Cracking a skill-specific interview, like one for Substance Abuse Awareness, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Substance Abuse Awareness Interview
Q 1. Explain the stages of substance use disorder.
Substance Use Disorder (SUD) isn’t a single event but a progressive process often characterized by several stages. While the progression isn’t always linear, and individuals may experience different trajectories, a common framework includes:
- Experimentation: Initial use, often driven by curiosity or social pressure. The individual may not experience significant consequences at this stage.
- Regular Use: Substance use becomes more frequent, shifting from occasional to habitual. The individual might start experiencing mild withdrawal symptoms when they abstain.
- Abuse: Substance use continues despite negative consequences impacting work, relationships, or health. The individual displays a clear pattern of impaired control.
- Dependence/Addiction: This is characterized by tolerance (needing more substance for the same effect) and withdrawal (experiencing unpleasant physical and psychological symptoms when stopping). The individual’s life revolves around obtaining and using the substance. This stage involves significant impairment in various life domains.
Think of it like a slippery slope: Experimentation is like taking the first step towards the edge, regular use is walking closer, abuse is nearing the brink, and dependence is falling over the edge. Early intervention is crucial to prevent progression to more severe stages.
Q 2. Describe different types of substance abuse treatment modalities (e.g., CBT, motivational interviewing, medication-assisted treatment).
Treatment for SUD is highly individualized and often involves a combination of modalities. Some key approaches include:
- Cognitive Behavioral Therapy (CBT): This helps individuals identify and change negative thought patterns and behaviors that contribute to substance use. For example, CBT can teach coping mechanisms to manage cravings and triggers.
- Motivational Interviewing (MI): This client-centered approach focuses on exploring and resolving ambivalence towards change. The therapist helps the individual clarify their goals and develop intrinsic motivation for recovery.
- Medication-Assisted Treatment (MAT): This uses medications to manage withdrawal symptoms, reduce cravings, and prevent relapse. Methadone, buprenorphine, and naltrexone are examples of medications used in MAT for opioid use disorder.
- 12-Step Programs: These peer-support groups, like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA), offer a community-based approach focusing on spiritual growth and mutual support.
It’s essential to remember that a combination of approaches is often most effective. For instance, a client might benefit from CBT to address underlying psychological issues while using MAT to manage physical withdrawal symptoms and cravings.
Q 3. What are the common co-occurring disorders associated with substance abuse?
Co-occurring disorders, also known as dual diagnoses, are common among individuals with SUD. These are mental health conditions that exist alongside a substance use disorder. Some frequent examples include:
- Depression and Anxiety: Substance use can be a way to self-medicate these conditions, creating a vicious cycle.
- Post-Traumatic Stress Disorder (PTSD): Trauma can significantly increase the risk of substance abuse as a coping mechanism.
- Personality Disorders: Certain personality traits can predispose individuals to substance abuse.
- Bipolar Disorder: The mood swings associated with bipolar disorder can be managed poorly through substance use.
Addressing both the SUD and the co-occurring disorder simultaneously is critical for successful treatment. Treating one without addressing the other often results in relapse.
Q 4. How would you assess a client’s risk for relapse?
Assessing relapse risk involves a comprehensive approach that considers various factors. I would use a combination of methods, including:
- Client History: Past attempts at treatment, duration of substance use, severity of dependence, and previous relapses are important indicators.
- Social Support System: The strength and quality of the client’s support network significantly impacts relapse risk. Lack of support increases the risk.
- Lifestyle Factors: Stress levels, exposure to triggers (people, places, things associated with past substance use), and coping mechanisms are assessed. High stress and poor coping skills increase vulnerability.
- Psychological Factors: Mental health conditions, motivation for change, and coping mechanisms significantly influence relapse likelihood.
- Use of Relapse Prevention Planning: This involves the client actively identifying high-risk situations and creating strategies to manage them. This is a proactive measure that reduces the probability of relapse.
A thorough assessment allows for the development of a tailored treatment plan that proactively addresses identified risk factors, emphasizing relapse prevention strategies.
Q 5. What are the ethical considerations when working with individuals with substance use disorders?
Ethical considerations in working with individuals with SUD are paramount. Key ethical principles include:
- Confidentiality: Protecting client information is crucial, adhering to HIPAA regulations and maintaining professional boundaries.
- Informed Consent: Clients need to fully understand the treatment plan, its risks and benefits, before consenting to participation. This includes respecting their autonomy and right to refuse treatment.
- Competence: Practitioners should only provide services within their scope of expertise and stay updated with the latest evidence-based practices.
- Non-Discrimination: Providing equal access to care, regardless of race, ethnicity, gender, sexual orientation, or socioeconomic status.
- Avoiding Dual Relationships: Maintaining professional boundaries and avoiding situations that could create conflicts of interest.
Ethical practice builds trust and fosters a therapeutic alliance, essential for successful recovery.
Q 6. Describe your experience with crisis intervention in the context of substance abuse.
My experience with crisis intervention in the context of substance abuse has involved situations ranging from acute intoxication to suicidal ideation linked to substance withdrawal. I’ve utilized a combination of techniques, including:
- Immediate Safety Assessment: Prioritizing the client’s safety and ensuring they are in a safe environment, potentially involving emergency services if necessary.
- De-escalation Techniques: Using calm and empathetic communication to reduce the client’s anxiety and agitation.
- Collaboration with Emergency Services: Coordinating with paramedics, hospitals, or mental health crisis teams when appropriate.
- Brief Intervention Strategies: Providing immediate support and connecting the individual to resources like detoxification facilities or crisis hotlines.
One example involved a client experiencing severe alcohol withdrawal. Immediate medical attention was necessary to prevent seizures. Following stabilization, I connected the client to a detox facility and assisted in creating a short-term safety plan for discharge.
Q 7. How would you handle a client who is resisting treatment?
Handling a client resisting treatment requires patience, empathy, and a collaborative approach. Instead of forcing treatment, I would focus on:
- Understanding Resistance: Exploring the reasons behind their resistance. This might involve fear, shame, lack of understanding, or past negative experiences with treatment.
- Motivational Interviewing Techniques: Using MI principles to help the client explore their ambivalence and develop their own reasons for change.
- Collaborative Goal Setting: Involving the client in setting realistic and achievable treatment goals, making them feel empowered in the process.
- Offering Alternatives: Exploring various treatment options that might better suit the client’s needs and preferences.
- Maintaining Hope and Support: Reinforcing that recovery is a journey, not a destination, and that setbacks are a normal part of the process.
It’s important to remember that it’s ultimately the client’s decision. My role is to support their autonomy while providing information and guidance to empower them to make informed choices about their recovery.
Q 8. Explain the concept of harm reduction.
Harm reduction is a set of practical strategies and ideas aimed at minimizing the negative consequences associated with drug use. It’s not about abstinence, but rather reducing the harms caused by drug use itself, whether that’s to the individual, their family, or the community. It acknowledges that some individuals may not be ready or able to stop using drugs completely, and instead focuses on helping them manage their use more safely.
Examples of harm reduction strategies include:
- Needle exchange programs: Providing clean needles to prevent the spread of infectious diseases like HIV and Hepatitis C.
- Naloxone distribution: Making the opioid overdose reversal medication naloxone widely available to first responders, family members, and people who use drugs.
- Supervised consumption sites: Providing a safe, medically supervised environment for people to use drugs, reducing the risk of overdose and providing access to healthcare and support services.
- Methadone and buprenorphine treatment: Offering medication-assisted treatment (MAT) to manage opioid dependence.
Imagine a person struggling with heroin addiction. Instead of focusing solely on immediate abstinence (which can be incredibly challenging), a harm reduction approach might prioritize getting them access to clean needles, naloxone, and perhaps MAT. This reduces the risk of overdose, infection, and other health problems, while simultaneously working toward eventual abstinence if and when the person is ready.
Q 9. What are some evidence-based practices for preventing substance abuse?
Evidence-based prevention strategies for substance abuse are multifaceted and target various risk factors. They include:
- Education: School-based programs teaching about the risks of substance use, refusal skills, and healthy coping mechanisms. This might include interactive workshops, role-playing scenarios, and engaging media campaigns.
- Family-based interventions: Programs that strengthen family communication, bonding, and parental monitoring to reduce risk factors associated with substance abuse in adolescents and young adults.
- Community-based prevention: Initiatives aimed at reducing the availability of drugs, promoting positive community norms around substance use, and improving access to treatment and support services.
- Early intervention: Identifying individuals at high risk of developing substance use disorders and providing them with timely support and interventions. This might involve screening tools, early identification programs, and referral to appropriate resources.
- Media campaigns: Public health campaigns targeting specific populations to raise awareness about the risks of substance abuse and promote healthy behaviors. These often utilize creative visuals and impactful messaging.
For example, a school might implement a comprehensive drug prevention program incorporating educational workshops, parent training sessions, and community outreach events, creating a layered approach to reduce substance abuse among students.
Q 10. How do you ensure client confidentiality and HIPAA compliance?
Client confidentiality and HIPAA compliance are paramount in substance abuse treatment. I adhere strictly to all HIPAA regulations and maintain the strictest confidentiality. This involves several key steps:
- Secure record-keeping: All client information is stored in locked, HIPAA-compliant files, both physical and electronic. Access is restricted to authorized personnel only.
- Protected electronic health records (EHR): Using password-protected EHR systems with appropriate access controls and encryption to prevent unauthorized access or data breaches.
- Limited information sharing: I only disclose client information to other healthcare professionals or authorized individuals with a clear need-to-know basis, always obtaining informed consent beforehand.
- Compliance training: Regular HIPAA compliance training ensures I remain updated on all regulations and best practices for protecting client privacy.
- Incident reporting: Any potential breach of confidentiality or HIPAA violation is immediately reported to the appropriate authorities and addressed accordingly.
Maintaining client confidentiality builds trust, which is essential for successful treatment. Clients need to feel safe and comfortable sharing sensitive information without fear of judgment or disclosure.
Q 11. Describe your experience with documentation and record-keeping in substance abuse treatment.
My experience with documentation and record-keeping in substance abuse treatment is extensive. Accurate and thorough documentation is critical for effective treatment and legal compliance. I utilize electronic health records (EHRs) to maintain comprehensive client files, including:
- Intake assessments: Detailed assessments of the client’s substance use history, medical history, psychological history, and social support network.
- Treatment plans: Collaborative treatment plans outlining goals, interventions, and progress monitoring.
- Session notes: Concise and accurate documentation of each therapy session, outlining client progress, challenges, and goals discussed.
- Medication management: Detailed records of any prescribed medications, including dosage, frequency, and any side effects.
- Progress notes: Regular updates on the client’s progress toward treatment goals, as well as any setbacks or changes in the treatment plan.
I follow strict guidelines to ensure my documentation is accurate, objective, and free of bias. This is crucial for continuity of care, facilitating smooth transitions between providers, and maintaining a clear audit trail for legal and regulatory purposes.
Q 12. How do you work with families affected by substance abuse?
Working with families affected by substance abuse involves a multi-faceted approach focused on education, support, and empowerment. I often involve families in treatment by:
- Providing education: Explaining the nature of addiction, the impact on the family system, and available resources.
- Facilitating family therapy: Utilizing evidence-based family therapy approaches to improve communication, address family conflict, and build healthier relationships.
- Offering support groups: Connecting families with support groups where they can share experiences and learn from others facing similar challenges.
- Empowering families: Encouraging family members to develop coping skills, set healthy boundaries, and prioritize their own well-being.
- Addressing co-occurring disorders: Recognizing that family members may also be experiencing mental health challenges and providing appropriate referrals.
For example, I might facilitate a family meeting where family members can learn about addiction as a disease, practice effective communication techniques, and discuss strategies for supporting their loved one without enabling harmful behaviors. The goal is to equip families with the knowledge and tools they need to navigate this difficult situation effectively and support the recovery process.
Q 13. What are the signs and symptoms of opioid withdrawal?
Opioid withdrawal symptoms can be severe and dangerous, varying in intensity depending on the type of opioid, the dosage, and the individual’s history. Symptoms typically begin within hours of the last dose and can last for several days to weeks. They include:
- Gastrointestinal issues: Nausea, vomiting, diarrhea, abdominal cramping
- Musculoskeletal symptoms: Muscle aches, bone pain
- Central nervous system effects: Anxiety, irritability, restlessness, insomnia, depression
- Autonomic nervous system effects: Sweating, dilated pupils, increased heart rate and blood pressure, chills and goosebumps
- Severe symptoms: In severe cases, opioid withdrawal can lead to seizures, hallucinations, and potentially death.
It’s crucial to understand that opioid withdrawal is a medical emergency and should be managed under the supervision of a qualified medical professional. Medication-assisted treatment (MAT), such as methadone or buprenorphine, can significantly reduce the intensity of withdrawal symptoms and improve the chances of successful recovery.
Q 14. Describe different types of pharmacological interventions for substance use disorders.
Pharmacological interventions for substance use disorders play a vital role in treatment, particularly for opioid, alcohol, and nicotine dependence. These interventions aim to reduce cravings, withdrawal symptoms, and relapse rates. Some examples include:
- Methadone and buprenorphine for opioid use disorder: These medications reduce opioid cravings and withdrawal symptoms, allowing individuals to stabilize and focus on other aspects of recovery.
- Naltrexone for opioid and alcohol use disorder: This medication blocks the effects of opioids and reduces alcohol cravings.
- Acamprosate and nalmefene for alcohol use disorder: These medications help reduce alcohol cravings and the risk of relapse.
- Nicotine replacement therapy (NRT) for nicotine dependence: NRT products, such as patches, gum, and lozenges, provide nicotine in a controlled manner to reduce withdrawal symptoms and cravings.
- Other medications: Various other medications may be used to treat co-occurring mental health disorders which often accompany substance use disorders.
It’s important to emphasize that medication should be part of a comprehensive treatment plan, including counseling, behavioral therapy, and support services. The choice of medication depends on the individual’s specific needs and the type of substance use disorder.
Q 15. What is your experience working with diverse populations struggling with substance abuse?
My experience working with diverse populations struggling with substance abuse spans over ten years, encompassing work in both inpatient and outpatient settings. I’ve worked with individuals from various socioeconomic backgrounds, ethnicities, ages, genders, and sexual orientations, each presenting unique challenges and needs related to their substance use. For example, I’ve supported LGBTQ+ individuals navigating the added complexities of stigma and discrimination within the substance abuse treatment system. I’ve also worked extensively with individuals experiencing homelessness, addressing the interconnectedness of substance abuse and housing instability. My approach is always culturally sensitive and trauma-informed, recognizing that individual experiences shape both substance use and the response to treatment.
Understanding the cultural context is crucial. What might be considered acceptable behavior in one culture could be interpreted differently in another, potentially affecting how someone interacts with treatment professionals and adheres to the treatment plan. For example, a client from a collectivist culture might prioritize family needs over individual treatment goals, a nuance that requires careful consideration and adaptation in my approach.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you assess a client’s readiness for change?
Assessing a client’s readiness for change is paramount in effective substance abuse treatment. I utilize a variety of tools and techniques, including motivational interviewing, to gauge their level of commitment to recovery. This involves exploring their ambivalence towards change, identifying their strengths and resources, and collaboratively setting realistic goals. I might use validated scales such as the Readiness to Change Questionnaire (RTCQ) to provide a structured assessment.
However, formal assessments are only part of the picture. I also pay close attention to the client’s verbal and nonverbal cues during our sessions. For instance, a client who consistently expresses doubt about their ability to change, or minimizes the severity of their substance use, might be demonstrating low readiness for change, even if their scores on a formal assessment suggest otherwise. Building trust and establishing a strong therapeutic alliance is critical to accurately assessing their readiness.
Q 17. Explain the stages of change model (Transtheoretical Model).
The Transtheoretical Model, or Stages of Change model, is a framework that describes the process of behavioral change, including recovery from substance abuse. It proposes that individuals move through five distinct stages:
- Precontemplation: The individual is unaware of or unwilling to acknowledge a problem.
- Contemplation: The individual recognizes a problem but hasn’t committed to change.
- Preparation: The individual is making plans to change.
- Action: The individual is actively taking steps to change their behavior.
- Maintenance: The individual is working to maintain the changes they’ve made.
Understanding these stages allows me to tailor interventions to meet the client where they are in their journey. For example, a client in the precontemplation stage might benefit from psychoeducation and motivational interviewing to raise their awareness of the problem. A client in the action stage might need support with relapse prevention strategies.
It’s important to remember that individuals can relapse and cycle back through the stages. This is a normal part of the recovery process and doesn’t indicate failure. My role is to provide ongoing support and encouragement throughout this process.
Q 18. How would you build rapport with a client who is distrustful?
Building rapport with a distrustful client requires patience, empathy, and a genuine commitment to understanding their perspective. It’s crucial to avoid judgmental language or pressure. I begin by actively listening, validating their feelings, and acknowledging their past experiences. I might say something like, “I understand that you’ve had negative experiences in the past, and it’s understandable that you might be hesitant to trust me.” Building trust is a gradual process, and it’s essential to respect their boundaries.
Demonstrating competence and consistency in my actions is vital. Following through on promises, being punctual, and maintaining confidentiality builds credibility. I also focus on collaboratively setting goals, empowering them to take ownership of their treatment. Small victories and gradual progress contribute significantly to fostering trust. For instance, successfully completing a small step in their recovery plan, such as attending a support group, can build confidence and encourage further engagement.
Q 19. What is your experience with motivational interviewing techniques?
Motivational Interviewing (MI) is a cornerstone of my practice. It’s a client-centered, directive method that helps individuals explore and resolve ambivalence about change. I use MI techniques such as open-ended questions, affirmations, reflective listening, and summaries to guide the client towards their own solutions. For example, instead of telling a client to quit smoking, I might ask, “What are some of the pros and cons of continuing to smoke?” and use reflective listening to help them explore their feelings and values around this behavior.
The core principles of MI – collaboration, evocation, autonomy, and compassion – inform my interactions. I avoid direct confrontation or arguments, focusing instead on understanding and supporting the client’s intrinsic motivation to change. I’ve found it particularly effective with clients who initially present with strong resistance to treatment, helping them move from resistance to contemplation and action.
Q 20. How do you handle ethical dilemmas in substance abuse treatment?
Ethical dilemmas in substance abuse treatment are frequent. For example, maintaining client confidentiality while also ensuring their safety might pose a conflict. If a client discloses a plan to harm themselves or others, I’m ethically obligated to breach confidentiality and notify the appropriate authorities. Balancing the client’s autonomy with their safety is a constant consideration.
I navigate ethical dilemmas by adhering to a code of ethics, consulting with colleagues and supervisors, and utilizing ethical decision-making frameworks. These frameworks often involve identifying the ethical issues involved, gathering relevant information, considering potential consequences, and seeking input from various stakeholders. Thorough documentation of all decisions and interactions is critical in protecting both the client and the professional.
Q 21. Describe your experience with community resources for substance abuse.
My experience working with community resources for substance abuse is extensive. I regularly collaborate with local hospitals, mental health clinics, support groups (e.g., AA, NA), halfway houses, and social service agencies. These collaborations are crucial in providing comprehensive and holistic care. For instance, I might refer a client to a local detox facility for medically-assisted withdrawal, connect them with housing support, or assist them in accessing medication-assisted treatment (MAT). I also regularly attend interagency meetings to stay abreast of available resources and coordinate care with other professionals.
Building strong relationships with these community partners is vital. Understanding their strengths, limitations, and referral processes ensures efficient and effective service delivery for my clients. For example, knowing which agencies have specialized programs for specific populations (e.g., pregnant women, veterans) helps ensure clients receive the most appropriate and effective care.
Q 22. What are some common barriers to treatment for substance use disorders?
Many barriers hinder individuals from seeking and completing substance use disorder (SUD) treatment. These can be broadly categorized into financial, logistical, systemic, and personal obstacles.
Financial Barriers: The high cost of treatment, including therapy, medication, and residential programs, is a significant hurdle. Lack of insurance coverage or insufficient income often prevents individuals from accessing necessary care. For example, someone might need to choose between paying for rent and attending a crucial therapy session.
Logistical Barriers: Geographic location, lack of transportation, childcare needs, and inflexible work schedules can all impede access to treatment. Someone living in a rural area with limited public transport might find it impossible to attend regular appointments in a distant city.
Systemic Barriers: Waitlists for treatment, insufficient treatment capacity, and the stigma surrounding SUDs create obstacles. The sheer wait time to enter a program can deter individuals already struggling with motivation and willpower.
Personal Barriers: Denial of the problem, fear of judgment, lack of self-efficacy, and comorbid mental health conditions can prevent individuals from seeking help. Someone struggling with both depression and addiction might be reluctant to disclose their struggles, believing they cannot cope with another layer of treatment.
Q 23. How would you adapt your treatment approach to different clients’ needs?
Adapting my treatment approach is crucial for effective care. I personalize treatment plans by considering each client’s unique needs, strengths, and preferences. This involves a thorough assessment, utilizing evidence-based practices, and fostering a strong therapeutic alliance.
Individualized Treatment Plans: I collaborate with clients to develop personalized goals and strategies, considering their specific substance(s) of choice, the severity of their addiction, co-occurring disorders, and personal circumstances. For example, someone with a history of trauma might benefit from trauma-informed therapy in addition to traditional addiction treatment.
Evidence-Based Practices: I utilize proven methods like Cognitive Behavioral Therapy (CBT), Motivational Interviewing (MI), and contingency management to address specific needs. CBT helps clients identify and change negative thought patterns contributing to their addiction, while MI supports self-motivation for change.
Collaboration and Referral: I work collaboratively with other healthcare professionals, such as psychiatrists, primary care physicians, and social workers, to provide holistic care. If a client requires medication-assisted treatment or needs support with housing or employment, I make appropriate referrals.
Therapeutic Alliance: Building a strong, trusting relationship with clients is paramount. This involves empathy, active listening, and respect for client autonomy. A comfortable and safe environment allows clients to feel understood and more open to exploring their issues.
Q 24. Describe your understanding of the disease model of addiction.
The disease model of addiction views addiction as a chronic, relapsing brain disease, similar to other chronic conditions like diabetes or heart disease. It emphasizes the biological, psychological, and social factors contributing to addiction. It’s crucial to understand that addiction isn’t simply a matter of willpower; it’s a complex interplay of factors that affect brain function and behavior.
Biological Factors: Genetic predisposition, brain chemistry imbalances, and the effects of substances on the brain are all crucial components. For instance, a person with a family history of alcoholism might have a higher genetic vulnerability to addiction.
Psychological Factors: Mental health disorders like depression, anxiety, and trauma can significantly increase the risk and severity of addiction. These conditions often lead to self-medication with substances.
Social Factors: Environmental influences, such as peer pressure, access to substances, and family dynamics, all play a significant role. Growing up in an environment where substance use is normalized can increase the risk of developing an addiction.
Treatment Implications: The disease model supports a long-term treatment approach that incorporates various interventions tailored to address the specific needs of the individual. This includes medication, therapy, support groups, and lifestyle changes.
Q 25. How do you ensure cultural competency in your work with clients?
Cultural competency is essential for effective treatment of SUDs. I ensure this by actively learning about and respecting diverse cultural backgrounds, beliefs, and practices. This means being mindful of how cultural factors can influence treatment outcomes and tailoring interventions to best suit the client.
Self-Reflection: I regularly engage in self-reflection to identify my own biases and assumptions about different cultures.
Cultural Humility: I approach each client with humility, acknowledging that I don’t have all the answers and actively seeking to learn from their experiences.
Culturally Appropriate Interventions: I utilize interventions that respect and incorporate clients’ cultural values and preferences. For example, if working with an indigenous client, I might incorporate traditional healing practices into the treatment plan.
Language Access: I ensure access to qualified interpreters and culturally appropriate materials when necessary.
Collaboration with Community Resources: I connect clients with culturally relevant community resources and support networks to strengthen their recovery journey.
Q 26. What are your strengths and weaknesses as a substance abuse professional?
My strengths include my strong therapeutic alliance building skills, my comprehensive understanding of addiction treatment modalities, and my ability to adapt to diverse client needs. I am also proficient in collaborating with other healthcare professionals to ensure holistic care. My weakness is sometimes over-committing myself, potentially leading to burnout. To mitigate this, I’m actively working on setting stronger boundaries and practicing self-care techniques.
Q 27. How do you maintain your own well-being while working in a demanding field like substance abuse treatment?
Maintaining well-being in this demanding field requires proactive strategies. Compassion fatigue and secondary trauma are real risks, so self-care is not a luxury, but a necessity.
Supervision and Peer Support: Regular supervision with experienced colleagues allows for processing challenging cases and prevents burnout. Peer support groups provide a safe space to share experiences and receive encouragement.
Self-Care Practices: Prioritizing activities that promote mental and physical health, such as exercise, mindfulness, spending time in nature, and engaging in hobbies are essential. Even small acts of self-care can significantly impact well-being.
Boundary Setting: Establishing and maintaining healthy professional boundaries is critical to prevent emotional exhaustion. This involves limiting work outside of designated hours and avoiding over-identification with clients.
Stress Management Techniques: Employing stress-reduction techniques such as deep breathing exercises, yoga, or meditation can help manage the emotional demands of the work.
Q 28. Describe a time you had to make a difficult decision in your work with clients.
I once had to make a difficult decision regarding a client who was mandated to attend treatment by the court but was actively resisting participation and expressing a lack of desire to change. I had to weigh the ethical obligation to follow the court mandate with my duty to provide client-centered care. After multiple sessions employing motivational interviewing techniques, it became clear that forcing treatment wasn’t going to be effective. I worked with the client to explore alternative solutions which would eventually lead to engagement with services, but not force participation.
The decision involved collaborating with the court and the client’s legal team to propose a modified treatment plan that prioritized the client’s autonomy while still addressing the legal requirements. It was a difficult decision because it required navigating complex legal and ethical considerations, but ultimately, prioritizing client autonomy, even if it meant not strictly adhering to the court mandate, led to a more collaborative and successful outcome.
Key Topics to Learn for Substance Abuse Awareness Interview
- Understanding Addiction: Explore the biological, psychological, and social factors contributing to substance use disorders. Consider the different models of addiction and their implications for treatment.
- Types of Substances and Their Effects: Familiarize yourself with the common types of substances (e.g., opioids, stimulants, depressants, alcohol) and their respective effects on the body and mind. Be prepared to discuss the short-term and long-term consequences of abuse.
- Prevention and Intervention Strategies: Learn about evidence-based prevention programs targeting various populations. Understand different intervention approaches, including motivational interviewing and harm reduction strategies.
- Treatment and Recovery: Research various treatment modalities (e.g., detoxification, medication-assisted treatment, therapy) and the stages of recovery. Understand the importance of relapse prevention and aftercare planning.
- Ethical and Legal Considerations: Become familiar with the ethical considerations surrounding confidentiality, mandated reporting, and informed consent in the context of substance abuse treatment. Understand relevant laws and regulations.
- Cultural Sensitivity and Diversity: Recognize the impact of culture, ethnicity, and socioeconomic status on substance use and treatment outcomes. Develop an understanding of culturally competent practices.
- Data Analysis and Program Evaluation: Learn how to interpret data related to substance use trends and the effectiveness of prevention and treatment programs. Be ready to discuss program evaluation methodologies.
Next Steps
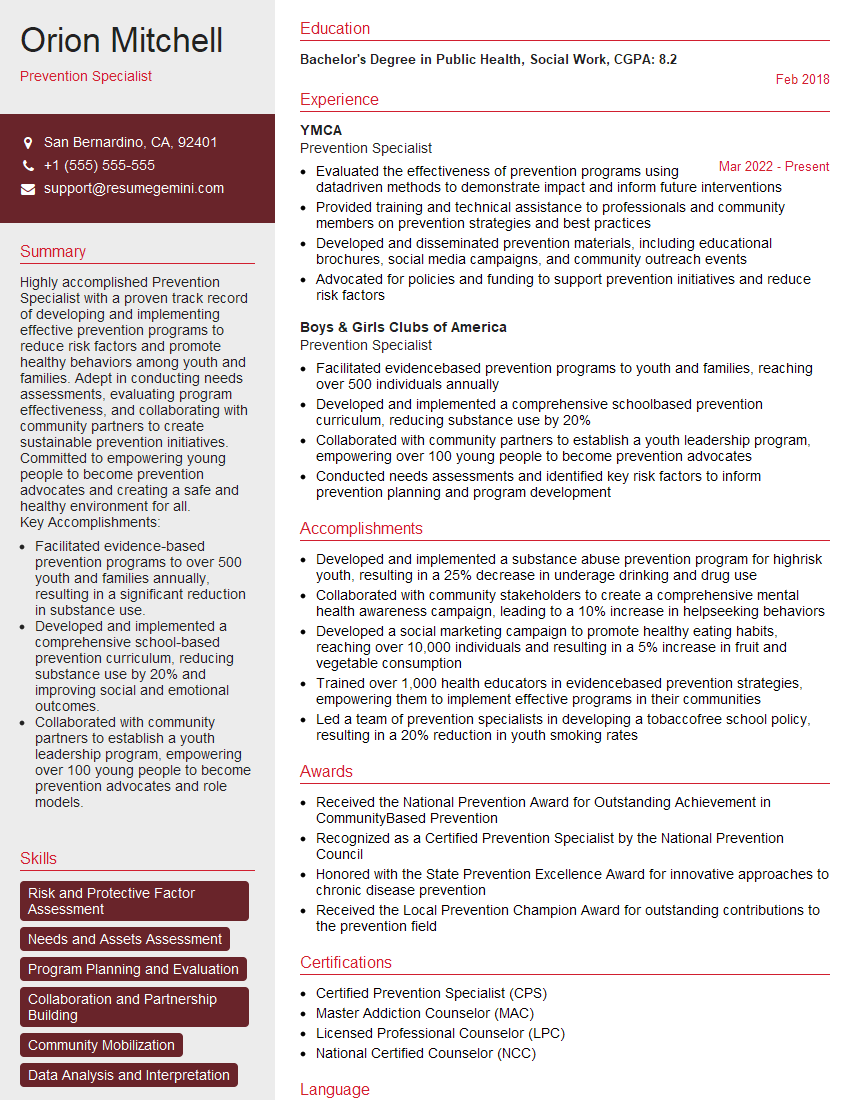
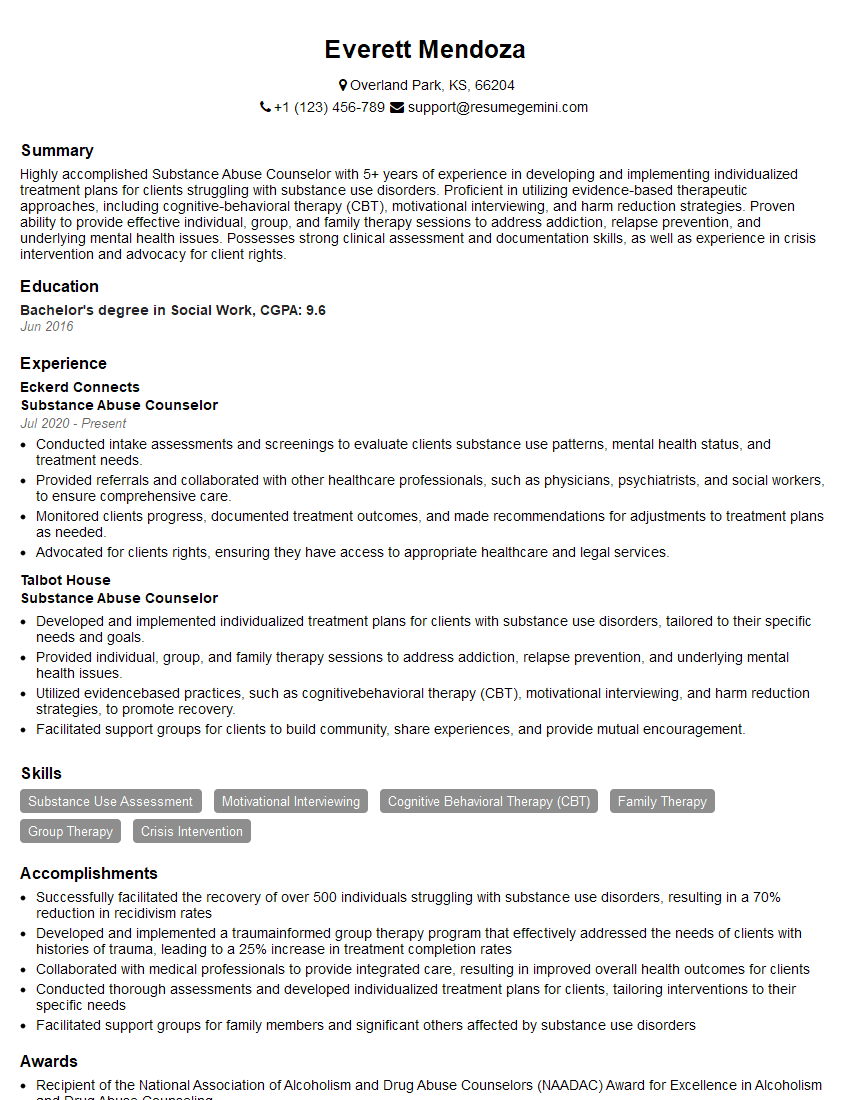
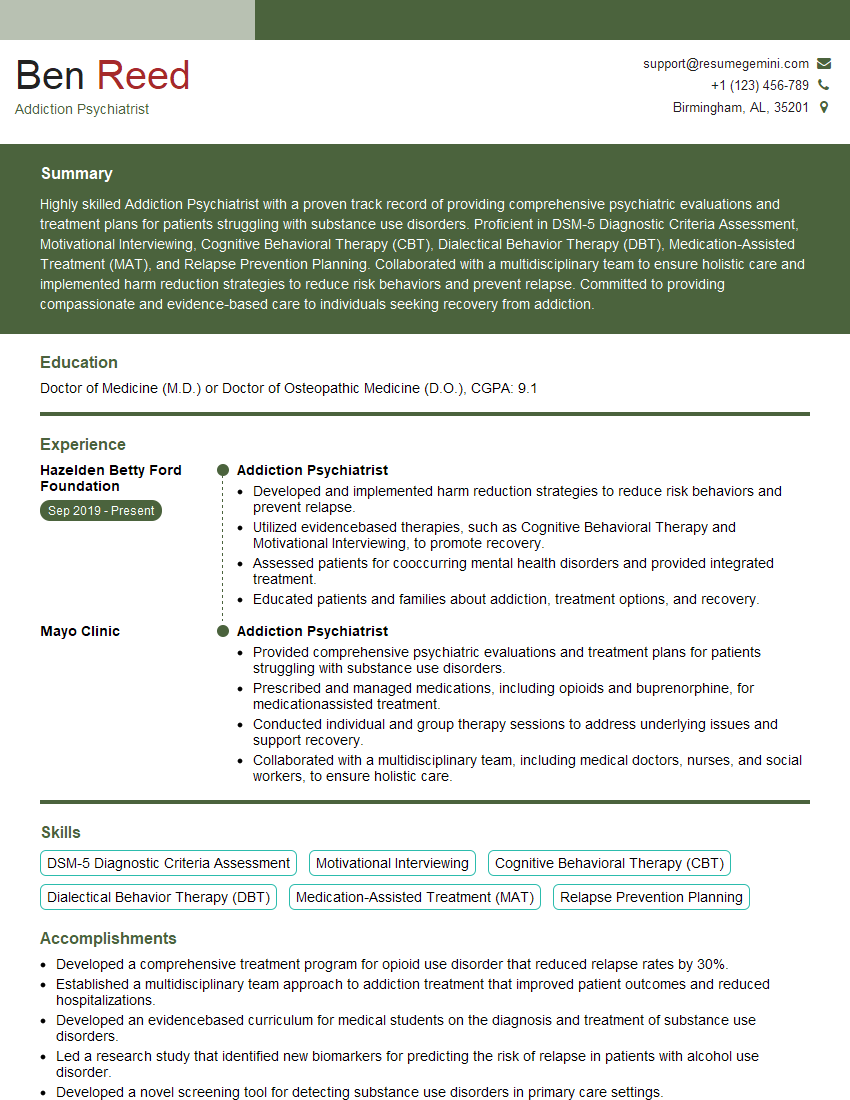
Mastering Substance Abuse Awareness is crucial for career advancement in this vital field. A strong understanding of these concepts demonstrates your commitment to helping individuals and communities overcome the challenges of addiction. To maximize your job prospects, creating an ATS-friendly resume is essential. ResumeGemini is a trusted resource to help you build a professional and impactful resume that highlights your skills and experience. Examples of resumes tailored to Substance Abuse Awareness roles are available within ResumeGemini to guide you in creating a compelling application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
I Redesigned Spongebob Squarepants and his main characters of my artwork.
https://www.deviantart.com/reimaginesponge/art/Redesigned-Spongebob-characters-1223583608
IT gave me an insight and words to use and be able to think of examples
Hi, I’m Jay, we have a few potential clients that are interested in your services, thought you might be a good fit. I’d love to talk about the details, when do you have time to talk?
Best,
Jay
Founder | CEO