Preparation is the key to success in any interview. In this post, we’ll explore crucial Physical Restraint Training interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Physical Restraint Training Interview
Q 1. Describe the different types of physical restraints.
Physical restraints are methods used to restrict a person’s movement. They range from simple to complex, depending on the individual’s behavior and the level of risk. The goal is always to ensure the safety of the individual and others, while minimizing the use of restraint.
- Soft restraints: These include wrist restraints made of soft material like cloth or padded leather, and sometimes ankle restraints. They are less restrictive than mechanical restraints and are often used for individuals at low risk of harming themselves or others.
- Mechanical restraints: These involve devices like belts, straps, or vests that limit movement more significantly. They are generally used when soft restraints are insufficient and are often secured to a bed frame or chair to prevent the individual from getting up.
- Chemical restraints: These use medications to sedate an individual, temporarily reducing their ability to act aggressively or impulsively. This is a last resort, and requires strict medical oversight and a doctor’s order. It’s crucial to note that this isn’t truly a ‘physical’ restraint but is categorized under restraint due to its similar purpose.
The choice of restraint depends on the specific situation and must always be the least restrictive option necessary.
Q 2. What are the legal and ethical considerations surrounding the use of physical restraints?
The use of physical restraints is governed by strict legal and ethical guidelines. Legally, restraints must only be used as a last resort, when all other de-escalation techniques have failed and there’s an immediate risk of harm to the individual or others. Improper use can lead to legal action, including negligence claims. Ethically, using restraints should always be considered carefully, weighing the potential benefits against the significant risks to the individual’s dignity, autonomy, and physical well-being. Consent, when possible, is crucial. The use of restraints should be documented meticulously, including the reason, the type of restraint used, and the duration.
For example, in a healthcare setting, the use of restraints requires a doctor’s order, regular monitoring by staff, and frequent reassessment of the need for continued restraint. Failure to follow these procedures can lead to serious repercussions.
Q 3. Explain the proper procedures for applying and removing restraints.
Applying and removing restraints requires precise procedures to minimize injury and maintain dignity. It’s typically a team effort, ensuring at least two trained staff members are involved.
- Application: Before applying any restraints, attempts should be made to de-escalate the situation using verbal de-escalation techniques. If restraints are necessary, they should be applied quickly, calmly, and firmly, but gently. Proper application techniques must be followed, ensuring the restraints are not too tight, and circulation and comfort are checked regularly. Always use the appropriate type and size of restraint for the individual.
- Removal: Once the need for restraint has subsided and the individual is calm and cooperative, the restraints should be removed immediately and carefully. The process should be documented, including the time of application and removal.
Regular checks, including skin integrity, circulation, and comfort, are vital during restraint, ensuring proper placement and preventing complications. These checks are documented and must be in accordance with facility policies. For instance, a wrist restraint might be checked every 15 minutes for proper fit and skin integrity.
Q 4. How do you assess the need for physical restraints?
Assessing the need for physical restraints is a crucial step and must be based on a thorough evaluation of the situation, focusing on imminent risk. It’s not about punishment or convenience; it’s about safety. This assessment must consider the following factors:
- Individual’s behavior: Is the individual exhibiting aggressive behavior, such as hitting, kicking, or verbal threats? What is their level of agitation?
- Environmental factors: Is the environment safe for the individual and those around them? Are there objects that could cause harm?
- Medical condition: Does the individual have a medical condition that contributes to their behavior? Are they experiencing delirium or psychosis?
- Alternative strategies: Have all other de-escalation techniques been attempted, such as verbal calming, distraction, and providing a safe space?
Documentation of this assessment is paramount, detailing the reasons for considering restraints and the specific behaviors observed. A failure to document this process could lead to legal or ethical problems.
Q 5. What are the potential risks and complications associated with physical restraints?
Physical restraints carry several potential risks and complications, including:
- Physical injury: Improper application can cause bruises, abrasions, nerve damage, or even fractures. Pressure sores are a risk from prolonged restraint.
- Psychological trauma: Restraint can be a frightening and humiliating experience leading to anxiety, fear, and post-traumatic stress disorder.
- Increased agitation: Paradoxically, restraint can sometimes increase agitation and aggression.
- Suffocation: Improperly applied restraints can restrict breathing.
- Death: In rare, extreme cases, death can occur due to complications related to restraint.
The potential for these complications emphasizes the need for careful assessment, proper application, and continuous monitoring. Regular checks, detailed documentation, and timely removal of restraints are vital in mitigating these risks.
Q 6. Describe your experience in de-escalating potentially violent situations.
My experience in de-escalating potentially violent situations involves a multifaceted approach emphasizing communication and understanding. I have successfully used various de-escalation techniques, including:
- Active listening: Paying close attention to the individual’s verbal and non-verbal cues to understand their concerns and needs.
- Empathy: Attempting to understand the individual’s perspective and feelings, even if I don’t agree with their actions.
- Calm and reassuring communication: Using a calm, soothing tone and avoiding confrontational language.
- Providing choices: Offering the individual options to regain a sense of control.
- Creating a safe space: Moving the individual to a less stimulating environment.
- Distraction: Shifting the individual’s focus to a different activity or topic.
One specific instance involved an individual experiencing acute psychosis. Through calm communication and distraction, I redirected their aggression, preventing the need for physical restraint and ensuring their safety. My approach always centers on prioritizing safety, building rapport, and seeking to de-escalate through dialogue before considering more restrictive methods.
Q 7. What is your understanding of the least restrictive alternative principle?
The least restrictive alternative principle is a cornerstone of ethical and legal guidelines for using physical restraints. It means that the least restrictive intervention necessary to ensure the safety of the individual and others should always be used. This principle prioritizes preserving the individual’s autonomy and dignity while ensuring safety. Before considering any form of restraint, all less restrictive options should be thoroughly explored and documented. These include verbal de-escalation, environmental modifications, behavioral interventions, medication (under medical supervision), and the use of less restrictive forms of restraint (such as a soft restraint over a mechanical restraint). The choice of intervention should be supported by professional judgement and always prioritized with the individual’s welfare in mind.
For instance, if a patient is becoming agitated, trying to calm them verbally should precede any attempts to apply restraints. If verbal interventions are unsuccessful, consider a less restrictive physical restraint before moving to a more restrictive measure. This principle isn’t just about choosing a restraint; it applies to the entire process of managing potentially violent behavior.
Q 8. How do you ensure the safety of both the individual being restrained and the staff involved?
Ensuring safety during physical restraint is paramount. It’s a delicate balance between protecting the individual and the staff. We achieve this through rigorous training, adherence to protocols, and continuous risk assessment.
For the individual: We prioritize minimizing harm by using the least restrictive restraint necessary, employing proper techniques to avoid injury (such as avoiding pressure points), and consistently monitoring for signs of distress. For example, we might use a less restrictive restraint like a lap belt instead of full restraints if the situation allows. We also ensure the restrained person’s airway is clear and that their position minimizes the risk of choking or injury.
For staff: Safety involves training in proper restraint techniques to prevent injuries from struggling individuals. Teamwork and clear communication are vital. We always use enough trained staff to safely manage the situation – never one person trying to restrain a struggling individual alone. We use de-escalation techniques first, resorting to restraint only as a last resort. Proper personal protective equipment (PPE) like gloves is always used.
Q 9. What documentation is required when using physical restraints?
Comprehensive documentation is crucial for legal and ethical reasons. It provides a record of the events leading to restraint, the type of restraint used, the duration, and any observations made during and after the procedure. This documentation protects both the individual and the staff.
- Incident Report: A detailed account of the behavior leading to restraint, time, location, individuals present, and description of the incident.
- Restraint Log: The type of restraint used, the time of application and release, regular observations on the person’s condition (e.g., pulse, respiration, skin color), and any significant events.
- Nurse’s Notes: If applicable, continuous monitoring and interventions documented by nursing staff.
- Physician’s Orders: If the restraint is ordered by a physician, documentation of those orders must be present.
All documentation should be objective, factual, and signed by the staff involved. Incomplete or inaccurate documentation can lead to serious legal consequences.
Q 10. How do you monitor an individual who is under physical restraints?
Monitoring a restrained individual is ongoing and requires vigilance. The frequency of observation depends on factors like the individual’s condition and the type of restraint used.
Typically, we monitor:
- Vital signs: Pulse, respiration, blood pressure, and skin color should be checked regularly, as per facility protocol (e.g., every 15 minutes, 30 minutes, or hourly).
- Airway: Ensuring the airway remains open and clear is critical. Any signs of respiratory distress necessitate immediate intervention.
- Skin integrity: Checking for pressure sores or skin breakdown, especially over bony prominences, is vital to prevent injury.
- Circulation: Assessing for signs of impaired circulation in the extremities (e.g., pallor, coldness, diminished pulse).
- General comfort: We constantly assess the individual’s comfort level and make adjustments where possible, while still ensuring safety.
All observations should be meticulously documented in the restraint log.
Q 11. What are the signs of potential injury or distress in a restrained individual?
Recognizing signs of injury or distress is essential for immediate intervention. We are trained to look for subtle and overt indicators.
- Respiratory distress: Labored breathing, cyanosis (blue discoloration of skin), wheezing.
- Circulatory compromise: Pale or blue skin, cold extremities, weak or absent pulse.
- Changes in consciousness: Lethargy, confusion, unresponsiveness.
- Pain: Complaints of pain, guarding behavior, facial expressions indicating discomfort.
- Skin breakdown: Redness, blistering, open sores.
- Increased agitation or anxiety: Increased heart rate, sweating, restlessness.
Any of these signs should trigger immediate action, including releasing the restraint (if safe to do so), notifying medical staff, and providing appropriate care. Documentation of these observations is also crucial.
Q 12. What are your strategies for managing resistance during restraint application?
Managing resistance during restraint application requires a calm, controlled approach focused on de-escalation and safety. Force should only be used as a last resort, and then only the minimum necessary to ensure safety.
Strategies include:
- De-escalation techniques: Using calming communication, empathy, and providing clear and simple instructions.
- Teamwork: A well-coordinated team using a standardized approach minimizes the risk of injury to both the individual and staff.
- Proper technique: Using appropriate holds and techniques to minimize injury while effectively controlling the individual.
- Verbal communication: Continuously communicating with the person, providing reassurance and explaining the steps being taken.
- Physical control: Employing appropriate physical techniques to control movement while ensuring safety.
It’s important to remember that the goal is to control behavior, not punish the person. Always prioritize safety and utilize the least restrictive means necessary.
Q 13. How do you communicate with the individual during and after the restraint procedure?
Communication is key throughout the entire process. Before, during, and after the restraint.
Before: Attempt to de-escalate and clearly explain why restraint might be necessary. Use simple and direct language, avoiding jargon or threats.
During: Maintain calm communication. Explain what is happening and why. Reassure the person that they are safe and that the restraint is temporary. Monitor their verbal and non-verbal cues.
After: Once the restraint is removed, offer support and explanations. Acknowledge their feelings and offer an apology if appropriate. This helps foster trust and prevent future incidents. Provide a safe space for them to process their experience.
Documentation of these communications is important, especially if any verbal resistance occurred.
Q 14. What is your understanding of liability and legal ramifications of inappropriate restraint use?
Inappropriate use of physical restraints carries significant legal and ethical implications. It can lead to civil lawsuits, criminal charges, and disciplinary actions.
Liability: Facilities and staff can be held liable for injuries resulting from improper restraint use, including negligence, assault, battery, and false imprisonment. Failure to follow protocols, inadequate training, or excessive force can significantly increase liability.
Legal Ramifications: The legal consequences vary by jurisdiction but can include fines, suspension of licenses, and even imprisonment in severe cases. A strong defense often relies on thorough documentation demonstrating the necessity of the restraint, adherence to protocols, and the use of appropriate force.
Understanding the legal framework governing restraint use is essential for minimizing risk and ensuring the safety and well-being of everyone involved.
Q 15. Describe your experience with different types of restraint equipment.
My experience encompasses a wide range of restraint equipment, from the commonly used methods like limb restraints (both soft and padded) and lap belts to less frequently employed options such as specialized vests and postural supports. I’m familiar with the strengths and limitations of each, understanding that the choice of equipment must always align with the individual’s needs, the specific situation, and the least restrictive approach. For instance, a soft wrist restraint might be suitable for a patient experiencing temporary agitation, whereas a more robust restraint system might be necessary in situations involving significant risk of harm to self or others. My expertise also extends to understanding the proper application and maintenance of this equipment to ensure safety and effectiveness.
- Soft restraints: These are typically made of fabric and are used for individuals who pose a low risk of injury to themselves or others.
- Hard restraints: These are typically made of metal or plastic and are used for individuals who pose a high risk of injury to themselves or others. The use of hard restraints requires careful consideration and rigorous documentation.
- Specialized restraints: These include devices like anti-elopement beds and postural supports, designed to address specific behavioral challenges and should only be used under specific circumstances.
It’s crucial to remember that restraint selection is never arbitrary. It’s a decision that must be made based on a comprehensive risk assessment, considering the individual’s specific needs and behaviors.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you ensure proper training and competency for staff involved in restraint procedures?
Ensuring staff competency in restraint procedures is paramount. Our training program is multi-faceted and includes both theoretical and practical components. It begins with comprehensive classroom sessions covering relevant policies, legal aspects, and the ethical considerations of using physical restraints. We emphasize de-escalation techniques and the importance of non-restraint approaches whenever possible. Then, we move into hands-on training, where staff practice proper restraint techniques using standardized mannequins. This ensures they develop the necessary skills and understand the correct application and release procedures. Regular competency assessments, including both written and practical evaluations, are conducted to ensure ongoing proficiency and to identify areas requiring further training or improvement. We also incorporate regular refresher courses and case studies to keep the training dynamic and relevant.
Furthermore, we emphasize continuous feedback and supervision. Experienced staff mentors new team members, and regular feedback sessions are provided to identify and address any knowledge gaps or skill weaknesses.
Q 17. How often should restraint procedures be reviewed and updated?
Restraint procedures are not static; they must be reviewed and updated regularly, ideally at least annually or whenever significant changes occur in policy, legislation, or best practice guidelines. This review includes an evaluation of the effectiveness of current procedures, identification of any incidents or near misses involving restraints, feedback from staff and individuals who have experienced restraint, and an examination of the latest research and best practices. The review process ensures that our methods are aligned with current standards and that they remain as safe and humane as possible. Changes may involve updating the types of restraints used, modifying the steps involved in the procedure, or implementing new de-escalation strategies. Any updates necessitate a complete retraining of staff.
Think of it like reviewing a safety manual for equipment; it needs regular checks and updates to reflect improvements and technological advancements.
Q 18. What is your understanding of relevant policies and regulations on physical restraints?
My understanding of policies and regulations on physical restraints is extensive and always kept up-to-date. We adhere strictly to all relevant legislation, including those addressing patient rights, safeguarding, and the use of force. We are familiar with the legal frameworks that govern the use of restraints, recognizing the need for informed consent (where possible) and comprehensive documentation. This includes precise records of the circumstances leading to the use of restraints, the type of restraint applied, the duration of the restraint, and the individual’s response. We fully understand the legal implications of inappropriate use of restraints and prioritize minimizing their use only as a last resort after all other de-escalation techniques have been attempted and documented.
We regularly attend professional development courses and stay informed of legal updates in this ever-evolving field. This helps to ensure that our procedures remain compliant and ethical.
Q 19. What is your role in post-restraint care and assessment?
Post-restraint care and assessment is a crucial element of our approach. Immediately after the restraint is released, a thorough assessment is conducted, focusing on the individual’s physical and psychological well-being. This includes monitoring for any signs of injury, checking vital signs, and assessing their emotional state. We provide comfort and support, offering reassurance and addressing any immediate needs. Comprehensive documentation of the post-restraint assessment is vital. This information is used to evaluate the effectiveness of the restraint procedure, to identify any areas for improvement, and to inform future interventions. We also ensure ongoing monitoring and support to prevent future incidents. Depending on the circumstances, a follow-up meeting might be held with the individual and relevant care team members to discuss the incident and develop strategies to prevent recurrence.
Q 20. How do you ensure the dignity and respect of the individual being restrained?
Maintaining the dignity and respect of the individual being restrained is paramount. Our training heavily emphasizes a person-centered approach. We strive to create a calm and reassuring environment, using clear and respectful communication throughout the process. We avoid unnecessary exposure or humiliation and ensure privacy whenever possible. Before initiating a restraint, we make every attempt to explain the reason for the restraint in a way that the individual can understand. We minimize the duration of restraint and regularly monitor the individual’s comfort and needs. Immediate post-restraint care includes a sincere apology, if appropriate, and a commitment to minimizing future instances.
Think of it this way: we treat every individual with the same level of care and respect we would want for ourselves or our loved ones in a similar situation.
Q 21. How do you deal with a situation where restraints are ineffective or necessary?
If restraints prove ineffective or unnecessary, our immediate response involves a reassessment of the situation. This involves reviewing the initial risk assessment, considering if the individual’s behavior has escalated or changed, and determining if alternative strategies or interventions are needed. We may need to consult with other members of the care team, including physicians, nurses, and mental health professionals, to develop a more comprehensive plan. This could involve medication adjustments, changing the environment, or seeking specialized support. If restraints are deemed unnecessary, they are immediately released. If the individual’s behavior continues to pose a risk, we document our efforts and the rationale for seeking alternative intervention methods. Our goal is always to find the least restrictive and most effective method of managing the situation while prioritizing the safety and well-being of everyone involved.
Q 22. What are the alternatives to physical restraints and when should they be considered?
Alternatives to physical restraints are crucial for ensuring the safety and well-being of individuals while minimizing the use of restrictive measures. These alternatives focus on de-escalation, preventative strategies, and creating a supportive environment.
- Environmental Modifications: Altering the physical space to reduce stimulation (e.g., quieter rooms, fewer distractions) can significantly decrease agitation.
- Behavioral Interventions: Techniques like positive reinforcement, redirection, and providing choices empower individuals and help prevent escalation. For example, offering a preferred activity instead of demanding compliance can be highly effective.
- Communication Strategies: Active listening, using calm and reassuring tones, and validating feelings can help build rapport and diffuse tense situations.
- Medication Management: In some cases, medication may be necessary to manage underlying conditions that contribute to challenging behaviors.
- Sensory Strategies: Using calming sensory tools such as weighted blankets, fidget toys, or aromatherapy can help regulate sensory input and reduce anxiety.
Alternatives should be considered before resorting to physical restraints. They are the preferred approach whenever feasible, especially when an individual exhibits signs of distress or agitation. A thorough assessment of the situation, the individual’s needs, and available resources is essential before deciding on any intervention, including restraints.
Q 23. Describe a time you had to make a difficult decision regarding the use of restraints.
One particularly challenging situation involved a resident with dementia who became increasingly agitated and aggressive during the evening. He was exhibiting behaviors that posed a risk to himself and others. While our team had exhausted many de-escalation techniques, including redirection, calming communication, and sensory interventions, the situation escalated, and he attempted to strike a staff member.
The decision of whether or not to use restraints was agonizing. We knew restraints could cause distress and potential injury, but we also had a duty to protect the resident and staff. Following our agency’s strict protocol, we thoroughly documented our attempts at de-escalation and consulted with the supervisor. After determining that all less restrictive interventions had failed, and the resident’s behavior posed an imminent threat, we proceeded with a minimal restraint intervention while prioritizing the resident’s safety and comfort. Post-incident, we debriefed as a team to review what happened, identify areas for improvement in our response, and reassess the resident’s care plan to prevent future incidents.
Q 24. How do you handle a situation where there is a conflict between staff members regarding the use of restraints?
Conflicts regarding restraint use are addressed promptly and professionally. A calm and neutral environment is essential. My approach involves the following steps:
- Facilitate Open Communication: Encourage staff members to express their concerns and perspectives openly, ensuring all feel heard and respected.
- Review Agency Policy: Refer back to the established policy and procedures regarding restraint use to provide a clear framework for the discussion.
- Assess the Situation: Examine the facts of the event objectively, analyzing the actions leading to the use of restraints and whether protocol was followed correctly.
- Mediate and Facilitate Consensus: Guide the discussion towards a common understanding. If the disagreement persists, I would involve a supervisor to oversee a more formal review process.
- Provide Training Reinforcement: If the disagreement stems from knowledge gaps or differing interpretations of procedures, additional training may be necessary.
It is crucial to emphasize that teamwork and shared responsibility for resident safety are paramount.
Q 25. How would you respond to allegations of improper restraint use?
Allegations of improper restraint use are taken extremely seriously. My response is guided by the following steps:
- Immediate Investigation: A thorough and impartial investigation must be initiated immediately. This will include gathering evidence (video footage, incident reports, witness statements) and interviewing all involved parties.
- Compliance Review: The agency’s restraint policies and procedures are reviewed to determine if they were adhered to.
- Documentation Review: All relevant documentation, including restraint records and care plans, is meticulously examined to ensure accuracy and completeness.
- Transparency and Communication: Maintain open communication with the individual, their family (if applicable), and regulatory bodies throughout the investigation.
- Corrective Action: If violations are found, appropriate disciplinary action will be implemented, including retraining or remedial measures.
- Reporting: All findings are reported to the appropriate authorities, as mandated by law and regulations.
Integrity and adherence to ethical standards are critical throughout the entire process.
Q 26. How do you maintain accurate and complete records of restraint use?
Maintaining accurate and complete records of restraint use is vital for legal, ethical, and quality-of-care reasons. Our system employs a multi-faceted approach:
- Detailed Incident Reports: These reports capture the events leading to restraint, the type of restraint used, the duration of the restraint, and any observations regarding the individual’s response.
- Electronic Documentation: We utilize electronic health records to ensure timely and accurate recording.
- Signatures and Verification: All reports and records require signatures from the staff involved to verify their accuracy and accountability.
- Regular Reviews: Supervision reviews the records regularly for completeness, consistency, and adherence to policies.
- Data Analysis: We analyze restraint data to identify patterns and trends that may indicate a need for improvements in care planning or training.
This comprehensive approach provides a transparent and verifiable record of restraint use, contributing to continuous improvement in our practices.
Q 27. What continuing education have you undertaken regarding physical restraint techniques and practices?
I consistently engage in continuing education to stay abreast of best practices in physical restraint techniques and practices. Recent trainings have included:
- Crisis Prevention Intervention (CPI): This comprehensive program teaches de-escalation techniques, physical intervention strategies (only when absolutely necessary), and post-intervention procedures.
- Positive Behavioral Support (PBS): This approach focuses on understanding the root causes of challenging behaviors and developing individualized support plans to promote positive behaviors.
- Trauma-Informed Care: This training emphasizes the impact of trauma on behavior and provides strategies for creating a safe and supportive environment for individuals who have experienced trauma.
- Updates on legal and regulatory requirements related to restraint use: Staying informed about changes in relevant legislation and guidelines is crucial to maintain compliance and ensure best practice.
I believe continuous professional development is vital for providing high-quality, safe, and ethical care.
Q 28. Describe your experience with reporting incidents involving physical restraints.
Reporting incidents involving physical restraints is a critical aspect of our accountability and commitment to safety. My experience involves:
- Immediate Reporting: All incidents are reported immediately to the supervisor and documented in the incident report system.
- Detailed Reporting: Reports include objective and factual information, avoiding subjective interpretations.
- Timely Follow-up: After the initial report, there’s a formal review process that involves a debriefing session and an assessment of the incident to identify any areas for improvement in our processes and training.
- Regulatory Reporting: When required by law or regulations, incidents are reported to the relevant authorities, adhering strictly to reporting guidelines.
- Internal Reviews: We conduct regular internal reviews of restraint data to identify patterns, trends, and areas for improvement in our systems.
Transparency and accountability are critical to ensuring continuous improvement in our use of physical restraints and protecting the safety of both staff and residents.
Key Topics to Learn for Physical Restraint Training Interview
- Legal and Ethical Considerations: Understanding the legal framework surrounding physical restraint, including laws, policies, and ethical implications. This includes knowing when restraint is justified and the potential consequences of improper use.
- Restraint Techniques and Procedures: Mastering various restraint techniques, including their proper application, release procedures, and safety precautions. Practical experience and the ability to explain the rationale behind each technique are crucial.
- Risk Assessment and De-escalation Strategies: Demonstrating knowledge of identifying and assessing potential risks before resorting to physical restraint. Highlighting skills in verbal de-escalation and conflict resolution techniques is vital.
- Post-Restraint Procedures: Understanding the necessary steps following a restraint incident, including documentation, reporting, and follow-up care. Knowledge of injury assessment and reporting protocols is key.
- Safety and Injury Prevention: Emphasizing the importance of minimizing injury risk to both the individual being restrained and the personnel involved. This includes understanding proper body mechanics and safe handling procedures.
- Documentation and Reporting: Demonstrating competence in accurate and thorough documentation of restraint incidents, adhering to all relevant reporting requirements and standards. This includes the ability to clearly and concisely communicate details in writing.
- Teamwork and Communication: Highlighting the importance of effective communication and teamwork within a multidisciplinary setting during restraint situations. Emphasize the need for clear communication and coordination among team members.
Next Steps
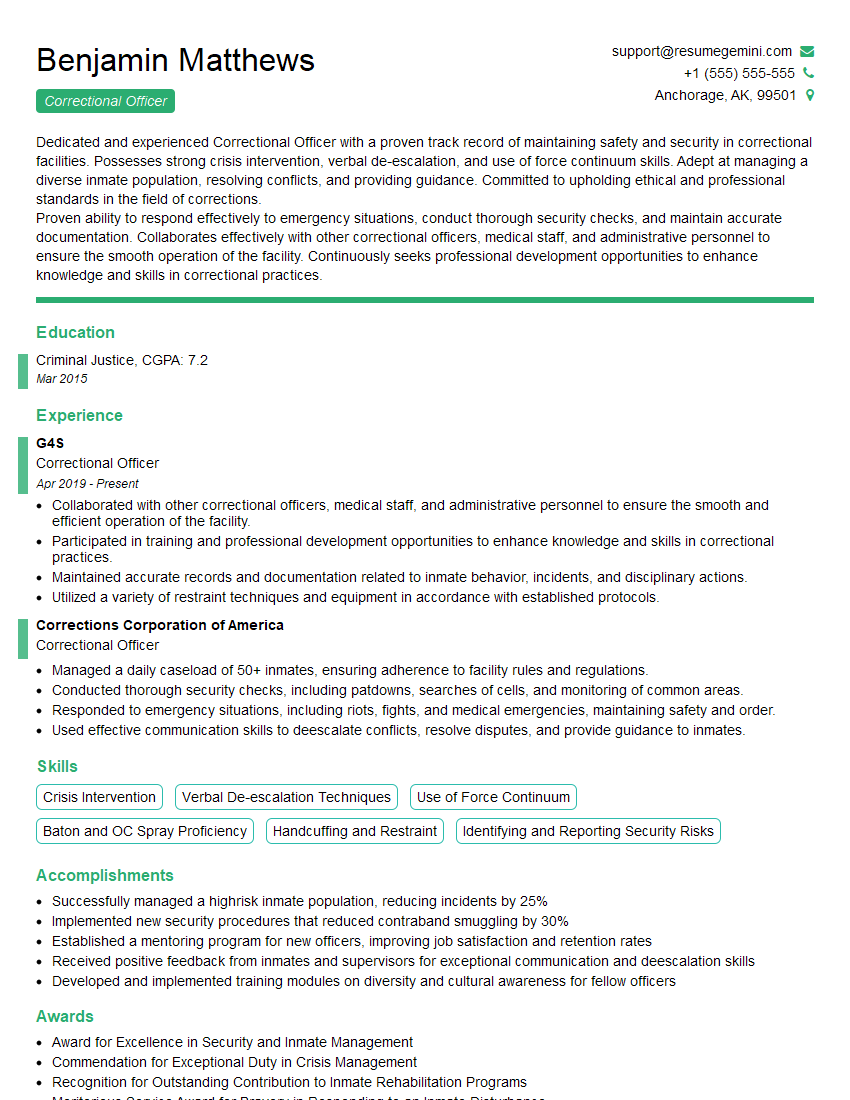
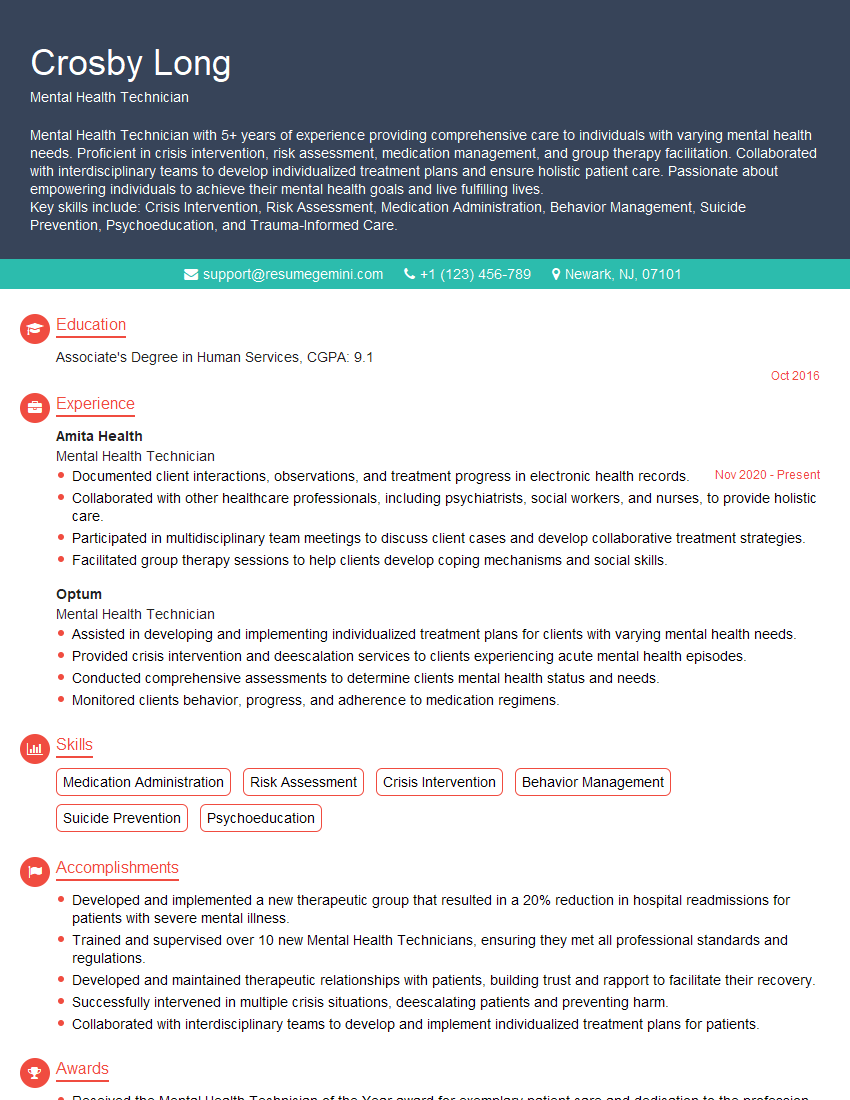
Mastering Physical Restraint Training is essential for career advancement in many fields, demonstrating your commitment to safety and responsible intervention. To maximize your job prospects, create a strong, ATS-friendly resume that effectively highlights your skills and experience. ResumeGemini is a trusted resource that can help you build a professional resume tailored to your specific career goals. Examples of resumes tailored to Physical Restraint Training are available to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO