Are you ready to stand out in your next interview? Understanding and preparing for Scribing Techniques interview questions is a game-changer. In this blog, we’ve compiled key questions and expert advice to help you showcase your skills with confidence and precision. Let’s get started on your journey to acing the interview.
Questions Asked in Scribing Techniques Interview
Q 1. Explain the difference between EMR and EHR.
While both EMR (Electronic Medical Record) and EHR (Electronic Health Record) are digital versions of a patient’s medical history, there’s a key distinction. Think of an EMR as a snapshot of a patient’s care within a single healthcare system, like a doctor’s office or a hospital. It contains information relevant to that specific provider. An EHR, on the other hand, is a more comprehensive, longitudinal record that follows the patient across multiple healthcare settings. It aims to provide a complete view of a patient’s health journey, integrating data from different sources like hospitals, clinics, and labs. For example, an EMR might contain notes from a recent visit to a cardiologist, while the EHR would include that information plus previous records from a general practitioner, allergy test results, and hospital discharge summaries.
In essence, an EHR is a broader, more interconnected system designed for better patient care coordination and data sharing, whereas an EMR is more limited in scope.
Q 2. Describe your experience with medical terminology.
My experience with medical terminology is extensive. During my years as a medical scribe, I’ve immersed myself in the language of medicine, learning not only the basic prefixes, suffixes, and root words but also the nuances of terminology specific to various medical specialties. I’m proficient in understanding and documenting complex medical conditions, procedures, and findings. I regularly consult medical dictionaries and online resources to ensure accuracy and stay updated with evolving terminology. For example, I can confidently interpret and document the significance of a diagnosis such as “idiopathic pulmonary fibrosis” or accurately transcribe the details of a complex surgical procedure like a “coronary artery bypass graft”. My understanding extends to differentiating between similar-sounding terms to ensure the physician’s notes reflect the precise clinical details.
Q 3. What software are you proficient in for scribing?
I’m proficient in using a variety of medical scribing software, including Epic, Cerner, and Meditech. My experience extends to both the charting functionalities and the specific features tailored for medical scribes. I’m adept at using these platforms to efficiently record patient history, physical examinations, diagnoses, and treatment plans, while adhering to HIPAA compliance standards. I understand the importance of navigating the software quickly and accurately to ensure minimal disruption to the physician’s workflow. Furthermore, I’m comfortable learning new platforms as needed, demonstrating my adaptability and commitment to professional growth. For instance, I can quickly navigate Epic’s charting interface to efficiently document a patient’s medications and allergies, or utilize Cerner’s note-templating options to streamline the documentation process.
Q 4. How do you handle interruptions during scribing?
Handling interruptions is a crucial skill for a medical scribe. I approach interruptions professionally and efficiently. When interrupted, I pause my scribing, politely acknowledge the interruption, and then efficiently address the issue or question before resuming my work. I use techniques like briefly summarizing my current task to quickly regain my focus once the interruption is resolved. I strive to minimize the disruption to the physician’s workflow by quickly getting back to my task. For example, if a nurse needs to ask the physician a question, I take the opportunity to quickly review what I’ve already documented to ensure accuracy and keep the flow of notes running smoothly.
Q 5. What is your typing speed (WPM)?
My typing speed is consistently above 75 words per minute (WPM) with a high degree of accuracy. However, speed is only part of the equation. Accuracy and comprehension are paramount. I prioritize precise documentation over sheer speed. I can adapt my typing speed to the physician’s dictation pace, ensuring I don’t compromise accuracy for speed.
Q 6. How do you ensure accuracy in your notes?
Ensuring accuracy is my top priority. I employ several strategies to achieve this. Firstly, I actively listen and engage with the physician’s dictation, clarifying any ambiguous terms or phrases immediately. I use spell check and grammar check features within the EMR/EHR system. Secondly, I regularly review my notes for completeness and accuracy before submitting them. Finally, I utilize the software’s features such as auto-suggestions and templates to minimize errors. I also take advantage of any opportunity to ask clarifying questions. If I’m unsure of a medical term or a patient’s specific detail, I’ll politely interrupt the physician for clarification to prevent inaccuracies. This proactive approach has consistently led to highly accurate and comprehensive medical notes.
Q 7. Describe your experience with different medical specialties.
My experience spans several medical specialties, including cardiology, pulmonology, gastroenterology, and general internal medicine. This diverse exposure has allowed me to develop a strong understanding of the unique terminology and workflow of each specialty. I’m comfortable working with different physicians and adapting to their individual communication styles. For instance, while a cardiologist might focus on echocardiogram results, a pulmonologist might emphasize lung function tests. I’m able to effectively transcribe and organize the pertinent information, regardless of the specialty, demonstrating adaptability and a strong command of medical terminology across various disciplines.
Q 8. How do you manage multiple tasks simultaneously?
Managing multiple tasks simultaneously as a scribe requires a structured approach. I utilize several techniques, including prioritization based on urgency and physician needs. For example, if one physician needs immediate assistance documenting a critical finding, I’ll focus on that first, even if another physician has a less urgent request. I also employ time-blocking techniques, allocating specific time slots to different physicians or tasks. Think of it like a conductor of an orchestra – each instrument (physician) needs attention, but some need it more urgently than others. This structured approach, combined with strong organizational skills and note-taking, ensures I can handle multiple tasks efficiently and accurately.
- Prioritization based on urgency.
- Time-blocking for different physicians.
- Effective note-taking for context switching.
Q 9. How do you handle sensitive patient information?
Handling sensitive patient information is paramount. My approach involves strict adherence to HIPAA regulations and the specific protocols established by the healthcare facility. This includes never discussing patient information outside of the clinical setting, using secure communication channels for any patient-related discussions, and properly securing all physical and electronic patient records. I also understand that even seemingly innocuous information, like a patient’s name, can be a privacy risk if disclosed inappropriately. Confidentiality is not just a rule; it’s a fundamental aspect of the job that I treat with utmost seriousness.
- Strict adherence to HIPAA regulations.
- Secure communication channels only.
- Proper disposal and storage of physical and electronic records.
Q 10. Explain your understanding of HIPAA regulations.
HIPAA, the Health Insurance Portability and Accountability Act, is a US federal law protecting the privacy and security of Protected Health Information (PHI). My understanding encompasses its key provisions, including the privacy rule, security rule, and breach notification rule. The privacy rule dictates how PHI can be used, disclosed, and protected. The security rule mandates administrative, physical, and technical safeguards to protect electronic PHI. Finally, the breach notification rule outlines procedures for reporting data breaches. As a scribe, I consistently apply these principles, ensuring that all my actions respect patient confidentiality and data security. For example, I only access information relevant to the immediate clinical task and immediately log out of systems when finished.
Q 11. How do you prioritize tasks when multiple physicians need assistance?
When multiple physicians need assistance simultaneously, I prioritize based on several factors: urgency of the clinical situation, the physician’s workflow, and the complexity of the task. For example, if one physician is conducting an emergency procedure, their needs are paramount. If several physicians have similar levels of urgency, I’ll consider their workflow – for instance, if one is about to move on to another patient, I would prioritize them. I communicate clearly with each physician, setting expectations and managing their requests efficiently. It’s like a triage system; the most critical cases get immediate attention. Effective communication is key to avoid frustration and ensure everyone receives the necessary support.
Q 12. Describe a challenging scribing experience and how you overcame it.
During a particularly busy shift, a physician was rapidly dictating notes for three patients concurrently, each with complex medical histories. My initial attempts to keep up felt overwhelming, resulting in some incomplete documentation. To overcome this, I employed a more structured approach. First, I slowed the dictation process down, asking the physician to clarify when necessary. Second, I actively used my note-taking system more efficiently, using abbreviations and keywords to capture the key information swiftly. Finally, I focused on accurate capture over speed, ensuring the physician reviewed and approved the notes before moving to the next patient. This experience reinforced the importance of clear communication, organized note-taking, and focusing on quality over speed in high-pressure situations.
Q 13. What is your experience with chart review and correction?
Chart review and correction are essential components of my role. I regularly review charts for accuracy, completeness, and consistency before the physician signs off on them. This often involves checking for missing information, verifying medication lists, and ensuring the notes accurately reflect the patient’s condition and treatment plan. If I identify discrepancies or errors, I bring them to the physician’s attention immediately. I also follow established protocols for correcting errors, ensuring the corrections are properly documented and maintain audit trails. Accuracy and attention to detail are crucial in this aspect of scribing, preventing errors that could impact patient care.
Q 14. How familiar are you with different documentation styles?
I’m familiar with various documentation styles, including SOAP (Subjective, Objective, Assessment, Plan), CHEDDAR (Chief Complaint, History, Examination, Details, Drugs, Assessment, Return), and narrative styles. My understanding extends to the nuances of each style, such as the specific information required for each section and how to structure the notes effectively. I can adapt my scribing style to meet the physician’s preference and the institution’s requirements. This adaptability is crucial for seamless collaboration and accurate documentation. Understanding these different styles enables me to work effectively with a wider range of physicians and healthcare settings.
Q 15. How do you maintain confidentiality in a busy medical environment?
Maintaining confidentiality in a busy medical environment is paramount. It’s not just about following regulations like HIPAA; it’s about building a culture of respect for patient privacy. My approach is multi-faceted.
- Physical Security: I ensure all patient charts and electronic records are stored securely, following facility protocols for access and disposal. This includes logging out of computer systems promptly and never leaving sensitive documents unattended.
- Digital Security: I utilize strong passwords, adhere to data encryption protocols, and am vigilant about phishing attempts and other online threats. I understand and follow all institution’s policies regarding data access and security.
- Communication: I only discuss patient information with authorized personnel and only in appropriate settings. I avoid discussing patients in public areas or hallways. If I need to share information, I do so using secure methods and only the minimum necessary information.
- Professional Boundaries: I understand the importance of maintaining professional boundaries and never disclosing patient information to anyone outside the designated medical team, even family members without proper authorization.
- Ongoing Education: I stay updated on the latest confidentiality regulations and best practices to ensure my methods remain current and effective. I actively participate in any training sessions or workshops related to patient privacy and data security.
For example, I once noticed a colleague inadvertently leaving a patient chart open on a desk. I discreetly alerted them and reminded them of the importance of securing sensitive information. This small act prevents potential breaches.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is your experience with different medical devices and equipment?
My experience with medical devices and equipment spans a wide range, encompassing both commonly used and specialized instruments. I’m proficient in operating and documenting the use of:
- Electronic Health Records (EHR) Systems: I’m familiar with various EHR systems, including Epic, Cerner, and Meditech, and I can navigate them efficiently to access and document patient information accurately.
- Dictation Software and Transcription Equipment: I’m skilled in using digital dictation systems, both voice-to-text software and traditional dictation equipment, ensuring accurate transcription of medical procedures and notes.
- Medical Imaging Systems: I have experience reviewing and documenting information from various imaging modalities such as X-rays, CT scans, and MRIs, understanding the importance of clear labeling and accurate record-keeping.
- Specialized Equipment (as applicable to the role): Depending on the specific clinical setting, I’ve had experience documenting information generated from specialized equipment – ranging from operating room equipment to cardiac monitoring devices. My training has focused on understanding the functional use of the instruments and not operating or calibrating them myself.
I understand that my role is not to operate these devices, but to accurately document the information they provide. I always prioritize understanding the context of the data generated by these devices so that I can accurately reflect it in the medical record.
Q 17. Explain your knowledge of medical abbreviations.
A solid grasp of medical abbreviations is critical for efficient and accurate documentation. My knowledge encompasses a broad range, including common abbreviations like:
BP(Blood Pressure)HR(Heart Rate)RR(Respiratory Rate)O2 Sat(Oxygen Saturation)Dx(Diagnosis)Rx(Prescription)Hx(History)
Beyond the common ones, I continually update my knowledge base with less frequent or specialty-specific abbreviations, carefully cross-referencing and verifying their meanings to prevent errors. I understand that using unverified or unclear abbreviations is potentially hazardous, and therefore I prioritize accuracy and clarity. If I encounter an abbreviation I am unsure of, I always clarify its meaning with the physician or a knowledgeable colleague before using it in my documentation.
For instance, understanding the subtle differences between abbreviations like TIA (Transient Ischemic Attack) and CVA (Cerebrovascular Accident) is vital for correct interpretation and documentation.
Q 18. How do you ensure the completeness and accuracy of medical reports?
Completeness and accuracy are non-negotiable in medical reports. I employ a systematic approach to ensure both:
- Verification and Clarification: I meticulously review all dictated or handwritten notes, clarifying any ambiguities or missing information with the physician before finalizing the report. I use standardized templates to ensure all essential fields are included.
- Consistent Formatting and Style: I adhere to established formatting guidelines, ensuring clarity and readability. This includes using proper grammar, punctuation, and consistent terminology throughout the report.
- Cross-referencing: I verify information across different sources, including patient charts, lab results, and imaging reports, to identify any inconsistencies or missing data. This helps prevent errors and omissions.
- Proofreading and Editing: I perform a thorough proofread of each report, checking for spelling and grammatical errors, as well as any inconsistencies in data.
- Timely Completion: I prioritize timely completion of reports to minimize delays in patient care and ensure prompt billing.
For instance, if a physician’s dictation mentions a specific lab value, I always verify the value in the patient’s lab results to ensure it’s correctly transcribed.
Q 19. How familiar are you with different medical billing and coding practices?
While I don’t directly handle medical billing and coding, I’m familiar with the general principles and their importance to accurate documentation. My understanding includes:
- ICD and CPT Codes: I understand the importance of accurate diagnoses (ICD codes) and procedures (CPT codes) for proper reimbursement and tracking of medical services. I’m trained to recognize the information needed for these codes to be accurately assigned by the billing department.
- Medical Necessity: I know that clear and accurate documentation is crucial in demonstrating medical necessity for procedures and treatments. Poor documentation can lead to denied claims.
- Compliance: I understand that accurate coding and billing practices are vital for compliance with regulatory requirements.
By ensuring complete and accurate documentation, I play a supportive role in facilitating the billing process. My focus on detail and precision indirectly assists in minimizing billing errors and delays.
Q 20. Describe your ability to work under pressure and meet deadlines.
Working under pressure and meeting deadlines is a regular part of my role. I manage this effectively by utilizing organizational skills and prioritizing tasks.
- Prioritization: I use task management techniques to prioritize urgent tasks, ensuring time-sensitive reports are completed on time. I focus on the highest priority tasks first.
- Time Management: I’m adept at breaking down large tasks into smaller, manageable steps and allocating appropriate time for each. I utilize time-blocking techniques to allocate specific time slots for each task.
- Multitasking: I can effectively manage multiple tasks simultaneously without compromising the quality of my work. I avoid context switching unnecessarily.
- Stress Management: I use effective stress management techniques, such as taking short breaks and practicing mindfulness, to maintain focus and productivity under pressure.
For example, during a particularly busy period with multiple urgent reports, I organized my workload using a priority matrix, ensuring that critical reports were completed first without compromising accuracy.
Q 21. How do you adapt to changes in physician preferences or documentation guidelines?
Adaptability is essential in this field. Physicians have individual preferences and documentation guidelines change over time. My approach involves:
- Open Communication: I actively communicate with physicians to understand their preferences and any specific requirements they may have for documentation.
- Proactive Learning: I stay updated on the latest documentation guidelines and best practices through professional development, attending training sessions, and reviewing updated institutional guidelines.
- Flexibility and Quick Learning: I’m quick to learn and adapt to new systems, templates, and physician preferences, minimizing any disruption to workflow.
- Feedback and Continuous Improvement: I value constructive criticism and use feedback to refine my techniques and improve my efficiency in meeting evolving documentation needs.
For example, when our institution transitioned to a new EHR system, I proactively sought out training and quickly adapted to the new platform, ensuring a seamless transition in my workflow.
Q 22. Describe your experience with different types of legal documents.
My experience encompasses a wide range of legal documents, including depositions, court hearings, arbitrations, client interviews, and various forms of legal correspondence. I’ve worked with documents pertaining to diverse legal fields such as personal injury, family law, corporate law, and criminal defense. This broad exposure has familiarized me with the unique structural and stylistic nuances of different document types. For instance, a deposition transcript requires meticulous attention to the question-and-answer format and accurate representation of objections, while a court hearing transcript demands precise recording of witness testimony and judge’s rulings. I’m comfortable navigating the complexities of each, ensuring accurate and complete transcription.
- Depositions: I’m adept at handling the fast-paced nature of depositions and capturing even subtle shifts in tone and emphasis.
- Court Hearings: I’m experienced in managing multiple speakers and distinguishing between various voices, ensuring clarity amidst overlapping dialogue.
- Client Interviews: I understand the importance of maintaining confidentiality and preserving the integrity of sensitive information shared during client interviews.
Q 23. What is your experience with legal terminology and jargon?
My experience with legal terminology is extensive. I understand and accurately transcribe terms such as voir dire, subpoena, habeas corpus, and numerous others. I have developed a robust legal vocabulary through years of experience and continuous self-study. I rely on legal dictionaries and online resources to ensure I correctly interpret and transcribe less frequently encountered terms. I prioritize context to aid understanding and accuracy, and when uncertain, I flag the term for review. Think of it like learning a specialized language – with consistent practice and attention to detail, complex terms become part of my working lexicon. I also actively maintain a personal glossary of commonly used legal terms to improve my efficiency and accuracy.
Q 24. How do you ensure accuracy and completeness in legal transcription?
Accuracy and completeness are paramount in legal transcription. My approach involves a multi-layered quality control process. Firstly, I employ advanced audio equipment and software to ensure high-quality audio capture, minimizing background noise and distortion. Secondly, I utilize professional transcription software which offers features such as foot pedal control for precise timestamps and playback capabilities for verification. Thirdly, I follow a rigorous proofreading process, comparing my transcript against the audio multiple times to identify and correct any errors, ensuring perfect accuracy. Furthermore, I always adhere to the strict formatting requirements specific to each type of document to maintain completeness and consistency. If I encounter any ambiguous audio, I flag it for clarification.
Q 25. How do you maintain confidentiality in a legal setting?
Confidentiality is of utmost importance. I strictly adhere to all relevant privacy laws and regulations. This includes signing confidentiality agreements, securely storing all audio files and transcripts, and only accessing and sharing information on a need-to-know basis. I use secure cloud storage and password-protected devices to ensure data is protected from unauthorized access. My workspace is private and free from distractions to prevent accidental disclosure of confidential information. Furthermore, I maintain a strict professional code of ethics, understanding the implications of breaching confidentiality in a legal context.
Q 26. How do you handle conflicting information during scribing?
Handling conflicting information requires careful attention and meticulous record-keeping. When discrepancies arise, I follow a structured process. First, I carefully review the audio to verify the source of the conflict. Second, I document the conflict clearly in the transcript, using brackets and notations to indicate uncertainty or discrepancies. This ensures complete transparency and prevents misrepresentation. Finally, I flag the conflicting information for clarification by the relevant parties. This approach ensures that the final transcript accurately reflects the conflicting information, allowing the involved parties to address the discrepancies.
Q 27. Describe your experience with audio recording equipment.
I have extensive experience with various audio recording equipment, including professional-grade digital recorders, microphones (both lavalier and tabletop), and audio software. I’m familiar with adjusting settings such as gain, sample rate, and bit depth to optimize audio quality. I understand the importance of properly testing equipment before each recording session to ensure optimal performance. My expertise extends to troubleshooting common audio issues such as background noise and distortion, and I’m adept at using audio editing software to enhance audio quality where necessary, while still maintaining the integrity of the recording.
Q 28. How do you improve your listening and comprehension skills?
Continuous improvement of my listening and comprehension skills is an ongoing process. I regularly practice active listening techniques, focusing on understanding the nuances of speech and identifying key information amidst distractions. I utilize various resources such as online courses, podcasts, and audiobooks to expand my vocabulary and improve my comprehension of different accents and speech patterns. Furthermore, I engage in regular self-assessment, reviewing my work and identifying areas for improvement. By actively seeking feedback and continuously refining my skills, I maintain a high level of proficiency in legal transcription.
Key Topics to Learn for Scribing Techniques Interview
- Listening and Comprehension: Mastering active listening to accurately capture key information and nuances during meetings or presentations.
- Note-Taking Strategies: Developing efficient note-taking methods like shorthand, symbol systems, or mind-mapping to concisely document information.
- Data Organization and Synthesis: Structuring notes logically, identifying key themes, and summarizing complex information into clear and coherent narratives.
- Transcription Accuracy and Speed: Achieving high accuracy in transcribing audio or visual information while maintaining efficient speed.
- Technical Proficiency (Software/Hardware): Demonstrating familiarity with relevant software (e.g., transcription tools) and hardware (e.g., recording devices).
- Professionalism and Communication: Understanding the importance of maintaining confidentiality, meeting deadlines, and communicating effectively with clients or colleagues.
- Problem-Solving and Adaptability: Handling challenges such as poor audio quality, technical difficulties, or ambiguous information with resilience and resourcefulness.
- Legal and Ethical Considerations: Understanding relevant legal and ethical guidelines related to data privacy and information handling.
Next Steps
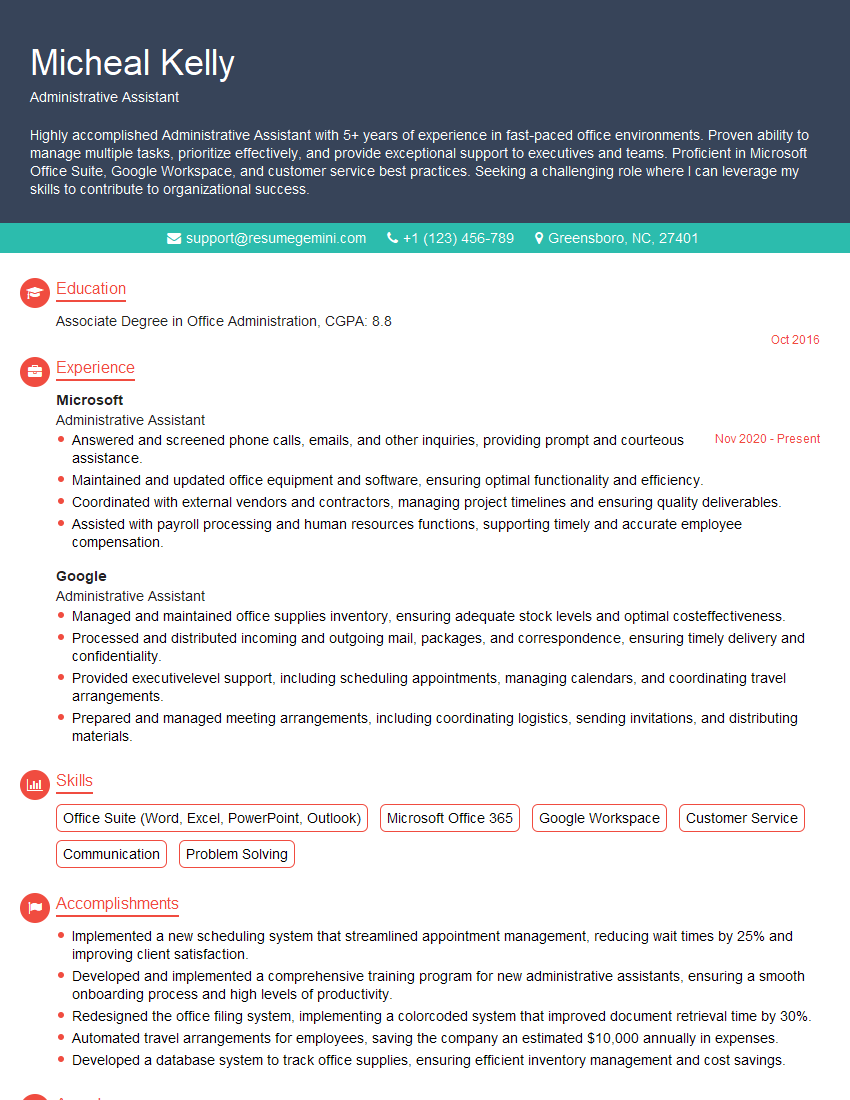
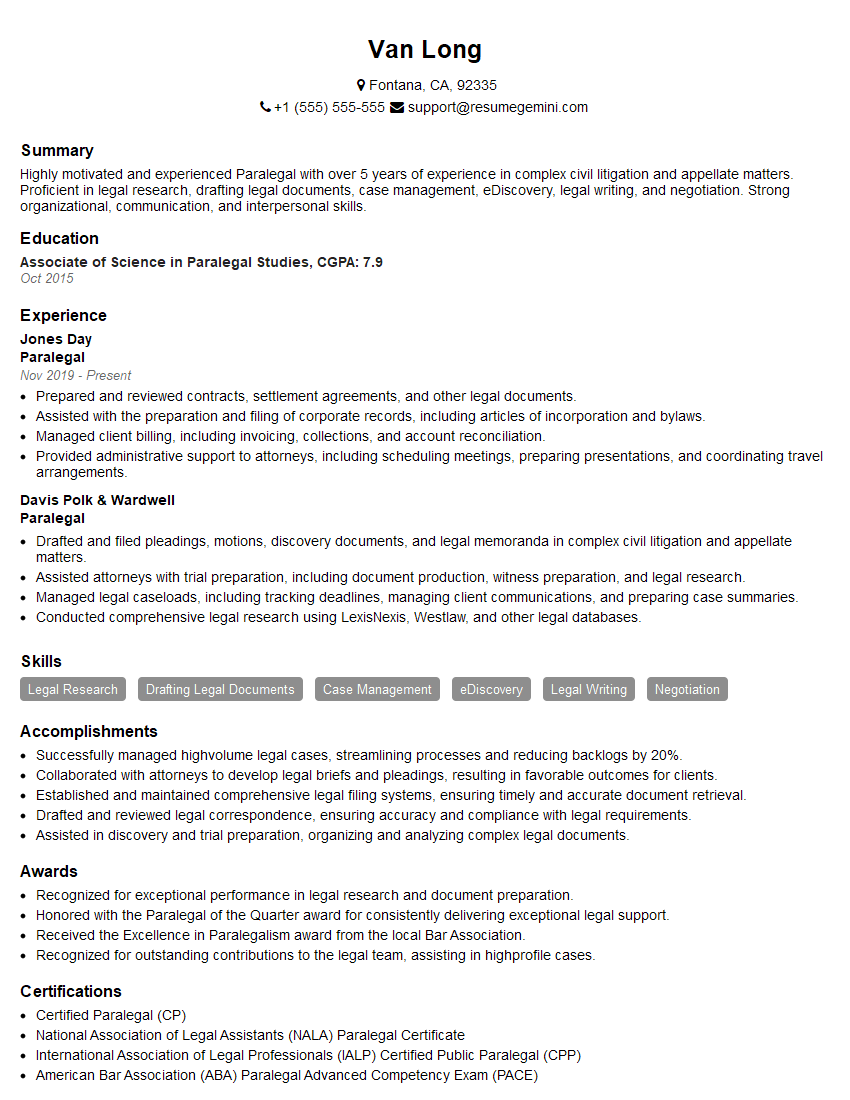
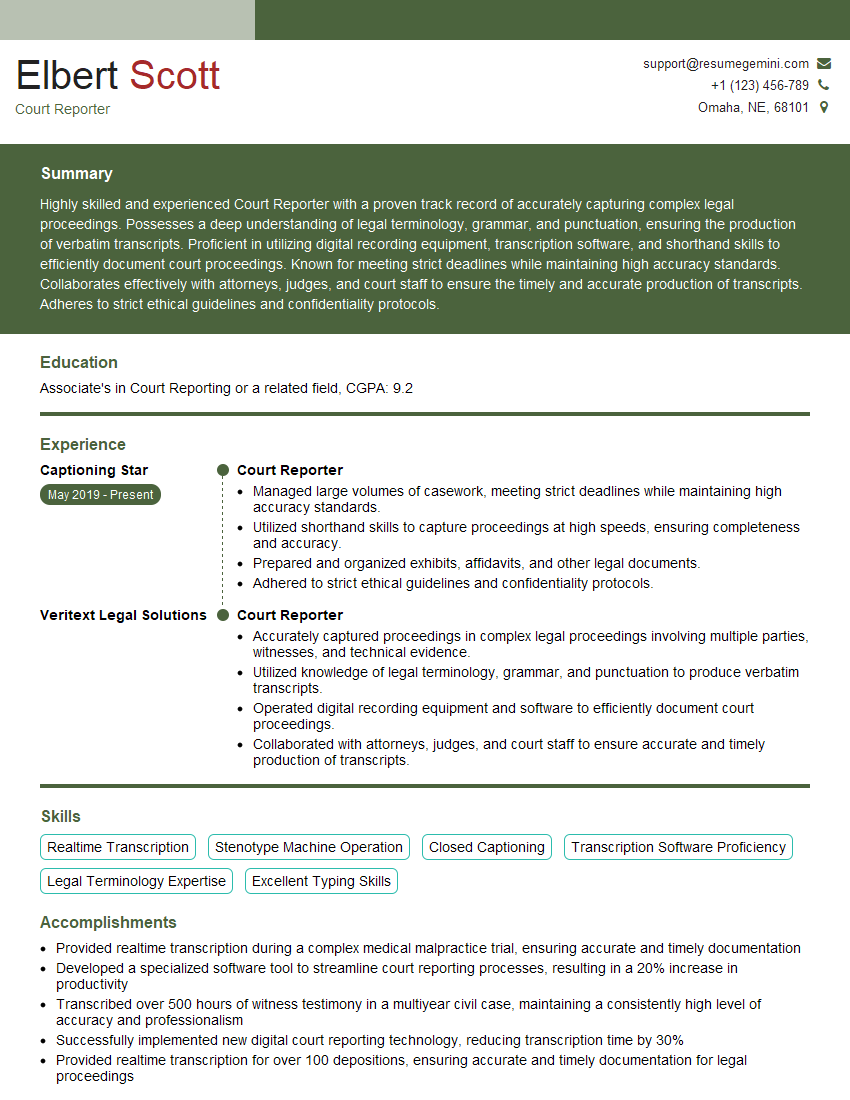
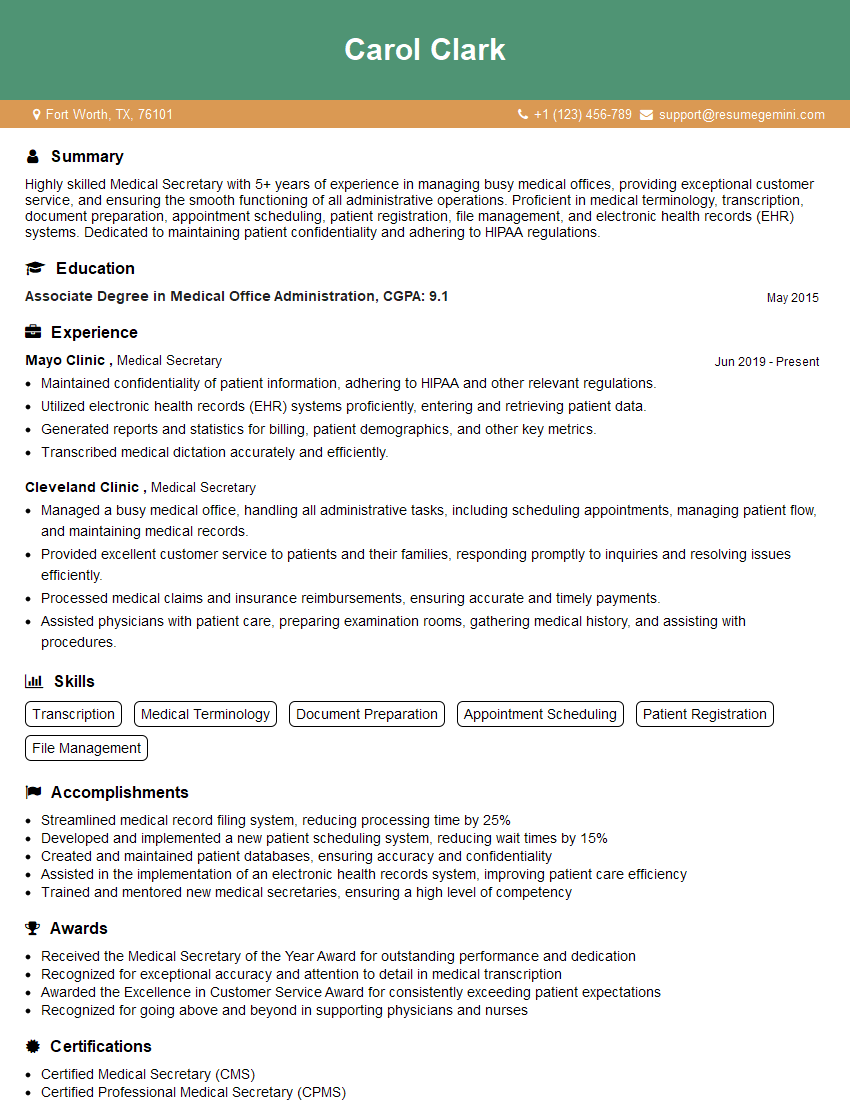
Mastering scribing techniques opens doors to exciting career opportunities in diverse fields requiring accurate and efficient documentation. To maximize your job prospects, invest in crafting an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini can be a valuable resource in this process, providing tools and guidance to build a professional resume that stands out. Examples of resumes tailored specifically to Scribing Techniques are available to help you showcase your unique qualifications. Take the next step towards your dream career today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO