The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Medical Lab Technician interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Medical Lab Technician Interview
Q 1. Explain the process of performing a complete blood count (CBC).
A Complete Blood Count (CBC) is a comprehensive blood test that provides information about various components of your blood. It’s like a blood health check-up! The process begins with obtaining a blood sample, usually through venipuncture. This sample is then analyzed using automated hematology analyzers. These sophisticated machines count and measure different blood cells: red blood cells (RBCs), white blood cells (WBCs), and platelets.
Here’s a breakdown of the process:
- Sample Collection: A small amount of blood is drawn from a vein, typically in the arm.
- Automated Analysis: The sample is loaded into an automated hematology analyzer, which uses sophisticated techniques like impedance and flow cytometry to count and size the various blood cells.
- Data Interpretation: The analyzer provides numerical results for numerous parameters including:
- RBC count: Number of red blood cells per microliter of blood.
- Hemoglobin (Hb): Amount of oxygen-carrying protein in the blood.
- Hematocrit (Hct): Percentage of blood volume occupied by red blood cells.
- Mean Corpuscular Volume (MCV): Average size of red blood cells.
- Mean Corpuscular Hemoglobin (MCH): Average amount of hemoglobin in each red blood cell.
- Mean Corpuscular Hemoglobin Concentration (MCHC): Average concentration of hemoglobin in each red blood cell.
- Red Cell Distribution Width (RDW): Variation in the size of red blood cells.
- WBC count: Number of white blood cells per microliter of blood, often further differentiated into various types (neutrophils, lymphocytes, monocytes, eosinophils, basophils).
- Platelet count: Number of platelets per microliter of blood.
- Manual Review (if needed): In some cases, a microscopic review of a blood smear may be necessary to confirm automated results or to investigate unusual findings.
- Reporting: The results are then reviewed by a medical laboratory professional and reported to the physician.
For example, an abnormally low RBC count might suggest anemia, while an elevated WBC count could point to an infection. The complete CBC, with its many parameters, paints a detailed picture of a patient’s overall hematologic status.
Q 2. Describe the proper technique for venipuncture.
Venipuncture, the process of drawing blood from a vein, requires meticulous technique to ensure patient safety and sample integrity. Think of it like a precise surgical procedure, even though it’s a common practice.
Proper technique involves these steps:
- Preparation: Gather all necessary supplies (gloves, tourniquet, antiseptic wipes, needles, tubes, gauze pads). Verify patient identity using two identifiers.
- Patient Positioning: Have the patient extend their arm and locate a suitable vein, usually in the antecubital fossa (the inner elbow area). A plump vein is the ideal target.
- Tourniquet Application: Apply the tourniquet 4-6 inches above the puncture site, snugly but not too tightly. It should temporarily restrict blood flow, making the veins more prominent.
- Antisepsis: Cleanse the puncture site with an antiseptic solution in a concentric circular motion, allowing it to air dry completely. This prevents contamination of the sample.
- Venipuncture: Insert the needle into the vein at a 15-30 degree angle, bevel up, with a smooth, swift motion. Observe for a flashback of blood in the hub of the needle. This signifies successful entry into the vein.
- Sample Collection: Collect the appropriate blood samples in the correct order (according to specific tube additive requirements). Remove the tourniquet once the samples are collected.
- Post-Procedure: Apply pressure to the puncture site with a gauze pad for at least 2-3 minutes, until bleeding has completely stopped. Proper pressure is vital to prevent hematoma (a collection of blood under the skin).
- Disposal: Dispose of used needles and other sharps immediately in an appropriate sharps container.
A common error is inserting the needle at too steep of an angle or failing to maintain adequate pressure after the procedure. These errors can lead to hematoma formation or even vein damage.
Q 3. What are the different types of blood collection tubes and their uses?
Different colored blood collection tubes contain various additives that are crucial for specific tests. Choosing the wrong tube can ruin a sample!
Here are some common types:
- Red-top tubes (no additive): Used for serum tests (e.g., cholesterol, glucose). The blood clots naturally within the tube. The serum, the liquid portion of the blood after clotting, is separated by centrifugation (spinning at high speed).
- Gold or tiger-top tubes (serum separator tube): Similar to red-top tubes, but contain a gel that separates serum from blood cells during centrifugation. This simplifies serum extraction and processing.
- Lavender-top tubes (EDTA): Contain ethylenediaminetetraacetic acid (EDTA), an anticoagulant that prevents blood clotting. Used for hematology tests (e.g., CBC) since it preserves the cellular components.
- Light blue-top tubes (sodium citrate): Contain sodium citrate, another anticoagulant, used for coagulation studies (e.g., PT/INR, aPTT) to assess blood-clotting ability.
- Green-top tubes (heparin): Contain heparin, an anticoagulant, used for tests requiring plasma (e.g., chemistry tests) and helps prevent blood from clotting. Plasma is the liquid portion of the blood that contains clotting factors.
- Gray-top tubes (sodium fluoride/potassium oxalate): Contain both sodium fluoride and potassium oxalate; the fluoride prevents glycolysis (breakdown of glucose) and the oxalate is an anticoagulant. Used for glucose testing as it preserves glucose levels.
Always ensure the correct tube is used for the right test; otherwise, results could be inaccurate and potentially harmful. For instance, using a lavender tube for a coagulation study would yield meaningless results.
Q 4. How do you identify and handle a hemolyzed blood sample?
Hemolysis refers to the rupture of red blood cells, resulting in the release of hemoglobin into the plasma. This causes the sample to turn pink or red and can significantly interfere with many laboratory tests. It’s like spilling the contents of the red blood cells into the surrounding liquid.
Identifying hemolysis is straightforward: visually inspect the sample; hemolyzed samples appear reddish or pinkish.
Handling hemolyzed samples:
- Reject the Sample: Most importantly, a severely hemolyzed sample should be rejected and a new sample should be collected. Hemolysis can dramatically alter test results, making them unreliable.
- Document the Observation: Record the observation in the laboratory information system, detailing the degree of hemolysis (e.g., slight, moderate, severe). This is crucial for quality control and tracking purposes.
- Investigate the Cause: Determine what caused the hemolysis. This may involve reviewing the venipuncture technique, the integrity of the needle or tube, or the handling of the sample after collection.
- Repeat the Test (if possible): If the hemolysis is slight, and the test is not highly sensitive to hemolysis, the test might be repeated with careful attention to avoiding any potential causes of hemolysis.
Hemolysis can occur due to several factors, including improper venipuncture technique (too forceful aspiration of blood into the syringe, drawing blood through a damaged vein), prolonged tourniquet application, or rough handling of the sample. It’s essential to prevent hemolysis, as it compromises the accuracy and reliability of numerous laboratory tests.
Q 5. Explain the importance of quality control in medical laboratory testing.
Quality control (QC) in medical laboratory testing is paramount to ensure accuracy and reliability of results. It’s the backbone of trust in medical diagnostics. Think of it as continuously verifying the instruments are playing the right notes.
Importance of QC:
- Accuracy of Results: QC procedures identify and correct instrument errors, reagent problems, or variations in techniques, ensuring accurate and reliable patient results.
- Patient Safety: Accurate test results directly impact patient care and treatment decisions. Incorrect results can lead to wrong diagnoses or inappropriate therapies with potentially harmful consequences.
- Legal and Regulatory Compliance: Accredited medical laboratories are held to strict QC standards outlined by regulatory bodies, like the Clinical Laboratory Improvement Amendments (CLIA) in the U.S. Maintaining these standards is essential for legal compliance.
- Maintaining Confidence: Robust QC practices build confidence in the laboratory’s performance and ensure that the results are trustworthy and reliable for physicians.
QC procedures involve several steps:
- Use of Control Materials: Running controls, which are samples with known values, alongside patient specimens. These control results are compared to expected ranges. Deviations from expected values trigger investigation of the problem and corrective actions.
- Calibration of Instruments: Regularly calibrating analytical instruments to ensure they are performing within specified limits.
- Proficiency Testing: Participating in external quality assessment (EQA) programs, where laboratories are sent unknown samples to analyze. Results are compared to other labs to ensure consistency and accuracy.
- Preventive Maintenance: Regular maintenance and calibration of equipment prevent failures and maintain optimal performance.
- Documentation: Thorough documentation of all QC procedures, results, and any corrective actions taken.
A well-established QC program is crucial for producing high-quality results and maintaining the integrity of a medical laboratory.
Q 6. Describe the different types of microscopes used in a medical laboratory.
Microscopes are essential tools in medical laboratories, used for visualizing microorganisms, cells, and tissues. Different types of microscopes provide unique capabilities, enhancing diagnostic possibilities. It’s like having multiple sets of eyes with varying powers of magnification.
Types of microscopes commonly used in medical labs:
- Bright-field microscope: The most common type, using visible light to illuminate the specimen. It provides a simple and clear view of stained specimens. This is excellent for looking at blood smears, bacterial cultures, and tissue sections.
- Phase-contrast microscope: Used to view unstained specimens, making it suitable for live cell observation. It enhances the contrast of transparent structures by exploiting differences in refractive index. This is frequently used in observing living cells or unstained microorganisms.
- Fluorescence microscope: Uses ultraviolet light and fluorescent dyes to visualize specific structures or molecules within the specimen. This is excellent for immunofluorescence techniques and other specialized staining procedures.
- Electron microscope (Transmission and Scanning): Electron microscopes use a beam of electrons instead of light to achieve far higher magnification than light microscopes. Transmission electron microscopy (TEM) provides extremely high resolution images suitable for detailed visualization of cellular ultrastructure. Scanning electron microscopy (SEM) creates 3D images of the specimen’s surface.
The choice of microscope depends on the type of specimen and the information being sought. For instance, a bright-field microscope is sufficient for examining stained blood smears, while a fluorescence microscope is needed for immunofluorescence studies.
Q 7. What are the safety precautions you take when handling biological specimens?
Safety is paramount when handling biological specimens, as they may contain infectious agents. Following established protocols is non-negotiable to protect both the laboratory staff and the community. Imagine working with invisible dangers.
Safety precautions:
- Personal Protective Equipment (PPE): Always wear appropriate PPE, including gloves, lab coats, eye protection, and face masks, depending on the type of specimen being handled. This forms a protective barrier between you and potentially infectious materials.
- Standard Precautions: Treat all specimens as potentially infectious and follow standard precautions, including hand hygiene, proper disposal of sharps and waste, and maintaining a clean workspace. The better prepared you are, the safer you will be.
- Biosafety Cabinets: Use biosafety cabinets (BSC) for handling high-risk biological agents. These enclosures provide a safe environment with HEPA filtration to prevent the release of airborne pathogens. BSCs are essential when handling highly infectious samples.
- Sharps Disposal: Properly dispose of all sharp instruments (needles, slides) immediately after use in designated sharps containers. This prevents accidental needlesticks and protects others from injury.
- Spill Management: Have a well-defined procedure to handle spills of infectious materials. This usually includes the use of appropriate disinfectants and absorbent materials to safely neutralize and clean the spill.
- Proper Labeling and Handling: Ensure all specimens are properly labeled with patient identifiers and any necessary biohazard warnings. Handle specimens with care to prevent breakage and spills.
- Training and Education: Ongoing training on safe laboratory practices, including infection control and handling of hazardous materials is essential. Safety training and procedures are reviewed regularly.
Adherence to these precautions is crucial for preventing the transmission of infectious diseases and maintaining a safe working environment in the medical laboratory.
Q 8. How do you prepare a blood smear for microscopic examination?
Preparing a blood smear is a crucial step in hematology, allowing for microscopic examination of blood cells. It involves creating a thin, even layer of blood on a microscope slide, enabling clear visualization of individual cells and their morphology. The process begins with collecting a small blood sample, usually via a fingerstick or venipuncture. Then:
- Slide Preparation: A clean microscope slide is placed on a flat surface.
- Blood Application: A small drop of blood is placed near one end of the slide.
- Spreader Slide: A second clean slide (the spreader slide) is held at a 30-45 degree angle to the first slide and pushed smoothly across the drop of blood. The blood spreads along the edge of the spreader slide, creating a feathered edge.
- Air Drying: The slide is allowed to air dry completely before staining.
- Staining: Once dry, the blood smear is stained using a suitable stain, such as Wright-Giemsa stain, to highlight cellular components and differentiate cell types. This staining process reveals the cellular details crucial for diagnosis.
Think of it like spreading butter on toast – you want an even, thin layer for optimal viewing. An uneven smear can make it difficult to identify abnormalities in cell size, shape, or number. In my experience, consistent practice leads to high-quality smears, essential for accurate diagnosis of conditions like anemia or leukemia.
Q 9. Explain the principle of ELISA testing.
ELISA, or Enzyme-Linked Immunosorbent Assay, is a powerful laboratory technique used to detect and quantify substances, typically proteins, in a liquid sample. It works on the principle of antigen-antibody binding. Imagine a lock (antigen) and a key (antibody). If the key fits the lock, a signal is produced.
The process involves coating a plate with an antigen (or antibody). A sample containing the target substance (e.g., a virus or hormone) is then added. If the target is present, it binds to the coated antigen. Next, an enzyme-linked antibody specific to the target is added. This antibody binds to the target-antigen complex. Finally, a substrate is added, causing the enzyme to produce a color change, the intensity of which is proportional to the amount of the target substance present. This color change is measured using a spectrophotometer, providing quantitative results.
ELISA is widely used in various applications, from diagnosing infectious diseases (like HIV) to detecting food allergens. The results are easily interpreted, offering both qualitative (positive or negative) and quantitative (amount present) information.
Q 10. Describe your experience with automated analyzers.
Throughout my career, I’ve extensively utilized various automated analyzers, including hematology analyzers (e.g., Sysmex, Beckman Coulter), chemistry analyzers (e.g., Roche Cobas), and immunoassay analyzers (e.g., Siemens). My experience encompasses all aspects of their operation: pre-analytical processes (sample preparation, handling), analytical phases (running the tests), and post-analytical phases (result verification, quality control).
I’m proficient in loading samples, performing instrument maintenance (following manufacturer’s guidelines), troubleshooting malfunctions, and interpreting quality control data. I’m adept at using the software associated with these analyzers to review results, flag outliers, and generate reports. For example, I regularly performed preventative maintenance on our Sysmex hematology analyzer, ensuring its accuracy and efficiency. In one instance, I quickly identified a malfunction in the reagent delivery system of our chemistry analyzer, preventing the generation of erroneous results. My training includes understanding the analytical methodologies used by these instruments, allowing me to interpret data critically.
Q 11. How do you troubleshoot common issues with laboratory equipment?
Troubleshooting laboratory equipment requires a systematic approach. My strategy involves:
- Identify the problem: What exactly is malfunctioning? Note any error messages displayed.
- Check the basics: Are the reagents fresh? Is the power cord plugged in? Are there any obvious blockages?
- Consult the manual: The instrument’s manual provides detailed troubleshooting guides and error codes.
- Perform routine checks: Regular preventative maintenance can prevent many issues. This includes cleaning, calibrating, and verifying the functionality of components.
- Contact technical support: If the issue persists, it’s crucial to contact the manufacturer’s technical support team.
- Document everything: Maintaining a detailed log of all troubleshooting steps, including the problem, solutions attempted, and outcomes, is essential.
For instance, when our centrifuge started making unusual noises, I first checked its balance and then consulted the manual. I found the problem was a loose component, which I carefully tightened, resolving the issue. In a separate instance, a recurring error on our automated analyzer was traced to a sensor issue – a problem quickly resolved with the manufacturer’s guidance.
Q 12. What are the normal ranges for key blood parameters (e.g., glucose, cholesterol)?
Normal ranges for blood parameters vary slightly depending on factors such as age, sex, and laboratory methods. However, typical ranges are:
- Glucose (fasting): 70-100 mg/dL
- Total Cholesterol: < 200 mg/dL
- HDL Cholesterol (good cholesterol): > 40 mg/dL (men), > 50 mg/dL (women)
- LDL Cholesterol (bad cholesterol): < 100 mg/dL (optimal)
- Triglycerides: < 150 mg/dL
It’s crucial to note that these are general ranges and interpretation requires considering the individual patient’s clinical picture and medical history. Results outside the normal range may indicate various conditions, prompting further investigation. For example, high glucose levels could suggest diabetes, while high cholesterol might indicate an increased risk of cardiovascular disease. A complete blood count (CBC) also provides further critical information.
Q 13. Explain the different types of urine tests and their clinical significance.
Urine tests are essential diagnostic tools providing valuable information about kidney function, metabolic processes, and the presence of infection or other diseases. Several types exist, including:
- Urinalysis (routine): This involves assessing the physical characteristics (color, clarity, odor), chemical components (pH, glucose, protein, ketones), and microscopic examination (cells, crystals, casts). It is a fundamental screening test.
- Culture and Sensitivity: This test identifies bacteria causing urinary tract infections (UTIs) and determines the antibiotics most effective against them. It plays a pivotal role in managing UTIs.
- Urine Chemistry Tests: These can detect specific substances such as glucose (diabetes), protein (kidney disease), or blood (kidney stones, infection).
- Microscopic Examination: Identifies cells (white blood cells indicating infection, red blood cells suggesting bleeding), casts (indicating kidney damage), and crystals (suggesting kidney stone formation).
For example, a urinalysis showing high levels of protein and red blood cells could indicate kidney disease. The clinical significance lies in its ability to provide early detection of various diseases and to guide further testing and treatment.
Q 14. Describe your experience with microbiology techniques (e.g., Gram staining, culturing).
My experience with microbiology techniques is extensive, encompassing both Gram staining and bacterial culturing. Gram staining is a crucial differential staining technique that distinguishes bacteria into Gram-positive (purple) and Gram-negative (pink) based on differences in their cell wall structure. This is crucial for initial bacterial identification and guiding antibiotic therapy. Culturing involves growing bacteria on various media to isolate and identify specific organisms.
I am proficient in performing Gram stains, interpreting the results, and selecting appropriate media for bacterial growth depending on the suspected organism. I’m also skilled in subculturing, performing biochemical tests, and using automated systems for bacterial identification. For example, I’ve worked extensively on isolating and identifying organisms from various clinical specimens like blood, urine, and wound swabs. Proper aseptic technique is crucial to prevent contamination during these procedures. My experience extends to working with anaerobic bacteria, requiring specialized techniques and media.
Q 15. How do you interpret a Gram stain result?
Gram staining is a crucial technique in microbiology used to differentiate bacteria based on their cell wall composition. It’s a differential staining method, meaning it uses multiple dyes to distinguish between different types of bacteria. The process involves applying crystal violet (primary stain), Gram’s iodine (mordant), decolorizer (usually alcohol or acetone), and safranin (counterstain).
Interpretation:
- Gram-positive bacteria: These bacteria retain the crystal violet dye, appearing purple or blue under the microscope. This is because they have a thick peptidoglycan layer in their cell wall, which traps the dye-iodine complex. Examples include Staphylococcus aureus and Streptococcus pneumoniae.
- Gram-negative bacteria: These bacteria lose the crystal violet dye during the decolorization step and take up the safranin counterstain, appearing pink or red. Their cell walls have a thinner peptidoglycan layer and an outer membrane that prevents the dye-iodine complex from being retained. Examples include Escherichia coli and Pseudomonas aeruginosa.
Practical Application: Knowing whether a bacteria is Gram-positive or Gram-negative is essential for guiding antibiotic treatment. For instance, Gram-positive bacteria are generally susceptible to penicillin, while Gram-negative bacteria often require different antibiotics.
For example, if a Gram stain reveals Gram-positive cocci in clusters, it strongly suggests Staphylococcus aureus, potentially causing a skin infection. Further tests would be required for confirmation, but the Gram stain provides a crucial initial clue.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain the principles of molecular diagnostic techniques (e.g., PCR).
Molecular diagnostic techniques, such as Polymerase Chain Reaction (PCR), are used to detect and identify specific DNA or RNA sequences in a sample. This allows for highly sensitive and specific detection of pathogens, genetic mutations, and other analytes.
Principles of PCR: PCR amplifies a specific DNA sequence exponentially using three main steps that are repeated many times:
- Denaturation: Heating the DNA to separate the double strands.
- Annealing: Cooling to allow short DNA sequences called primers to bind to complementary sequences on the DNA template.
- Extension: Using a DNA polymerase enzyme to synthesize new DNA strands complementary to the template DNA, extending from the primers.
Each cycle doubles the amount of target DNA. This process allows even tiny amounts of target DNA to be detected. Different types of PCR exist, like real-time PCR (qPCR), which allows for quantitative measurement of the target DNA.
Practical Application: PCR is widely used in infectious disease diagnosis (e.g., detecting viral load in HIV patients), genetic testing (e.g., identifying cystic fibrosis mutations), and forensic science. For example, PCR is used to detect COVID-19 virus RNA from patient samples.
Q 17. What is the role of a Medical Lab Technician in infection control?
Medical Lab Technicians play a vital role in infection control by ensuring the safe handling of potentially infectious specimens. This involves adhering to strict protocols to prevent the spread of infections both within the laboratory and to the wider community.
Specific roles include:
- Proper specimen handling: Following standard operating procedures for receiving, processing, and storing specimens, including using appropriate personal protective equipment (PPE) like gloves, masks, and eye protection.
- Decontamination and sterilization: Ensuring work surfaces, equipment, and instruments are properly decontaminated and sterilized to eliminate potential pathogens.
- Waste disposal: Correctly disposing of infectious waste according to established guidelines and regulations.
- Quality control: Participating in quality control programs to ensure the reliability and accuracy of tests, reducing the risk of false-positive or false-negative results that could impact infection control measures.
- Reporting: Reporting suspected outbreaks or unusual laboratory findings to appropriate personnel to initiate timely interventions.
For example, a lab tech might immediately report a high number of positive results for a particular pathogen to the infection control officer in a hospital, triggering investigations and potentially preventing an outbreak.
Q 18. How do you ensure the accuracy and reliability of laboratory results?
Ensuring the accuracy and reliability of laboratory results is paramount. It involves a multi-faceted approach encompassing meticulous attention to detail at every step of the testing process.
Key strategies include:
- Proper specimen collection and handling: Correct identification of patients, appropriate collection techniques, and prompt transportation of specimens to prevent degradation or contamination.
- Calibration and maintenance of equipment: Regularly calibrating and maintaining laboratory instruments to guarantee their accurate functioning. This involves using certified reference materials and performing quality control checks.
- Adherence to standard operating procedures (SOPs): Following established SOPs for each test method to ensure consistency and reduce the likelihood of errors.
- Quality control (QC): Incorporating QC procedures at each phase, using control materials and proficiency testing to monitor accuracy and precision.
- Proficiency testing: Regularly participating in external proficiency testing programs to compare results with other laboratories and identify any potential biases or issues.
- Documentation: Maintaining detailed and accurate records of all procedures, results, and corrective actions taken.
For instance, if a QC sample consistently produces out-of-range results, this immediately triggers an investigation to identify and correct the problem, preventing the release of inaccurate patient results.
Q 19. What are the legal and ethical considerations in medical laboratory practice?
Medical laboratory practice is governed by stringent legal and ethical considerations, focusing on patient safety, confidentiality, and the integrity of results. These are crucial to maintaining public trust and upholding professional standards.
Legal considerations include:
- Compliance with regulations: Adhering to local, state, and federal regulations regarding laboratory safety, quality assurance, and patient privacy (e.g., HIPAA in the US).
- Proper handling of patient information: Maintaining patient confidentiality and adhering to data protection laws.
- Accurate reporting of results: Providing accurate and timely reports to healthcare providers, which can have significant legal repercussions if errors occur.
Ethical considerations include:
- Maintaining professional competence: Engaging in ongoing professional development to ensure proficiency and competence in performing laboratory procedures.
- Objectivity and integrity: Providing unbiased results and reporting findings honestly, avoiding conflicts of interest.
- Respect for patients’ rights: Respecting patients’ rights to privacy, informed consent, and access to their own health information.
A breach in confidentiality or an inaccurate test result could lead to legal action and severe reputational damage.
Q 20. Describe your experience with laboratory information systems (LIS).
Laboratory Information Systems (LIS) are crucial for managing and tracking laboratory data efficiently. My experience includes extensive use of LIS for specimen tracking, test ordering, result reporting, and quality control.
Specific functionalities I’m proficient with include:
- Specimen accessioning: Entering patient information, assigning unique identification numbers to samples, and managing sample workflow within the LIS.
- Test ordering and result entry: Entering test orders from physicians and entering the results generated by the lab analyses.
- Result verification and reporting: Reviewing results for accuracy and completeness before release to healthcare providers. This often includes flagging critical values or abnormalities.
- Quality control data entry and analysis: Entering and analyzing quality control data to monitor the performance of laboratory equipment and procedures.
- Generating reports: Generating reports for various purposes such as patient results, QC data summaries, and billing information.
I’m comfortable with various LIS platforms and can quickly adapt to new systems. For example, in my previous role, we transitioned to a new LIS, and I was instrumental in training my colleagues on the new system and ensuring a smooth transition.
Q 21. How do you maintain proper documentation and record-keeping in a laboratory?
Proper documentation and record-keeping are essential in a laboratory setting to ensure traceability, accuracy, and compliance with regulations. Maintaining meticulous records is crucial for quality control, patient safety, and legal protection.
Key aspects of proper documentation include:
- Accurate and legible handwriting or typed entries: All entries should be clear, concise, and legible. Corrections must be made properly, with the original entry still visible.
- Complete information: Recording all relevant details such as patient identification, test performed, date and time of testing, results, and any relevant observations.
- Chain of custody: Maintaining proper chain of custody for specimens, documenting every individual who handles the sample from collection to disposal. This is especially crucial for legal cases.
- Calibration and maintenance logs: Maintaining detailed logs for all equipment calibration and maintenance activities.
- Adherence to standard operating procedures (SOPs): Following SOPs for every test method and documenting any deviations or problems encountered.
- Use of LIS: Utilizing the LIS effectively to capture all essential data and maintain electronic records that are readily retrievable.
Maintaining this level of documentation helps with troubleshooting problems, ensuring accurate results are reported, and maintaining compliance with laboratory standards.
Q 22. How do you handle discrepancies or errors in laboratory results?
Discrepancies in lab results are a critical aspect of quality control. My approach involves a systematic investigation to identify the root cause. This starts with verifying the pre-analytical phase – ensuring proper patient identification, sample collection, and handling. I then meticulously review the analytical phase, checking for instrument malfunctions, reagent issues, or calculation errors. Finally, I examine the post-analytical phase, including data entry and reporting.
For instance, if a blood glucose result is significantly higher than expected, I’d first check the patient’s identification to eliminate the possibility of sample mix-up. Next, I’d verify the calibration and controls of the glucose analyzer, checking for any out-of-range results. If no issues are found there, I’d examine the sample itself for hemolysis or lipemia (which can interfere with results). Ultimately, I’d document all findings, and if necessary, repeat the test or initiate a corrective action report (CAR) to prevent recurrence.
Q 23. Explain your experience with quality assurance and quality control procedures.
Quality assurance (QA) and quality control (QC) are fundamental to accurate and reliable laboratory testing. My experience encompasses various aspects of both. QC involves the use of control materials—samples with known values—to monitor the accuracy and precision of analytical methods. Daily, weekly, and monthly QC runs are performed, and results are plotted on Levey-Jennings charts to identify trends or shifts in performance.
QA, on the other hand, encompasses broader processes, including staff training and competency assessments, equipment calibration and maintenance, and adherence to established procedures. I’m experienced in documenting QC data, interpreting QC charts, implementing corrective actions when needed, and participating in internal and external proficiency testing programs. I believe that maintaining high QA/QC standards is crucial for delivering trustworthy patient results.
Q 24. Describe a situation where you had to solve a problem in the laboratory. What was your approach?
During a busy period, our automated hematology analyzer malfunctioned, causing a significant backlog. My approach was methodical and focused on minimizing disruption. First, I contacted the biomedical engineering department to report the malfunction and request immediate attention. Meanwhile, I prioritized critical tests by manually performing differential counts on urgent samples using a microscope, ensuring the most time-sensitive results wouldn’t be delayed. Once the analyzer was repaired, I implemented a plan to process the backlog effectively, working overtime with my colleagues to catch up.
This experience highlighted the importance of teamwork and the need to have contingency plans in place. It also reinforced the value of clear communication in a high-pressure environment.
Q 25. How do you prioritize tasks and manage your workload in a busy laboratory setting?
Prioritization in a busy lab setting relies on effective time management and understanding the urgency of different tests. I utilize a combination of techniques, including prioritizing tests based on the physician’s requests (stat orders first), sample type (e.g., blood cultures are prioritized due to time sensitivity), and test turnaround time requirements. I use a workflow management system, a list, or similar tool to keep track of tasks, and I regularly reassess priorities as new requests come in.
For example, I might prioritize a stat blood culture over a routine complete blood count. I’m also adept at managing interruptions effectively, such as quickly handling phone inquiries while maintaining focus on hands-on tasks. Knowing when to delegate tasks, if possible, also helps manage workload and ensures timely completion.
Q 26. Are you familiar with CLIA regulations?
Yes, I am thoroughly familiar with the Clinical Laboratory Improvement Amendments (CLIA) regulations. CLIA establishes quality standards for all laboratory testing performed on humans in the U.S., regardless of the setting. My understanding encompasses the regulations surrounding personnel qualifications (including proficiency testing), quality control and quality assurance procedures, proficiency testing participation, and record-keeping requirements. I am aware of the different levels of complexity of testing and the associated requirements for each level. Compliance with CLIA is crucial for ensuring patient safety and the accuracy of lab results.
Q 27. Describe your experience with various laboratory instruments and their maintenance.
My experience includes operating and maintaining a wide range of laboratory instruments. This includes automated analyzers (hematology, chemistry, immunochemistry), microscopes (light and fluorescence), centrifuges, and various specialized equipment such as blood gas analyzers. I am proficient in performing routine maintenance tasks, such as cleaning, calibrating, and troubleshooting minor issues. I understand the importance of preventative maintenance to ensure optimal instrument performance and to minimize downtime.
For example, I’m skilled in performing daily quality control checks on our automated chemistry analyzer, which involves running control samples and interpreting the results to ensure the accuracy of patient tests. If a problem arises, such as a malfunctioning sensor, I follow the manufacturer’s instructions to resolve the issue, or if necessary, contact the vendor for technical support.
Q 28. What are your strengths and weaknesses as a Medical Lab Technician?
My strengths as a Medical Lab Technician include my meticulous attention to detail, my ability to work efficiently and accurately under pressure, and my strong problem-solving skills. I am a quick learner and adapt easily to new technologies and procedures. I also value teamwork and believe in maintaining clear and effective communication with colleagues and other healthcare professionals.
One area for improvement I’m actively working on is enhancing my leadership skills. While I’m proficient in my role, I recognize the value of further developing my ability to mentor and guide junior staff members. I’m pursuing opportunities to take on additional responsibilities and gain experience in leadership roles within the laboratory.
Key Topics to Learn for Medical Lab Technician Interview
- Clinical Laboratory Techniques: Understanding and demonstrating proficiency in various laboratory techniques like hematology, urinalysis, microbiology, and blood banking. Consider the practical application of these techniques in a clinical setting and be prepared to discuss your experience and skill levels.
- Laboratory Instrumentation and Equipment: Familiarize yourself with the operation, maintenance, and troubleshooting of common laboratory instruments such as automated analyzers, microscopes, and centrifuges. Be ready to discuss your experience with specific equipment and any problem-solving experiences you’ve had.
- Quality Control and Assurance: Mastering the principles of quality control and assurance in a medical laboratory is crucial. Understand the importance of maintaining accuracy and precision in test results and be prepared to discuss your approach to quality control procedures and troubleshooting discrepancies.
- Safety Regulations and Procedures: Demonstrate a thorough understanding of safety protocols and regulations within a medical laboratory environment. This includes infection control, handling of hazardous materials, and proper waste disposal. Be prepared to discuss specific safety procedures you’ve followed.
- Laboratory Information Systems (LIS): Familiarity with LIS software and its applications in managing patient data, test results, and quality control. Be ready to discuss your experience using LIS systems and how you’ve utilized them to improve efficiency.
- Medical Terminology and Anatomy & Physiology: A strong understanding of medical terminology, anatomy, and physiology is essential for effective communication and interpretation of test results. Be prepared to discuss relevant concepts and their application in laboratory testing.
- Critical Thinking and Problem Solving: Highlight your ability to analyze data, identify discrepancies, and troubleshoot issues independently. Prepare examples demonstrating your analytical and problem-solving skills within a laboratory setting.
Next Steps
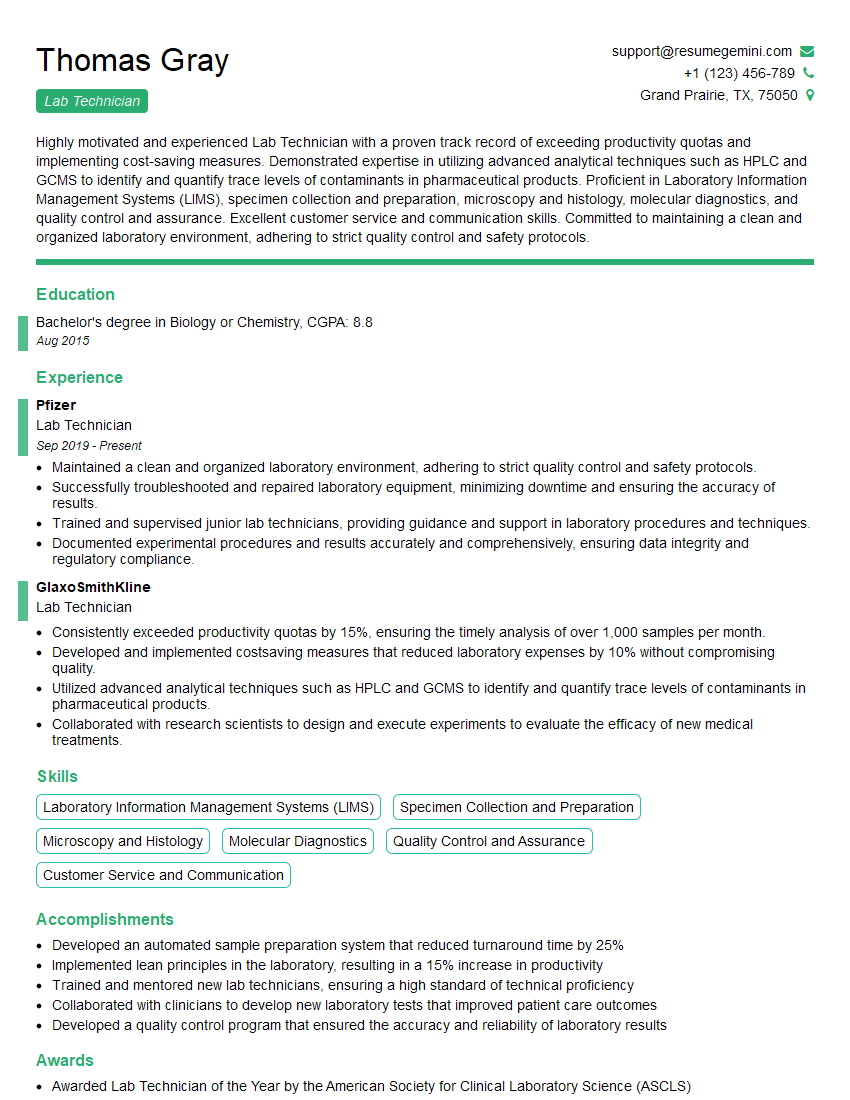
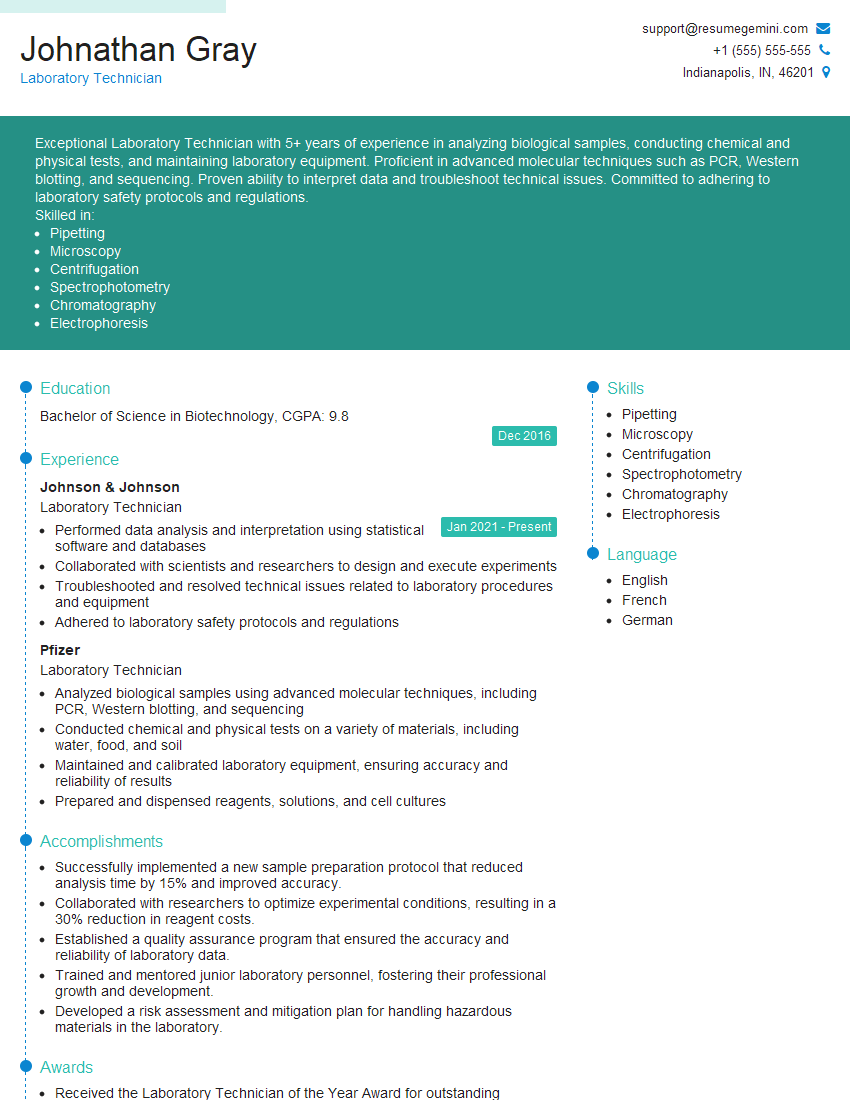
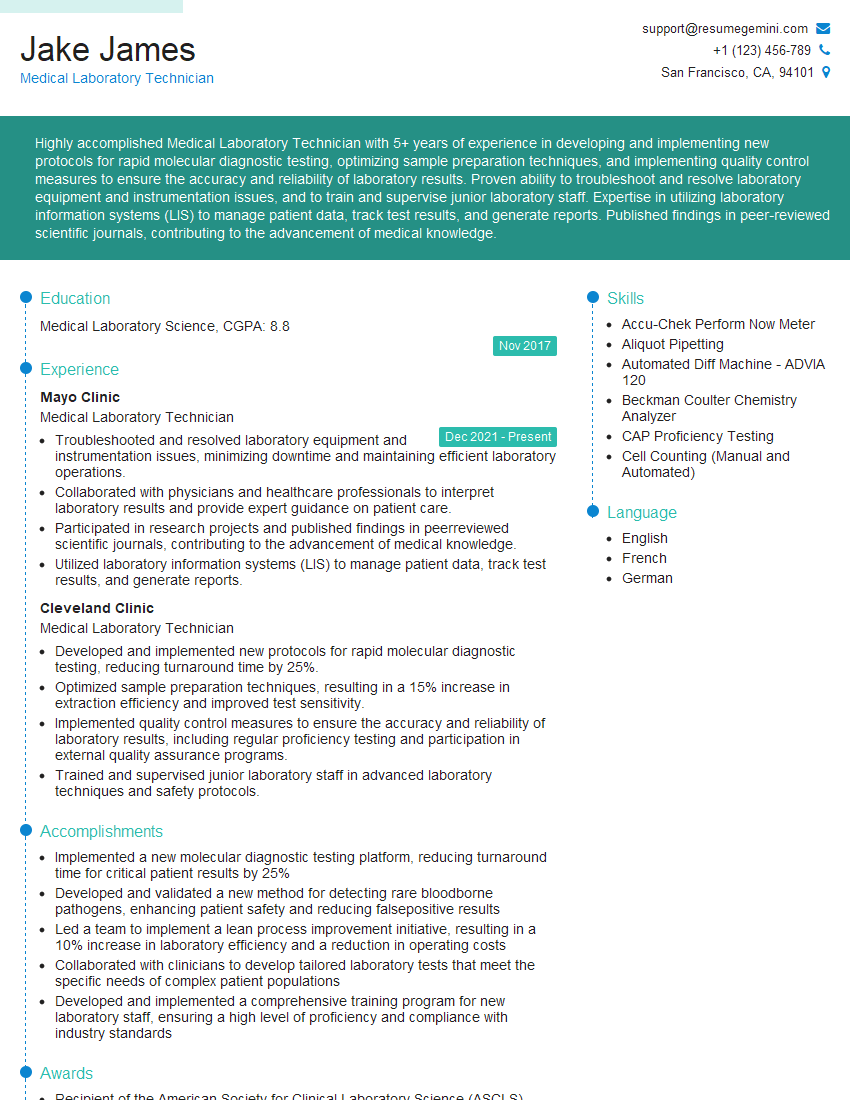
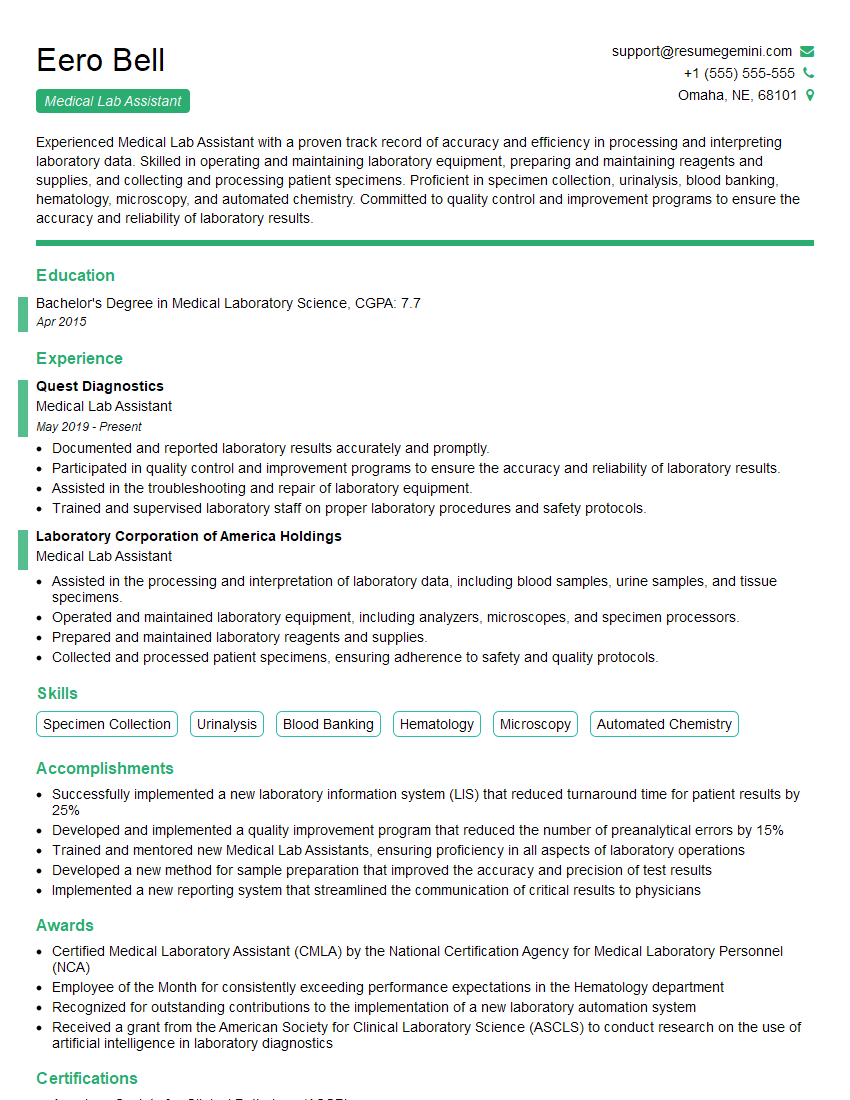
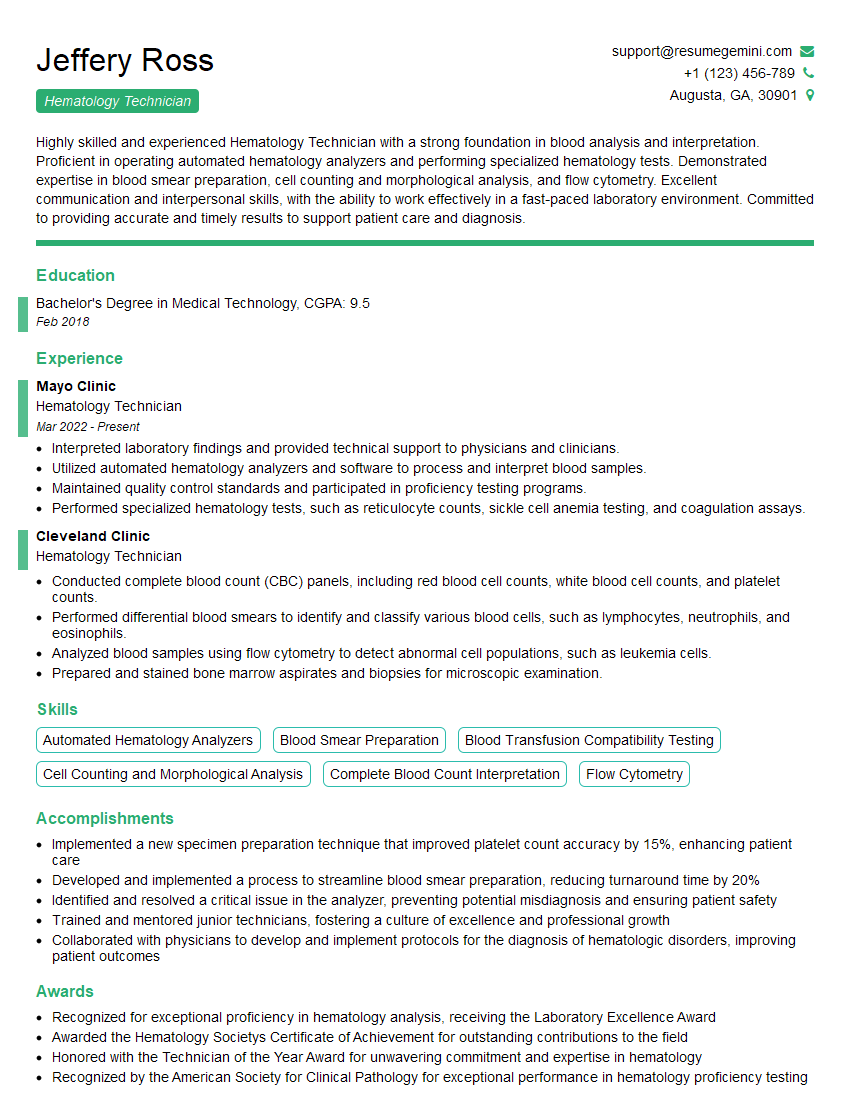
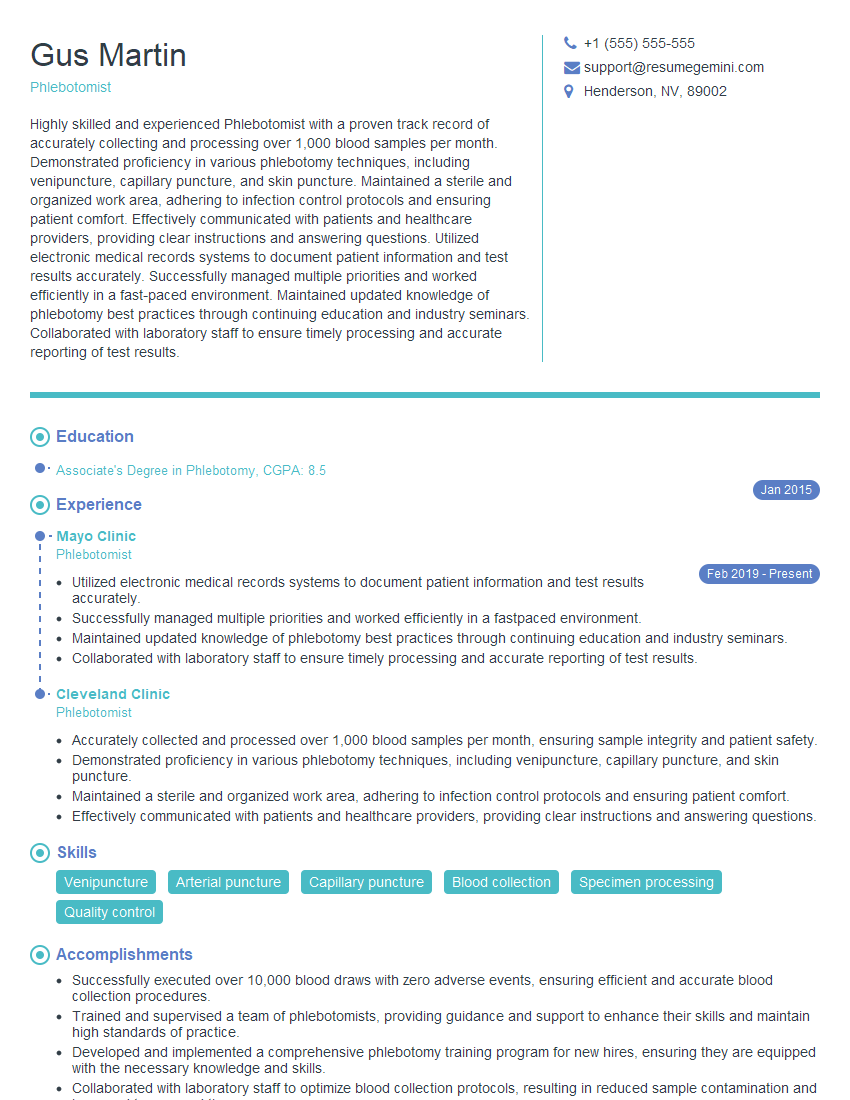
A successful career as a Medical Lab Technician offers a rewarding blend of scientific knowledge and direct patient impact. To maximize your job prospects, creating a strong, ATS-friendly resume is paramount. This ensures your qualifications are effectively highlighted to potential employers. ResumeGemini is a trusted resource that can help you build a professional and impactful resume, tailored to showcase your skills and experience. Examples of resumes tailored to Medical Lab Technicians are available to guide you in building your own. Take the next step and craft a resume that reflects your potential!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO