends. Conferences and webinars are invaluable for networking and learning from experts.
Legal Counsel: I maintain close communication with legal counsel specializing in HIPAA compliance to get clarity on complex issues and ensure we are interpreting regulations correctly. They provide invaluable insight and guidance.
Continuous Monitoring: I continuously monitor relevant news and publications to stay informed about enforcement actions, emerging threats, and evolving technologies that impact HIPAA compliance. This proactive approach allows us to anticipate potential issues and adapt our strategies accordingly.
Q 25. What is your understanding of HIPAA Omnibus Rule?
The HIPAA Omnibus Rule, enacted in 2013, significantly expanded the scope of HIPAA regulations. It’s like a major software update for HIPAA. Key changes include:
Business Associate (BA) Provisions: The Omnibus Rule strengthened the accountability of business associates who handle PHI on behalf of covered entities. It clarified their responsibilities for compliance and imposed stricter penalties for violations.
Breach Notification Rules: The rule clarified and strengthened breach notification requirements, making it clearer when and how organizations must notify individuals and the government about data breaches.
Genetic Information Nondiscrimination Act (GINA) Protections: The Omnibus Rule integrated protections under GINA, ensuring that genetic information is treated as PHI and is protected under HIPAA.
Enforcement Actions: The Omnibus Rule increased the potential penalties for HIPAA violations, significantly raising the stakes for non-compliance. This emphasizes the importance of robust compliance programs.
Understanding the Omnibus Rule is critical because it significantly increased the responsibilities and liabilities associated with handling PHI. Ignoring it isn’t an option.
Q 26. Explain your approach to managing HIPAA related risks and vulnerabilities.
Managing HIPAA-related risks and vulnerabilities requires a proactive and multi-layered approach. My approach focuses on:
Risk Assessment: Regular risk assessments are the cornerstone of this process. We identify potential vulnerabilities in our systems, processes, and employee practices. This involves examining everything from physical security to data access controls and employee training.
Mitigation Strategies: Once vulnerabilities are identified, we develop and implement mitigation strategies to address them. This might include implementing stronger access controls, encrypting data, conducting regular security awareness training, and using multi-factor authentication.
Data Security Measures: We use a variety of security measures to protect PHI, including encryption, access controls, audit trails, and intrusion detection systems. Think of this like building a multi-layered security fortress around patient data.
Employee Training: Training is crucial in mitigating risk. Our employees are trained on appropriate handling of PHI, security protocols, and the importance of reporting any suspicious activity. This isn’t a one-time event; it’s ongoing.
Incident Response Plan: A well-defined incident response plan is essential for effectively handling security breaches or other incidents. This plan outlines the steps to take, from initial detection to notification and remediation.
Risk management isn’t about eliminating all risk; it’s about proactively identifying, mitigating, and managing the risks to an acceptable level. It’s a constant process of evaluation and adaptation.
Q 27. How would you handle a situation where a staff member violates HIPAA policy?
Handling a situation where a staff member violates HIPAA policy requires a structured and fair approach. My response would involve:
Investigation: A thorough investigation is the first step. This involves gathering all the facts, interviewing relevant personnel, and reviewing any relevant documentation. The goal is to understand the nature and extent of the violation.
Disciplinary Action: Based on the findings of the investigation, appropriate disciplinary action would be taken. This could range from mandatory retraining to suspension or termination, depending on the severity of the violation. The action should be consistent with organizational policies and relevant regulations.
Reporting: Depending on the circumstances, the violation may need to be reported to the appropriate authorities, such as the Office for Civil Rights (OCR). This is particularly true in cases involving a breach of unsecured protected health information.
Remediation: Corrective actions are implemented to prevent future violations. This might involve updating policies, improving training, or enhancing security measures. The goal is to learn from the mistake and strengthen the overall compliance program.
Documentation: Meticulous documentation of the entire process is crucial, including the investigation findings, disciplinary actions taken, and corrective actions implemented. This documentation is important for both internal review and potential external audits.
The key is to address the violation swiftly, fairly, and effectively while prioritizing the protection of patient information and maintaining a culture of compliance.
Key Topics to Learn for HIPAA Training Interview
- The HIPAA Privacy Rule: Understanding protected health information (PHI), permitted disclosures, and patient rights. Practical application: Analyzing scenarios to determine appropriate PHI handling.
- The HIPAA Security Rule: Administrative, physical, and technical safeguards for ePHI. Practical application: Evaluating the security of a hypothetical healthcare system’s electronic data storage.
- HIPAA Breach Notification: Procedures for identifying, reporting, and mitigating data breaches. Practical application: Developing a response plan for a simulated breach scenario.
- HIPAA Enforcement and Penalties: Understanding the consequences of non-compliance. Practical application: Assessing the potential risks and liabilities associated with various HIPAA violations.
- The HIPAA Omnibus Rule: Understanding its impact on business associates and the expansion of privacy protections. Practical application: Analyzing how the Omnibus Rule affects data sharing agreements.
- HIPAA Compliance Best Practices: Proactive measures to ensure ongoing compliance. Practical application: Designing a HIPAA compliance training program for a healthcare organization.
Next Steps
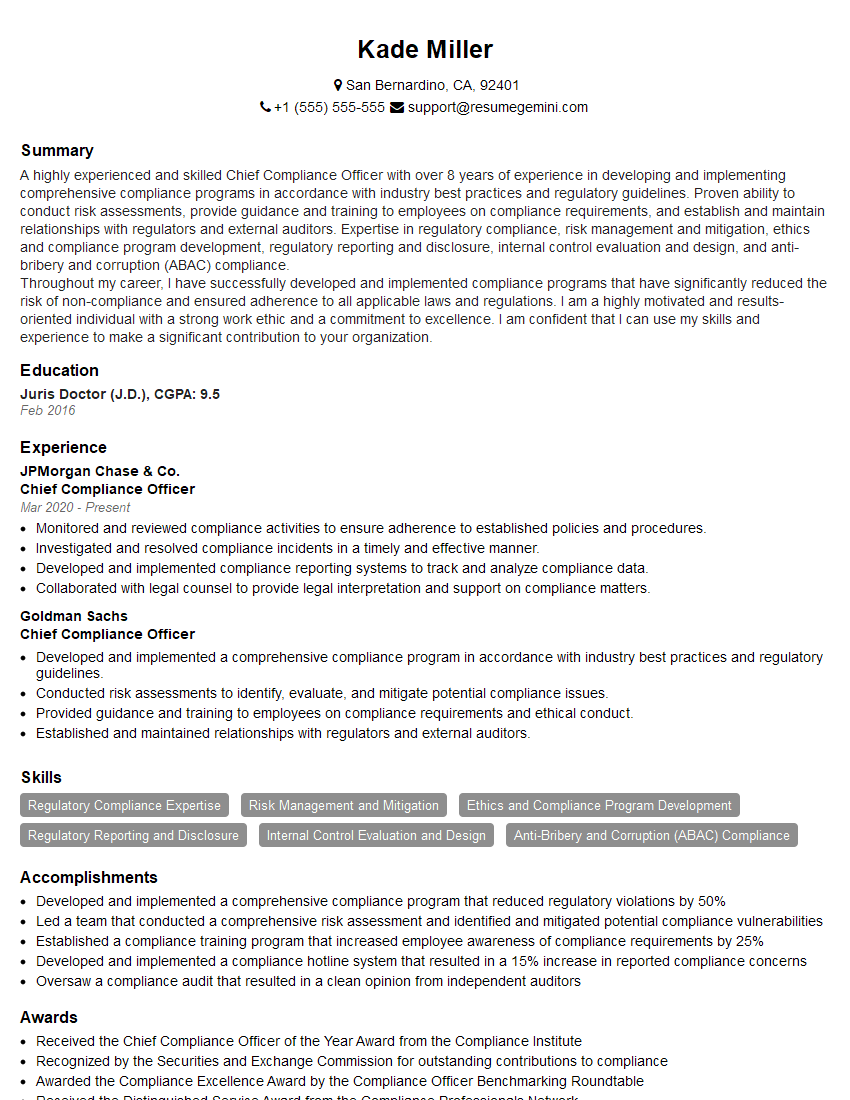
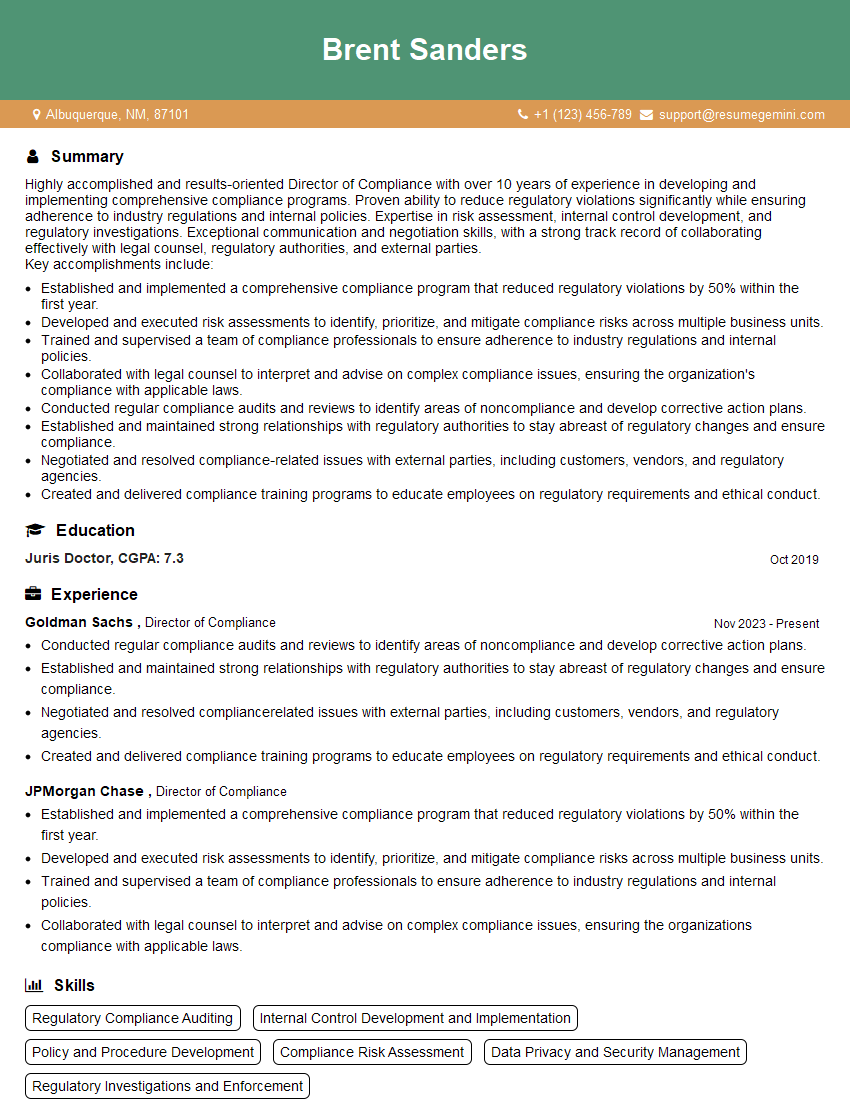
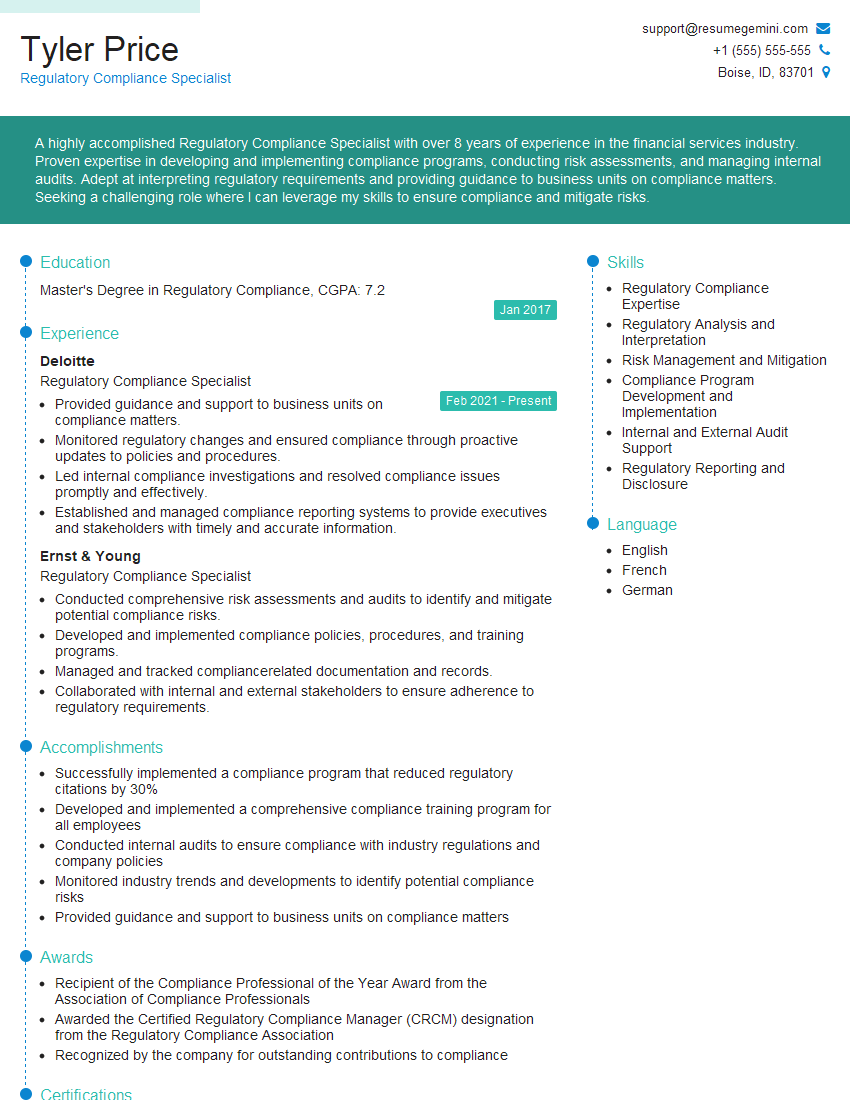
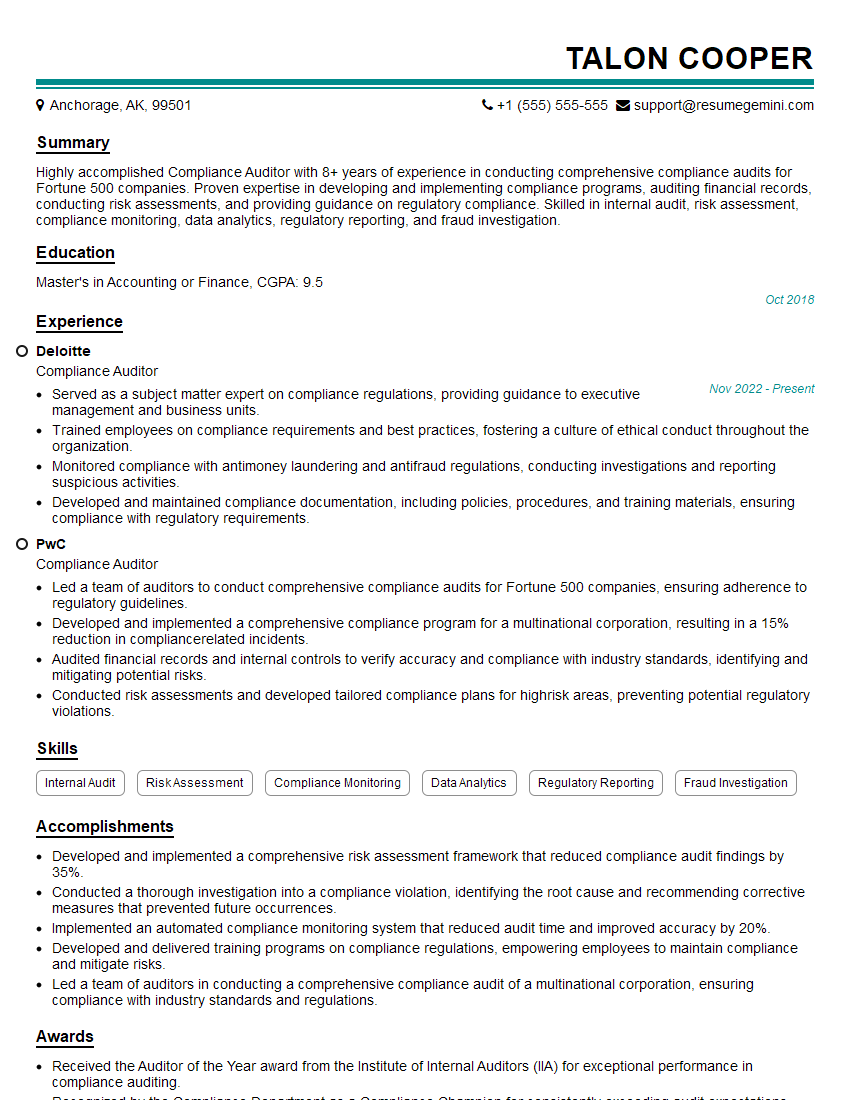
Mastering HIPAA training significantly enhances your career prospects in healthcare, opening doors to rewarding roles with increased responsibility and compensation. To maximize your chances of landing your dream job, creating a strong, ATS-friendly resume is crucial. ResumeGemini is a trusted resource that can help you build a professional resume that highlights your HIPAA expertise and catches the eye of recruiters. We offer examples of resumes tailored to HIPAA Training to help guide you. Invest the time to craft a compelling resume – it’s a vital step in your job search journey.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO