Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Sensory Motor Skills Development interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Sensory Motor Skills Development Interview
Q 1. Explain the concept of sensory integration.
Sensory integration is the neurological process of organizing sensory information from the body and the environment, and using this information to plan and execute adaptive responses. Think of it like this: your brain is a conductor, and all your senses (sight, sound, touch, taste, smell, movement, and body position) are the musicians in an orchestra. Sensory integration is how the conductor organizes these musicians to create a harmonious and functional performance. Without proper integration, the ‘orchestra’ might sound chaotic, leading to difficulties with everyday tasks.
For example, a child struggling with sensory integration might find the feel of certain fabrics overwhelming, leading to sensory defensiveness, or they might struggle to follow instructions in a noisy classroom because their auditory system is not effectively filtering out extraneous sounds. This process is crucial for everything from motor skills to cognitive functions.
Q 2. Describe the typical developmental milestones of sensory motor skills in children.
Typical sensory-motor development follows a predictable, yet variable, timeline. Early milestones involve reflexive movements, gradually transitioning to voluntary control. Here are some key developmental stages:
- Infancy (0-12 months): Reflexes like rooting and grasping give way to purposeful reaching, grasping, and eventually, crawling and sitting. Sensory exploration through touch, mouth, and vision is intense.
- Toddlerhood (1-3 years): Walking, running, jumping, and climbing emerge. Fine motor skills like scribbling and stacking blocks develop. Children refine their sensory processing, showing more selective attention and increased ability to self-regulate.
- Preschool (3-5 years): More complex motor skills, like riding a tricycle and using scissors, develop. They demonstrate improved hand-eye coordination and increasingly sophisticated sensory discrimination.
- School-age (5-12 years): Motor skills become refined and specialized, supporting activities like writing, sports, and musical instruments. Sensory modulation improves, allowing children to filter out irrelevant sensory information and focus on tasks.
It’s important to note that individual children develop at different rates, and some variation is normal. However, significant delays or deviations from these milestones warrant professional evaluation.
Q 3. What are the common signs and symptoms of sensory processing disorder?
Sensory Processing Disorder (SPD) manifests differently in each child, but common signs include:
- Sensory Over-responsivity (Hypersensitivity): Extreme reactions to light, sound, touch, taste, or smell. For example, a child might scream at the sound of a vacuum cleaner or refuse to wear certain clothes due to texture.
- Sensory Under-responsivity (Hyposensitivity): Reduced response to sensory input. A child might not notice pain, bumps, or changes in temperature, or seem unaware of their body in space.
- Sensory Seeking/Craving: A constant need for sensory input, leading to behaviors like rocking, bumping into things, or seeking intense physical pressure.
- Sensory-Motor Difficulties: Problems with balance, coordination, posture, and fine motor skills like writing or buttoning clothes. This may manifest as clumsiness, poor handwriting, or difficulties with self-care.
- Difficulties with Self-Regulation: Challenges managing emotions and behavior, often related to sensory overload or under-stimulation.
It’s crucial to remember that these symptoms should be evaluated by a qualified professional to rule out other conditions and receive an accurate diagnosis.
Q 4. How would you assess a child’s sensory motor skills?
Assessing a child’s sensory motor skills requires a multi-faceted approach. It’s not just about observing their ability to catch a ball; it involves a comprehensive evaluation of their sensory processing and motor performance.
- Developmental History: A detailed history of milestones, medical conditions, and family history is essential.
- Observation: Observing the child’s spontaneous play and interactions in various environments is crucial. This allows me to see how they respond to different sensory stimuli.
- Standardized Assessments: Using standardized tests like the Sensory Profile or the Bruininks-Oseretsky Test of Motor Proficiency provides quantitative data on their sensory processing and motor abilities.
- Clinical Observation and Interviews: I’d use formal and informal assessments to observe how a child handles sensory input across different situations. This involves interviewing parents and teachers to gain a holistic understanding of a child’s challenges.
The goal is to identify strengths and weaknesses, and understand how their sensory processing impacts their motor skills and daily functioning. The assessment results inform intervention planning, tailoring strategies to the child’s specific needs.
Q 5. What are some evidence-based interventions for sensory processing difficulties?
Evidence-based interventions for sensory processing difficulties are tailored to the individual child’s needs and may include:
- Sensory Integration Therapy (SIT): A structured therapy approach that uses carefully selected sensory activities to improve sensory processing and motor skills. For example, swinging, using weighted blankets, or engaging in activities that promote proprioceptive input (awareness of body position).
- Occupational Therapy (OT): OTs use various techniques, including adaptive equipment and strategies, to help children improve their daily life skills.
- Behavioral Interventions: Strategies that target specific problem behaviors linked to sensory processing difficulties, often involving positive reinforcement and environmental modifications.
- Environmental Modifications: Adjusting the child’s environment to minimize sensory overload or under-stimulation. This might involve reducing noise levels in the classroom or providing a quiet space for breaks.
- Adaptive Equipment: Utilizing specialized tools and equipment to improve sensory motor performance, such as weighted vests or adapted utensils.
The key to success is a collaborative approach involving the child, family, therapists, educators, and other relevant professionals. Regular monitoring and adjustments to the intervention plan are crucial.
Q 6. Explain the difference between sensory modulation and sensory discrimination.
Sensory modulation and sensory discrimination are distinct but related aspects of sensory processing:
- Sensory Modulation: This refers to the ability to regulate the intensity and duration of responses to sensory input. It’s the neurological ‘volume control’ that helps us respond appropriately to our environment. A child with good sensory modulation can filter out distractions and focus on a task, while someone with poor modulation may be easily overwhelmed or under-stimulated.
- Sensory Discrimination: This is the ability to distinguish between different sensory stimuli. It’s about the quality, not the quantity, of sensory input. For example, discriminating between the feel of velvet and sandpaper, or identifying different musical notes. Poor sensory discrimination can lead to difficulties with tasks requiring fine motor control or distinguishing between similar objects.
Think of it like this: sensory modulation is about managing the *amount* of sensory input, while sensory discrimination is about understanding the *type* of sensory input. Both are crucial for successful daily functioning.
Q 7. Describe your experience with using adaptive equipment to improve sensory motor skills.
Throughout my career, I’ve extensively used adaptive equipment to support children with sensory-motor challenges. For instance, I worked with a child who had difficulty with handwriting due to poor grasp and limited fine motor control. We introduced adaptive writing tools like pencil grips and slant boards which significantly improved his writing posture and grip, leading to improved legibility and reduced fatigue.
Another example involved a child with difficulties with balance and coordination. Using a therapy ball during activities like reading and playing games improved his core strength and balance, allowing him to participate more actively in classroom activities and play. Weighted vests were also useful for children with sensory seeking behaviors, providing a calming and organizing effect. The selection and implementation of adaptive equipment always involves careful assessment to identify the specific needs of each child and is part of a broader, individualized therapy plan.
Q 8. How do you adapt therapeutic interventions to meet the specific needs of diverse learners?
Adapting therapeutic interventions for diverse learners is paramount. It involves understanding each child’s unique sensory profile, cognitive abilities, physical limitations, and learning styles. I begin by conducting a thorough assessment, considering their strengths and challenges across various sensory systems (visual, auditory, tactile, vestibular, proprioceptive). This includes observing their responses in different environments and activities, using standardized assessments like the Sensory Profile or the Bruininks-Oseretsky Test of Motor Proficiency (BOT-2), and gathering information from parents and caregivers.
For example, a child with autism and significant auditory sensitivities might benefit from a quiet workspace with noise-canceling headphones during therapy sessions, while a child with Down syndrome might require more physical support and adapted activities to promote motor skill development. I then tailor the interventions – choosing activities, modifying materials, adjusting the pace and intensity – to ensure optimal engagement and progress. This might include adapting the size and weight of objects, using visual supports, breaking down complex tasks into smaller steps, providing positive reinforcement, and integrating play-based learning. Ultimately, the goal is to create a supportive and stimulating environment that fosters the child’s self-confidence and maximizes their learning potential.
Q 9. What is your experience with creating and implementing sensory diets?
Creating and implementing sensory diets is a significant part of my practice. A sensory diet is not a diet in the traditional sense, but rather a personalized plan of sensory activities designed to help regulate a child’s sensory system and improve their ability to focus, self-regulate, and participate in daily activities. I work collaboratively with parents and the child to create a diet tailored to their individual needs. This involves a careful assessment to identify sensory sensitivities and preferences. For instance, a child who struggles with tactile defensiveness might benefit from activities involving deep pressure touch, such as weighted blankets or firm hugs, while a child with vestibular issues might need more opportunities for movement and spinning.
The diet is not static; it evolves over time as the child’s needs change and they progress. I often include a range of activities, like brushing activities (to calm the tactile system), swinging or rocking (vestibular input), and heavy work activities (proprioceptive input) throughout their day. The key is to help the child develop strategies for self-regulation, empowering them to choose and implement appropriate sensory activities to manage their sensory experiences and improve their overall functioning.
Q 10. Describe your approach to collaborating with parents and caregivers.
Collaboration with parents and caregivers is essential for successful sensory motor interventions. I view parents as partners in the therapeutic process. I begin by establishing open communication, actively listening to their concerns and observations, and explaining the child’s sensory needs in a clear and understandable manner. Regular meetings and updates, either in person or via phone/email, are crucial.
I involve parents in the assessment process, sharing observations and discussing potential strategies. I also provide them with tools and strategies they can utilize at home, demonstrating activities and explaining the rationale behind them. This might involve suggesting specific toys or sensory activities for home use, or coaching them on how to modify the child’s environment to better support their sensory needs. This collaborative approach not only ensures consistency but also empowers parents to be active participants in their child’s development, improving their confidence and competence in supporting their child at home.
Q 11. How do you measure the effectiveness of your sensory motor interventions?
Measuring the effectiveness of sensory motor interventions involves a multifaceted approach. I use a combination of objective and subjective measures. Objective measures might include standardized assessments such as the BOT-2, which quantifies motor skills, or the Sensory Profile, which assesses sensory processing. I also observe the child’s performance during therapy sessions, noting improvements in motor skills, self-regulation, and participation in activities.
Subjective measures include feedback from parents and caregivers, documenting changes in the child’s behavior and daily functioning at home and school. I regularly track progress using graphs and charts, highlighting changes in specific skills over time. Furthermore, I use qualitative data, like anecdotal records and video recordings, to capture the nuances of the child’s progress and identify areas where adjustments to the intervention plan are needed. This holistic approach allows for a comprehensive understanding of the intervention’s effectiveness and enables me to adapt and refine the therapy plan as needed.
Q 12. Explain the role of proprioception in motor skill development.
Proprioception, often described as the ‘sixth sense’, is the body’s awareness of its position and movement in space. It’s crucial for motor skill development because it provides the brain with constant feedback about where our limbs are, how much force to apply, and how to coordinate movements smoothly. Think of it as the body’s internal GPS.
For example, when learning to write, proprioception enables the child to know where their hand and fingers are in relation to the paper, allowing for precise pencil control. Weakness in proprioception can lead to clumsiness, poor posture, difficulty with fine motor tasks, and challenges with balance. Activities promoting proprioception include heavy work activities like carrying heavy objects, pushing or pulling resistance, crawling, climbing, and activities involving resistance bands or weighted vests. These activities stimulate the sensory receptors in muscles, joints, and tendons, enhancing body awareness and improving motor control.
Q 13. How would you address a child’s difficulty with tactile defensiveness?
Tactile defensiveness is an over-reactive response to touch, often manifesting as avoidance, anxiety, or even aggression when touched. Addressing this requires a gradual and systematic approach. I start by creating a safe and predictable environment. The first step involves building trust and rapport with the child.
I use a ‘just-right’ challenge approach, introducing tactile input gradually, starting with light touch and progressing to more intense stimulation only when the child is comfortable. This might involve brushing activities with soft-bristled brushes, starting on the child’s extremities and slowly moving towards the torso. I use activities involving different textures, allowing the child to explore and choose the textures that they find tolerable. Deep pressure activities, such as weighted blankets or firm hugs, are often helpful, as they can provide a calming and organizing effect on the nervous system. Positive reinforcement and celebrating successes are vital throughout the process. It’s crucial to avoid forcing the child, respecting their limits and celebrating small victories to build confidence and desensitize them over time.
Q 14. Describe your experience with vestibular interventions.
Vestibular interventions focus on improving the function of the vestibular system, which governs balance and spatial orientation. I often incorporate activities that provide vestibular input, like spinning, swinging, and rocking. The intensity and duration of these activities are carefully controlled, and they are adjusted based on the child’s tolerance and responses. For example, slow, rhythmic rocking can be calming, while faster spinning might be stimulating.
I also utilize activities that challenge the child’s balance, such as walking on uneven surfaces, balancing on beams, and playing games that require dynamic balance. The goal is not just to improve balance but also to enhance spatial awareness, coordination, and overall motor planning. I might also use specialized equipment such as a therapy ball or a swing to provide controlled vestibular input. The selection of activities depends heavily on the child’s specific needs and challenges, with a focus on gradual adaptation and individualized approach.
Q 15. Explain the relationship between sensory processing and social-emotional development.
Sensory processing and social-emotional development are intricately intertwined. Effective sensory processing is the foundation upon which social-emotional skills are built. Think of it like this: if a child is constantly overwhelmed or understimulated by sensory input (light, sound, touch, etc.), their ability to focus on social cues, regulate emotions, and engage in social interactions will be significantly impacted.
For example, a child hypersensitive to touch might avoid physical interactions like hugs or handshakes, leading to social isolation. Conversely, a child who seeks intense sensory input might be overly boisterous and disruptive in social settings, hindering their ability to form positive relationships. Proper sensory regulation allows children to attend to their environment, process information accurately, and respond appropriately in social situations. This leads to improved self-awareness, emotional control, and the ability to empathize with others.
- Improved Attention: When sensory needs are met, children can better focus on social interactions and instructions.
- Emotional Regulation: Sensory activities help children develop coping mechanisms for stress and emotional regulation.
- Social Interaction Skills: Successful sensory processing facilitates participation in group activities and social play.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you incorporate play therapy techniques into your sensory motor interventions?
Play therapy is an invaluable tool in sensory motor interventions. It allows children to engage with therapeutic concepts in a natural, engaging way, reducing anxiety and resistance often associated with traditional therapy. We use play to address sensory challenges indirectly, making the process fun and motivating.
For instance, a child struggling with tactile defensiveness might participate in a play session involving sand, playdough, or water play. These activities gradually desensitize the child to touch, while simultaneously fostering creativity and social interaction. Other examples include using weighted blankets during quiet play to improve proprioceptive input (body awareness), incorporating obstacle courses for vestibular input (balance and movement), or engaging in imaginative play with props to address sensory integration challenges. We tailor the play activities specifically to the child’s sensory profile and therapeutic goals.
The key is to subtly introduce sensory challenges within a playful context, constantly monitoring the child’s response and adjusting the intensity and type of stimulation as needed. The therapist observes and guides the play, addressing sensory issues while building the child’s confidence and self-esteem.
Q 17. What are the ethical considerations when working with children with sensory processing challenges?
Ethical considerations in working with children with sensory processing challenges are paramount. Our primary responsibility is to ensure the child’s safety, well-being, and respect. This encompasses several key areas:
- Informed Consent: Obtaining informed consent from parents or guardians about all assessment and intervention procedures is crucial. This includes explaining the process, potential benefits and risks, and ensuring they understand their rights.
- Confidentiality: Maintaining the confidentiality of the child’s information is vital, sharing only necessary information with relevant professionals and with the explicit consent of the parents/guardians.
- Cultural Sensitivity: Recognizing and respecting the child’s cultural background and family values are essential in creating a comfortable and effective therapeutic environment. Interventions must be culturally appropriate.
- Avoidance of Harm: Sensory activities must be carefully planned and implemented to prevent injury or further sensory distress. Regular assessment of the child’s comfort level is necessary. If a child is showing signs of distress, the activity needs to be stopped immediately.
- Competence: Therapists need to ensure they have the appropriate training and skills to effectively assess and treat children with sensory processing challenges. Referring cases to other specialists when necessary is also ethically crucial.
Q 18. What are some common challenges you’ve encountered while working in this field?
Some common challenges include:
- Diagnosing SPD: Sensory Processing Disorder (SPD) can be difficult to diagnose definitively, as its symptoms often overlap with other developmental delays. This requires careful observation and assessment, often involving multiple professionals.
- Parental Understanding and Engagement: Securing parental understanding and active participation in the intervention plan is essential for success, but can be challenging if parents are not fully informed or are hesitant to engage.
- Resource Limitations: Accessing appropriate resources, such as specialized equipment or skilled therapists, can be limited depending on geographical location and funding. This creates barriers to providing adequate care.
- Individualized Approaches: Each child’s sensory profile is unique, requiring highly individualized interventions. Creating and implementing these tailored programs can be time-consuming and require creativity.
- Measuring Progress: Measuring the effectiveness of interventions can be complex. While observable changes are often seen, it can be challenging to quantify the improvement objectively.
Q 19. Describe your experience using various assessment tools for sensory motor skills.
My experience with assessment tools is extensive. I routinely utilize both standardized tests and observational measures. Standardized tools like the Sensory Profile, Sensory Integration and Praxis Test (SIPT), and the Bruininks-Oseretsky Test of Motor Proficiency (BOT-2) provide quantitative data on specific sensory processing abilities. These tests help identify strengths and weaknesses across various sensory systems. However, these tests only paint part of the picture.
Equally important are observational measures, where I directly observe the child’s behavior in various settings. This involves assessing their response to different sensory stimuli, their ability to self-regulate, and their overall participation in activities. The combination of standardized testing and observational data allows for a holistic evaluation of the child’s sensory motor skills and provides a more comprehensive picture. I also incorporate parent interviews and questionnaires to gather additional information on the child’s sensory behaviors at home.
Q 20. How do you differentiate between sensory processing disorder and other developmental delays?
Differentiating between Sensory Processing Disorder (SPD) and other developmental delays requires a careful and comprehensive assessment. SPD is characterized by challenges in the way the nervous system receives, processes, and organizes sensory information from the body and the environment. This leads to difficulties with motor coordination, attention, behavior, and social interaction.
Other developmental delays, such as autism spectrum disorder (ASD), intellectual disability, or ADHD, can present with overlapping symptoms. For instance, both SPD and ASD can manifest as social difficulties or sensory sensitivities. However, the core issue in SPD is the sensory processing itself, while ASD involves broader impairments in social communication and repetitive behaviors. A thorough evaluation by a multidisciplinary team involving occupational therapists, psychologists, and other specialists is necessary to distinguish between these conditions. The key is to look at the overall pattern of symptoms and the child’s developmental trajectory to arrive at a comprehensive diagnosis.
Q 21. Explain your understanding of the impact of sensory processing on academic performance.
Sensory processing significantly impacts academic performance. Children with unresolved sensory challenges often struggle with attention, focus, and self-regulation, making it difficult to succeed in the classroom. For example, a child hypersensitive to auditory input might be easily distracted by classroom noise, leading to difficulties in concentrating on lessons. A child with poor proprioceptive awareness might have difficulty with handwriting, fine motor skills needed for writing, or maintaining appropriate posture during classroom activities. Similarly, a child with vestibular challenges (balance and movement) might struggle with physical activities such as participating in physical education or even walking across the classroom without bumping into things.
These difficulties can lead to academic frustration, decreased self-esteem, and behavioral problems. Addressing sensory processing issues through appropriate interventions can significantly improve a child’s ability to focus, participate in class, and ultimately, achieve academic success. In my work, I frequently collaborate with educators to develop classroom strategies and modifications tailored to a child’s individual sensory needs, fostering a more supportive and inclusive learning environment.
Q 22. What are some strategies to improve sensory motor skills in children with autism spectrum disorder?
Improving sensory motor skills in children with autism spectrum disorder (ASD) requires a multifaceted approach tailored to the individual’s needs. Many children with ASD experience sensory sensitivities or differences, impacting their ability to process and respond to sensory information. This can manifest as hypersensitivity (over-reaction) or hyposensitivity (under-reaction) to touch, sound, light, taste, smell, movement, or even body awareness (proprioception).
Sensory Integration Activities: These activities aim to regulate the nervous system. Examples include weighted blankets for calming, heavy work activities like pushing or pulling heavy objects to improve body awareness, and activities involving varied textures to improve tactile processing. We might use a therapy ball for vestibular input (balance) or a swing to provide proprioceptive and vestibular input simultaneously.
Structured Play: Creating predictable and structured play environments helps reduce anxiety and allows children to focus on motor skills. This could involve building towers with blocks (fine motor), playing with large balls to improve gross motor skills, or engaging in activities like obstacle courses to combine multiple skill sets.
Adaptive Physical Activity: Activities like swimming, cycling or even dance, adapted to the child’s abilities, can be incredibly beneficial. The rhythmic nature and varied sensory input are often very calming and promote coordination.
Visual Supports: Using visual schedules and timers can help children with ASD understand expectations and transitions, reducing anxiety and increasing engagement. This is especially useful for children with challenges processing verbal instructions.
Occupational Therapy: This involves working closely with an occupational therapist to assess specific sensory needs and create a personalized intervention plan. They might employ techniques like sensory diets (regularly scheduled sensory activities throughout the day to regulate the child’s sensory system).
Q 23. How would you address the challenges of working with a child who has limited communication skills?
Working with a child with limited communication skills requires patience, creativity, and a deep understanding of nonverbal communication. It’s crucial to remember that communication isn’t solely verbal; it encompasses all forms of expression.
Observation: I would closely observe the child’s body language, facial expressions, and vocalizations to understand their needs and preferences. A subtle shift in posture, a change in breathing, or a particular sound could indicate discomfort or engagement.
Alternative Communication Methods: I would utilize augmentative and alternative communication (AAC) methods such as picture exchange systems (PECS), sign language, or communication apps. This allows the child to express themselves, reducing frustration.
Nonverbal Cues: I’d use clear nonverbal cues during activities, such as demonstrating the action first, using visual aids (pictures or gestures), and providing ample opportunities for physical interaction.
Building Trust: Establishing a strong, trusting relationship is paramount. This takes time and requires consistently demonstrating sensitivity and patience. Positive reinforcement and a calm, predictable environment are crucial.
For example, if a child is struggling to express their needs during a sensory activity, I might present them with a choice of two options (e.g., a soft ball or a firm ball) using pictures and allow them to point to their preference. This empowers them to participate and communicate in a way that is accessible to them.
Q 24. Describe your knowledge of different types of sensory integration therapy approaches.
Sensory integration therapy aims to improve the way the brain processes and organizes sensory information. There are various approaches, each tailored to specific needs:
Wilbarger Brushing Protocol: This involves using a specific brush with a particular technique to stimulate proprioceptive input (body awareness) and reduce tactile defensiveness. It’s often used for children with strong sensory sensitivities.
Ayres Sensory Integration (ASI): This is a well-established approach that focuses on providing specific sensory experiences to challenge the child’s sensory systems and promote adaptive responses. ASI uses playful activities to improve sensory processing and motor planning.
Sensory Diet: A sensory diet is a personalized plan of sensory activities that helps to regulate a child’s sensory system throughout the day. This isn’t a diet in the traditional sense but rather a series of planned sensory experiences that address specific sensory needs. It could include activities like weighted blankets, rocking, chewing on chewy tubes, or deep pressure touch.
The specific approach will depend on the child’s unique sensory profile and the goals of therapy. A thorough assessment is essential to determine the most appropriate and effective strategy.
Q 25. How do you ensure the safety of a child during sensory motor activities?
Safety is paramount in any sensory motor activity. Several strategies ensure a safe and positive experience:
Risk Assessment: Before any activity, I conduct a thorough risk assessment considering the child’s developmental stage, sensory profile, and potential hazards. This involves identifying potential risks and implementing precautions.
Appropriate Supervision: Activities are always supervised by trained professionals, ensuring close monitoring and immediate intervention if necessary. The level of supervision is adjusted to the child’s needs and the activity’s complexity.
Adaptive Equipment: When needed, adaptive equipment such as soft mats, padded surfaces, and appropriately sized apparatus are used to minimize the risk of injury.
Clear Instructions and Demonstrations: Instructions are given clearly and concisely, often supported by visual aids or demonstrations. This minimizes confusion and potential accidents.
Gradual Introduction: New activities are introduced gradually, starting with simpler movements and progressing to more complex ones as the child’s comfort and skills develop.
Emergency Preparedness: I am familiar with first aid procedures and have access to necessary emergency equipment. A clear emergency plan is in place.
Q 26. How do you incorporate family involvement into treatment plans?
Family involvement is crucial for successful sensory motor skill development. Parents and caregivers are the primary caregivers and can significantly influence the child’s progress outside therapy sessions.
Collaboration: I work closely with families, ensuring that the treatment plan aligns with their expectations and resources. This includes regular communication updates and shared decision-making.
Education and Training: I provide families with education and training on sensory processing, strategies for managing sensory sensitivities, and techniques to implement at home. This could involve demonstrations of specific activities or provision of written resources.
Home Programs: I collaboratively develop home programs consisting of fun and engaging activities that complement the therapy sessions. These programs are carefully designed to be feasible within the family’s daily routine.
Ongoing Support: I provide ongoing support to families, addressing their concerns, offering guidance, and making adjustments to the treatment plan as needed. This may involve regular check-in calls or emails.
For example, I might work with a family to create a visual schedule for sensory activities throughout the day, incorporating calming activities like weighted blanket time before bedtime and heavy work activities such as pushing a shopping cart during grocery runs. This helps integrate the therapeutic strategies into the family’s daily life.
Q 27. What is your approach to ongoing professional development in this area?
Ongoing professional development is essential to stay updated with the latest research, best practices, and advancements in sensory motor skill development. My approach involves a multi-pronged strategy:
Continuing Education Courses: I regularly attend workshops, seminars, and conferences related to sensory integration, autism spectrum disorder, and child development. This keeps me abreast of new techniques and interventions.
Professional Organizations: I actively participate in professional organizations, such as the American Occupational Therapy Association (AOTA), to network with peers and access resources.
Peer Supervision and Consultation: I engage in regular peer supervision and consultation with other professionals in the field to discuss cases and refine my practice.
Journal Articles and Research: I regularly review professional journals and research articles to stay updated on the latest scientific evidence and advancements in the field.
Mentorship: I seek out mentorship opportunities from experienced professionals, providing invaluable guidance and insights into complex cases.
Q 28. How would you modify activities to accommodate children with different levels of ability?
Modifying activities to accommodate children with different abilities is crucial for maximizing participation and engagement. This requires careful observation, flexibility, and creativity.
Adapting Difficulty: I adjust the difficulty of activities based on the child’s skill level. This could involve simplifying complex movements, providing extra support, or breaking down tasks into smaller, more manageable steps.
Assistive Technology: I use assistive technology such as adaptive equipment or specialized tools whenever needed. This could include using weighted vests, adapted toys, or specialized seating to enhance participation.
Environmental Modifications: I modify the environment to enhance safety and accessibility. This might involve adjusting lighting, reducing noise levels, or providing quiet spaces for breaks.
Differentiated Instruction: I utilize differentiated instruction, providing different levels of support and challenge based on individual needs. Some children may require more one-on-one support, while others might benefit from group activities.
Positive Reinforcement: I consistently use positive reinforcement to encourage participation and motivate the child. Celebrating small successes is crucial to build confidence and maintain motivation.
For example, if a child struggles with fine motor skills during a block-building activity, I might start with larger blocks, provide hand-over-hand assistance, or allow them to use a different medium, like playdough, to achieve the same developmental goals.
Key Topics to Learn for Sensory Motor Skills Development Interview
- Neurological Foundations: Understanding the brain’s role in sensory processing and motor control, including key neural pathways and developmental milestones.
- Sensory Integration: Exploring how different sensory systems (visual, auditory, tactile, vestibular, proprioceptive) interact and influence motor planning and execution. Practical application: Analyzing a child’s challenges in handwriting based on their sensory processing profile.
- Motor Skill Acquisition: Examining the stages of motor development, from reflexes to complex movements, and the factors that influence skill learning. Practical application: Designing an intervention program to improve gross motor skills in children with developmental delays.
- Assessment and Evaluation: Familiarizing yourself with various assessment tools and methods used to evaluate sensory motor skills, including standardized tests and observational techniques. Practical application: Interpreting the results of a sensory profile assessment and formulating appropriate recommendations.
- Intervention Strategies: Learning about different therapeutic approaches and interventions used to address sensory motor challenges, such as occupational therapy techniques, adaptive equipment, and sensory integration activities. Practical application: Developing a personalized intervention plan for a child with autism spectrum disorder exhibiting sensory sensitivities.
- Adaptive and Assistive Technology: Understanding the role of technology in supporting sensory motor development, including examples of adaptive equipment and assistive technologies. Practical application: Evaluating the effectiveness of a specific piece of assistive technology for an individual with cerebral palsy.
- Research and Evidence-Based Practice: Staying current with the latest research in sensory motor development and applying evidence-based practices in your work. Practical application: Critically evaluating research articles on the effectiveness of a particular intervention technique.
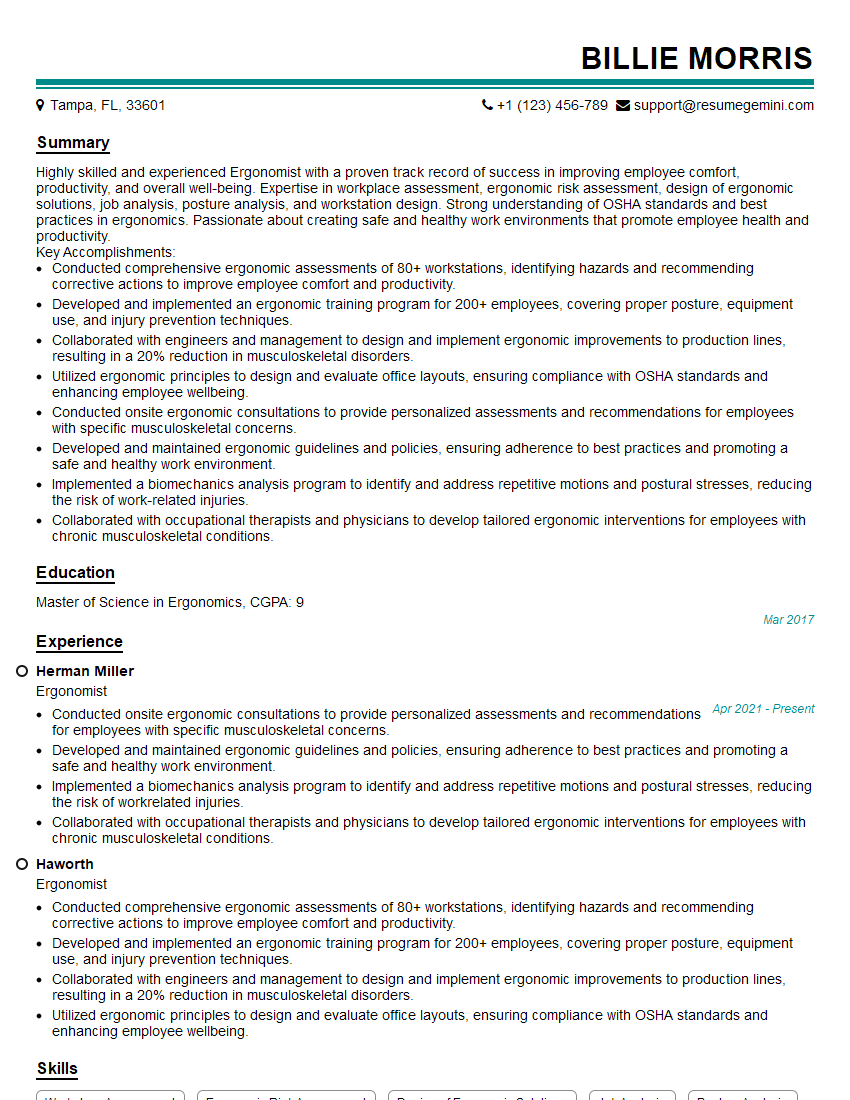
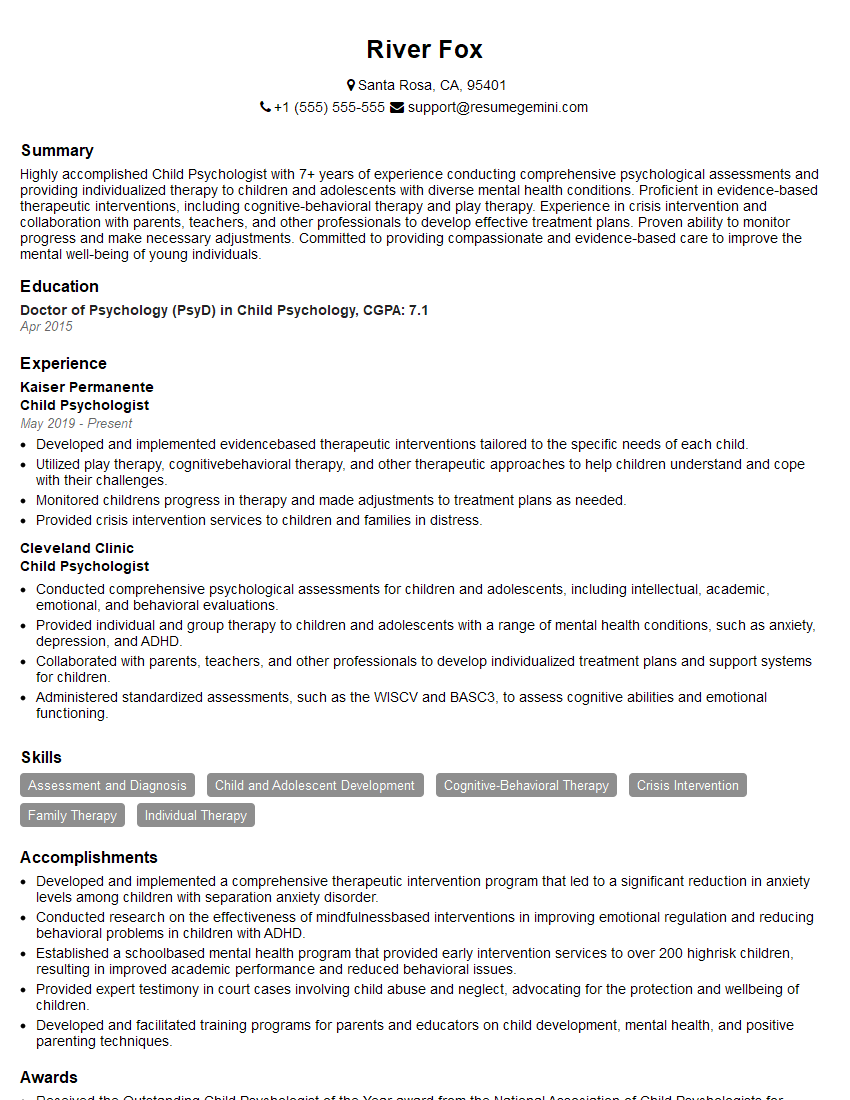
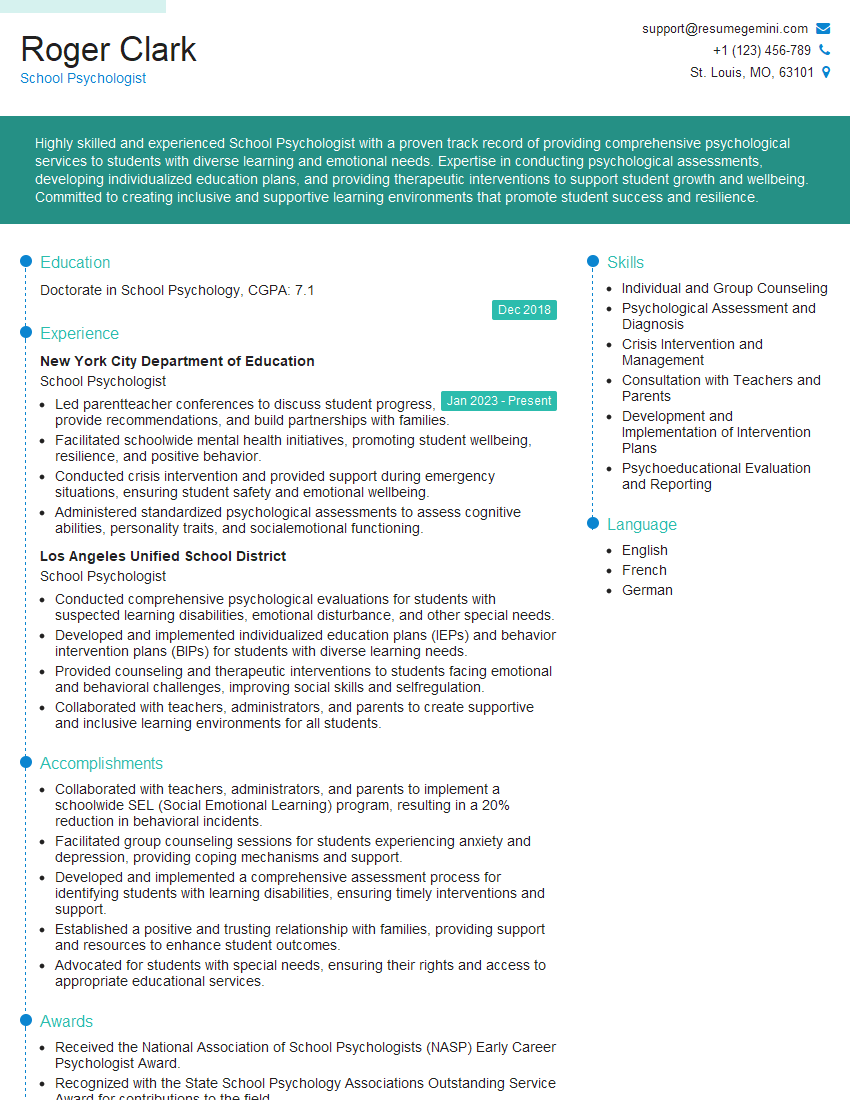
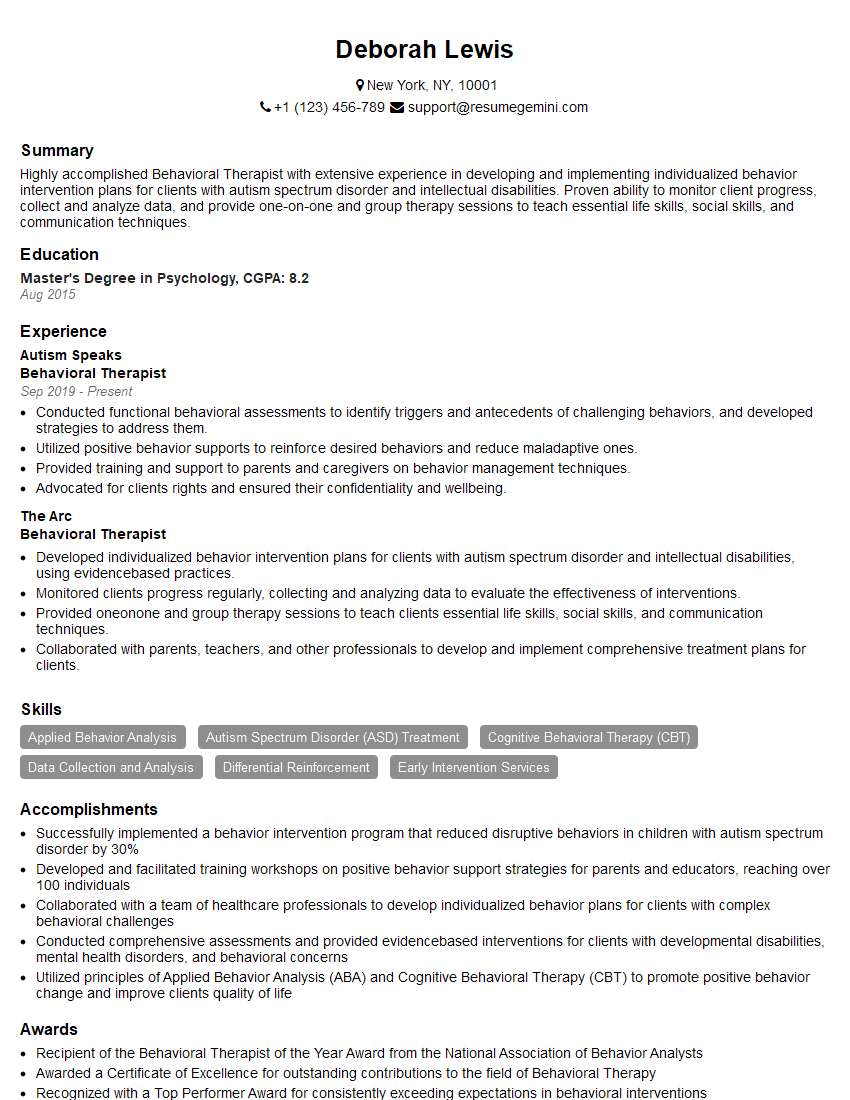
Next Steps
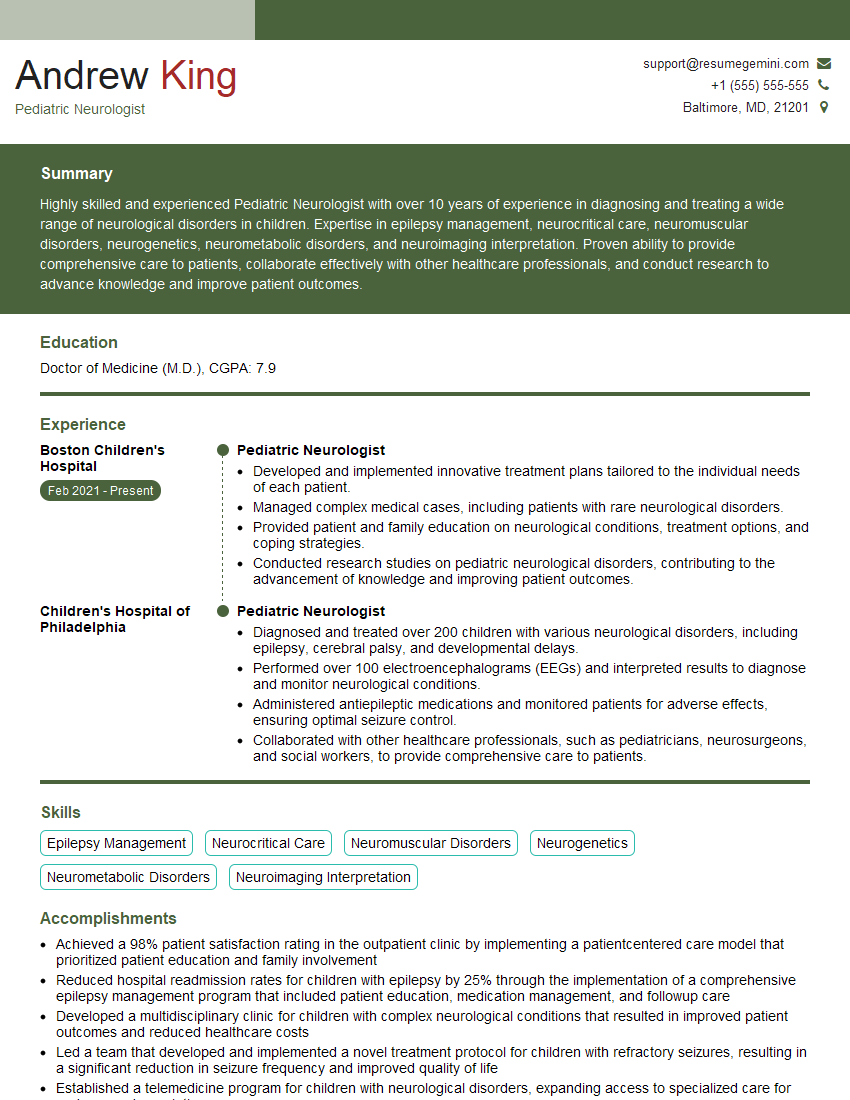
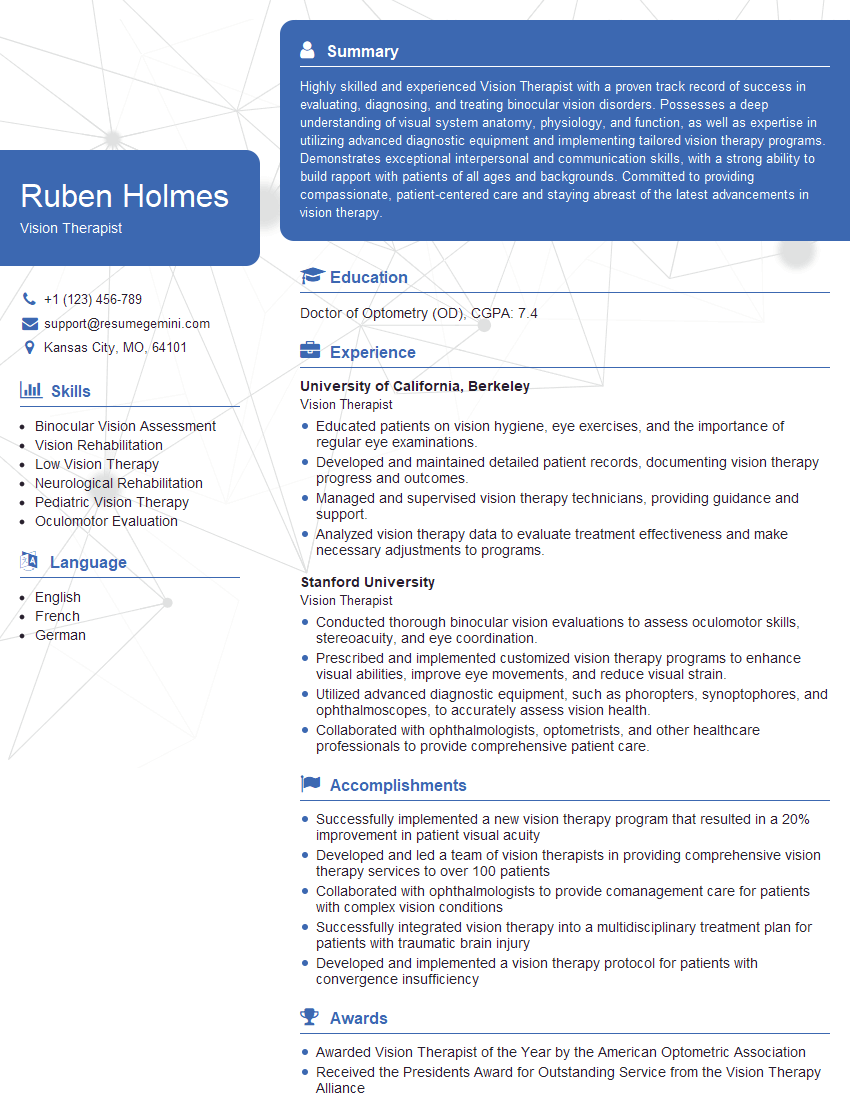
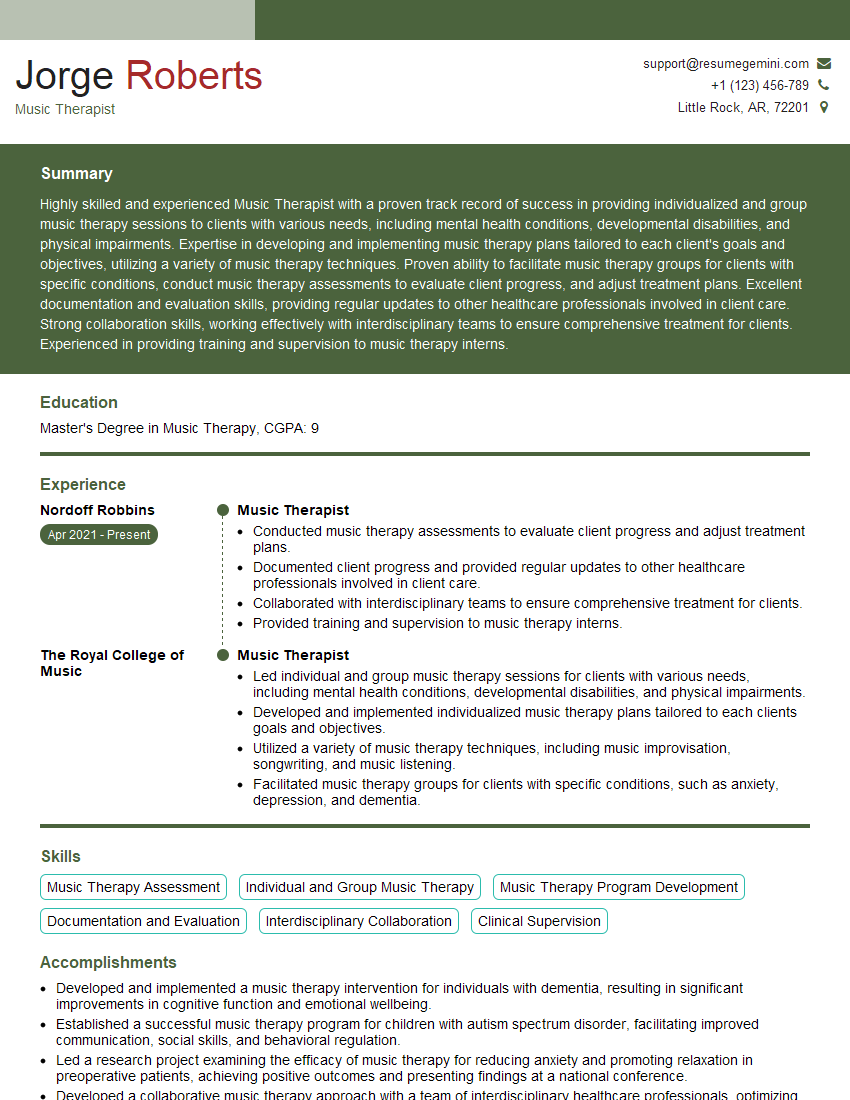
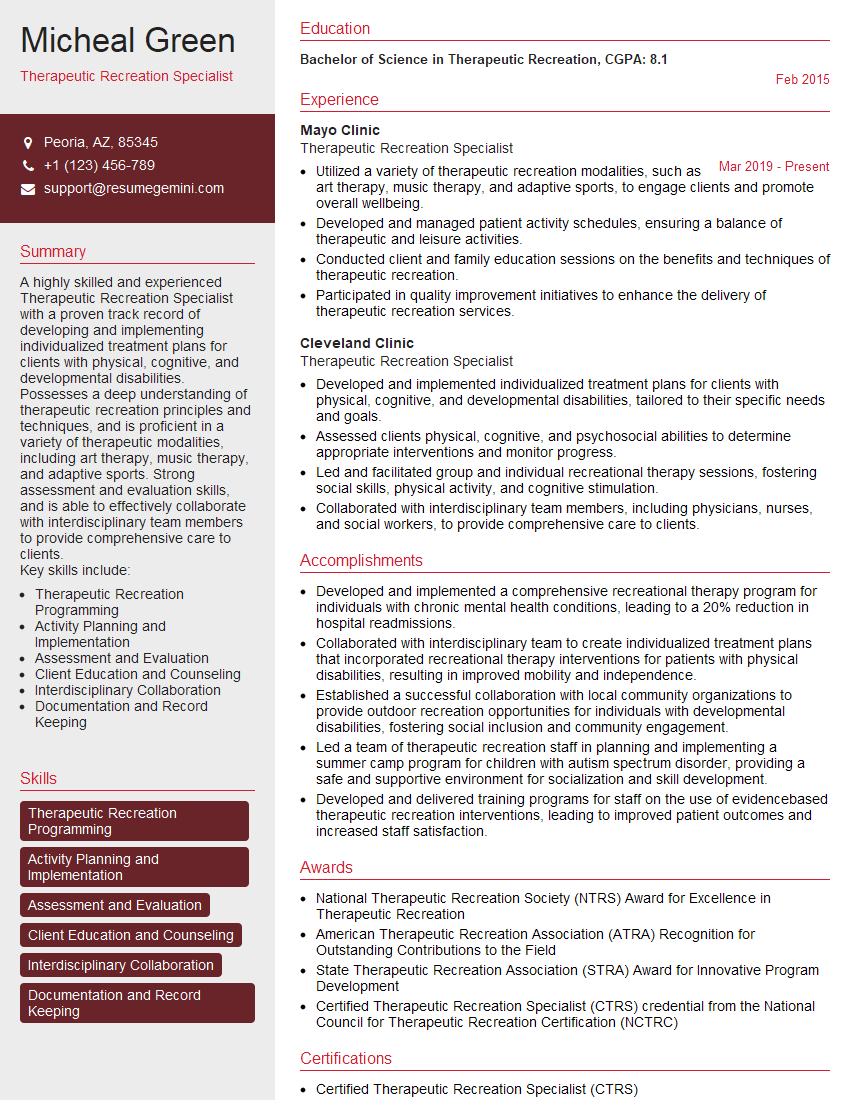
Mastering Sensory Motor Skills Development opens doors to rewarding careers in various fields, including occupational therapy, physical therapy, and special education. To maximize your job prospects, it’s crucial to present your skills effectively. Creating an ATS-friendly resume is key to getting your application noticed. We highly recommend using ResumeGemini to build a professional and impactful resume that highlights your expertise. ResumeGemini provides examples of resumes tailored to Sensory Motor Skills Development, allowing you to showcase your qualifications in the best possible light. Invest time in crafting a compelling resume – it’s your first impression on potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO