Cracking a skill-specific interview, like one for Patient Registration and Intake, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Patient Registration and Intake Interview
Q 1. Explain the process of patient registration from initial contact to appointment scheduling.
Patient registration begins the moment a patient contacts our facility, whether by phone, online portal, or in person. The process is designed to be efficient and welcoming. Initially, we gather basic identifying information such as name, date of birth, and contact details. This information helps us locate the patient in our system if they are already registered. For new patients, we collect a comprehensive set of demographic data, including address, employment information, emergency contact details, and insurance information. This is often done using an electronic intake form that helps to reduce errors and ensure completeness. Once the demographic information is verified and updated, we proceed to schedule the appointment, considering the patient’s preferences, physician availability, and the nature of the visit. We confirm the appointment details, including date, time, location, and any pre-appointment instructions. Finally, the patient receives a confirmation, often via email or text message, with all the necessary information for their visit.
For example, if a patient calls to schedule a routine check-up, we collect their name and date of birth, verify their insurance details, and then find a suitable time slot with their preferred doctor. If they are a new patient, we’ll ask for more comprehensive information such as their address, employment details, and the reason for their first visit, all while maintaining a friendly and professional demeanor. The entire process is designed for both speed and accuracy.
Q 2. How do you verify patient insurance eligibility and benefits?
Verifying patient insurance eligibility and benefits is crucial for accurate billing and to avoid delays in care. We utilize electronic claims processing systems that connect directly with insurance carriers’ databases. This allows us to verify the patient’s insurance coverage in real-time. We verify the following key details: the patient’s identification number, the effective date of their coverage, whether the patient is currently covered, and the specifics of their plan (deductible, copay, co-insurance). We also check for pre-authorization requirements, which are often needed for specific procedures or specialists. If the patient’s insurance is not recognized in the system, or if there are issues with the identification, we have a process for contacting the insurance provider directly to resolve discrepancies. We clearly communicate the patient’s financial responsibility (deductibles, co-pays) up front to promote transparency and prevent surprises.
For instance, if a patient presents with an insurance card, we enter the details into our system. The system automatically checks for coverage and returns details on co-pays, deductibles, and whether a referral is needed. We then inform the patient of their expected out-of-pocket expenses for the upcoming visit.
Q 3. Describe your experience with various insurance plans and payer requirements.
Throughout my career, I’ve gained extensive experience with a wide array of insurance plans, including HMOs, PPOs, POS plans, Medicare, Medicaid, and various commercial insurance carriers. I understand the nuances of each plan type, including their coverage limitations, referral requirements, and reimbursement methodologies. Each insurer has its unique claim submission requirements and eligibility verification processes, such as specific claim forms, codes, and documentation needed. My experience allows me to accurately interpret the plan details and ensure that the required information is obtained and submitted correctly to avoid claim denials. I also have experience with different state-specific Medicaid and Medicare regulations, adapting my approach based on the patient’s location and plan type. The ability to effectively navigate these diverse systems and requirements is critical in ensuring timely reimbursements and efficient claim processing.
For example, I’m familiar with the prior authorization process that many plans require before specialized procedures can be performed. I understand how different plans handle pre-existing conditions and manage the required documentation accurately.
Q 4. How do you handle a patient who is uninsured or underinsured?
When a patient is uninsured or underinsured, we offer several options to ensure they receive the necessary medical care. First, we discuss various financial assistance programs, including government subsidies like Medicaid or state-sponsored programs. We also explore options for payment plans or charity care, depending on the healthcare facility’s policies and the patient’s financial situation. We work with the patient to understand their financial limitations and explore all available resources to make healthcare accessible. Open communication is critical here, ensuring the patient understands their options and feels supported throughout the process. It’s important to be empathetic and guide them towards resources that can assist them with their healthcare expenses.
For example, we might connect an uninsured patient with local non-profit organizations offering financial assistance for healthcare costs or provide them with information about sliding-scale payment options provided by the hospital.
Q 5. What is your experience with electronic health record (EHR) systems for patient registration?
I have extensive experience using various EHR (Electronic Health Record) systems for patient registration. My expertise ranges from using the system to create new patient records, update existing ones, efficiently managing patient demographics and insurance details to scheduling appointments and generating reports. I’m proficient in using EHR systems to ensure data accuracy and integrity and adhere to HIPAA regulations for patient confidentiality. The key to successful EHR utilization is efficient data entry, ensuring all fields are accurately populated and identifying any inconsistencies. This requires strong attention to detail and proficiency in the specific software used. Furthermore, familiarity with the system’s reporting capabilities helps monitor key performance indicators, such as registration time, patient throughput, and error rates.
For example, I’m proficient in Epic and Cerner EHR systems, capable of using their registration modules to streamline the entire patient intake process, minimizing the time it takes to register a patient and improving accuracy.
Q 6. How do you maintain patient confidentiality and comply with HIPAA regulations?
Maintaining patient confidentiality and complying with HIPAA regulations is paramount. We strictly adhere to HIPAA guidelines, ensuring that Protected Health Information (PHI) is only accessed by authorized personnel on a need-to-know basis. Our EHR systems employ robust security measures, including access controls, encryption, and audit trails, to protect patient data. We provide regular HIPAA training to all staff involved in patient registration and handle patient information with the utmost care. We also follow strict protocols for data disposal and secure destruction of paper records. We have processes in place to handle requests for access to medical records, ensuring that all such requests are verified and handled according to HIPAA regulations. Furthermore, we educate patients about their HIPAA rights, empowering them to take control of their health information.
For example, we use secure messaging systems for communication with patients, ensuring that all electronic communications are encrypted and protected, and we don’t leave patient records unattended on computer screens.
Q 7. How do you manage patient demographics and contact information accurately?
Accurate management of patient demographics and contact information is crucial for efficient patient care and billing. We utilize the EHR system to ensure that all information is entered correctly and consistently. Data entry staff are trained to follow standardized protocols to minimize errors, and we employ data validation techniques to verify the accuracy of information entered into the system. We establish procedures to update patient information promptly, as changes such as address or insurance details occur. We use automated systems to verify patient addresses and insurance information against national databases. This helps to identify and correct inaccuracies that may otherwise lead to delays or complications. Moreover, we use data integrity checks within our EHR system to ensure that no inconsistencies exist within the demographic data. This focus on data accuracy helps streamline the overall patient experience and prevents administrative delays.
For instance, if a patient moves or changes insurance providers, the updated information is immediately documented in our system to ensure all communication and billing accurately reflect this change.
Q 8. How do you address patient inquiries and concerns effectively?
Addressing patient inquiries and concerns effectively hinges on active listening, empathy, and clear communication. I approach each interaction with the goal of understanding the patient’s perspective completely before offering solutions. This involves not just hearing their words, but also observing their body language and tone to pick up on any unspoken anxieties.
For example, if a patient is worried about the cost of a procedure, I would first validate their concerns by saying something like, “I understand that cost can be a significant concern. Let’s explore your insurance coverage and payment options together.” Then, I’d systematically explain their billing options, available financial assistance programs, or payment plans. I always ensure to provide accurate information and follow up to confirm they’re satisfied with the resolution.
In cases where I don’t have the answer, I’ll readily admit it and escalate the question to the appropriate department or individual, keeping the patient updated throughout the process. Transparency and follow-up are key to building trust and ensuring positive patient experiences.
Q 9. Describe your experience with appointment scheduling and managing patient flow.
My experience with appointment scheduling and managing patient flow is extensive. I’m proficient in using various scheduling software, such as Epic and Cerner, to optimize appointment slots, minimizing patient wait times and maximizing provider efficiency. I understand the importance of considering factors like appointment duration, provider availability, and patient preferences (e.g., morning vs. afternoon appointments).
Managing patient flow often involves coordinating with multiple teams: nurses, medical assistants, and providers. In a busy environment, I use clear communication and a well-organized workflow to ensure a smooth patient experience. For example, I might proactively contact patients to confirm appointments and send reminders, and I’m adept at handling last-minute cancellations and rescheduling requests with minimal disruption.
I have implemented strategies to improve patient flow, such as using pre-registration processes (discussed further in question 4) and optimizing registration forms to gather necessary information efficiently. Real-time tracking of patient arrival and progress through the system helps identify potential bottlenecks and allows for timely interventions.
Q 10. How do you handle a high-volume patient registration workload?
Handling a high-volume patient registration workload necessitates efficiency and organization. My approach involves prioritizing tasks, utilizing efficient workflows, and leveraging technology to its fullest extent. This includes mastering the use of electronic health records (EHRs) and patient registration systems, ensuring accuracy and speed.
- Prioritization: I prioritize patients based on urgency (e.g., emergency patients, those with pre-scheduled appointments).
- Workflow optimization: Streamlining the registration process by eliminating redundant steps, using templates, and implementing quick data entry techniques.
- Technology utilization: Proficient use of EHR systems to automate data entry, validate insurance information, and generate necessary forms.
- Teamwork: Collaborating with colleagues to distribute workload efficiently and share knowledge.
During periods of exceptionally high volume, I’ll communicate proactively with patients, informing them of potential delays and setting realistic expectations. This ensures transparency and prevents unnecessary frustration.
Q 11. Explain your experience with pre-registration processes and procedures.
Pre-registration processes are crucial for streamlining the patient experience and improving operational efficiency. My experience includes collecting patient demographic information, insurance details, and medical history prior to their arrival. This can be done via phone, mail, or secure online portals. This approach significantly reduces wait times on the day of the appointment.
For example, I’ve worked in settings where patients complete pre-registration forms online, uploading necessary documents securely. This ensures all information is readily available when they arrive, allowing for a quicker check-in process. I also have experience verifying insurance benefits preemptively, identifying potential issues and proactively addressing them before the patient’s appointment. This avoids delays and ensures a smooth billing process.
The effectiveness of pre-registration also hinges on clear communication and providing patients with easily accessible instructions. This minimizes errors and ensures a positive experience.
Q 12. How do you identify and resolve registration errors or discrepancies?
Identifying and resolving registration errors or discrepancies requires attention to detail and a systematic approach. I begin by carefully reviewing the patient’s information against various sources, such as their identification documents, insurance cards, and previous records (if available). I use data validation tools within the EHR to flag potential inconsistencies.
For example, a mismatch between the name on the insurance card and the patient’s identification might indicate an error requiring immediate correction. I would then contact the patient or insurance provider to clarify the discrepancy and ensure accuracy. In cases of more complex discrepancies, I collaborate with the billing department to determine the best course of action.
Maintaining accurate patient records is paramount. Errors can lead to billing problems, delays in treatment, and compromised patient care. A proactive approach that emphasizes thorough data verification is essential to avoiding such issues.
Q 13. Describe your experience with collecting patient payments or co-pays.
Collecting patient payments or co-pays involves professionalism, accuracy, and a clear understanding of billing policies and procedures. I’m proficient in using various payment processing systems, including credit card terminals and online payment portals. I always ensure to clearly communicate the payment amount, the accepted payment methods, and any available payment plans.
I prioritize patient privacy and security when handling financial information, adhering to HIPAA regulations at all times. For example, I would never discuss a patient’s financial information in a public area. I handle sensitive data with discretion and follow established security protocols for electronic transactions.
I provide patients with a detailed receipt upon successful payment and always answer any questions they may have regarding their billing statement. In situations involving financial hardship, I’m trained to discuss available financial assistance options or payment arrangements.
Q 14. How do you handle patient complaints or difficult situations professionally?
Handling patient complaints or difficult situations professionally requires patience, empathy, and strong communication skills. My approach begins with active listening to fully understand the patient’s concerns. I strive to validate their feelings, even if I don’t agree with their perspective. Empathetic responses like, “I understand your frustration,” or “I’m sorry you’re having this experience,” can significantly de-escalate a tense situation.
I then work to find a mutually acceptable solution, offering possible options and explaining the rationale behind any decisions made. For example, if a patient complains about a long wait time, I might apologize for the inconvenience, offer a discount on their next visit, or explain the reason for the delay. Documentation of the complaint and the steps taken to resolve it is critical.
In situations I can’t resolve immediately, I’ll escalate the issue to the appropriate supervisor or manager, keeping the patient informed of the progress. My ultimate goal is to resolve the issue fairly and leave the patient feeling heard and respected, even if the outcome isn’t precisely what they had hoped for.
Q 15. What is your experience with medical terminology and coding?
My experience with medical terminology and coding is extensive. I’ve worked with a wide range of medical terms, from common diagnoses like hypertension and diabetes to more specialized terminology related to cardiology, oncology, and orthopedics. I’m proficient in interpreting and utilizing ICD-10 and CPT codes, ensuring accurate billing and data analysis. For example, understanding the nuances of different ICD-10 codes for pneumonia allows for precise tracking of disease prevalence and treatment effectiveness. My knowledge extends to understanding the relationship between diagnostic codes (ICD-10) and procedural codes (CPT), which is crucial for accurate patient record maintenance and reimbursement processes.
Furthermore, I have a solid understanding of medical abbreviations and their implications, ensuring that I can accurately interpret and input information into patient records without introducing errors. This is vital for patient safety and the integrity of the healthcare data.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you prioritize tasks and manage your time effectively in a fast-paced environment?
Prioritizing tasks and managing time in a fast-paced environment is essential in patient registration. I use a combination of techniques, including prioritizing urgent tasks based on deadlines and patient needs, and employing time management tools like task lists and calendars. For example, patients requiring immediate attention for emergencies are prioritized over routine check-ins.
I leverage tools such as scheduling software to optimize appointments and reduce wait times. I also utilize time blocking to dedicate specific time slots for different tasks, such as phone calls, data entry, and assisting patients. I constantly reassess my workload and adjust my plan to accommodate unforeseen circumstances, which is a crucial skill in the fast-paced environment of a medical facility. Think of it like conducting an orchestra; each instrument (task) needs to play at the right time and with the right tempo to create a harmonious whole (efficient workflow).
Q 17. How do you work effectively as part of a team?
Effective teamwork is paramount in healthcare. I thrive in collaborative settings and actively contribute to a positive team dynamic. I communicate clearly and respectfully, sharing information and offering assistance to colleagues. I believe in fostering open communication and mutual respect to achieve common goals.
For example, during a period of high patient volume, I proactively assisted my colleagues with tasks outside my immediate responsibility, such as checking in patients or verifying insurance information. This collaborative effort ensured smooth patient flow and reduced wait times. I also actively participate in team meetings, offering suggestions and contributing to problem-solving sessions, promoting a shared understanding of goals and responsibilities.
Q 18. Describe a time you had to resolve a conflict with a patient or colleague.
I once had a conflict with a patient who was frustrated by a long wait time. Instead of becoming defensive, I actively listened to their concerns, empathized with their frustration, and apologized for the inconvenience. I explained the reason for the delay and offered a solution, such as providing them with a more comfortable waiting area or offering an estimated wait time.
Through calm and respectful communication, I was able to de-escalate the situation and resolve the conflict amicably. The patient appreciated my empathy and understanding, ultimately leaving with a positive impression despite the initial frustration. This experience reinforced my belief in the power of active listening and empathy in resolving conflicts.
Q 19. How familiar are you with different types of healthcare facilities (hospitals, clinics, etc.)?
I am familiar with a variety of healthcare settings, including hospitals (both large and small), clinics (speciality and general practice), urgent care centers, and physician’s offices. My experience encompasses understanding the unique registration processes and workflows for each type of facility. For instance, hospital registration often involves more complex processes, such as pre-admission testing and coordinating with various departments. In contrast, clinic registration might focus on a quicker check-in process for routine appointments.
This broad understanding allows me to adapt readily to different environments and requirements, providing efficient and accurate patient registration services irrespective of the specific healthcare setting.
Q 20. What is your experience with various registration systems?
I have extensive experience with various registration systems, including both electronic health record (EHR) systems like Epic and Cerner, and standalone patient registration software. My experience includes data entry, system maintenance and troubleshooting minor issues. I’m proficient in utilizing these systems to capture accurate patient demographics, insurance information, and medical history. I’m also familiar with the process of integrating different systems, which often involves understanding data fields and mapping to ensure seamless data flow between platforms.
For instance, I’ve worked with systems that require specific data formatting for insurance verification, and I’m adept at adhering to those requirements. Understanding these diverse systems helps me maintain accurate and consistent patient information across the entire healthcare system.
Q 21. How do you ensure the accuracy and completeness of patient registration data?
Ensuring accuracy and completeness of patient registration data is crucial for patient safety and the efficient operation of a healthcare facility. I utilize a multi-pronged approach to achieve this. First, I employ meticulous attention to detail during data entry, verifying all information against identification documents and insurance cards.
Second, I use various validation tools and processes to ensure that information entered matches established parameters. For example, I use built-in system checks to identify incorrect zip codes or invalid insurance information. Third, I follow established protocols for handling incomplete data, seeking clarification from patients or their representatives where necessary. Finally, regular data audits are conducted to identify and correct errors to improve data quality. These comprehensive measures ensure that patient information is accurate, complete, and reliable, fostering a safe and efficient healthcare environment.
Q 22. How do you maintain patient privacy and security within the registration process?
Maintaining patient privacy and security during registration is paramount. It’s not just about compliance; it’s about building trust. We achieve this through a multi-layered approach.
- Strict adherence to HIPAA regulations: This includes implementing robust security measures like access controls, encryption of electronic health records (EHRs), and regular security audits. We ensure only authorized personnel have access to patient data, based on the principle of least privilege.
- Secure data storage: All patient data, whether paper or electronic, is stored securely, following best practices for physical and digital security. This includes secure servers, firewalls, and intrusion detection systems.
- Data minimization: We collect only the absolutely necessary information from patients, avoiding unnecessary data collection to minimize potential risks.
- Employee training: Regular training for all staff on HIPAA compliance, data security best practices, and privacy protocols is crucial. This includes awareness of phishing attempts, social engineering, and other potential security threats.
- Privacy notices and consent forms: Patients are provided with clear and concise privacy notices explaining how their information will be used and protected. Informed consent is obtained before collecting or using any data.
For example, I once discovered a minor flaw in our access control system that could potentially allow unauthorized access to patient data. I immediately reported this to the IT department, and we implemented a fix before any breach occurred. This proactive approach underlines our commitment to patient privacy.
Q 23. Explain your understanding of the revenue cycle and its relation to patient registration.
The revenue cycle encompasses all administrative and clinical functions related to billing and collecting payments for healthcare services. Patient registration is the crucial first step in this cycle, directly impacting its efficiency and success.
Accurate and complete patient registration is essential for accurate billing. Think of it like the foundation of a house. If the foundation is weak (incomplete or inaccurate registration), the entire structure (revenue cycle) is at risk. Incorrect insurance information, missing demographic data, or errors in patient identifiers can lead to claim denials, delayed payments, and ultimately, revenue loss.
Specifically, accurate registration ensures:
- Correct insurance verification: This allows for timely processing of claims and minimizes denials due to incorrect insurance information.
- Appropriate billing codes: Accurate patient information is needed to select the correct procedural and diagnostic codes for billing purposes.
- Effective payment processing: Having accurate payment information streamlines the payment process and reduces accounts receivable days.
- Improved patient experience: A smooth registration process contributes to patient satisfaction, which positively affects the overall revenue cycle.
For instance, imagine a patient with an outdated insurance card. If this isn’t caught during registration, it could delay payment for several weeks, impacting the organization’s cash flow.
Q 24. Describe your experience with utilizing patient portals or online registration tools.
I have extensive experience implementing and utilizing both patient portals and online registration tools. These technologies significantly streamline the registration process and improve patient experience.
Patient portals allow patients to access their medical records, schedule appointments, request prescription refills, and communicate with their providers securely. Online registration tools allow patients to complete the registration process from the comfort of their homes, reducing wait times at the facility. This can include pre-populating forms with data from existing records, making the process incredibly efficient.
In a previous role, I helped implement a new patient portal that integrated with our EHR system. This reduced registration time by approximately 50% and improved patient satisfaction scores considerably. The system also allowed for automated appointment reminders, reducing no-shows and improving appointment scheduling efficiency. We specifically designed the portal to be user-friendly, with intuitive navigation and helpful prompts. Regular feedback from patients helped us make iterative improvements and ensure a positive user experience.
Q 25. How do you stay updated on changes in healthcare regulations and best practices related to patient registration?
Staying current on healthcare regulations and best practices is crucial in this field. It’s an ongoing commitment, not a one-time event.
- Professional organizations: I actively participate in professional organizations like the American Health Information Management Association (AHIMA) to stay informed about regulatory changes and industry best practices. These organizations offer webinars, conferences, and publications that keep me up-to-date.
- Regulatory websites: I regularly consult websites like the Centers for Medicare & Medicaid Services (CMS) and the Office for Civil Rights (OCR) for updates on HIPAA regulations and other relevant guidelines.
- Industry publications and journals: I subscribe to industry publications and journals to read about new technologies, best practices, and emerging trends in patient registration.
- Continuing education: I regularly participate in continuing education courses to maintain my knowledge and skills in this area. Many of these courses focus on regulatory changes, compliance issues, and new technologies.
For example, when the recent changes to HIPAA regulations were announced, I immediately reviewed the updates and implemented necessary changes to our registration processes to ensure full compliance. This included updating our privacy notices and staff training materials.
Q 26. How would you handle a situation where a patient refuses to provide necessary information?
Handling a situation where a patient refuses to provide necessary information requires a delicate balance of understanding and adherence to policy. The approach must always be patient-centered and respectful, but also firm in the need for essential information.
My first step would be to understand why the patient is hesitant. Open, empathetic communication is key. Is there a language barrier? Are there concerns about privacy or data security? Are there cultural sensitivities at play?
Once the reason is understood, I would try to address their concerns. I might offer alternative methods of providing information, or explain how the information will be used and protected. In some cases, I may need to involve a supervisor, interpreter, or social worker, depending on the situation.
However, if the information is absolutely essential for providing care (like insurance details for billing or contact information for follow-up) and the patient remains unwilling to provide it, I would document the situation thoroughly in the patient’s record, clearly stating the patient’s refusal and any steps taken to address their concerns. The next steps would then depend on the organization’s specific policies and procedures – in some cases, care may be delayed until the necessary information is provided.
For instance, I once encountered a patient who was hesitant to provide their social security number due to concerns about identity theft. I addressed these concerns by explaining our robust security measures and emphasized the importance of the information for insurance purposes. Ultimately, with reassurance and a clear explanation, they felt comfortable providing it.
Q 27. Describe your experience with managing patient data in compliance with data privacy laws.
Managing patient data in compliance with data privacy laws, such as HIPAA, is a critical responsibility. This involves more than just following regulations; it’s about cultivating a culture of privacy protection.
- Data encryption: All electronic patient data is encrypted both in transit and at rest to protect against unauthorized access.
- Access controls: Strict access controls are implemented to limit access to patient data based on the principle of least privilege. Only authorized personnel have access to the information they need to perform their jobs.
- Regular security audits: Regular security audits and vulnerability assessments are conducted to identify and address potential security weaknesses.
- Data breach response plan: A comprehensive data breach response plan is in place to outline procedures for handling potential data breaches, including notification procedures and remediation steps.
- Staff training: Ongoing staff training on data privacy laws and security best practices is crucial to ensure that everyone understands their responsibilities.
- Data disposal: Secure disposal methods are used for both electronic and paper patient records to protect against unauthorized access to discarded data.
In a previous experience, we implemented multi-factor authentication for all staff accessing the EHR system, significantly improving security. We also held regular training sessions to refresh employees’ knowledge of HIPAA guidelines and best practices. I’ve personally participated in security audits and data breach response drills, ensuring that our processes are up-to-date and effective.
Q 28. How do you ensure a positive and welcoming experience for patients during the registration process?
Creating a positive and welcoming registration experience is crucial for patient satisfaction and overall healthcare outcomes. It sets the tone for their entire visit.
- Warm and friendly greeting: Patients should be greeted warmly and with a smile, making them feel comfortable and valued from the start.
- Clear and concise instructions: Instructions should be clear, simple, and easy to understand. Avoid using medical jargon.
- Efficient process: Minimize wait times by streamlining the registration process. Consider using technology like online pre-registration or kiosks to speed up the process.
- Personalized attention: Treat each patient as an individual, addressing their specific needs and concerns with patience and understanding.
- Comfortable waiting area: Ensure the waiting area is comfortable and welcoming, with comfortable seating, magazines, and a pleasant atmosphere.
- Follow-up: If there are any delays or unexpected issues, provide updates and keep the patient informed. A sincere apology if things don’t go as planned goes a long way.
For instance, I once implemented a system where patients received text message updates about their wait time, which reduced anxiety and improved their experience significantly. We also created short, simple videos explaining the registration process that patients could watch while waiting, helping them feel more prepared and less overwhelmed.
Key Topics to Learn for Patient Registration and Intake Interview
- Patient Demographics and Insurance Verification: Understanding the importance of accurate data entry, verifying insurance coverage and eligibility, and navigating different insurance plans.
- Medical Records Management: Practical application of maintaining patient confidentiality, proper filing systems, both electronic and physical, and handling medical records requests.
- Scheduling and Appointment Management: Efficiently scheduling appointments, managing patient flow, handling cancellations and rescheduling, and utilizing appointment scheduling software.
- HIPAA Compliance and Patient Confidentiality: Theoretical understanding of HIPAA regulations and their practical application in protecting patient privacy and maintaining confidentiality.
- Patient Communication and Customer Service: Effective communication techniques for handling patient inquiries, addressing concerns, and providing a positive patient experience. Problem-solving approaches for managing difficult situations.
- Medical Terminology and Abbreviations: Understanding common medical terms and abbreviations to ensure accurate data entry and communication within the healthcare setting.
- EMR/EHR Systems: Familiarity with various Electronic Medical Record/Electronic Health Record systems, data entry procedures, and troubleshooting common technical issues.
- Billing and Coding (if applicable): Basic understanding of medical billing and coding practices, particularly as they relate to patient registration and insurance verification.
- Understanding Patient Flow and Processes: Analyzing the patient journey from initial contact to check-in, and identifying potential areas for improvement in efficiency and patient satisfaction.
Next Steps
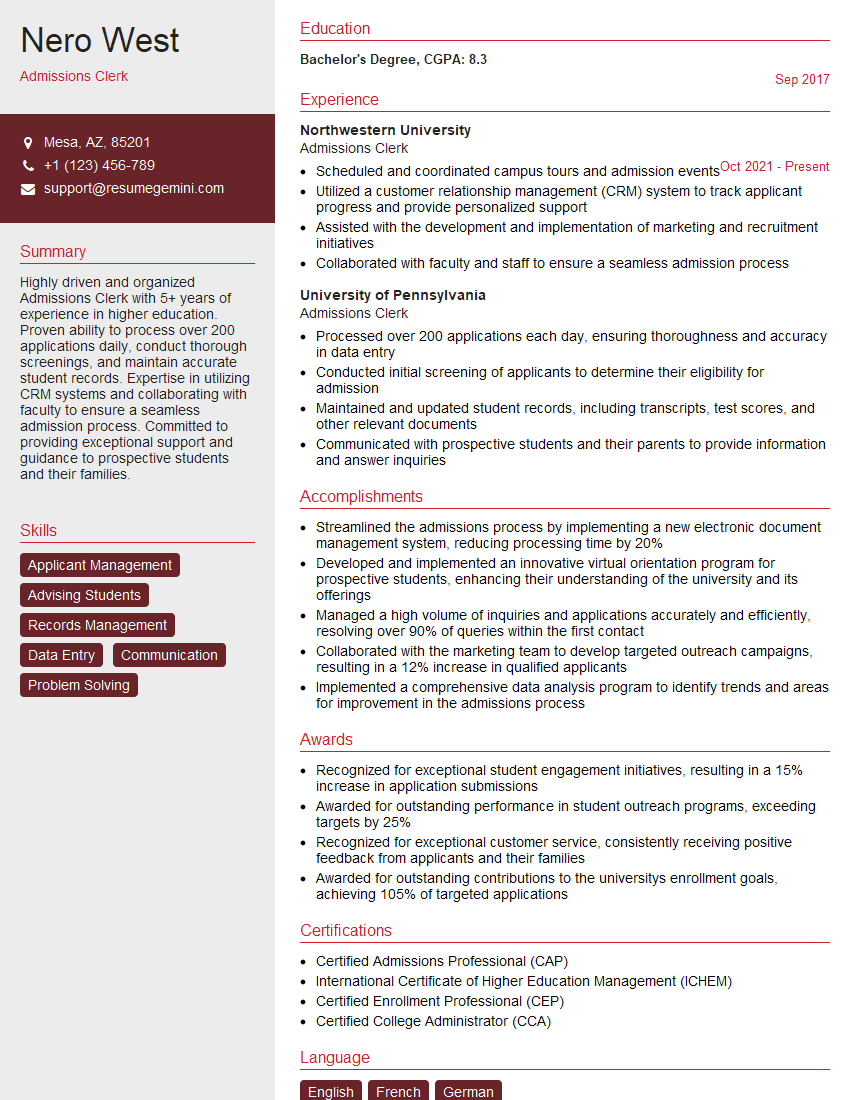
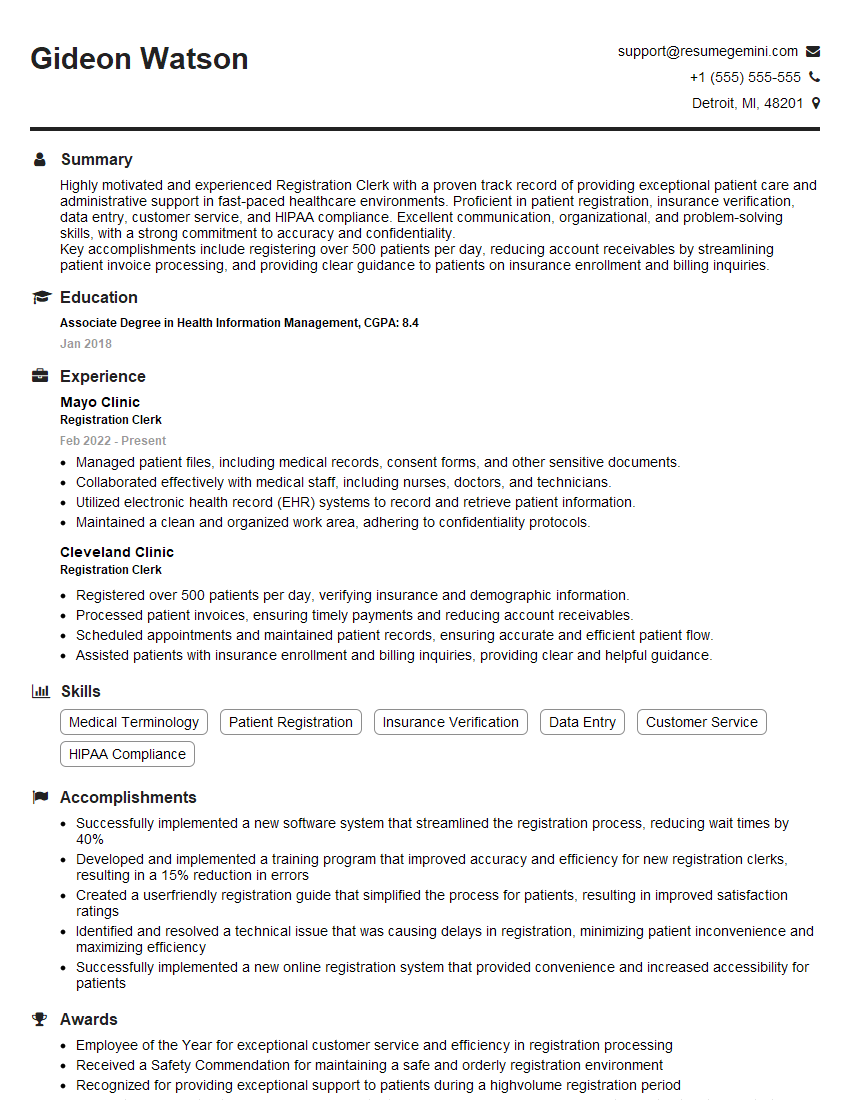
Mastering Patient Registration and Intake is crucial for career advancement in the healthcare field. It demonstrates your ability to be organized, detail-oriented, and a key contributor to a smooth and efficient patient experience. Building a strong, ATS-friendly resume is vital for showcasing your skills and experience to potential employers. We strongly encourage you to use ResumeGemini to craft a compelling resume that highlights your qualifications. ResumeGemini provides an enhanced resume-building experience and offers examples of resumes tailored to Patient Registration and Intake roles to help you get started.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
There are no reviews yet. Be the first one to write one.